Abstract
Background
Magnetic resonance enterography (MRE) is increasingly used in children due to growing concerns of radiation.
Objective
To determine the performance of MRE, imaging findings were compared to wireless capsule endoscopy (WCE) and histology results in children with/or suspected inflammatory bowel disease (IBD).
Materials and methods
Pathology and WCE reports were retrospectively reviewed in 23 patients who had MRE.
Results
The sensitivity of MRE was 75.0% while the sensitivity of WCE was 77.8%.
Conclusion
MRE and WCE are complementary techniques in evaluation of the small bowel in IBD.
Keywords: Magnetic Resonance Enterography (MRE), Wireless Capsule Endoscopy (WCE), Inflammatory bowel disease (IBD), Crohn disease, Terminal Ileum (TI)
Introduction
Crohn disease is relatively common in the pediatric population, with up to 20–30% of affected individuals presenting during either childhood or adolescence (1). Its incidence in children appears to be increasing, having doubled during a recent 10-year period, and it may present in children younger than 3 years of age (1). Crohn disease is a syndrome diagnosis based on the clinical presentation and findings at endoscopy, histology, and small bowel radiology (2). While the imaging assessment of pediatric Crohn disease was limited primarily to endoluminal barium studies (such as small bowel follow-through, small bowel enteroclysis and contrast enema) in the past (1), recently WCE, MRE, and computed tomography enterography (CTE) have been increasingly used (2, 3).
This change in practice pattern, however, is based on limited medical evidence, as there are very few studies comparing MRE findings to histopathology specimens in children with Crohn disease (1). Moreover there is only one study (4) comparing the diagnostic value of WCE with MRE in children with suspected or already established Crohn disease. The place that these new procedures will occupy in the diagnostic algorithm of suspected Crohn disease remains to be fully determined. Therefore, the aim of this retrospective study is to evaluate the efficacy of MRE and WCE in children using histopathology as the reference standard in diagnosing Crohn disease.
Materials and methods
This retrospective study was approved by the institutional review board. Endoscopy/histology (E/H) reports and WCE reports of 23 patients who underwent MRE from January 2008 to June 2010 for the evaluation of inflammatory bowel disease (IBD) were retrospectively reviewed. The mean age (± standard deviation) of the patients was 15 years ± 3.3 years (range 8–21 years). Of the 23 patients, 20 had E/H reports and 11 had WCE reports available.
MRE was performed using a 1.5-T magnet (Signa HDxt, GE Medical Systems, Milwaukee, Wisconsin) and a surface phased-array coil. Forty-five minutes prior to imaging, VoLumen 15 mg/kg PO was administered. Glucagon 0.5mg IV was given immediately preceding intravenous contrast administration to inhibit peristalsis. Intravenous contrast consisted of 0.1 mmol/kg gadopentetate dimeglumine (Magnevist, Bayer Healthcare Pharmaceuticals, Germany). Axial and coronal T2 steady state (FIESTA; TR/TE 3.4–3.8/1.5–1.7; flip angle 75; slice thickness 4.0–4.2mm; matrix 192–160 × 320–224), cine FIESTA, axial and coronal single-shot fast spin-echo (SSFSE; TR/TE 476–825/86–102; flip angle 90; slice thickness 4.0; matrix 512 × 192), post-contrast axial and pre- and post-contrast ultrafast spoiled gradient-echo (LAVA; TR/TE 3.5–3.6/1.6–1.8; TI 7; flip angle 12–15; slice thickness 4.8; matrix 288–192 × 192–288) sequences were obtained. No patients required sedation for the examination. The MRE images were retrospectively reviewed by two board-certified pediatric radiologists using consensus reading without knowledge of the E/H and WCE findings. MR findings were scored according to the scoring system outlined in Table 1. Each of the scores was added up and positive /negative variables were assigned using a cutoff score of ≥ 3 as positive. Pathology reports from upper and lower endoscopic biopsies of the 20 patients who had MRE were retrospectively reviewed. The mean interval time between imaging and E/H was 3.6 months. E/H results from the pathology reports were scored according to a scoring index previously reported (4) (Table II). Each of the scores were summed and converted to positive/negative variables using a cutoff score of ≥ 1 as positive for all patients. WCE was performed in 11 patients with the PillCam SB videocapsule (Given Imaging, Israel) as described previously (5, 6). The WCE images were independently interpreted by two pediatric gastroenterologists according to the parameters and weightings for the capsule endoscopy scoring index described by Gralnek et al (7) which is based on three main capsule endoscopic variables; villous appearance, ulcers and stenosis. A score <135 was designated normal or clinically insignificant mucosal inflammatory change, a score between 135 and 790 was mild, and a score ≥790 was moderate to severe. These results were coded as 0 for normal, 1 for a score between 135–790 and 2 for a score >790(Table III). Scores were converted to positive/negative variables using a cutoff score of ≥ 1 as positive for all patients.
Table I.
MRI scoring index
| Wall thickening | 0–3 mm | 0 |
| 3–6 mm | 1 | |
| >6 mm | 2 | |
| Enhancement | No | 0 |
| Mild | 1 | |
| Severe | 2 | |
| Lymph nodes | No | 0 |
| Yes | 1 | |
| Vascular congestion | No | 0 |
| Yes | 1 | |
| Mesenteric fatty infiltration | No | 0 |
| Yes | 1 | |
| Stricture | No | 0 |
| Yes | 1 | |
| Abscess | No | 0 |
| Yes | 1 | |
| Fistula | No | 0 |
| Yes | 1 | |
| # of segments involved (duodenum, jejunum, ileum, ascending, transverse, and descending, sigmoid, rectum) | 0–8 | |
Table II.
Scoring system for histological assessment.
| Epithelial damage | Normal | 0 |
| Focal pathology | 1 | |
| Extensive pathology | 2 | |
| Architectural changes | Normal | 0 |
| Moderately disturbed (<50%) | 1 | |
| Severely disturbed (>50%) | 2 | |
| Lamina propria mononuclear cells | Normal | 0 |
| Moderate increase | 1 | |
| Severe increase | 2 | |
| Lamina propria PMNs | Normal | 1 |
| Moderate increase | 2 | |
| Severe increase | 3 | |
| Intraepithelial PMNs | In surface epithelium | 0 |
| Cryptitis | 1 | |
| Crypt abscess | 2 | |
| Erosions/ulcers | No | 0 |
| Yes | 1 | |
| Granulomas | No | 0 |
| Yes | 1 | |
| Number of biopsy specimens affected | None | 0 |
| ≤ 33% | 1 | |
| 33–66% | 2 | |
| >66% | 3 | |
Table III.
Scoring system for WCE results
| WCE score <135 | 0 |
| WCE score between 135–790 | 1 |
| WCE score .790 | 2 |
Terminal ileum subgroup
A subgroup of 12 out of 20 patients (8 females, 4 males) with a mean age of 15.6 years (range 10–21 years) had pathology slides available for review. The pathology slides of these patients were re-evaluated and scored by an abdominal pathologist with regard to the terminal ileum only. 7 of the 12 patients also had WCE results available which were scored according to the parameters and weightings for the capsule endoscopy scoring index described by Gralnek et al (7). Histology scores (dichotomized as 1–6 vs. 8–10) of the terminal ileum were compared with MRE (dichotomized as <3 versus≥3) and WCE scores (dichotomized as (<2 versus ≥ 2).
Statistical analysis
The sensitivity and specificity of MR score (dichotomized as <3 vs. ≥3) and WCE (dichotomized as 0 vs. ≥ 1) for the detection of IBD in all patients were calculated using pathology score as the gold standard (dichotomized as 0 vs. ≥ 1).
For the terminal ileum subgroup sensitivity and specificity of MR score (dichotomized as <3 vs. ≥3) and WCE (dichotomized as <2 vs. ≥ 2) were calculated using pathology score as the gold standard (dichotomized as 1–6 vs. 8–10). The Pearson correlation coefficient (r) or Spearman-rank correlation coefficient was used, as appropriate, to assess the degree of agreement between 1) MRE score and pathology score and 2) WCE score and pathology score. ROC analysis was further utilized to assess the predictive accuracy (area under the curve [AUC]) of MR score in relation to binary pathology score, for a subset of patients with scored terminal ileum findings. All p-values are two-sided with statistical significance evaluated at the 0.05 alpha level. All analyses were performed in SPSS Version 19.0 (SPSS Inc., Chicago, IL).
Results
MRE, E/H and WCE scores of all 20 patients are summarized in Table IV. Preliminary data demonstrated a high sensitivity (75.0% [95% CI = 47.6%, 92.7%]) of MRE for the detection of Crohn disease using histology as gold standard (Table V). The sensitivity of WCE using histology as gold standard was similar (77.8% [95% CI = 40.0%, 97.2%]) (Table VI).
Table IV.
MRE, E/H and WCE scores of all 20 patients. MRE scores were converted to positive /negative variables using a cutoff score of ≥ 3 as positive. E/H and WCE scores were converted to positive/ negative variables using a cutoff score of ≥ 1 as positive for all patients.
| Patient | MRE score (+/−) | E/H score (+/−) | WCE score (+/−) |
| 1 | 6 (+) | 6 (+) | 2 (+) |
| 2 | 6 (+) | 5 (+) | 1 (+) |
| 3 | 7 (+) | 4 (+) | 1 (+) |
| 4 | 5 (+) | 6 (+) | 2 (+) |
| 5 | 9 (+) | 0 (−) | 2 (+) |
| 6 | 5 (+) | 0 (−) | none |
| 7 | 1 (−) | 1 (+) | none |
| 8 | 0 (−) | 0 (−) | 1 (+) |
| 9 | 9 (+) | 9 (+) | 2 (+) |
| 10 | 11 (+) | 6 (+) | none |
| 11 | 2 (−) | 9 (+) | 0 (−) |
| 12 | 7 (+) | 0 (−) | 2 (+) |
| 13 | 8 (+) | 5 (+) | none |
| 14 | 4 (+) | 6 (+) | none |
| 15 | 6 (+) | 3 (+) | 0 (−) |
| 16 | 0 (−) | 0 (−) | none |
| 17 | 0 (−) | 0 (−) | none |
| 18 | 1 (−) | 4 (+) | 2 (+) |
| 19 | 4 (+) | 2 (+) | none |
| 20 | 7 (+) | 4 (+) | none |
Table V.
MR score and histology cross tabulation. Sensitivity of MRE = 12/16 = 75.0%. Specificity of MRE = 2/4 = 50.0%.
| Patdology | ||||
| Positive | Negative | Total | ||
| MR Score | Positive | 12 | 2 | 14 |
| Negative | 4 | 2 | 6 | |
| Total | 16 | 4 | 20 | |
Table VI.
WCE and histology cross tabulation. Sensitivity of WCE = 7/9 = 77.8%. Specificity of WCE = 0/2 = 0.0%.
| Patdology | ||||
| Positive | Negative | Total | ||
| Capsule | Positive | 7 | 2 | 9 |
| Negative | 2 | 0 | 2 | |
| Total | 9 | 2 | 11 | |
The most common findings detected on MRE were the presence of lymph nodes (75%), bowel wall thickening (70%) and enhancement (70%). Terminal ileum was involved in 16 out of 20 patients (Fig.1 and 2). Overall small bowel distension was satisfactory and only one patient had suboptimal distension of the proximal small bowel. Three patients with positive MRE findings had negative E/H which was due to inability to reach the terminal ileum during colonoscopy and/or inadequate sampling of the terminal ileum. In three other patients with negative MRE findings, the E/H reports were consistent with more superficial mucosal edema/erythema involving the colonic segments which were not detected by MRE. Of the three patients with negative MRE and positive E/H, only two had WCE done. One of these was positive, the other one did not comment on the colonic findings but had normal small bowel.
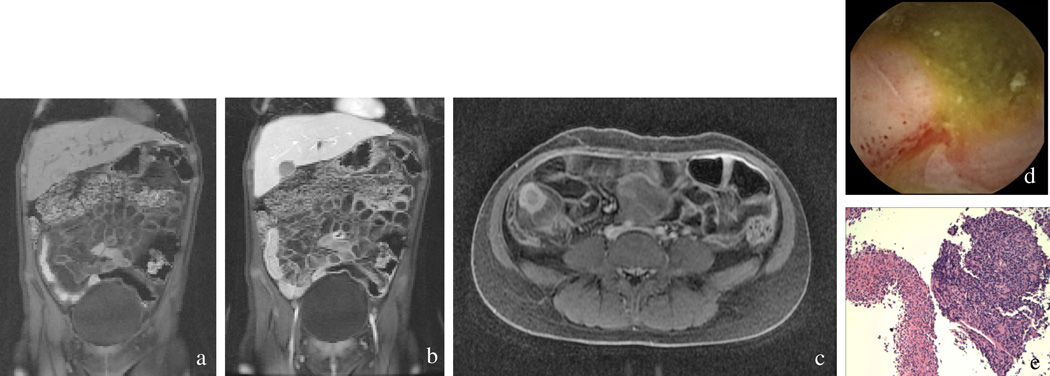
Figure 1.
Pre (a) and post-contrast (b) coronal LAVA images demonstrate mucosal enhancement, wall thickening, and vascular dilatation and tortuosity of the vasa recta (comb sign). Axial LAVA image (c) demonstrates wall thickening and striated mucosal enhancement. Capsule endoscopy (d) shows an edematous, ulcerated small bowel with loss of normal villi. The terminal ileum is erythematous with erosions, edema, hemorrhage, and purulent exudate. Histopathology at 40 × magnification (e) shows a friable, edematous ulcer of the terminal ileum with purulent exudate and granulomatous change.
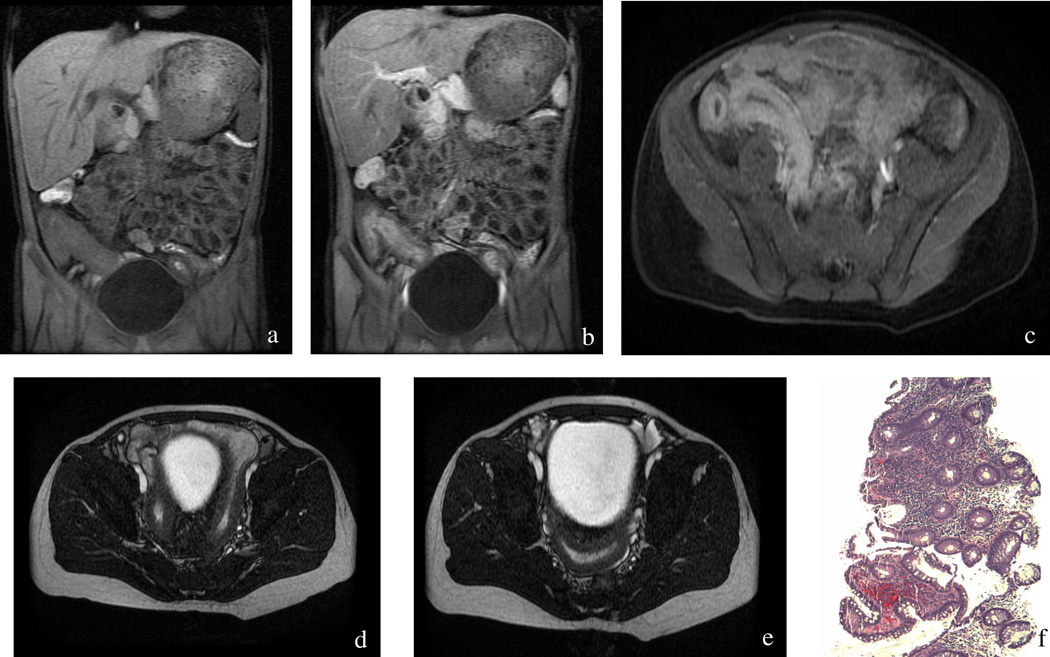
Figure 2.
Pre (a) and post-contrast (b) coronal LAVA images demonstrate mucosal enhancement and wall thickening of the cecum and terminal ileum. Axial post contrast LAVA image (c) demonstrates thickening of the cecum and terminal ileum with striated enhancement. Axial noncontrast FIESTA images (d, e) show terminal ileal wall thickening with luminal narrowing and proximal dilatation. Histopathology at 40× (f) shows active ileitis with friable mucosa, cobblestoning, and hemorrhage.
When MRE and WCE results were compared in all patients, there were 3 mismatches. The two patients with positive WCE and negative MRE had very superficial ulcers. One patient with predominant finding of bowel wall thickening had positive MRE and negative WCE.
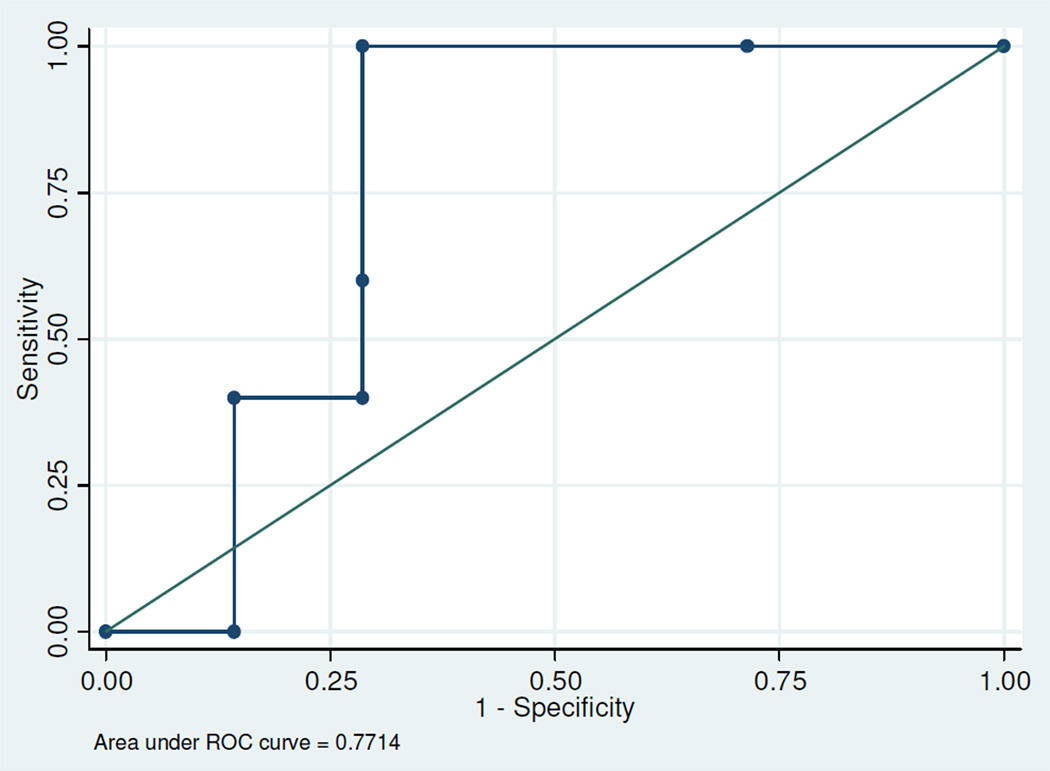
Table VII summarizes the MRE, WCE and E/H results of the terminal ileum findings in 12 patients whose pathology slides were available for re-evaluation. A statistically significant correlation was found between MRE and E/H scores (Pearson correlation coefficient = 0.71, P=0.01) of the terminal ileal findings in 12 patients. Among this subset of 12 patients, a ROC analysis was performed for MRE score and E/H score (dichotomized as 1–6 vs. 8–10), with area under the curve = 77.1% (i.e., predictive accuracy of MR score in relation to binary pathology score; P=0.12) (Fig. 3).The correlations between WCE and E/H scores (Spearman-rank correlation coefficient = 0.52, P=0.23) and the correlations between WCE and MRE scores (Spearman-rank correlation coefficient = 0.54, P=0.22) were fairly good. Although not statistically significant, the correlations are still considered fair to moderate. The lack of significance is likely due to the small sample size available for analysis, with only 7 patients contributing to usable WCE scores. Sensitivity and specificity of MRE score (dichotomized as ≥3 versus <3), based on E/H score (gold standard; dichotomized as 1–6 versus 8–10), were calculated as 100% and 71.4%, respectively, while the sensitivity and specificity for WCE score based on E/H score were 50% and 60% respectively for this subset of patients with a specific focus on the terminal ileum.
Table VII.
MRE, E/H and WCE scores based on terminal ileum findings in 12 patients whose pathology slides were available.
| Patient | MRE score | E/H score | WCE score |
|---|---|---|---|
| 2 | 3 | 8 | none |
| 3 | 5 | 6 | 0 |
| 4 | 4 | 9 | 1 |
| 5 | 7 | 6 | 2 |
| 7 | 1 | 1 | none |
| 8 | 0 | 1 | 0 |
| 9 | 6 | 10 | 2 |
| 11 | 1 | 1 | 0 |
| 13 | 6 | 9 | none |
| 14 | 3 | 8 | none |
| 16 | 0 | 6 | none |
| 18 | 1 | 1 | 2 |
Figure 3.
ROC Analysis for MR Score and E/H score (E/H score was dichotomized as 1–6 vs. 8–10) in the terminal ileum subgroup.
Discussion
The purpose of this study was to assess the efficacy of MRE and WCE in evaluating pediatric patients with Crohn disease. The results of this study indicate an overall sensitivity of 75.0% for MRE and 77.8% for WCE for detecting Crohn disease using histology as gold standard. Prior studies in adult populations have reported no statistically significant difference in the sensitivity between MRE and WCE for detecting Crohn disease in adult populations, with a slight preference for WCE (7, 8, 9). While our results are similar to previous comparative studies of WCE and MRE in adult populations, they are slightly low compared to the only comparative pediatric study in the literature (4). This discrepancy may be explained by the fact that frank disease is often easier to diagnose than mild disease or remission. The higher sensitivities of MRE and WCE in Casciani et al’s study may be the result of imaging only symptomatic patients which makes parameters indicative of disease more pronounced. Furthermore, the awareness of the clinical and laboratory values when evaluating the imaging studies also improves accuracy.
While the overall sensitivity of MRE was 75%, the sensitivity increased to 100% when only the terminal ileum was assessed. For WCE, the sensitivity in the terminal ileum subgroup was 50%. However, the WCE analysis was based on only 7 patients with WCE scores, so this analysis is not accurate given the very small sample size. Furthermore, the predominant finding of transmural inflammation in the terminal ileum rather than mucosal inflammation in the subgroup of 12 patients may account for the lower sensitivity of WCE when compared to MRE. Superficial mucosal pathology may have disappeared with treatment but mural and extramural changes might not have responded to treatment yet.
The correlations between WCE and MRE scores although not statistically significant, were fair to moderate. The lack of significance is likely due to the small number of patients with available WCE scores. The majority of discrepancies resulted from the higher incidence of superficial mucosal lesions in the proximal small bowel and the tendency of WCE to identify more superficial mucosal lesions. Golder et al have also reported the superiority of WCE in diagnosing lesions in the proximal small bowel compared to MRE which may contribute to the fair to moderate correlation in our study between WCE and MRE.
Recording of WCE was incomplete in one patient in which the capsule did not reach the cecum in eight hours excluding terminal ileum. Incomplete recording is reported in the literature to range between 15% and 27% (8).
This study has limitations. No gold standard can be offered for the correlation of every single lesion identified with either modality due to known sampling errors associated with endoscopic biopsies (1). Furthermore, only 11 patients had WCE making it impossible to compare MRE and WCE with the gold standard in all patients. Our patient population was small but this study should be viewed as a preliminary study comparing MRE and WCE in pediatric patients with or suspected Crohn disease. The high diagnostic yield of WCE in superficial mucosal lesions and MRE in transmural or extramural pathology makes them complementary modalities in the evaluation of pediatric Crohn patients.
Supplementary Material
Acknowledgements
Dr. Paul Christos was partially supported by the following grant: Clinical Translational Science Center (CTSC) (UL1-RR024996).
References
- 1.Dillman JR, Ladino-Torres MF, Adler J, DeMatos-Malliard V, McHugh JB, Khalatbari S, Strouse PJ. Comparison of MR enterography and histopathology in the evaluation of pediatric Crohn disease. Pediatric Radiology. 2011;41(12):1552–1558. doi: 10.1007/s00247-011-2186-0. [DOI] [PubMed] [Google Scholar]
- 2.Jensen MD, Nathan T, Rafaelsen SR, Kjeldsen J. Diagnostic accuracy of capsule endoscopy for small bowel Crohn disease is superior to that of MR enterography or CT enterography. Clinical Gastroenterology and Hepatology. 2011;9(2):124–129. doi: 10.1016/j.cgh.2010.10.019. [DOI] [PubMed] [Google Scholar]
- 3.Gee MS, Nimkin K, Hsu M, Israel EJ, Biller JA, Katz AJ, Mino-Kenudson M, Harisinghani MG. Prospective evaluation of MR enterography as the primary imaging modality for pediatric Crohn disease assessment. American Journal of Roentgenology. 2011;197:224–231. doi: 10.2214/AJR.10.5970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Casciani E, Masselli G, Di Nardo G, Polettini E, Bertini L, Oliva S, Floriani I, Cucchiara S, Gualdi G. MR enterography versus capsule endoscopy in paediatric patients with suspected Crohn disease. European Radiology. 2011;21(4):823–831. doi: 10.1007/s00330-010-1976-3. [DOI] [PubMed] [Google Scholar]
- 5.Shamir R, Eliakim R. Capsule endoscopy in pediatric patients. World Journal of Gastroenterology. 2008;14(26):4152–4155. doi: 10.3748/wjg.14.4152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Iddan G, Meron G, Blukhovsky A, Swan P. Wireless capsule endoscopy. Nature. 2000:405–417. doi: 10.1038/35013140. [DOI] [PubMed] [Google Scholar]
- 7.Gralnek IM, Defranchis R, Seidman E, Leighton JA, Legnani P, Lewis BS. Development of a capsule endoscopy scoring index for small bowel mucosal inflammatory change. Alimentary Pharmacology & Therapeutics. 2008;27(2):146–154. doi: 10.1111/j.1365-2036.2007.03556.x. [DOI] [PubMed] [Google Scholar]
- 8.Tillack C, Seiderer J, Brand S, Göke B, Reiser MF, Schaefer C, Diepolder H, Ochsenkühn T, Herrmann KA. Correlation of magnetic resonance enteroclysis (MRE) and wireless capsule endoscopy (CE) in the diagnosis of small bowel lesions in Crohn disease. Inflammatory bowel diseases. 2008;14(9):1219–1228. doi: 10.1002/ibd.20466. [DOI] [PubMed] [Google Scholar]
- 9.Albert JG, Martiny F, Krummenerl A, Stock K, Lesske J, Göbel CM, Lotterer E, Nietsch HH, Behrmann C, Fleig WE. Diagnosis of small bowel Crohn disease: a prospective comparison of capsule endoscopy with magnetic resonance imaging and fluoroscopic enteroclysis. Gut. 2005;54(12):1721–1727. doi: 10.1136/gut.2005.069427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gölder SK, Schreyer AG, Endlicher E, Feuerbach S, Schölmerich J, Kullmann F, Seitz J, Rogler G, Herfarth H. Comparison of capsule endoscopy and magnetic resonance (MR) enteroclysis in suspected small bowel disease. International Journal of Colorectal Disease. 2006;21(2):97–104. doi: 10.1007/s00384-005-0755-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.