Abstract
This article reports on the case of a 63-year-old Jamaican man who presented with progressive dysphagia and dysphonia. CT was able to visualise several large anterior cervical osteophytes, which were protruding into soft tissue structures such as the pharynx and oesophagus. Surgical removal of C3–C6 was undertaken but severe damage to local structures had already occurred. The patient remained nil by mouth and had a percutaneous gastrostomy feeding tube for means of nutrition. Four months later, despite the removal of the osteophytes, videofluoroscopy demonstrated that the patients swallow remained unsafe. The patient suffered three episodes of aspiration pneumonia and although their speech improved, they remain nil by mouth at the time of going to publication.
Background
Diffuse idiopathic skeletal hyperostosis (DISH) describes a condition in which there is tendency towards ossification of ligament, tendon or joint capsule insertion, usually involving the spine.1–3 It is usually completely asymptomatic with a normal physical examination. Radiologically, however, changes appear as a distinct paravertebral mass anterior to vertebral body. It can occur at any level throughout the spine. The most common causes of cervical anterior osteophytes are ankylosing spondylitis and DISH.4
Case presentation
A 63-year-old Jamaican man presented to the emergency department with increasingly strange behaviour observed by neighbours, audible upper airway noises and changes in the tone of his speech. On closure questioning he described a history of progressive dysphagia with mild odynophagia, weight loss and shortness of breath. He had no fever, change in bowel habit or symptoms of anaemia.
He was well known to the psychiatric services in the area because of longstanding issues relating to treatment-resistant schizophrenia. On examination, he was a mildly cachexic man with obvious difficulties in swallowing his saliva. There were audible bubbling noises emanating from his upper airway and he was drooling at the mouth. On auscultation of the lungs, there were widespread crackles faintly audible above the upper airway noises. Examination was otherwise unremarkable.
Investigations
Erect chest x-ray
Increased opacification seen within the right lower zone which is suggestive of infective consolidation. Given the history, these findings could indicate aspiration pneumonia. The left lung appears clear.
Videofluoroscopy
The control view demonstrated large osteophytes of the cervical spine with marked degenerative changes. The anterior osteophytes anteriorly displace the oesophagus. Further evaluation with formal cervical spine x-rays are advised.
MRI lumbar spine
There is some mild-to-moderate white matter T2 hyperintensity which is non-specific but most likely on the basis of small vessel disease. There are multilevel cervical and upper thoracic osteophytes with vertebral body fusion. This is suggestive of DISH. It results in some impingement on the dorsal wall of hypopharynx which may relate to the clinical findings. There is no brain stem or base of skull abnormality.
CT cervical spine
There is extensive anterior cervical osteophytosis involving all vertebral levels. The most bulky element of this process is from C3 to C5 and is indenting the posterior inferior oropharyngeal wall and laryngeal inlet. The maximal depth is at C4, where the osteophyte measures 17 mm in antero-posterior diameter (approximately the same as the adjacent vertebral body) (figures 1 and 2 ).
Figure 1.
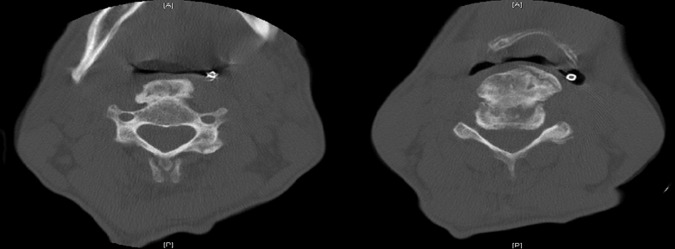
CT transverse sections of cervical spine showing anterior cervical osteophyte.
Figure 2.

CT showing sagittal section through cervical spine with prominent anterior cervical osteophytes.
Anteriorly, there is multilevel fusion of the cervical spine at every level except for C2/3 where there is probably an old fracture of the connecting anterior osteophyte. Posteriorly, there is fusion of the left C2/3, C5/6 and C6/7 facet joints, on the right there is fusion of the C5/6 facet joint.
Mild uncovertebral osteophytosis is seen from C3 to C5, but no resultant canal stenosis is seen on CT. There is foraminal narrowing bilaterally at C3/4 and C4/5.
Differential diagnosis
The causes of dysphagia can be divided into luminal, mural or extramural. With a robust history of progressive dysphagia and weight loss the most important differential to exclude is oesophageal carcinoma. Other conditions that commonly affect swallowing include achalasia, pharyngeal pouch, stroke, Parkinson's disease and motor neuron disease. Rarer causes include head and neck malignancies, ankylosing spondylitis and anterior cervical osteophytes and seen in DISH (figure 3).
Figure 3.

Image from videofluoroscopic scan showing unsafe swallow.
Treatment
Medical
Medical therapy used in this case included simple analgesics such as paracetamol, diclofenac and tramadol as required. However, due to the severity of this patient's symptoms, surgical removal of osteophytes was the definitive option.
Surgical
The surgical intervention in this case consisted of removal of the offending anterior osteophytes on vertebral levels C3–C6 (figure 4). The patient was placed in a supine horseshoe position. Intravenous antibiotics were given on induction and a transverse right collar incision was made over C4. Dissection to anterior cervical spine was undertaken. The thick prevertebral fascia was divided into layers. The carotid artery was felt and retracted laterally. Large osteophytes were then clearly visible. These were removed using a drill and nibbler. The drill was further used to smooth the anterior surface. Postoperative x-rays were taken to ensure all relevant levels had been successfully decompressed. The wound was closed with 2.0 vicryl to platsyma, 3.0 undyed vicryl subcut, steristrips to skin and a further absorbable dressing applied.
Figure 4.

Image intensifier picture taken during surgical removal of anterior cervical osteophytes.
Outcome and follow-up
The postoperative period provided a number of challenges for the patient and for the healthcare team. The patient required sectioning under the Mental Health Act because he refused to remain nil by mouth. He suffered three further episodes of aspiration pneumonia. He also pulled his Percutaneous Endoscopic gastrostomy (PEG) tube out on several occasions and also required 1:1 supervision to prevent him absconding. His symptoms were unchanged following surgery and he became increasingly disenchanted with his situation. His swallow was repeatedly assessed with videofluoroscopy which demonstrated only mild improvement over the next 4 months.
Discussion
DISH is a common non-inflammatory spinal enthesopathy of unknown aetiology characterised by osteophyte formation. More common in the elderly5 and in men, it is diagnosed by radiography. Characterised by the presence of osteophytes afflicting four sequential vertebral bodies together with the preservation of disc height (Reswick diagnostic criteria)5—in contrast to ankylosing spondylosis and degenerative disc disease. Despite first being described in the 1950s by Forestier and Rotes-Querol6 much about the aetiology of the condition remains unknown, with several risk factors postulated.7
The condition can affect anywhere along the vertebral column—most commonly afflicting the thoracic spine, causing back pain and stiffness. In the cervical spine, ossification of soft tissue on its anterior aspect and the formation of large osteophytes can result in a rare cause dysphagia due to mechanical oesophageal compression. Other complications include tracheal displacement, airway compromise, increased risk of fracture and potential spinal cord compression, as evidence by prior case reports.8 9 As the extent of oesophageal compression increases, so the dysphagia worsens and as in any patient with progressive dysphagia, oesophageal malignancy is an important differential.10
Management of this condition is primarily conservative including dietary modifications—soft diet and medications including bisphosphonates.11 12 However, in severe cases, where intrinsic oesophageal dysfunction has been ruled out, surgical intervention can provide an effective last resort.13
Limited case reports from surgical intervention have shown good results in the short term with effective symptom resolution.12–18 However, it still remains unclear regarding long-term outcomes, and as with any operation, risks include damage to surrounding structures, most significantly damage to recurrent and superior laryngeal nerves resulting in postoperative dysphagia.
As above, our patient presented with progressive dysphagia, dysarthria and weight loss over the last few months. His eventual CT scan showed extensive anterior cervical osteophytosis and multilevel fusion involving all vertebral levels, with the largest osteophytes seen from C3 to C5 and mass effect on the anterior soft tissue structures. Videofluoroscopy prior to the procedure showed severe oropharyngeal dysphagia, and pharyngeal weakness, and it was felt that despite the osteophytes contributing significantly to his dysphagia, there was an additional neurological component not explained by the mechanical compression.
As a result, despite a successful surgery, our patient has remained PEG fed, with his latest videofluoroscopy 1 month postoperatively showing a pharyngeal wall profile much improved, but continued lack of swallow coordination and high risk of aspiration.
Learning points.
Anterior cervical osteophytes should be considered a rare cause of progressive dysphagia.
Surgery may not necessarily improve symptoms.
Patients with psychiatric illness often present late, possibly when irreparable damage has been done.
Footnotes
Acknowledgements: We wish to thank the patient for agreeing to be involved is this case report. We also wish to thank him for allowing us to use images of his disease.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Miyazawa N, Akiyama I. Ossification of the ligamentum flavum of the cervical spine. J Neurosurg Sci 2007;2013:139–44 [PubMed] [Google Scholar]
- 2.Fornasier VL, Littlejohn G, Urowitz MB, et al. Spinal entheseal new bone formation: the early changes of spinal diffuse idiopathic skeletal hyperostosis. J Rheumatol 1983;2013:939–47 [PubMed] [Google Scholar]
- 3.Westerveld LA, Verlaan JJ, Oner FC. Spinal fractures in patients with ankylosing spinal disorders: a systematic review of the literature on treatment, neurological status and complications. Eur Spine J 2009;2013:145–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.De Jesus-Monge WE, Cruz-Cuevas EI. Dysphagia and lung aspiration secondary to anterior cervical osteophytes: a case report and review of the literature. Ethn Dis 2008;2013(2 Suppl 2):S2-137–40 [PMC free article] [PubMed] [Google Scholar]
- 5.Resnick D, Niwayama G. Diffuse idiopathic skeletal hyperostosis (DISH), in diagnosis of bone and joint disorders. 3rd edn Philadelphia: WB Saunders, 1995;. 2013:1463–95 [Google Scholar]
- 6.Forestier J, Rotes-Querol J. Senile ankylosing hyperostosis of the spine. Ann Rheum Dis 1950;2013:321–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Manatsathit W, Yen Phi Ha K. Narala a rare cause of dysphagia in an elderly patient. Gastroenterology 2012;20131154–400 [DOI] [PubMed] [Google Scholar]
- 8.Verlaan JJ, Boswijk BJ, de Ru JA,, et al. Diffuse idiopathic skeletal hyperostosis of the cervical spine: an underestimated cause of dysphagia and airway obstruction Spine J 2011;2013:1058–67 [DOI] [PubMed] [Google Scholar]
- 9.Naik B, Lobato EB, Sulek CA. Dysphagia, obstructive sleep apnea, and difficult fiberoptic intubation secondary to diffuse idiopathic skeletal hyperostosis. Anesthesiology 2004;2013:1311–12 [DOI] [PubMed] [Google Scholar]
- 10.Hanallah D, White AP, Goldberg G, et al. Diffuse idiopathic skeletal hyperostosis. Oper Tech Orthop 2007;2013:174–7 [Google Scholar]
- 11.Laus M, Malaguti MC, Alfonso C, et al. Dysphagia due to cervical osteophytosis. Chir Organi Mov 1995;2013:263–71 [PubMed] [Google Scholar]
- 12.Ozgocmen S, Kiris A, Kocakoc E, et al. Osteophyte-induced dysphagia: report of three cases. Joint Bone Spine 2002;2013:226–9 [DOI] [PubMed] [Google Scholar]
- 13.Urrutia J, Bono CM. Long-term results of surgical treatment of dysphagia secondary to cervical diffuse idiopathic skeletal hyperostosis. Spine J 2009;2013:e13–17 [DOI] [PubMed] [Google Scholar]
- 14.Fuerderer S, Eysel-Gosepath K, Schröder U, et al. Retro-pharyngeal obstruction in association with osteophytes of the cervical spine. J Bone Joint Surg Br 2004;2013:837–40 [DOI] [PubMed] [Google Scholar]
- 15.Goel R, Sampath P, Mikaelian DO. Dysphagia caused by cervical osteophytes: three cases treated successfully by surgery. Otolaryngol Head Neck Surg 1999;2013:92–6 [DOI] [PubMed] [Google Scholar]
- 16.Humphreys SC, Eck JC, Hodges SD, et al. Preliminary experience with a new surgical treatment for dysphagia due to anterior cervical osteophytes. J Surg Orthop Adv 2004;2013:106–9 [PubMed] [Google Scholar]
- 17.Saffouri MH, Ward PH. Surgical correction of dysphagia due to cervical osteophytes. Ann Otol Rhinol Laryngol 1974;2013:65–70 [DOI] [PubMed] [Google Scholar]
- 18.Yee C, Wong HY, Fewer HD, et al. Two cases of dysphagia due to cervical spine osteophytes successfully treated surgically. Can Med Assoc J 1985;2013:810–12 [PMC free article] [PubMed] [Google Scholar]


