Abstract
Spectral domain optical coherence tomography (SD-OCT) was performed in two cases of bilateral X linked foveal retinoschisis of different age groups. On fundus examination spoke wheel and honeycomb pattern of cysts were observed along with retinal nerve fibre layer (RNFL) defects. On SD-OCT, schisis was observed in the outer plexiform layer. External limiting membrane disruption was observed in the subfoveal area, along with disruption of outer nuclear layer (ONL) and inner–outer segment junction. Elevation of ONL due to tractional pull of central palisade was a novel observation. Retinoschisis extended beyond the optic disc up to the nasal region. Extracted RNFL tomogram presented an unprecedented visualisation of schisis along 360° of the optic disc. Tractional elevation in the foveal area and schisis involving nasal region, not observed upon clinical examination, was highlighted on SD-OCT. This investigative modality is an important adjunct in the assessment of foveal retinoschisis.
Background
Two cases of bilateral X linked foveal retinoschisis of different age groups were examined. On fundus examination spoke-wheel and honeycomb pattern of cysts were observed along with retinal nerve fibre layer (RNFL) defects. On Spectral domain optical coherence tomography (SD-OCT), schisis was observed in the outer plexiform layer. External limiting membrane disruption was observed in the subfoveal area, a novel finding, along with disruption of outer nuclear layer (ONL) and inner–outer segment junction. Elevation of ONL due to tractional pull of central palisade was observed. Retinoschisis extended beyond the optic disc up to the nasal region.
Extracted RNFL tomogram presented an unprecedented visualisation of schisis along 360° of the optic disc. Tractional elevation in the foveal area and schisis involving nasal region, not observed upon clinical examination, was highlighted on SD-OCT. X linked foveal retinoschisis is an inherited ocular disorder that occurs in males and has an incidence of about 1:5000 to 1:25000.1–3 Macular changes are present in almost all cases.4 RS1 gene that causes X linked foveal retinoschisis is a 24 kD protein expressed exclusively in retina and pineal gland.5 Retinoschisis is highly penetrant6 and up to 95% of affected males show some degree of foveal schisis. Variable expressivity of the same genetic disease has been seen within family members.7
The disease is characterised by degeneration of vitreous and splitting of retina at nerve fibre layer. Schisis is bilateral but may be asymmetric.7 Intraretinal cysts form in macula and impair visual acuity. Two-thirds of the males show classical macular linear cystic cavities which involve inner retina and additional layers.8 These cavities extend from fovea in a spoke wheel pattern for 1–1.5 disc diameter.
On wide field SD-OCT, the foveomacular schisis was seen most frequently in the inner nuclear layer (INL). Carriers were schisis-free.9
Both the cases were seen at the retina clinic of the Department of Ophthalmology, King George's Medical University, Lucknow, India.
Case presentation
Case report 1
A 24-year-old man presented with gradual progressive diminution of vision in both the eyes for the past 2 years. The best-corrected visual acuity (BCVA) was 20/120 in the right eye and 20/200 in the left eye with no change on manifest refraction or on pinhole testing. There was no systemic abnormality detected. Anterior segment examination was unremarkable. Stereoscopic slit-lamp examination of fundus revealed classical spoke-wheel pattern in macular area in the right eye. The left eye had a honeycomb pattern in macular area (figure 1A). Wedge-shaped defects were also noted in the nerve fibre layer in both the eyes.
Figure 1.
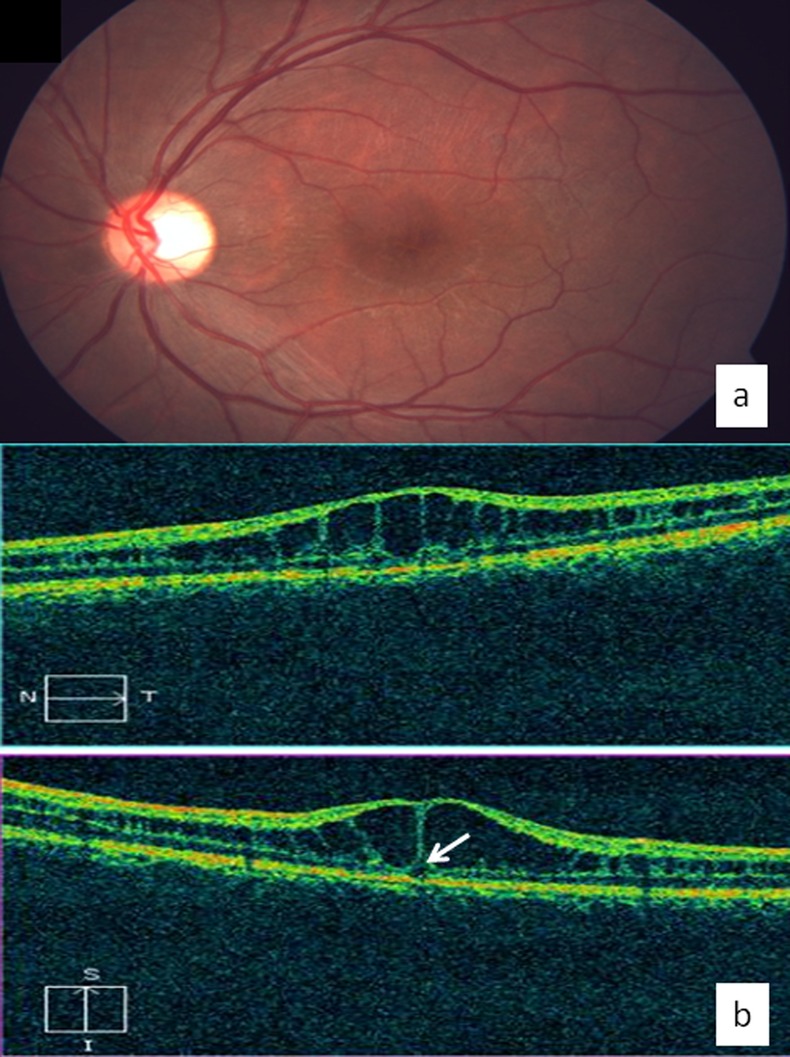
(a) Colour fundus photograph of the left eye of case 1 shows honeycomb pattern of cysts in macular area. Wedge-shaped defect were also seen in the nerve fibre layer. (b) Spectral domain optical coherence tomography shows splitting of the retina at the level of outer plexiform layer in the foveal region. A large hyporeflective cavity bridged by oblique and linear moderately reflective palisades is seen. It also shows tractional pull on outer nuclear layer by central connecting palisade (arrow). Schisis cavities are clearly demonstrated in foveal area.
In the right eye, SD-OCT showed splitting of the retina at the level of outer plexiform layer (OPL) in the foveal region. It demonstrated a large hyporeflective cavity bridged by oblique and linear moderately reflective palisades. Cysts formed intercommunications in centre of fovea. ONL and inner segment–outer segment (IS–OS) junction disruption was observed. However, external limiting membrane (ELM) disruption was observed for the first time in the subfoveal area.
The left eye showed similar splitting in foveal area, however, schisis cyst was larger and foveal elevation was pronounced. Elevation of ONL due to tractional pull of central palisade was observed for the first time. The inner nuclear and ganglion cell layer were compressed in both the eyes (figure 1B). Similar findings were observed on three-dimensional (3-D) imaging in the x, y and z axes. On internal limiting membrane-retinal pigment epithelium (ILM-RPE) and ILM maps elevation in the foveal area was noted.
Case report 2
A 14-year-old boy presented with progressive painless diminution of vision. Both eyes were examined. Visual acuity was 20/200 in the right eye and 20/30 in the left eye, not improving further on refraction. Anterior segment examination was unremarkable. On fundus examination there was honeycomb appearance of cysts on macula in either eye. Wedge-shaped nerve fibre layer defects were also noted.
On SD-OCT, in the right eye two large central cystic spaces were observed in OPL of the foveal region. Three small cystic spaces were also noted in inner nuclear layer. ONL, ELM and IS-OS junction disruption was observed in the subfoveal area (figure 2B). The left eye was observed to have smaller central cysts. Two parafoveal cysts in INL could be appreciated. Schisis extended up to optic disc and was also observed in nasal region in both the eyes (figure 3A). Extracted retinal nerve fibre layer tomogram presented an unprecedented visualisation of schisis along 360° of the optic disc (figure 3B). On 3-D imaging, schisis was well demonstrated in both the eyes. However, foveal elevation, seen as tenting of retina on 3-D sections was observed in the right eye (figure 4).
Figure 2.
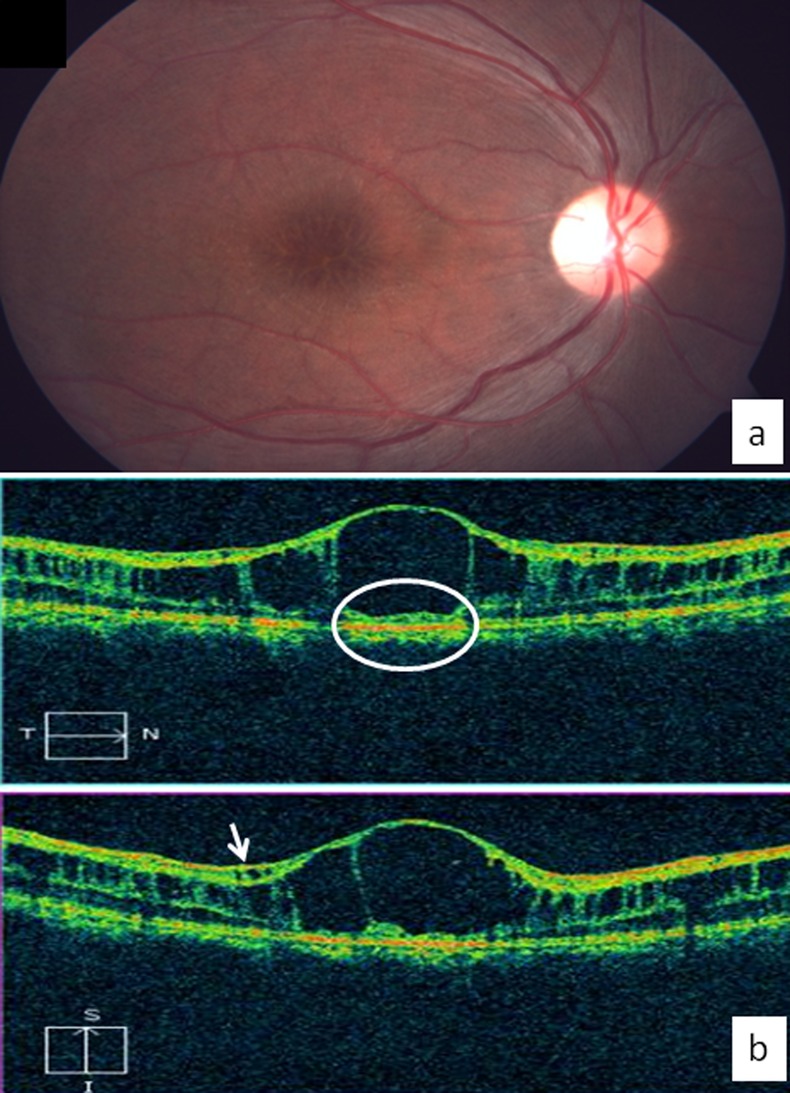
(a) Colour fundus photograph of the right eye of case 2 shows honeycomb pattern of cysts in macular area. (b) Spectral domain optical coherence tomography shows two large central cysts with intervening connecting palisade in outer plexiform layer in the foveal region. Three small cysts are observed in inner nuclear layer (arrow). Disruption of outer nuclear layer, external limiting membrane and inner segment-outer segment junction is also demonstrated (oval area).
Figure 3.
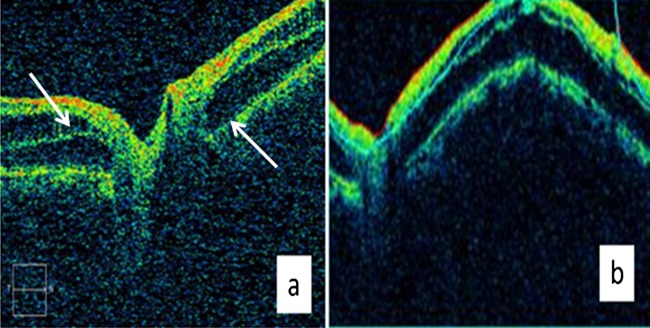
(A) Advanced visualisation of optic disc cube on SD-OCT shows retinoschisis extending up to the optic disc and involving nasal side of the optic disc as well (shown by arrows). (B) Extracted retinal nerve fibre layer tomogram of the optic disc cube shows retinoschisis involving 360° of the optic disc.
Figure 4.
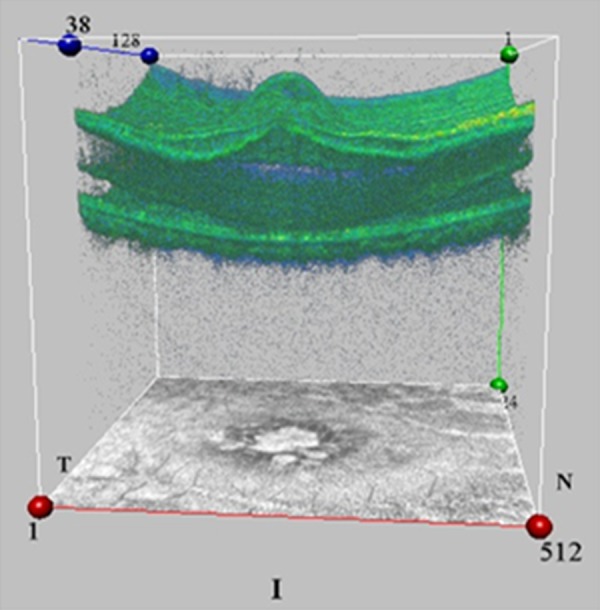
Three-dimensional spectral domain optical coherence tomography image of the right eye of case 2 shows tractional elevation of inner layers of retina leading to tenting in that region. Schisis in inner nuclear layer and connecting palisades between schitic cavities are also well discerned.
Investigations
Fundus photography and spectral domain optical coherence tomography.
Discussion
In vivo characterisation of retinal structures in X linked foveal retinoschisis using SD-OCT has been reported. Novel findings were observed on horizontal and vertical scans and 3-D imaging in our cases. The patients, aged 14 and 24 years, showed no difference in the pattern and extent of disease. However, presentation in the two eyes of the same patient varied significantly. An earlier report had correlated retinal layer abnormalities with age.10 In vivo morphological studies, using time-domain and Fourier-domain OCT, demonstrated schisis cysts occurring in a number of different layers of the neurosensory retina (RNFL, INL and ONL/OPL) and disruption of IS-OS junction and ONL.11 In our study, we not only noted disruption of ONL and IS-OS junction but also of the ELM. The ELM and IS-OS junction disruption explains the visual loss. SD-OCT helped us in detecting retinal schisis extending up to the optic disc area and beyond. Retinoschis in nasal region and foveal elevation was not observed upon clinical examination and was highlighted on 3-D SD-OCT imaging. It also exquisitely demonstrated foveal elevation.
Optical coherence tomography should be considered as an investigative procedure in children with hyperopic amblyopia to rule out early stages of X linked foveal retinoschisis.12 SD-OCT has also been used as a follow-up tool and prognostic indicator in myopic retinoschisis.13 SD-OCT is an important adjunct in assessment of foveoschisis.
Learning points.
Spectral domain optical coherence tomography (SD-OCT) should be considered in children with hyperopic amblyopia to rule out early stages of X linked foveal retinoschisis.
Traction on retinal layers and schisis not observed on slit lamp biomicroscopic examination is well discerned on SD-OCT.
SD-OCT is helpful in detecting retinal schisis extending up to the optic disc area and beyond.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Mooy CM, Van Den Born LI, Baarsma S, et al. Hereditary X-linked juvenile retinoschisis: a review of the role of Müller cells. Arch Ophthalmol 2002;2013:979–84 [PubMed] [Google Scholar]
- 2.Hiriyanna K, Singh-Parikshak R, Bingham EL, et al. Searching for genotype-phenotype correlations in X-linked juvenile retinoschisis. In: Anderson RE, La Vail MM, Hollyfield JG, eds. New insights into retinal degenerative diseases. New York: Plenum Publishers, 2001:45–53 [Google Scholar]
- 3.Wang T, Waters CT, Rothman AM, et al. Intracellular retention of mutant retinoschisin is the pathological mechanism underlaying X-linked retinoschisis. Hum Mol Genet 2002;2013:3097–105 [DOI] [PubMed] [Google Scholar]
- 4.Tantri A, Vrabec TR, Cu-Unjieng A, et al. X-linked retinoschisis: a clinical and molecular genetic review. Surv Ophthalmol 2004;2013:214–30 [DOI] [PubMed] [Google Scholar]
- 5.Sauer CG, Gehrig A, Warneke-Wittstock R, et al. Positional cloning of the gene associated with X-linked juvenile retinoschisis. Nat Genet 1997;2013:164–70 [DOI] [PubMed] [Google Scholar]
- 6.Forsius H, Krause U, Helve J, et al. Visual acuity in 183 cases of X-chromosomal retinoschisis. Can J Ophthalmol 1973;2013:385–93 [PubMed] [Google Scholar]
- 7.Leng T. Two cases of X-linked retinoschisis with different spectral domain optical coherence tomography findings. Clin Ophthalmol 2012;2013:1563–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yanoff M, Kertesz RE, Zimmerman LE. Histopathology of juvenile retinoschisis . Arch Ophthalmol 1968;2013:49–53 [DOI] [PubMed] [Google Scholar]
- 9.Gregori NZ, Lam BL, Gregori G, et al. Wide-field spectral-domain optical coherence tomography in patients and carriers of X-linked retinoschisis. Ophthalmology 2013;2013:169–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gerth C, Zawadzki RJ, Werner JS, et al. Retinal morphological changes of patients with X-linked retinoschisis evaluated by Fourier-domain optical coherence tomography. Arch Ophthalmol 2008;2013:807–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yu J, Ni Y, Keane PA, et al. Foveomacular schisis in juvenile X-linked retinoschisis: an optical coherence tomography study. Am J Ophthalmol 2010;2013:973–8 [DOI] [PubMed] [Google Scholar]
- 12.Kyung SE, Lee M. Foveal retinoschisis misdiagnosed as bilateral amblyopia. Int Ophthalmol 2012;2013:595–8 [DOI] [PubMed] [Google Scholar]
- 13.Wang S, Peng Q, Zhao P. SD-OCT use in myopic retinoschisis pre- and post-vitrectomy. Optom Vis Sci 2012;2013:678–83 [DOI] [PubMed] [Google Scholar]


