Abstract
NADPH oxidase (NOX) was originally identified in immune cells as playing an important microbicidal role. In stroke and cerebrovascular disease, inflammation is increasingly being recognized as contributing negatively to neurological outcome, with NOX as an important source of superoxide. Several labs have now shown that blocking or deleting NOX in the experimental stroke models protects from brain ischemic. Recent work has implicated glucose as an important NOX substrate leading to reperfusion injury, and that NOX inhibition can improve the detrimental effects of hyperglycemia on stroke. NOX inhibition also appears to ameliorate complications of thrombolytic therapy by reducing blood brain barrier disruption, edema formation and hemorrhage. Further, NOX from circulating inflammatory cells seems to contribute more to ischemic injury more than NOX generated from endogenous brain residential cells. Several pharmacological inhibitors of NOX are now available. Thus, blocking NOX activation may prove to be a promising treatment for stroke as well as an adjunctive agent to prevent its secondary complications.
Keywords: ischemia, inflammation, neuroprotection, superoxide, NADPH oxidase
I. Introduction
The major therapeutic strategy for treatment of acute ischemic stroke is rapid recanalization, either by pharmacological means through thrombolytic agents, or mechanical thrombectomy 1, 2. However, the time window for intervention limits these therapies to a small number of patients, and their inappropriate use can actually worsen outcome. This worsened outcome has been blamed on complications of delayed recanalization such as worsened brain edema or symptomatic brain hemorrhage, a phenomenon commonly referred to as ‘reperfusion injury’ 3, 4. Thus, therapies to minimize reperfusion injury might expand populations of stroke patients eligible for treatment. Reactive species, radicals derived from oxygen or nitric oxide are thought to be major contributors to this damage. Upon reperfusion, the brain is quickly exposed to oxygenated blood, and injured mitochondria of the ischemic brain are rendered incapable of detoxifying free radicals 5. Further, immune cells which infiltrate ischemic tissue or plug ischemic microvasculature can also generate reactive species through several enzyme systems 6. Recent studies have focused on the role of superoxide generating systems in immune cells and their consequences on reperfusion injury. One enzyme system is nicotinamide adenine dinucleotide phosphate (NADPH) oxidase, or NOX, originally found on leukocytes, but now recognized in several types of cells in the brain. Inhibition of NOX can potentially reduce the amount of superoxide generated during reperfusion, and thus limit reperfusion injury. Such a strategy has the potential to not only treat acute ischemic stroke, but also reduce complications of recanalizing strategies by using it in combination with thrombolytics or mechanical thrombectomy devices.
NOX, classically viewed as a purely peripheral phagocytic enzyme involved in the killing of bacteria, fungi and microbes, is now recognized as a major contributor of this ROS in the vast majority of CNS diseases. The superoxide produced by activation of the NADPH oxidase enzyme is soluble in solution and can combine with other ROS to form more toxic reagents in vivo. The importance of NOX in the production of ROS and subsequent neuronal cell death cannot be overstated. Several other enzymes found throughout the cell are involved in ROS generation including, xanthine oxidase, lipoxygenase, cylcooxygenases and substrate coupled nitric oxide synthetase but none of these can produce the large amount of ROS observed in non-phagocytic cells in both normal and pathological conditions 7. In the last 10 years, the research into the NOX enzyme has led to a better understanding of its role in stroke and related diseases, and the development of inhibitors has opened up the field to a potentially important therapeutic target.
I. NADPH oxidase
NOX is a membrane-bound enzyme complex with components can be found in the plasma membrane as well as in the cytoplasm. NOX was originally found in leukocytes and is a major source of reactive oxygen species generation 8. The complex is normally latent in neutrophils and is activated to assemble in the membranes during respiratory burst. NOX is a multi-component enzyme comprising a cytoplasmic subunits (p47phox, p67phox, and p40phox and Rac2) and upon phosphorylation, these subunits can form a complex and translocate to the plasma membrane to dock with the plasma membrane subunits (p91phox, p22phox) 9. The catalytic core of the enzyme is thought comprise gp91phox and p22phox 10. Catalysis of NOX occurs in the p91phox subunit (Nox2) and is initiated by transferring of electrons from molecular oxygen through redox coupling with NADPH, FAD and heme to produce superoxide anion (O2•−) 11.
Superoxide can be produced in phagosomes, which contain ingested bacteria and fungi, or it can be produced outside of the cell. In a phagosome, superoxide can spontaneously form hydrogen peroxide that will undergo further reactions to generate reactive oxygen species (ROS). Superoxide is capable of killing bacteria and fungi by mechanisms that are not yet fully understood, but may inactivate critical metabolic enzymes, initiate lipid peroxidation and liberate redox active iron.
NOX activation depends on phosphorylation, especially of the p47phox subunit 10. While other subunits can be phosphorylated, p47phox phosphorylation appears to be the key in the membrane translocation of other subunits. Kinases known to phosphorylate p47 include several of protein kinase C isoforms (β,δ and ζ) as well as p38 and p21 mitogen activated kinases (MAPK) and protein kinase B. Further, it appears that NOX can be regulated by the inflammatory transcription factor, nuclear factor kappa B (NFκB). NFκB can induce gp91phox expression, as cells deficient in NFκB’s p65 subunit express less gp91phox in response to lipopolysaccharide (LPS) stimulation 12. Vascular ROS are produced in endothelial, adventitial, and VSMCs and derived primarily from NOX, a multisubunit enzyme catalyzing a superoxide anion production by the 1 electron reduction of oxygen using NADPH as the electron donor: 2O2 + NADPH → 2O2− + NADP + H+ 13.
An important breakthrough came through in 1999 with the discovery of a gp91phox homolog in non-phagocytic cells, Nox1, which was originally named Mox-1 14. This Nox1 was first discovered in vascular smooth muscle cells. To date, 6 homologues of a gp91phox have been identified, Nox1, Nox3–5, Duox1 and Duox2 14–16. The gp91phox is now referred to as Nox2 and all the Nox homologs are the catalytic components of the enzyme involved in the electron transport function. All NOX family members share a core structure consisting of 6-transmembrane domains (including the 2 heme-binding regions) and a cytoplasmic c-terminus which contains the NADPH binding region 17.
NOX has also been detected in the brain, but knowledge of its distribution and function in normal CNS tissue has been lacking. This is partly due to the lack of tools and, in particular, the lack of good specific antibodies available for any components of this enzyme. A detailed description of the expression of all the NOX isoforms are described in a recent review by Sorce and Krause 18. mRNA for all the subcomponents of NADPH Oxidase have been observed in both neurons and microglial 19–21. An immunohistochemical study in mice using polyclonal antibodies revealed all the major components of NADPH oxidase (p22phox, Nox2, p47phox, p67phox and p40phox) predominantly in the neurons of hippocampus, cortex, amygdala, striatum, and thalamus but not in the cerebellum 22. Nox4 has also been identified in very specific neurons in the cortex, hippocampus and cerebellum of mice by both in situ hybridization and immunohistochemistry 23. More recently Nox5 has shown to be expressed in the cerebrum and Duox1 is highly expressed in the cerebellum 24. In rats, neuronal immunohistochemistry staining for Nox2 and p47phox was found predominantly in the hippocampus, cerebral cortex and cerebellum 25. This is in contrast to the study by Green et al 20 who found that in the normal rat brain Nox2 is present only on perivascular cells but can be highly expressed in activated microglial cells. These differences in expression patterns are probably due to different affinities, expression patterns and staining procedures of the antibodies as well as species differences. In addition to the neuronal and glial expression patterns of Nox, the cerebral vasculature has also been shown to express subunits of NADPH oxidase as well as many of the Nox homologs. This is important because ROS are consistently involved with certain cerebral vascular diseases such as hypertension and stoke. mRNA for Nox1, Nox2, Nox4, p22phox and p47phox have been shown to be expressed in rat basilar arteries and Nox4 is also expressed at the protein level 26, 27. In vitro studies have shown NOX expression in neurons, astrocytes, and in microglia 11. Immunohistochemistry studies have shown that NOX subunits are widely distributed in the cortex, the hippocampus, and in the cerebellum in vivo 19, 22, 25, 28.
II. NADPH oxidase involvement in cerebrovascular disease
NOX isoforms have been described in the cerebral vasculature. Thus, cerebrovascular disease may benefit from NOX as a target in the brain, but its blood vessels as well. NOX may also be an important target in the prevention of reperfusion injury, an increasingly observed complication of recanalizing strategies used to treat stroke in patients. Upon reperfusion, the brain is quickly exposed to oxygenated blood, and injured mitochondria of the ischemic brain are rendered incapable of detoxifying reactive species 5. Further, immune cells which infiltrate ischemic tissue or plug ischemic microvasculature can also generate reactive species through several enzyme systems 6. Recent studies have focused on the role of the superoxide generating NOX systems in immune cells and their consequences on reperfusion injury. NOX can potentially reduce the amount of superoxide generated during reperfusion, and thus limit such injury. This strategy has the potential to not only treat acute ischemic stroke, but also reduce complications of recanalizing strategies by using it in combination with thrombolytics or mechanical thrombectomy devices.
There is increasing evidence that inflammation accompanying ischemic stroke accounts for some of its progression, at least acutely 6, 29, 30. A robust inflammatory reaction characterized by peripheral leukocyte influx into the cerebral parenchyma and activation of endogenous microglia follows focal cerebral ischemia. This leads to the generation of ROS which can then stimulate ischemic cells, even ischemic neurons, to secrete inflammatory factors. Generation of ROS by inflammatory cells occurs via several enzyme systems, but NOX is the major enzyme that generates superoxide. How NOX is activated in stroke is not entirely clear, but phosphorylation of the p47phox subunit appears important. p47phox phosphorylation can occur through several kinases also upregulated and activated by brain ischemia, including several protein kinase C isoforms and the p38 and p21 MAPKs. While numerous forms of the enzyme have now been described 8, phagocytic NOX, also referred to as NOX2, is associated with immune cells.
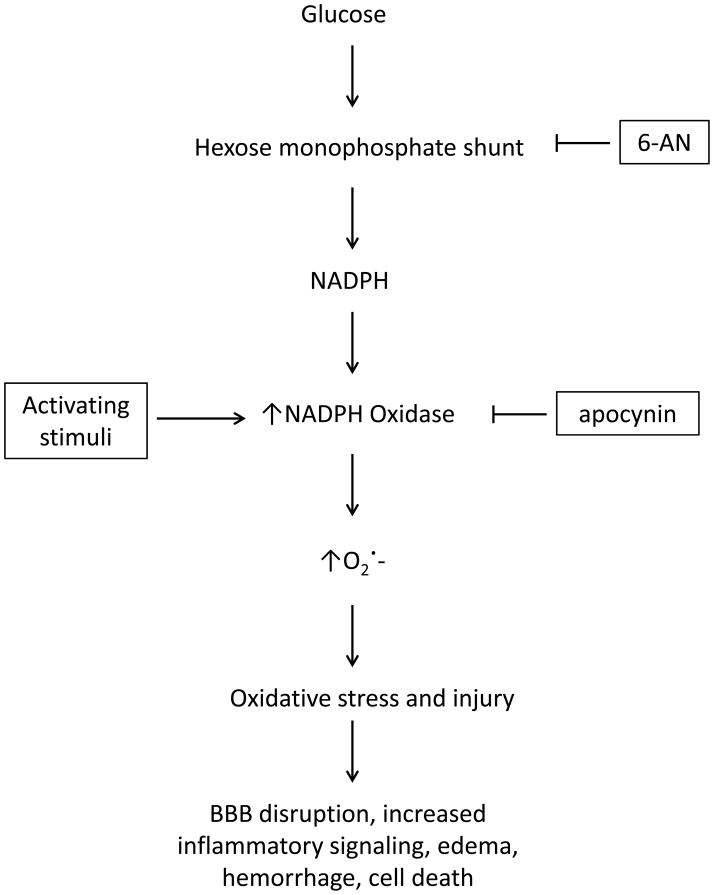
NOX has been documented to increase in the brain after experimental stroke 23. Mice deficient in the gp91phox subunit had smaller infarcts than mice with an intact enzyme in models of focal cerebral ischemia followed by reperfusion 31–33. Further, NOX appears to play a significant role in reperfusion injury, as reperfusion permits the restoration of glucose to the ischemic brain. Interestingly, reperfusion in the presence of glucose appears to increase neuronal NOX activity and NOX deficiency or inhibition prevents this (Figure). Further, NOX requires glucose metabolism through the hexose monophosphate shunt to supply NADPH, and blocking this pathway with 6-aminonicotinamide prevented the detrimental effects of reperfusion. Thus, the restoration of glucose (rather than oxygen, which is traditionally thought to be a source of ROS in this setting) appears to ‘fuel’ NOX by serving as a requisite electron donor to produce damaging levels of superoxide 34. NOX also appears to be a primary source of ROS generated by NMDA receptor activation 35.
Figure.
Participation of glucose in NADPH oxidase-mediated superoxide generation. A proposed scheme of how glucose during the reperfusion phase of stroke may contribute to oxidative stress via NADPH oxidase. As glucose is metabolized through the hexose monophosphate shunt, it generates NADPH. In the presence of activating stimuli, such as ischemia and other pro-inflammatory signals, NADPH oxidase is activated and through electron transfer, generates superoxide (O2·−). Superoxide can then lead to a variety of injurious downstream processes including blood brain barrier (BBB) disruption, edema formation, brain hemorrhage, further inflammatory signaling and cell death). This pathway is blocked by 6-aminonicotinamide (6-AN) or apocynin at the sites shown. Apocynin, by virtue of its ability to inhibit NADPH oxidase activation, has been shown limit damage and complications of experimental stroke.
The importance of glucose and NOX raises another important question. Since many stroke victims also have diabetes mellitus (DM), NOX may be highly activated in this population. To address this, we generated a rodent model of hyperglycemia where animals given intravenous glucose to cause acute elevations in blood levels were subjected to 90 minutes of transient middle cerebral artery occlusion (MCAO). We found that compared to animals subjected to MCAO but maintained normoglycemic, hyperglycemic animals suffered larger infarcts and worse neurological outcome. We then developed a model of hemorrhagic transformation caused by tPA treatment. Under condition of hyperglycemia, rats had more severe hemorrhage and higher mortality. This was also associated with increased infarct size, blood brain barrier disruption and superoxide production. However, these negative consequences of tPA treatment could be abrogated by treatment with a NOX inhibitor, in this case apocynin. Our results indicate that hyperglycemia can exacerbate post-tPA brain hemorrhage, and this effect might be mediated by NOX through increased superoxide generation 36.
NOX may also explain a relatively new phenomenon of ischemic ‘postconditioning’. Post-conditioning is a phenomenon of reduced ischemic injury when interrupted reperfusion is applied using three cycles of 15 sec reperfusion followed by 15 sec occlusion followed by eventual reperfusion. One group found that post-conditioning group led to less superoxide generation compared to conventional reperfusion. This was correlated to decreased expression of NOX subunits gp91phox and p47phox and activated Rac1–GTP in the post-conditioning group with subsequent reduction in superoxide generation 37.
The role of NOX in the inflammatory response accompanying stroke has certainly been widely studied for obvious reasons. Mice deficient in NOX’s gp91 demonstrated decreased mRNA expression of TNFα, CCL2, CCL3, and iNOS compared to wildtype litter mates. IL-1β protein expression was also reduced in gp91 KO mice 1 d and 3 d after cerebral ischemia, and this is was related to reduced ischemic brain damage 38. Bradykinin, well known to participate in blood brain barrier permeability, was shown to increase after experimental stroke. This led to the release of IL-1β which in turn activated NOX and led to blood brain barrier (BBB) breakdown. Animals treated with apocynin to inhibit NOX led to decreased IL-1β release and BBB breakdown compared to those treated with vehicle 39. Blocking NOX with apocynin decreased nitrogen species generation, inflammatory molecule release, apoptosis, and transcriptional factor degradation in rat model of experimental stroke. Rats treated with apocynin actually had reduced IκB-degradation with subsequent reduction in IL-1β and ICAM-1 presumably because NFκB activation was suppressed. Apocynin treatment was also associated with an overall anti-apoptotic effect of preventing Bcl-2 decrease and decreased expression of Bax 40.
Immune cells are known to participate in ischemic brain injury in two broad compartments: within the brain itself and the peripheral circulation. This is supported by the observations that inhibition of brain resident microglia or the inhibition or the prevention of infiltration of circulating leukocytes both appear to ameliorate damage from experimental stroke. In the ischemic brain, cells that generate superoxide through NOX are largely the brain’s resident immune cell, the microglia. Another source is from circulating leukocytes that have infiltrated the ischemic brain. NOX2 is well known to exist on microglia and leukocytes. To determine which compartment contributes more to NOX-mediated brain injury, we used a bone marrow chimera model, where we transplanted bone marrow from wild-type or NOX2-deficient mice into NOX2 or wild-type hosts, respectively 41. In the resulting phenotypes, NOX2 was present only in the circulating cells in one type of chimera, and present only in the brain of the other. Following experimental stroke, we found that NOX2 deletion in the circulation or the brain led to better outcomes compared to animals with fully intact NOX2, but the effect was most pronounced when NOX2 was deleted in the circulating cells. Thus, it appears that NOX2 derived from circulating cells contributes significantly to stroke pathogenesis, and may suggest an important intravascular target which may circumvent any requirement that a pharmaceutical needs to penetrate the blood brain barrier.
Other NOX subtypes have been studied in stroke models. In a recent study by Kleinschnitz et al. 42, NOX4 was found to have an especially profound effect in experimental stroke, as NOX4 deficient, but not NOX2 or NOX1 deficient mice were found to have improved neurological outcome. A pharmacological inhibitor had a similar effect. The lack of any effect by NOX1 or NOX2 deficiency goes against other reports in the scientific literature, and the authors could not identify any specific factors to explain this discrepancy as many of their models and paradigms matched those previously published.
III. NOX Inhibitors
Several NOX inhibitors are currently available, but are generally very low in specificity and selectivity. There has not been much clinical development since many are associated with toxicities that could hinder their use in humans. Yet, safer and more specific inhibitors are under development.
The most promising NOX inhibitor is apocynin which has been mentioned above. Its chemical name is 4-hydroxy-3-methoxy-acetophenone, and it is a methoxy-substituted catechol which is derived from the root extract of Picrorhiza kurroa, a medicinal herb that has been used for centuries by the Chinese to treat inflammatory diseases 43. Apocynin is a commonly used NOX inhibitor with relatively low affinity (IC50 ~10 μmol/L) in neutrophils 44. It does not seem to interfere with other PMN defense mechanisms, as it does not affect phagocytosis or intracellular killing 43. Apocynin inhibits the release of superoxide through NOX by blocking migration of p47phox to the membrane, thus interfering with assembly of the functional NOX complex 45. The inhibitory action of the compound is not entirely specific to NOX, however. Some of its inhibitory activity at least initially may involve myeloperoxidase (MPO) because apocynin does not inhibit NOX in cells deficient in MPO 46. MPO together with hydrogen peroxide can facilitate apocynin dimerization, and these dimers can prevent assembly of an active enzyme complex. Furthermore, agents such as zymosan that promote the release of MPO also enhance the efficacy of apocynin 47. In cells that are not rich in MPO, apocynin can reduce oxidant stress through a nonspecific oxidative scavenger effect instead of NOX inhibition 48. However, besides MPO, other peroxidases, such as horseradish peroxidase, can also induce apocynin dimer formation with a consequent NOX inhibitory effect 45, 49. In addition, in vivo studies showed that MPO secreted by neutrophils can be taken up by endothelial cells, in which apocynin can then be metabolized to active dimers, thus inhibiting vascular NOX 45. In line with this concept, it was observed that supplementation with thiol provided either as glutathione or cysteine prevents the inhibitory effect of apocynin on the NAPDH oxidase. Apocynin dimer formation may be responsible for its delayed inhibitory property 50, and it has been suggested that this dimer is what blocks NOX activity 47.
Apocynin has been studied by a few groups in brain ischemia models. From our own lab, we found that a dose of 2.5 mg/kg given parenterally just prior to reperfusion, or 1.5 h after ischemia onset, resulted in reduced infarct volume and improved neurological outcome 51. We also found that superoxide is largely generated in neurons and some microglia/monocytes, with no generation in brain vascular endothelial cells. Apocynin markedly reduced superoxide in the brain. However, apocynin at higher doses (3.75 and 5 mg/kg) failed to show any benefit, and actually increased the severity of brain hemorrhage. Thus, this rather narrow therapeutic dose range may limit its translation to the clinical level. However, other groups have shown salutary effects of apocynin at doses as high as 50 mg/kg 31, 52. In global cerebral ischemia, 5 mg/kg apocynin attenuated hippocampal injury when given prior to ischemia onset 53. In safety studies of uninjured mice, apocynin was well tolerated in single oral doses of up to 1000 mg/kg 54. Interestingly, apocynin failed to have an further beneficial effect in NOX2 deficient mice subjected to stroke, and might speak somewhat to its specificity or its dependence on NOX2 41.
In addition to apocynin, there are several other inhibitors with a more limited scope as they pertain to stroke. Diphenyleneiodonium (DPI) is the most commonly used inhibitor of NADPH oxidase 55. DPI impairs NADPH oxidase by flavoprotein inhibition so that NADPH oxidase cannot produce superoxide. One experimental study has shown that its administration in combination with dimethylsulfoxide (DMSO) reduced infarct size and blood brain barrier disruption 56. However, DPI can also inhibit other flavoenzymes in vivo. Flavoenzymes play a crucial role in many metabolic pathways so this is not a therapeutically viable inhibitor but it is valuable as a standard in vitro assays.
Another inhibitor is 4-(2-Aminoethyl)-benzenesulfonyl fluoride (AEBSF), is an irreversible serine protease inhibitor 57. AEBSF appears to have a direct affect on the plasma membrane components of NADPH oxidase and interferes with the binding of the cytosolic components p47phox and p67phox. AEBSF does not interfere with the electron transport and does not scavenge the oxygen radicals. Unfortunately AEBSF modifies many proteins by covalent attachment preferentially on tyrosine, and to a lesser extent on lysine, histidine, and the amino-terminus. AEBSF is quite stable in aqueous solution and the extent to which the protein is modified continues to increase for several days and this significantly limits its use in vivo. Tosylphenylalanychloromethane is another irreversible serine protease inhibitor similar to AEBSF and has a similar mechanism of action 58.
Other NADPH oxidase inhibitors include phenylarsine oxide (PAO) and gliotoxin (GTX) 59. PAO appears to prevent assembly of the NADPH enzyme complex via interacting with cysteine residues. However this interaction with the cysteine groups makes this inhibitor quite non-specific as it will also interact with other enzymes and proteins 60, 61. GTX is extracted from Aspergillus and it appears to inhibit the enzyme by blocking the phosphorylation of p47phox 47, 62. It also seems to react with the thiol groups thus limiting its specificity.
Honokiol is one of a group of NOX inhibitors that have been extracted from plants. Honokiol was isolated from the herb Magnolia officinalis and has been of particular interest because this compound appears to inhibit superoxide production after the respiratory burst and not before the enzyme is activated as with other inhibitors 63. Honokiol has also been shown to reduce lesion size in experimental focal cerebral ischemia followed by reperfusion 63, 64, and this decrease was correlated to a reduction in neutrophil infiltration and activation, and decreased lipid peroxidation 63.
The only inhibitor to date that directly interacts with a specific NOX homolog appears to be a plant derived naphthoquinone called plumbagin 65. Plumbagin (5-hydroxy-2-methyl-1,4-naphthoquinone) is a natural yellow pigment that comes from the roots of the black walnut plant Plumbago zeylanica. Plumbagin inhibits non-phagocytic NOX activity in HEK293 and LN229, a cell line that only express NOX4 and in a cell line transfected for NOX4 65. The regulation of NOX4 appears to be different from the other NOX homologs which require p47phoxand p67 phox and it has been observed that NOX4 alone can produce superoxide activity 14, 66, 67. The method by which it inhibits NOX-4 is unknown but it is unlikely that it is due to cytotoxic effects as the cells were viable after one hour incubation with plumbagin 65. It has been shown to have significant anti-cancer activity 68, 69 and may work by blocking superoxide production as many cancers have been shown to produce ROS and specifically express NOX homologs 16, 70. NOX4 is the dominant NOX homolog in vascular smooth muscle cells and its inhibition by plumbagin may well explain its anti-atheroscerotic effect.
The most selective NADPH oxidase inhibitor to date is a chimeric peptide gp91ds-tat 71. This peptide is constructed from the sequence of gp91phox that is known to be involved in the binding of gp91phox to p47phox and can inhibit the oxygen radical production in cell free assays (gp91 docking sequence or gp91ds). In order to deliver this peptide into the cells, the gp91ds was linked to HIV coat peptide (HIV-tat) that is known to be involved in internalization 71. This gp91ds-tat specifically binds to p47phox and prevents the formation of the NADPH oxidase complex. While this is the most specific inhibitor for NADPH oxidase it cannot distinguish between the phagocytic or non-phagocytic enzyme and it has little oral bioavailability as it is a peptide.
In addition to the above inhibitors there are NADPH oxidase inhibitors that have either been specifically developed by the pharmaceutical industry or are in clinical trials. Ebselen, 2-phenyl-1,2-benzisoselenazol-3(2H)-one, a mimic of glutathione peroxidase which also reacts with peroxynitrite, inhibits a variety of enzymes such as lipoxygenases, nitric oxide synthases, NADPH oxidase, protein kinase C and H+/K+-ATPase 72. Ebselen is therefore quite non-specific, but is being used at some centers for the treatment of stroke in Japan. Ebselen has shown efficacy if the treatment is started within 24 hours of the stroke 73, 74. Currently, a multicenter phase 3 ebselen trial is underway. A few other inhibitors have been developed by the pharmaceutical industry including VAS2870 (Vasopharm) 75, 76 and S17834 (Servier) 77. There is no information regarding these compounds mechanism of action although VAS2870 seems more specific to inhibit Nox2 whereas S17834 seems more specific in inhibiting vascular Nox. Finally, as noted in a review by Miller et al. 78, angiotensin converting enzyme inhibitors (ACE), angiotensin receptor-1 antagonists and the HMG-CoA (statins) drugs can all indirectly inhibit NADPH oxidase activity 79, 80. These are very effective cardiovascular drugs and it is tempting to suggest that their beneficial clinical effects may be enhanced by their ability to inhibit superoxide production in vivo.
IV. Conclusions
NADPH oxidase is an enzyme that broadly expressed in immune cells, especially those that reside in and infiltrate into the brain parenchyma after ischemic injury. While contributing to the oxidative stress exacerbated by reperfusion, NOX appears to depend on glucose as a substrate, further emphasizing the detrimental effects of hyperglycemia in stroke. By blocking the NOX activation in experimental stroke, several preclinical studies have demonstrated improved neurological outcome, and reduced severity of brain injury. This is associated with the reduced superoxide generation and the activation of downstream activities, such as reduced apoptosis, detrimental cytokine release and thus inflammatory responses. Further, inhibiting NOX within the intravascular space seems to also be a robust therapeutic strategy, thus circumventing the need for an inhibitor to necessarily penetrate into the brain in order to be effects. Yet, an effect and safe inhibitor has yet to make it to the clinical level.
Acknowledgments
This work was supported by grants to MAY from: NIH NINDS (R01 NS40516, P50 NS014543), and a Veterans Affairs Merit Award, which were administered by the Northern California Institute for Research and Education, and with resources of the Veterans Affairs Medical Center, San Francisco, California.
Footnotes
Conflict of interest statement: None of the authors have any financial interest relevant to the work presented in this manuscript.
References
- 1.Jahan R. Hyperacute therapy of ischemic stroke: Intravenous thrombolysis. Tech Vasc Interv Radiol. 2005;8:81–86. doi: 10.1053/j.tvir.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 2.Jahan R. Hyperacute therapy of acute ischemic stroke: Intraarterial thrombolysis and mechanical revascularization strategies. Tech Vasc Interv Radiol. 2005;8:87–91. doi: 10.1053/j.tvir.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 3.Kuroda S, Siesjo BK. Reperfusion damage following focal ischemia: Pathophysiology and therapeutic windows. Clin Neurosci. 1997;4:199–212. [PubMed] [Google Scholar]
- 4.Aronowski J, Strong R, Grotta JC. Reperfusion injury: Demonstration of brain damage produced by reperfusion after transient focal ischemia in rats. J Cereb Blood Flow Metab. 1997;17:1048–1056. doi: 10.1097/00004647-199710000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Chan PH. Reactive oxygen radicals in signaling and damage in the ischemic brain. J Cereb Blood Flow Metab. 2001;21:2–14. doi: 10.1097/00004647-200101000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Wang Q, Tang XN, Yenari MA. The inflammatory response in stroke. J Neuroimmunol. 2007;184:53–68. doi: 10.1016/j.jneuroim.2006.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Munzel T, Hink U, Heitzer T, Meinertz T. Role for nadph/nadh oxidase in the modulation of vascular tone. Ann N Y Acad Sci. 1999;874:386–400. doi: 10.1111/j.1749-6632.1999.tb09253.x. [DOI] [PubMed] [Google Scholar]
- 8.Lambeth JD. Nox enzymes and the biology of reactive oxygen. Nat Rev Immunol. 2004;4:181–189. doi: 10.1038/nri1312. [DOI] [PubMed] [Google Scholar]
- 9.Bokoch GM, Knaus UG. Nadph oxidases: Not just for leukocytes anymore! Trends Biochem Sci. 2003;28:502–508. doi: 10.1016/S0968-0004(03)00194-4. [DOI] [PubMed] [Google Scholar]
- 10.Groemping Y, Rittinger K. Activation and assembly of the nadph oxidase: A structural perspective. Biochem J. 2005;386:401–416. doi: 10.1042/BJ20041835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bedard K, Krause KH. The nox family of ros-generating nadph oxidases: Physiology and pathophysiology. Physiol Rev. 2007;87:245–313. doi: 10.1152/physrev.00044.2005. [DOI] [PubMed] [Google Scholar]
- 12.Anrather J, Racchumi G, Iadecola C. Nf-kappab regulates phagocytic nadph oxidase by inducing the expression of gp91phox. J Biol Chem. 2006;281:5657–5667. doi: 10.1074/jbc.M506172200. [DOI] [PubMed] [Google Scholar]
- 13.Lassegue B, Clempus RE. Vascular nad(p)h oxidases: Specific features, expression, and regulation. Am J Physiol Regul Integr Comp Physiol. 2003;285:R277–297. doi: 10.1152/ajpregu.00758.2002. [DOI] [PubMed] [Google Scholar]
- 14.Suh YA, Arnold RS, Lassegue B, Shi J, Xu X, Sorescu D, Chung AB, Griendling KK, Lambeth JD. Cell transformation by the superoxide-generating oxidase mox1. Nature. 1999;401:79–82. doi: 10.1038/43459. [DOI] [PubMed] [Google Scholar]
- 15.Lambeth JD, Cheng G, Arnold RS, Edens WA. Novel homologs of gp91phox. Trends Biochem Sci. 2000;25:459–461. doi: 10.1016/s0968-0004(00)01658-3. [DOI] [PubMed] [Google Scholar]
- 16.Cheng G, Cao Z, Xu X, van Meir EG, Lambeth JD. Homologs of gp91phox: Cloning and tissue expression of nox3, nox4, and nox5. Gene. 2001;269:131–140. doi: 10.1016/s0378-1119(01)00449-8. [DOI] [PubMed] [Google Scholar]
- 17.Quinn MT, Gauss KA. Structure and regulation of the neutrophil respiratory burst oxidase: Comparison with nonphagocyte oxidases. J Leukoc Biol. 2004;76:760–781. doi: 10.1189/jlb.0404216. [DOI] [PubMed] [Google Scholar]
- 18.Sorce S, Krause KH. Nox enzymes in the central nervous system: From signaling to disease. Antioxid Redox Signal. 2009;11:2481–2504. doi: 10.1089/ars.2009.2578. [DOI] [PubMed] [Google Scholar]
- 19.Infanger DW, Sharma RV, Davisson RL. Nadph oxidases of the brain: Distribution, regulation, and function. Antioxid Redox Signal. 2006;8:1583–1596. doi: 10.1089/ars.2006.8.1583. [DOI] [PubMed] [Google Scholar]
- 20.Green SP, Cairns B, Rae J, Errett-Baroncini C, Hongo JA, Erickson RW, Curnutte JT. Induction of gp91-phox, a component of the phagocyte nadph oxidase, in microglial cells during central nervous system inflammation. J Cereb Blood Flow Metab. 2001;21:374–384. doi: 10.1097/00004647-200104000-00006. [DOI] [PubMed] [Google Scholar]
- 21.Tammariello SP, Quinn MT, Estus S. Nadph oxidase contributes directly to oxidative stress and apoptosis in nerve growth factor-deprived sympathetic neurons. J Neurosci. 2000;20:RC53. doi: 10.1523/JNEUROSCI.20-01-j0006.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Serrano F, Kolluri NS, Wientjes FB, Card JP, Klann E. Nadph oxidase immunoreactivity in the mouse brain. Brain Res. 2003;988:193–198. doi: 10.1016/s0006-8993(03)03364-x. [DOI] [PubMed] [Google Scholar]
- 23.Vallet P, Charnay Y, Steger K, Ogier-Denis E, Kovari E, Herrmann F, Michel JP, Szanto I. Neuronal expression of the nadph oxidase nox4, and its regulation in mouse experimental brain ischemia. Neuroscience. 2005;132:233–238. doi: 10.1016/j.neuroscience.2004.12.038. [DOI] [PubMed] [Google Scholar]
- 24.Lambeth JD. Nox enzymes, ros, and chronic disease: An example of antagonistic pleiotropy. Free Radic Biol Med. 2007;43:332–347. doi: 10.1016/j.freeradbiomed.2007.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim MJ, Shin KS, Chung YB, Jung KW, Cha CI, Shin DH. Immunohistochemical study of p47phox and gp91phox distributions in rat brain. Brain Res. 2005;1040:178–186. doi: 10.1016/j.brainres.2005.01.066. [DOI] [PubMed] [Google Scholar]
- 26.Paravicini TM, Chrissobolis S, Drummond GR, Sobey CG. Increased nadph-oxidase activity and nox4 expression during chronic hypertension is associated with enhanced cerebral vasodilatation to nadph in vivo. Stroke. 2004;35:584–589. doi: 10.1161/01.STR.0000112974.37028.58. [DOI] [PubMed] [Google Scholar]
- 27.Miller AA, Drummond GR, Schmidt HH, Sobey CG. Nadph oxidase activity and function are profoundly greater in cerebral versus systemic arteries. Circ Res. 2005;97:1055–1062. doi: 10.1161/01.RES.0000189301.10217.87. [DOI] [PubMed] [Google Scholar]
- 28.Tejada-Simon MV, Serrano F, Villasana LE, Kanterewicz BI, Wu GY, Quinn MT, Klann E. Synaptic localization of a functional nadph oxidase in the mouse hippocampus. Mol Cell Neurosci. 2005;29:97–106. doi: 10.1016/j.mcn.2005.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zheng Z, Yenari MA. Post-ischemic inflammation: Molecular mechanisms and therapeutic implications. Neurol Res. 2004;26:884–892. doi: 10.1179/016164104X2357. [DOI] [PubMed] [Google Scholar]
- 30.Chamorro A, Hallenbeck J. The harms and benefits of inflammatory and immune responses in vascular disease. Stroke. 2006;37:291–293. doi: 10.1161/01.STR.0000200561.69611.f8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kahles T, Luedike P, Endres M, Galla HJ, Steinmetz H, Busse R, Neumann-Haefelin T, Brandes RP. Nadph oxidase plays a central role in blood-brain barrier damage in experimental stroke. Stroke. 2007;38:3000–3006. doi: 10.1161/STROKEAHA.107.489765. [DOI] [PubMed] [Google Scholar]
- 32.Walder CE, Green SP, Darbonne WC, Mathias J, Rae J, Dinauer MC, Curnutte JT, Thomas GR. Ischemic stroke injury is reduced in mice lacking a functional nadph oxidase. Stroke. 1997;28:2252–2258. doi: 10.1161/01.str.28.11.2252. [DOI] [PubMed] [Google Scholar]
- 33.Chen H, Song YS, Chan PH. Inhibition of nadph oxidase is neuroprotective after ischemia-reperfusion. J Cereb Blood Flow Metab. 2009;29:1262–1272. doi: 10.1038/jcbfm.2009.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Suh SW, Shin BS, Ma H, Van Hoecke M, Brennan AM, Yenari MA, Swanson RA. Glucose and nadph oxidase drive neuronal superoxide formation in stroke. Ann Neurol. 2008;64:654–663. doi: 10.1002/ana.21511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brennan AM, Suh SW, Won SJ, Narasimhan P, Kauppinen TM, Lee H, Edling Y, Chan PH, Swanson RA. Nadph oxidase is the primary source of superoxide induced by nmda receptor activation. Nat Neurosci. 2009;12:857–863. doi: 10.1038/nn.2334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Won SJ, Tang XN, Suh SW, Yenari MA, Swanson RA. Hyperglycemia promotes tissue plasminogen activator-induced hemorrhage by increasing superoxide production. Ann Neurol. 2011;70:583–590. doi: 10.1002/ana.22538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shen J, Bai XY, Qin Y, Jin WW, Zhou JY, Zhou JP, Yan YG, Wang Q, Bruce IC, Chen JH, Xia Q. Interrupted reperfusion reduces the activation of nadph oxidase after cerebral i/r injury. Free Radic Biol Med. 2011;50:1780–1786. doi: 10.1016/j.freeradbiomed.2011.03.028. [DOI] [PubMed] [Google Scholar]
- 38.Chen H, Kim GS, Okami N, Narasimhan P, Chan PH. Nadph oxidase is involved in post-ischemic brain inflammation. Neurobiol Dis. 2011;42:341–348. doi: 10.1016/j.nbd.2011.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Woodfin A, Hu DE, Sarker M, Kurokawa T, Fraser P. Acute nadph oxidase activation potentiates cerebrovascular permeability response to bradykinin in ischemia-reperfusion. Free Radic Biol Med. 2011;50:518–524. doi: 10.1016/j.freeradbiomed.2010.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Genovese T, Mazzon E, Paterniti I, Esposito E, Bramanti P, Cuzzocrea S. Modulation of nadph oxidase activation in cerebral ischemia/reperfusion injury in rats. Brain Res. 2011;1372:92–102. doi: 10.1016/j.brainres.2010.11.088. [DOI] [PubMed] [Google Scholar]
- 41.Tang XN, Zheng Z, Giffard RG, Yenari MA. Significance of marrow-derived nicotinamide adenine dinucleotide phosphate oxidase in experimental ischemic stroke. Ann Neurol. 70:606–615. doi: 10.1002/ana.22476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kleinschnitz C, Grund H, Wingler K, Armitage ME, Jones E, Mittal M, Barit D, Schwarz T, Geis C, Kraft P, Barthel K, Schuhmann MK, Herrmann AM, Meuth SG, Stoll G, Meurer S, Schrewe A, Becker L, Gailus-Durner V, Fuchs H, Klopstock T, de Angelis MH, Jandeleit-Dahm K, Shah AM, Weissmann N, Schmidt HH. Post-stroke inhibition of induced nadph oxidase type 4 prevents oxidative stress and neurodegeneration. PLoS Biol. 2010:8. doi: 10.1371/journal.pbio.1000479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stolk J, Hiltermann TJ, Dijkman JH, Verhoeven AJ. Characteristics of the inhibition of nadph oxidase activation in neutrophils by apocynin, a methoxy-substituted catechol. Am J Respir Cell Mol Biol. 1994;11:95–102. doi: 10.1165/ajrcmb.11.1.8018341. [DOI] [PubMed] [Google Scholar]
- 44.Simons JM, Hart BA, Ip Vai Ching TR, Van Dijk H, Labadie RP. Metabolic activation of natural phenols into selective oxidative burst agonists by activated human neutrophils. Free Radic Biol Med. 1990;8:251–258. doi: 10.1016/0891-5849(90)90070-y. [DOI] [PubMed] [Google Scholar]
- 45.Touyz RM. Apocynin, nadph oxidase, and vascular cells: A complex matter. Hypertension. 2008;51:172–174. doi: 10.1161/HYPERTENSIONAHA.107.103200. [DOI] [PubMed] [Google Scholar]
- 46.Stolk J, Rossie W, Dijkman JH. Apocynin improves the efficacy of secretory leukocyte protease inhibitor in experimental emphysema. Am J Respir Crit Care Med. 1994;150:1628–1631. doi: 10.1164/ajrccm.150.6.7952625. [DOI] [PubMed] [Google Scholar]
- 47.Van den Worm E, Beukelman CJ, Van den Berg AJ, Kroes BH, Labadie RP, Van Dijk H. Effects of methoxylation of apocynin and analogs on the inhibition of reactive oxygen species production by stimulated human neutrophils. Eur J Pharmacol. 2001;433:225–230. doi: 10.1016/s0014-2999(01)01516-3. [DOI] [PubMed] [Google Scholar]
- 48.Heumuller S, Wind S, Barbosa-Sicard E, Schmidt HH, Busse R, Schroder K, Brandes RP. Apocynin is not an inhibitor of vascular nadph oxidases but an antioxidant. Hypertension. 2008;51:211–217. doi: 10.1161/HYPERTENSIONAHA.107.100214. [DOI] [PubMed] [Google Scholar]
- 49.Vejrazka M, Micek R, Stipek S. Apocynin inhibits nadph oxidase in phagocytes but stimulates ros production in non-phagocytic cells. Biochim Biophys Acta. 2005;1722:143–147. doi: 10.1016/j.bbagen.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 50.Ximenes VF, Fernandes JR, Bueno VB, Catalani LH, de Oliveira GH, Machado RG. The effect of ph on horseradish peroxidase-catalyzed oxidation of melatonin: Production of n1-acetyl-n2-5-methoxykynuramine versus radical-mediated degradation. J Pineal Res. 2007;42:291–296. doi: 10.1111/j.1600-079X.2007.00419.x. [DOI] [PubMed] [Google Scholar]
- 51.Tang XN, Cairns B, Cairns N, Yenari MA. Apocynin improves outcome in experimental stroke with a narrow dose range. Neuroscience. 2008;154:556–562. doi: 10.1016/j.neuroscience.2008.03.090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tang LL, Ye K, Yang XF, Zheng JS. Apocynin attenuates cerebral infarction after transient focal ischaemia in rats. J Int Med Res. 2007;35:517–522. doi: 10.1177/147323000703500411. [DOI] [PubMed] [Google Scholar]
- 53.Wang Q, Tompkins KD, Simonyi A, Korthuis RJ, Sun AY, Sun GY. Apocynin protects against global cerebral ischemia-reperfusion-induced oxidative stress and injury in the gerbil hippocampus. Brain Res. 2006;1090:182–189. doi: 10.1016/j.brainres.2006.03.060. [DOI] [PubMed] [Google Scholar]
- 54.Pandey A, Kour K, Bani S, Suri KA, Satti NK, Sharma P, Qazi GN. Amelioration of adjuvant induced arthritis by apocynin. Phytother Res. 2009 doi: 10.1002/ptr.2803. [DOI] [PubMed] [Google Scholar]
- 55.Ellis JA, Cross AR, Jones OT. Studies on the electron-transfer mechanism of the human neutrophil nadph oxidase. Biochem J. 1989;262:575–579. doi: 10.1042/bj2620575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Nagel S, Genius J, Heiland S, Horstmann S, Gardner H, Wagner S. Diphenyleneiodonium and dimethylsulfoxide for treatment of reperfusion injury in cerebral ischemia of the rat. Brain Res. 2007;1132:210–217. doi: 10.1016/j.brainres.2006.11.023. [DOI] [PubMed] [Google Scholar]
- 57.Diatchuk V, Lotan O, Koshkin V, Wikstroem P, Pick E. Inhibition of nadph oxidase activation by 4-(2-aminoethyl)-benzenesulfonyl fluoride and related compounds. J Biol Chem. 1997;272:13292–13301. doi: 10.1074/jbc.272.20.13292. [DOI] [PubMed] [Google Scholar]
- 58.Gillibert M, Dehry Z, Terrier M, El Benna J, Lederer F. Another biological effect of tosylphenylalanylchloromethane (tpck): It prevents p47phox phosphorylation and translocation upon neutrophil stimulation. Biochem J. 2005;386:549–556. doi: 10.1042/BJ20041475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Jaquet V, Scapozza L, Clark RA, Krause KH, Lambeth JD. Small-molecule nox inhibitors: Ros-generating nadph oxidases as therapeutic targets. Antioxid Redox Signal. 2009;11:2535–2552. doi: 10.1089/ars.2009.2585. [DOI] [PubMed] [Google Scholar]
- 60.Doussiere J, Poinas A, Blais C, Vignais PV. Phenylarsine oxide as an inhibitor of the activation of the neutrophil nadph oxidase--identification of the beta subunit of the flavocytochrome b component of the nadph oxidase as a target site for phenylarsine oxide by photoaffinity labeling and photoinactivation. Eur J Biochem. 1998;251:649–658. doi: 10.1046/j.1432-1327.1998.2510649.x. [DOI] [PubMed] [Google Scholar]
- 61.Kutsumi H, Kawai K, Johnston RB, Jr, Rokutan K. Evidence for participation of vicinal dithiols in the activation sequence of the respiratory burst of human neutrophils. Blood. 1995;85:2559–2569. [PubMed] [Google Scholar]
- 62.Yoshida LS, Abe S, Tsunawaki S. Fungal gliotoxin targets the onset of superoxide-generating nadph oxidase of human neutrophils. Biochem Biophys Res Commun. 2000;268:716–723. doi: 10.1006/bbrc.2000.2192. [DOI] [PubMed] [Google Scholar]
- 63.Liou KT, Shen YC, Chen CF, Tsao CM, Tsai SK. Honokiol protects rat brain from focal cerebral ischemia-reperfusion injury by inhibiting neutrophil infiltration and reactive oxygen species production. Brain Res. 2003;992:159–166. doi: 10.1016/j.brainres.2003.08.026. [DOI] [PubMed] [Google Scholar]
- 64.Chen CM, Liu SH, Lin-Shiau SY. Honokiol, a neuroprotectant against mouse cerebral ischaemia, mediated by preserving na+, k+-atpase activity and mitochondrial functions. Basic Clin Pharmacol Toxicol. 2007;101:108–116. doi: 10.1111/j.1742-7843.2007.00082.x. [DOI] [PubMed] [Google Scholar]
- 65.Ding Y, Chen ZJ, Liu S, Che D, Vetter M, Chang CH. Inhibition of nox-4 activity by plumbagin, a plant-derived bioactive naphthoquinone. J Pharm Pharmacol. 2005;57:111–116. doi: 10.1211/0022357055119. [DOI] [PubMed] [Google Scholar]
- 66.Barry-Lane PA, Patterson C, van der Merwe M, Hu Z, Holland SM, Yeh ET, Runge MS. P47phox is required for atherosclerotic lesion progression in apoe(−/−) mice. J Clin Invest. 2001;108:1513–1522. doi: 10.1172/JCI11927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Shiose A, Kuroda J, Tsuruya K, Hirai M, Hirakata H, Naito S, Hattori M, Sakaki Y, Sumimoto H. A novel superoxide-producing nad(p)h oxidase in kidney. J Biol Chem. 2001;276:1417–1423. doi: 10.1074/jbc.M007597200. [DOI] [PubMed] [Google Scholar]
- 68.Hazra B, Sarkar R, Bhattacharyya S, Ghosh PK, Chel G, Dinda B. Synthesis of plumbagin derivatives and their inhibitory activities against ehrlich ascites carcinoma in vivo and leishmania donovani promastigotes in vitro. Phytother Res. 2002;16:133–137. doi: 10.1002/ptr.867. [DOI] [PubMed] [Google Scholar]
- 69.Parimala R, Sachdanandam P. Effect of plumbagin on some glucose metabolising enzymes studied in rats in experimental hepatoma. Mol Cell Biochem. 1993;125:59–63. doi: 10.1007/BF00926835. [DOI] [PubMed] [Google Scholar]
- 70.Szatrowski TP, Nathan CF. Production of large amounts of hydrogen peroxide by human tumor cells. Cancer Res. 1991;51:794–798. [PubMed] [Google Scholar]
- 71.Rey FE, Cifuentes ME, Kiarash A, Quinn MT, Pagano PJ. Novel competitive inhibitor of nad(p)h oxidase assembly attenuates vascular o(2)(−) and systolic blood pressure in mice. Circ Res. 2001;89:408–414. doi: 10.1161/hh1701.096037. [DOI] [PubMed] [Google Scholar]
- 72.Cotgreave IA, Duddy SK, Kass GE, Thompson D, Moldeus P. Studies on the anti-inflammatory activity of ebselen. Ebselen interferes with granulocyte oxidative burst by dual inhibition of nadph oxidase and protein kinase c? Biochem Pharmacol. 1989;38:649–656. doi: 10.1016/0006-2952(89)90211-6. [DOI] [PubMed] [Google Scholar]
- 73.Parnham M, Sies H. Ebselen: Prospective therapy for cerebral ischaemia. Expert Opin Investig Drugs. 2000;9:607–619. doi: 10.1517/13543784.9.3.607. [DOI] [PubMed] [Google Scholar]
- 74.Yamaguchi T, Sano K, Takakura K, Saito I, Shinohara Y, Asano T, Yasuhara H. Ebselen in acute ischemic stroke: A placebo-controlled, double-blind clinical trial. Ebselen study group. Stroke. 1998;29:12–17. doi: 10.1161/01.str.29.1.12. [DOI] [PubMed] [Google Scholar]
- 75.ten Freyhaus H, Huntgeburth M, Wingler K, Schnitker J, Baumer AT, Vantler M, Bekhite MM, Wartenberg M, Sauer H, Rosenkranz S. Novel nox inhibitor vas2870 attenuates pdgf-dependent smooth muscle cell chemotaxis, but not proliferation. Cardiovasc Res. 2006;71:331–341. doi: 10.1016/j.cardiores.2006.01.022. [DOI] [PubMed] [Google Scholar]
- 76.Stielow C, Catar RA, Muller G, Wingler K, Scheurer P, Schmidt HH, Morawietz H. Novel nox inhibitor of oxldl-induced reactive oxygen species formation in human endothelial cells. Biochem Biophys Res Commun. 2006;344:200–205. doi: 10.1016/j.bbrc.2006.03.114. [DOI] [PubMed] [Google Scholar]
- 77.Cayatte AJ, Rupin A, Oliver-Krasinski J, Maitland K, Sansilvestri-Morel P, Boussard MF, Wierzbicki M, Verbeuren TJ, Cohen RA. S17834, a new inhibitor of cell adhesion and atherosclerosis that targets nadph oxidase. Arterioscler Thromb Vasc Biol. 2001;21:1577–1584. doi: 10.1161/hq1001.096723. [DOI] [PubMed] [Google Scholar]
- 78.Miller AA, Drummond GR, Sobey CG. Novel isoforms of nadph-oxidase in cerebral vascular control. Pharmacol Ther. 2006;111:928–948. doi: 10.1016/j.pharmthera.2006.02.005. [DOI] [PubMed] [Google Scholar]
- 79.Warnholtz A, Nickenig G, Schulz E, Macharzina R, Brasen JH, Skatchkov M, Heitzer T, Stasch JP, Griendling KK, Harrison DG, Bohm M, Meinertz T, Munzel T. Increased nadh-oxidase-mediated superoxide production in the early stages of atherosclerosis: Evidence for involvement of the renin-angiotensin system. Circulation. 1999;99:2027–2033. doi: 10.1161/01.cir.99.15.2027. [DOI] [PubMed] [Google Scholar]
- 80.Wagner AH, Kohler T, Ruckschloss U, Just I, Hecker M. Improvement of nitric oxide-dependent vasodilatation by hmg-coa reductase inhibitors through attenuation of endothelial superoxide anion formation. Arterioscler Thromb Vasc Biol. 2000;20:61–69. doi: 10.1161/01.atv.20.1.61. [DOI] [PubMed] [Google Scholar]