Abstract
Liver abscesses are infectious, space occupying lesions in the liver, the two most common abscesses being pyogenic and amoebic. A pyogenic liver abscess (PLA) is a rare condition with a reported incidence of 20 per 100 000 hospital admissions in the western population. The right lobe of the liver is the most common site in both types of liver abscess. Clinical presentation is elusive with complaints of fever, right upper quadrant pain in the abdomen and hepatomegaly with or without jaundice. The aetiology of PLA has changed in the past few decades and may be of biliary, portal, arterial or traumatic origin, but many cases are still cryptogenic. The most common organisms causing PLA are Gram-negative aerobes, especially Escherichia coli and Klebsiella pneumoniae. Studies have shown a high degree of antimicrobial susceptibility of isolated organism resulting in an overall lower mortality in PLA. Here, we present a case of PLA caused by multidrug-resistant Citrobacter freundii, which is an unusual organism to be isolated.
Background
Multidrug-resistant Citrobacter freundii infection in a healthy individual with no prior risk factor is a rare entity.
Though this pathogen affects populations at extremes of age or those who are immunocompromised, clinical isolation from disseminated infection in immunocompetent patients is a reality.
Pyogenic liver abscess has multiple clinical complications of which spontaneous rupture is one of the major concerns of physicians. Rupture in the thoracic cavity may prove life-threatening in cases involving the pleural or pericardial cavity; however, rupture into the bronchus carries a relatively benign course.
There are no comparative studies of antibiotic therapy to establish a treatment strategy for infections caused by the various Citrobacter species.
Case presentation
A 58-year-old previously healthy male farmer by occupation, who was a chronic alcoholic, came with complaints of low-grade intermittent fever since 1 week, right upper quadrant pain in abdomen since 5 days, right-sided chest pain since 3 days and productive cough since 2 days. On examination, the patient was febrile with a temperature of 101 F, pulse rate 108/min, BP 124/70 mm Hg. There was no pallor, icterus, clubbing or pedal oedema. On abdominal examination, tender hepatomegaly was present. Respiratory examination showed reduced air entry along with fine crepts in the right infrascapular and axillary regions. Cardiovascular and cental nervous system examination were within normal limits.
Investigations
Laboratory investigations revealed a total leucocyte count (TLC) count of 26 400/mm3 with a differential leucocyte count of 84% polymorphs, 15% lymphocytes. Blood sugar, renal function, liver function tests and serum electrolytes were normal except for serum alkaline phosphatase which was markedly raised at 927 IU/l. Sputum Gram stain and acid-fast bacilli were negative. ELISA was negative for HIV, amoebic serology and blood cultures. The chest x-ray was suggestive of minimal right-sided pleural effusion with an elevated right dome of the diaphragm with an air-fluid level (figure 1). The ultrasound-guided abdomen showed a hypoechoic area in the right lobe of the liver, probably an abscess. We managed the patient on the lines of liver abscess with injections of ceftriaxone and metronidazole.
Figure 1.
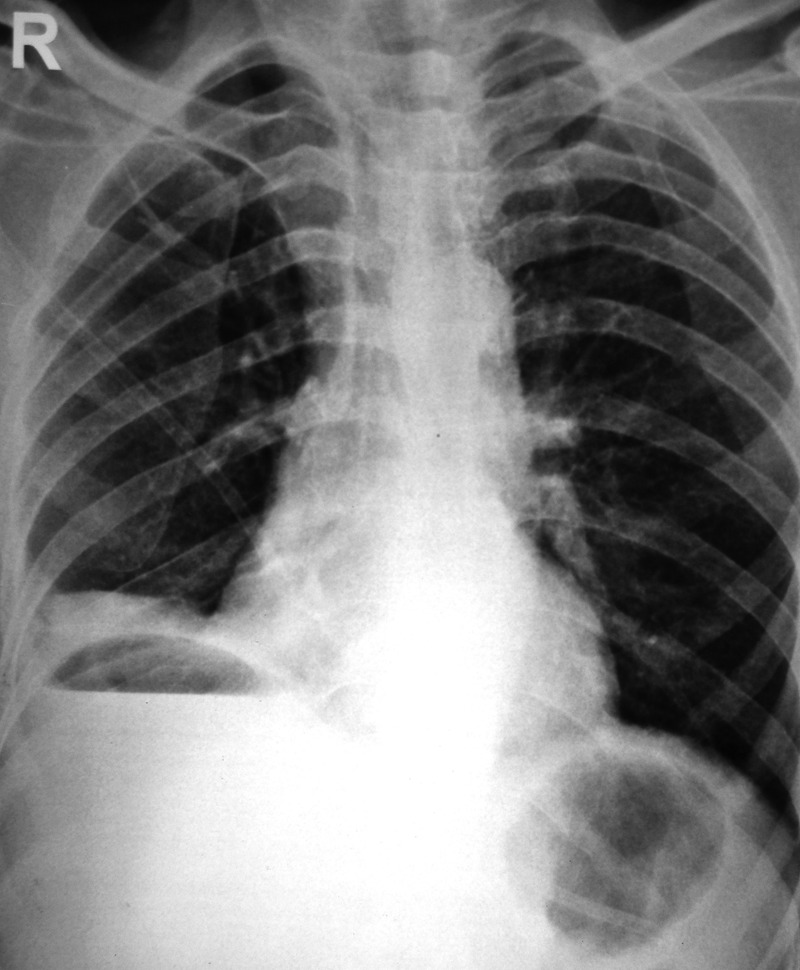
Posteroanterior view of a chest radiograph 3 days after the onset of fever, showing a minimal right-sided pleural effusion and a raised right dome of the diaphragm with an air-fluid level.
However, even after 48 h of intravenous antibiotics, there was minimal improvement in his symptoms. So contrast-enhanced CT (CECT) of the abdomen was done, which showed a large subcapsular liver abscess in segments 7 and 8 measuring 13.1×12.7×7.3 cm with contained air foci with mild right-sided pleural effusion and basal atelectasis (figures 2–4). A therepeutic pleural tap was done, and the biochemical evaluation showed sugar 109 mg/dl, protein 4 g/dl, with 300cells (65% polymorph, 35% mononuclear cells). On culture, C freundii was grown, which was resistant to ampicillin, gentamycin, ciprofloxacin, cotrimoxazole, amikacin, ceftriaxone and piperacillin+tazobactam and sensitive to meropenem only.
Figure 2.
Transverse section contrast-enhanced CT of the chest showing right-sided consolidation with loculated pleural effusion.
A CT-guided percutaneous liver abscess drainage was done with a pigtail insertion under all aseptic precautions and approximately 300 ml of pus was aspirated (figure 5). A subsequent chest radiograph showed the formation of right lower zone pneumonia with moderate pleural effusion (figure 9). On culture, again C freundii was grown from the pus sample, which was resistant to gentamycin, ciprofloxacin, cotrimoxazole, amikacin, ceftriaxone and piperacillin+tazobactam and sensitive to meropenem and aztreonam (figures 6–8).
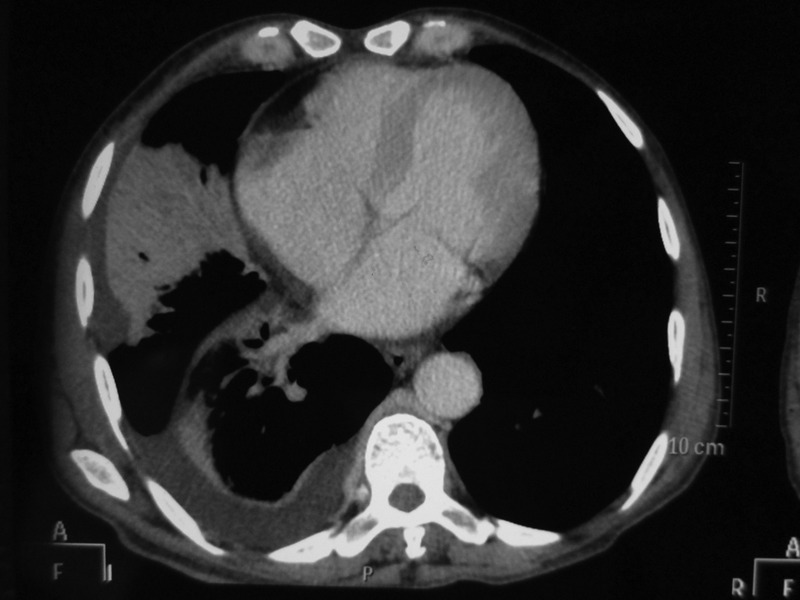
Figure 3.

Transverse contrast-enhanced CT section of the upper abdomen revealing a large subcapsular hypoechoic homogeneous space occupying lesion in the right lobe of the liver with evidence of multiple air pockets suggestive of an abscess.
Figure 4.
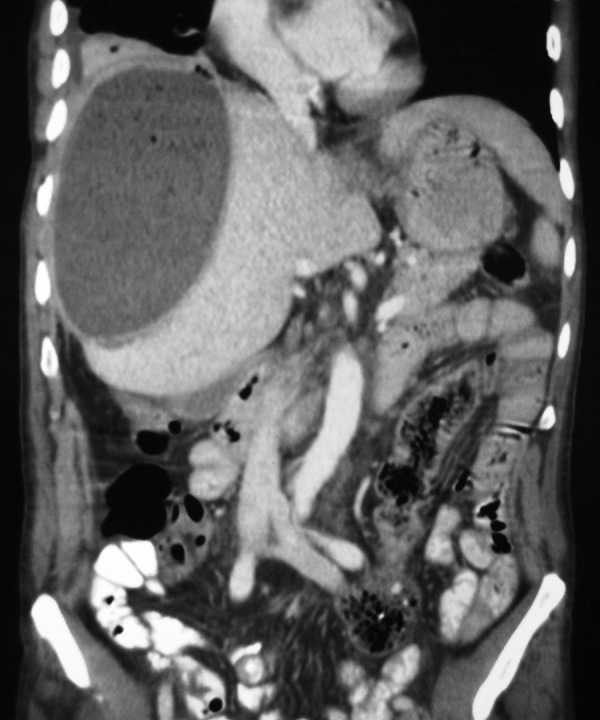
Coronal section of contrast-enhanced CT abdomen showing right lobe hepatomegaly with the large abscess abutting the hepatic capsule.
Figure 5.

Check non-contrast CT liver of the same patient after pigtail drainage of the abscess.
Treatment
The patient's drug treatment was revised based on the culture and sensitivity report, and the patient was given an injection of meropenem over the next 2 weeks.
Outcome and follow-up
The patient showed marked improvement within a few days with a gradual decrease in symptoms. His TLC count after 1 week of meropenem was 8700/mm3. A repeat CECT of the abdomen after 2 weeks of intravenous antibiotics showed residual liver abscess in the right lobe of the liver with minimal right pleural effusion. The patient was discharged on oral antibiotics and is doing well on follow-up visits.
Discussion
Citrobacter is a genus of Gram-negative coliform bacteria in the Enterobacteriaceae family. Citrobacter species are commonly found in water, soil, food and the intestinal tracts of animals and humans. Many infections are nosocomially acquired; however, they can also be community-acquired. They are rarely the source of illnesses. Two groups of patients are at risk of acquiring Citrobacter infections. The first group is of neonates, who may develop sepsis, meningitis and brain abscesses.1 The second group is of debilitated or immune-compromised patients.2 Citrobacter can cause a wide spectrum of infections in humans, such as infections in the urinary tract, respiratory tract, wounds, bone, peritoneum, endocardium, meninges and bloodstream.3 Among the various sites of infection, the urinary tract is the most common, followed by the skin/soft tissues. However, liver abscess caused by Citrobacter is a rare entity with only a few cases reported so far, with Citrobacter koseri being more frequent than C freundii (figures 6–9).
Figure 6.

Citrobacter spp. growth: pink coloured mucoid, velvety, smooth colonies cultured in MacConkey's media.
Figure 7.

Citrobacter spp. growth: pale white discrete colonies cultured on blood agar.
Figure 8.

Citrobacter fruendii identified on biochemical analysis with indole-negative, Triple sugar iron-positive with H2S production, citrate-positive and urease-negative (from left to right).
Figure 9.
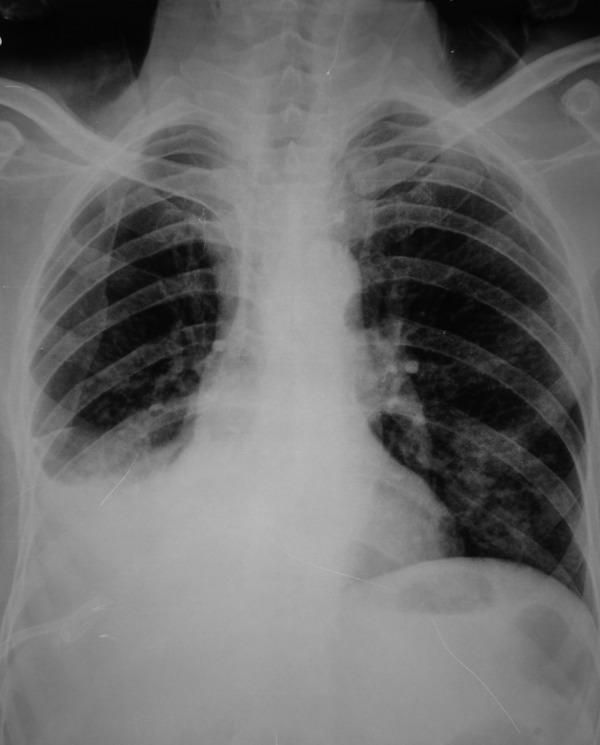
Repeat chest x-Ray demonstrating right lower zone pneumonia and moderate pleural effusion.
Different species of Citrobacter demonstrate different antimicrobial susceptibility profiles. C freundii is generally much more resistant to antimicrobial agents than C koseri and Citrobacter amalonaticus. The minimum inhibitory concentrations (MICs) of various antimicrobial agents for C freundii are higher than those for C koseri.4 C freundii isolates have recently been reported to express resistance to anti-pseudomonal penicillins, first, second and third generation cephalosporins, gentamicin, tobramycin and aztreonam.5 Cefepime, cefpirome, imipenem and meropenem remained the most active agents against C freundii.6
In the present case, the patient arrived at the medical emergency department with sepsis secondary to a large pyogenic liver abscess due to the gas-forming bacteria, Citrobacter. Owing to the increased intracavitary pressure of the abscess, the patient presented with subsequent complaints of productive cough and chest pain, as a result of formation of hepatobronchial fistula, which in turn led to the development of pneumonia and infected pleural effusion.
From a review of the literature of Citrobacter causing hepatic abscess, two instances were found, one reported by Laynez Bretones et al,7 and the other as an ascending cholangitis as a cause of pyogenic liver abscesses due to C fruendii complicated by a gastric submucosal abscess and fistula reported by Yamada et al.8
There are no comparative studies of antibiotic therapy for Citrobacter infections. Thus, the treatment of Citrobacter infections follows the principles for treatment of other Enterobacteriaceae infections. It is also not really known whether there is any difference between the treatment of Citrobacter infections and the treatment of other Enterobacteriaceae infections. So with this case of the multidrug-resistant Citrobacter liver abscess, we recommend that more studies on citrobacter infection should be done to get a better understanding of its risk factor, aetiology and management.
Learning points.
Citrobacter species are a rare cause of illness and are most commonly associated with nosocomial infections.
Different species of Citrobacter demonstrate different antimicrobial susceptibility profiles with Citrobacter freundii being much more resistant to antimicrobial agents than Citrobacter koseri and Citrobacter amalonaticus.
Complications such as rupture of the abscess in cases of pyogenic liver abscess must be highly suspect, especially in this case where the patient also developed a productive cough. However, hepatobronchial fistula acts as a safety valve by decompressing the abscess cavity.
Treatment with antimicrobials depends on the culture and drug susceptibility report, but in view of the emerging drug resistance in Gram-negative isolates, a physician should give a broad coverage of antibiotics till laboratory reports are available.
Footnotes
Contributors: PK prepared and wrote the manuscript. SG was involved in the complete workup of the case. AKG managed the patient through the period. DR was involved in the diagnosis of the patient.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Kline MW. Citrobacter meningitis and brain abscess in infancy: epidemiology, pathogenesis, and treatment. J Pediatr 1988;2013:430–4 [DOI] [PubMed] [Google Scholar]
- 2.Whalen JG, Mully TW, Enlgish JC., III ‘Spontaneous Citrobacter freundii infection in an immunocompetent patient’. Arch Dermatol 2007;2013:124–5 [DOI] [PubMed] [Google Scholar]
- 3.Lipsky BA, Hook EW, III, Smith AA, et al. Citrobacter infections in humans: experience at the Seattle Veterans Administration Medical Center and a review of the literature. Rev Infect Dis 1980;2013:746–60 [DOI] [PubMed] [Google Scholar]
- 4.Samonis G, Ho DH, Gooch GF, et al. In vitro susceptibility of Citrobacter species to various antimicrobial agents. Antimicrob Agents Chemother 1987;2013:829–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim PW, Harris AD, Roghmann MC, et al. Epidemiological risk factors for isolation of ceftriaxone-resistant versus -susceptible citrobacter freundii in hospitalized patients. Antimicrob Agents Chemother 2003;2013:2882–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang JT, Chang SC, Chen YC, et al. Comparison of antimicrobial susceptibility of Citrobacter freundii isolates in two different time periods. J Microbiol Immunol Infect 2000;2013:258–62 [PubMed] [Google Scholar]
- 7.Bretones F Laynez, López Martínez G, Díez García F, et al. Citrobacter freundii, a rare cause of hepatic abscess. Ann Med Int 1998;2013:452. [PubMed] [Google Scholar]
- 8.Yamada T, Murakami K, Tsuchida K, et al. Ascending cholangitis as a cause of pyogenic liver abscesses complicated by a gastric submucosal abscess and fistula. J Clin Gastroenterol 2000;2013:317–20 [DOI] [PubMed] [Google Scholar]


