Abstract
Atopic dermatitis (AD, atopic eczema) is driven by a complex relationship between genetic predisposition and environmental exposures. We sought to determine the impact of specific climatic factors on the US prevalence of AD. We used a merged analysis of the 2007 National Survey of Children's Health from a representative sample of 91,642 children age 0–17 years and the 2006–2007 National Climate Data Center and Weather Service measurements of relative humidity (%), indoor heating degree days (HDD), clear sky UV indices ozone levels, and outdoor air temperature. As a proxy for AD, we used an affirmative response to the NSCH survey question asking whether the participant’s child has been given a doctor diagnosis of “eczema or any other kind of skin allergy” in the previous 12 months. In multivariate models controlling for sex, race/ethnicity, age and household income, eczema prevalence was significantly lower with highest-quartile mean annual relative humidity (logistic regression, adjusted odds ratio [95% confidence interval]=0.82 [0.71–0.96], P=0.01) and issued UV index (0.73 [0.64–0.84], P<0.0001), and with two other factors associated with increased UV exposure. Eczema prevalence was decreased with highest-quartile air temperature (0.80 [0.70–0.92], P=0.002), but increased with 3rd–quartile mean annual HDD (1.26 [1.11–1.43], P=0.0003). This study provides evidence of climate influences on the US prevalence of childhood eczema.
Keywords: eczema prevalence, atopic dermatitis, relative humidity, dew point, indoor heating, ultraviolet index, air temperature, pediatric, children
Introduction
Atopic Dermatitis (AD, atopic eczema) is a chronic pruritic skin disorder that is a significant cause of morbidity and healthcare costs in the United States and worldwide. The prevalence of AD in childhood was 2–3% before 1960, 9–12% after 1970,and is now as high as 20% (Wuthrich, 1999; Wuthrich and Schmid-Grendelmeier, 2003). Several international studies demonstrated increased prevalence of eczema and allergic disorders in children and adolescents between 1995 and 2007 (Kabir et al., 2011; Selnes et al., 2005; Zar et al., 2007). The reasons for this increase are not well understood.
Dynamic climate factors may play a role in driving eczema prevalence. Several classic case reports and series correlated low humidity with eczematous eruptions (Chernosky, 1962; Gaul and Underwood, 1952; Rycroft and Smith, 1980). In a questionnaire series of 21 dermatologists in 19 countries by Rajka (Rajka, 1986), AD was thought to be related to cold/dry and hot/humid weather. However, there are conflicting data regarding the impact of specific climate factors. A Spanish study found an inverse association of eczema prevalence with temperature and number of sunny hours, and a positive association with precipitation and outdoor humidity (Suarez-Varela et al., 2008). In contrast, an international study of climate factors found an inverse association with temperature and humidity (Weiland et al., 2004). A small-scale exploratory study of children with AD found that hot weather, damp weather, sweating and stress were also associated with increased disease flares with lags of 0 – 4 days after exposure (Langan et al., 2006). Moreover, little is known about the effects of US climate factors on state- and nationwide eczema prevalence. We hypothesized that low indoor and outdoor humidity exacerbates subclinical eczema, thus increasing disease prevalence, via detrimental effects on the skin barrier. In the present study, we examine the effects of climate variables, namely outdoor humidity and heating degree days (HDD) as a modifier of indoor humidity on childhood eczema prevalence in the US. Moreover, we hypothesized that increased ultraviolet (UV) radiation exposure in areas with warmer climate might protect against eczema given the anti-inflammatory effects of UV and possible therapeutic effects of vitamin D. We therefore also examined the effects of UV exposure and temperature on eczema prevalence.
Results
Population characteristics
Overall the prevalence of eczema was 12.23% (95% CI=11.73–12.73). After exclusion of the 12.45% of respondents that reported no healthcare interactions within the past 12 months, the final eczema prevalence was 12.98% (95% CI=12.43–13.54). Children with eczema were significantly younger (mean: 7.5 vs. 8.5 years, P<0.0001) and were more frequently African-American (22.2% vs. 13.5%, P<0.0001) compared with children with no eczema (Table 1). There were no differences of sex or household income between children with eczema vs. no eczema.
Table 1.
Subject characteristics*.
| Variable | No eczema | Eczema | P-value# |
|---|---|---|---|
| Age (yr) – mean (95% CI) | 8.4 (8.3–8.5) | 7.5 (7.3–7.7) | < 0.0001 |
| Race/ethnicity – no. (%) | < 0.0001 | ||
| African-American | 6495 (13.5) | 1618 (22.2) | |
| Hispanic | 8582 (20.4) | 1215 (15.6) | |
| White | 46777 (57.1) | 6326 (52.5) | |
| Other/mixed | 6186 (9.0) | 1079 (9.7) | |
| Female sex – no. (%) | 33165 (48.3) | 5016 (49.8) | 0.25 |
| Household income (Poverty level) – no. (%) | 0.76 | ||
| 0 – 99% | 8023 (18.2) | 1253 (17.5) | |
| 100 – 199% | 11356 (20.4) | 1756 (20.4) | |
| 200 – 399% | 22966 (30.9) | 3478 (32.0) | |
| ≥400% | 26835 (30.5) | 3921 (30.1) |
Rao-Scott chi square test.
Missing data were encountered in 79 subjects (0.001%) for the eczema outcome, 0 (0.0%) for age, 4,517 for race/ethnicity (5.7%), 79 for sex (0.001%) and 0 (0.0%) for household income.
Relative humidity
Residence in a state with the highest quartile mean annual relative humidity was associated with decreased prevalence of eczema compared with lowest quartile (11.2% vs. 13.6%; logistic regression, OR=0.80, 95% CI=0.69–0.93, P=0.003) (Table 2). This association remained significant in multivariate models including age, race/ethnicity, sex and household income (P=0.01). However, the second and third quartile humidity were not associated with eczema prevalence (P≥0.1).
Table 2.
Association between eczema prevalence and mean relative humidity, issued UV index, annual temperature, heating degree days (HDD) and precipitation.
| Quartile (min, max) | Eczema Frequency |
Eczema Prevalence (95% CI) |
OR* (95% CI) |
P-value | Adjusted OR** (95% CI) |
P-value |
|---|---|---|---|---|---|---|
| Mean relative humidity (%)# | ||||||
| 1st (24.3, 62.8) | 2572 | 13.6 (12.7 14.5) |
1.00 | – | 1.00 | – |
| 2nd (63.0, 66.9) | 2528 | 14.7 (13.7, 15.6) |
1.09 (0.98, 1.22) |
0.10 | 1.08 (0.97, 1.21) |
0.15 |
| 3rd (67.0, 69.5) | 2556 | 13.5 (12.6, 14.4) |
1.00 (0.89, 1.11) |
0.93 | 1.00 (0.90, 1.12) |
0.97 |
| 4th (69.7, 74.3) | 2350 | 11.2 (9.9, 12.4) |
0.80 (0.69, 0.93) |
0.003 | 0.82 (0.71, 0.96) | 0.01 |
| Issued UV index## | ||||||
| 1st (1.8 – 4.1) | 2959 | 14.0 (13.1 – 15.0) |
1.00 | – | 1.00 | – |
| 2nd (4.1 – 4.6) | 2854 | 13.3 (12.5 – 14.1) |
0.94 (0.84 – 1.04) |
0.24 | 0.92 (0.83 – 1.03) |
0.13 |
| 3rd (4.7 – 5.7) | 2720 | 12.4 (11.7 – 13.1) |
0.87 (0.78 – 0.96) |
0.006 | 0.83 (0.75 – 0.92) |
0.0006 |
| 4th (5.9 – 9.2) | 2797 | 10.8 (9.8 – 11.7) |
0.74 (0.65 – 0.84) |
<0.0001 | 0.73 (0.64 – 0.84) |
<0.0001 |
| Annual mean temperature (deg F)### | ||||||
| 1st (42.7 – 47.2) | 2384 | 14.8 (13.5, 16.0) |
1.00 | – | 1.00 | – |
| 2nd (47.2 – 53.3) | 2482 | 13.8 (12.9, 14.7) |
0.93 (0.82, 1.05) |
0.23 | 0.95 (0.84, 1.07) |
0.40 |
| 3rd (53.4 – 57.5) | 2430 | 11.5 (10.4, 12.7) |
0.76 (0.65, 0.87) |
0.0002 | 0.75 (0.65, 0.88) |
0.0002 |
| 4th (59.2 – 72.9) | 2397 | 12.9 (11.9, 13.9) |
0.85 (0.75, 0.98) |
0.02 | 0.80 (0.70, 0.92) |
0.002 |
| Mean annual HDD#### | ||||||
| 1st (51.2 – 290.3) | 2397 | 12.9 (11.9, 13.9) |
1.00 | – | 1.00 | – |
| 2nd (297.1 – 427.3) | 2430 | 11.5 (10.4 12.7) |
0.88 (0.76, 1.02) |
0.09 | 0.94 (0.81, 1.09) |
0.41 |
| 3rd (431.6 – 562.2) | 2615 | 14.7 (13.8, 15.7) |
1.17 (1.04, 1.31) |
0.01 | 1.26 (1.11, 1.43) |
0.0003 |
| 4th (571.3 – 707.1) | 2251 | 13.1 (12.1, 14.2) |
1.02 (0.90, 1.17) |
0.72 | 1.11 (0.97, 1.27) |
0.14 |
| Mean annual precipitation (in)##### | ||||||
| 1st (0.6 – 2.3) | 2111 | 10.2 (8.6 – 11.8) |
1.00 | – | 1.00 | – |
| 2nd (2.3 – 3.5) | 2376 | 13.1 (12.2, 14.1) |
1.33 (1.11 – 1.60) |
0.002 | 1.22 (1.01 – 1.47) |
0.03 |
| 3rd (3.5 – 3.8) | 2360 | 14.3 (13.4, 15.3) |
1.47 (1.22 – 1.76) |
< 0.0001 | 1.34 (1.11 – 1.62) |
0.002 |
| 4th (3.9 – 4.5) | 2406 | 13.6 (12.8, 14.4) |
1.39 (1.16 – 1.66) |
0.0003 | 1.29 (1.07 – 1.54) |
0.007 |
Annual statewide mean values of relative humidity (%) for 2006 – 2007 were downloaded from National Oceanic & Atmospheric Administration (NOAA), National Climate Data Center (NCDC) at http://www7.ncdc.noaa.gov/CDO/dataproduct. Relative humidity is a measure of water vapor in the air that is dependent on both the air temperature and pressure.
Monthly statewide mean values of issued UV indices for 2006 – 2007 were downloaded from the NOAA, National Weather Service, Climate Prediction Center at ftp://ftp.cpc.ncep.noaa.gov/long/uv/cities. The issued UV index accounts for the cloud effects on UV transmission. N.B. There were no states with extreme issued UV indices (≥ 11) during the time period of 2006 – 2007.
Annual statewide mean values of “time-bias” corrected temperatures (Degrees Fahrenheit to 10ths) for 2006–2007 were downloaded from the NOAA, NCDC at ftp://ftp.ncdc.noaa.gov/pub/data/cirs/.
Annual statewide mean HDD for 2006 – 2007 were downloaded from the NOAA, NCDC at ftp://ftp.ncdc.noaa.gov/pub/data/cirs/. HDD is a statewide population-weighted measure of energy demand to heat indoor structures by one degree for one day using a baseline temperature of 65 degrees Fahrenheit. HDD are calculated as the sum of differences between the average daily temperature and a base of 65 deg Fahrenheit averaged over the span of 12 months.
Monthly statewide mean values of “time-bias” corrected annual precipitation (in) for 2006 – 2007 were downloaded from the NOAA, NCDC at ftp://ftp.ncdc.noaa.gov/pub/data/cirs/.
Univariate logistic regression models were constructed with eczema (yes/no) modeled as the dependent variable and relative humidity, issued UV index, mean annual temperature, HDD and precipitation values as independent variables.
Multivariate logistic regression models were constructed with eczema (yes/no) modeled as the dependent variable and relative humidity values, issued UV index, mean annual temperature, HDD and precipitation as independent variables, including age (continuous), race/ethnicity (African-American, Hispanic, Caucasian, or Multi/Other), sex (male or female), household income (0–99%, 100–199%, 200–399%, 400+% of poverty level).
UV index
Residence in a state with the third and highest quartile mean annual issued UV index was associated with decreased prevalence of eczema compared with lowest quartile (12.4 and 10.8% vs. 14.0%; P=0.006 and <0.0001, respectively) (Table 2). These association remained significant in multivariate models including age, race/ethnicity, sex and household income (P=0.0006 and <0.0001). However, the second quartile issued UV index was not associated with eczema prevalence (P≥0.13).
UV index was also categorized according to the WHO classification. Since <1% of respondents lived in states with low (0–2) or very high (8–10), and no states had extreme (≥11) mean annual UV indices, UV indices were dichotomized into mild–moderate (0–5) vs. high–very high (6–10) in order to avoid biased estimates of OR and CI,. Residence in a state with high– very high mean annual issued UV index (6–10) was associated with decreased prevalence of eczema compared with mild–moderate (0–5) (11.1% vs. 14.0%; OR=0.77, 95% CI=0.67–0.87, P<0.0001) (Table 3). This association remained significant in a multivariate model including age, race/ethnicity, sex and household income (P=0.0005). Similar results were found for clear sky UV index and probability of clear skies (Table 3). Conversely, highest-quartile stratospheric ozone levels were associated with increased prevalence of eczema. However, 2nd and 3rd quartiles were not associated with eczema prevalence.
Table 3.
Association between eczema prevalence, issued UV index, clear sky UV index, stratospheric ozone levels and probability of clear skies.
| Variable – percent | Eczema Frequency |
Eczema Prevalence (95% CI) |
OR* (95% CI) |
P-value | Adjusted OR** (95% CI) |
P-value |
|---|---|---|---|---|---|---|
| Issued UV index – (min – max) | ||||||
| Low – Moderate (0 – 5) | 8288 | 14.0 (13.5, 14.6) |
1.00 | – | 1.00 | – |
| High – Extreme (6 – 10) | 2120 | 11.1 (9.9, 12.3) |
0.77 (0.67, 0.87) |
<0.0001 | 0.78 (0.68, 0.90) |
0.0005 |
| Clear sky UV index – (min – max) | ||||||
| Low – Moderate (0 – 5) | 5743 | 14.4 (13.7, 15.0) |
1.00 | – | 1.000 | – |
| High – Extreme (6 – 10) | 4665 | 11.9 (11.1, 12.7) |
0.81 (0.73, 0.89) |
< 0.0001 | 0.80 (0.72, 0.88) |
< 0.0001 |
| Stratospheric ozone levels (parts per billion) – quartile (min – max) | ||||||
| 1st (276.5 – 300.6) | 2563 | 12.7 (11.7, 13.8) |
1.00 | – | 1.00 | – |
| 2nd (301.7 – 316.3) | 2598 | 11.1 (9.8, 12.4) |
0.86 (0.73, 1.01) |
0.06 | 0.92 (0.78, 1.09) |
0.33 |
| 3rd (316.9 – 325.1) | 2445 | 13.9 (13.0, 14.7) |
1.10 (0.98, 1.25) |
0.11 | 1.15 (1.01, 1.30) |
0.04 |
| 4th (327.6 – 373.4) | 2802 | 14.9 (13.8, 15.9) |
1.20 (1.06, 1.36) |
0.005 | 1.28 (1.12, 1.46) |
0.0004 |
| Probability of clear skies – quartile (min – max) | ||||||
| 1st (72.5 – 81.0) | 2757 | 14.6 (13.7, 15.6) |
1.00 | – | 1.00 | – |
| 2nd (81.3 – 83.5) | 2379 | 13.2 (12.4, 14.0) |
0.89 (0.80, 0.99) |
0.02 | 0.89 (0.80, 0.99) |
0.03 |
| 3rd (83.6 – 86.3) | 2768 | 13.3 (12.2, 14.4) |
0.90 (0.80, 1.02) |
0.09 | 0.84 (0.74, 0.95) |
0.007 |
| 4th (86.4 – 95.8) | 2504 | 11.1 (9.9, 12.4) |
0.73 (0.63, 0.85) |
<0.0001 | 0.73 (0.63, 0.85) |
<0.0001 |
Monthly statewide mean values of clear sky index, stratospheric ozone levels (parts per billion) and percent probability of clear skies for 2006 – 2007 were downloaded from the NOAA, National Weather Service, Climate Prediction Center at ftp://ftp.cpc.ncep.noaa.gov/long/uv/cities. The issued sky UV index accounts for cloud effects on UV transmission, while the clear sky UV index does not. UV index exposure was dichotomized by the World Health Organization criteria for low – moderate (0 – 5) and to high to very high (6 – 10). N.B. There were no states with extreme issued UV indices (≥ 11) during the time period of 2006 – 2007.
Univariate logistic regression models were constructed with eczema (yes/no) modeled as the dependent variable and environmental variables as independent variables. Ozone levels and probability of clear skies were divided into quartiles.
Multivariate logistic regression models were constructed with eczema (yes/no) modeled as the dependent variable and environmental variables as independent variables, including age, race/ethnicity (African-American, Hispanic, Caucasian, or Multi/Other), sex (male or female), household income (0–99%, 100–199%, 200–399%, 400+% of poverty level). Ozone levels and probability of clear skies were divided into quartiles.
Temperature
Residence in a state with highest quartile mean annual temperature was associated with decreased prevalence of eczema compared with lowest quartile (12.9% vs. 14.8, respectively; OR=0.85, 95% CI=0.75–0.98, P=0.02) (Table 2). This association remained significant in multivariate models including age, race/ethnicity, sex and household income (P=0.002).
We further evaluated how eczema prevalence varied by seasonal temperature means owing to concern for dominant effects of a particular season. We found that the highest-quartile mean temperatures were significantly associated with lower eczema prevalence in all seasons except autumn (Table S1). However, the 2nd and 3rd quartiles were only associated with eczema prevalence in some seasons.
HDD
Residence in a state with the 3rd quartile mean annual HDD was associated with an increased prevalence of eczema compared to the lowest quartile (P=0.01) (Table 2). This association remained significant in a multivariate model including age, race/ethnicity, sex and household income (P=0.0003). However, the second and fourth quartile humidity were not associated with eczema prevalence (P≥0.09).
We further evaluated the effect of seasonal HDD on eczema prevalence and found the association between 3rd quartile HDD and eczema prevalence remained significant in all seasons, while the 4th quartile remained significant in all seasons except autumn (Table S2).
Precipitation
Residence in a state with higher mean annual precipitation was associated with increased prevalence of eczema compared to the lowest quartile (Table 2). These associations remained significant for the 3rd and 4th quartiles in multivariate models including age, race/ethnicity, sex and household income (P≤0.007). We further evaluated how eczema prevalence varied by seasonal precipitation means and found that the higher quartile mean precipitation were associated with a higher eczema prevalence in spring and autumn (Table S3).
Principal component analysis
PCA was used to determine the most common combinations of climate variables (factors) occurring in the US. Two factors were identified by principal components analysis: factor 1) high temperature, low HDD and high issued UV index and factor 2) high humidity and precipitation (Table 4). Factor 1 was associated with lower odds of eczema (OR=0.93, 95% CI=0.88–0.98; P=0.008), suggesting that residence in locations with combined higher temperature and UV index and lower HDD is protective against eczema. Factor 2 was associated with higher odds of eczema (OR=1.09, 95% CI=1.04–1.15; P=0.001), suggesting that residence in a location with high humidity combined with high precipitation and low UV index may predispose toward eczema.
Table 4.
Principal component analysis of the association between eczema prevalence and environmental variables.
| Variable | Factor 1 | Factor 2 |
|---|---|---|
| Loading values | ||
| Relative humidity | −0.05 | 0.91* |
| Issued UV index | 0.86* | −0.41* |
| HDD | −0.98* | −0.16 |
| Temperature | 0.98* | 0.12 |
| Precipitation | 0.08 | 0.92* |
|
Eigenvalues (Percent variance explained) |
2.67 (53.4%) |
1.88 (37.5%) |
| Factor description | High temperature and UV index | High humidity and precipitation, low UV index |
|
OR (95% CI) P-value |
0.931 (0.88 – 0.98) P = 0.008 |
1.09 (1.04 – 1.15) P = 0.001 |
|
Adjusted OR (95% CI) P-value |
0.913 (0.86 – 0.97) P = 0.002 |
1.05 (0.99 – 1.11) P = 0.07 |
Principal component analysis with varimax rotation was used to estimate the combined effects of relative humidity, UV index, temperature, and HDD. Factors were retained if eigenvalue >1, proportion of variance accounted for > 10% and loading value > 0.4. Logistic regression was then performed using separate factor scores for each of the retained factors. Odds ratios (OR) and 95% confidence intervals (95% CI) were calculated. Adjusted odds ratios (aOR) and 95% CI were calculated from multivariate models including age, sex, race/ethnicity, and household income.
Discussion
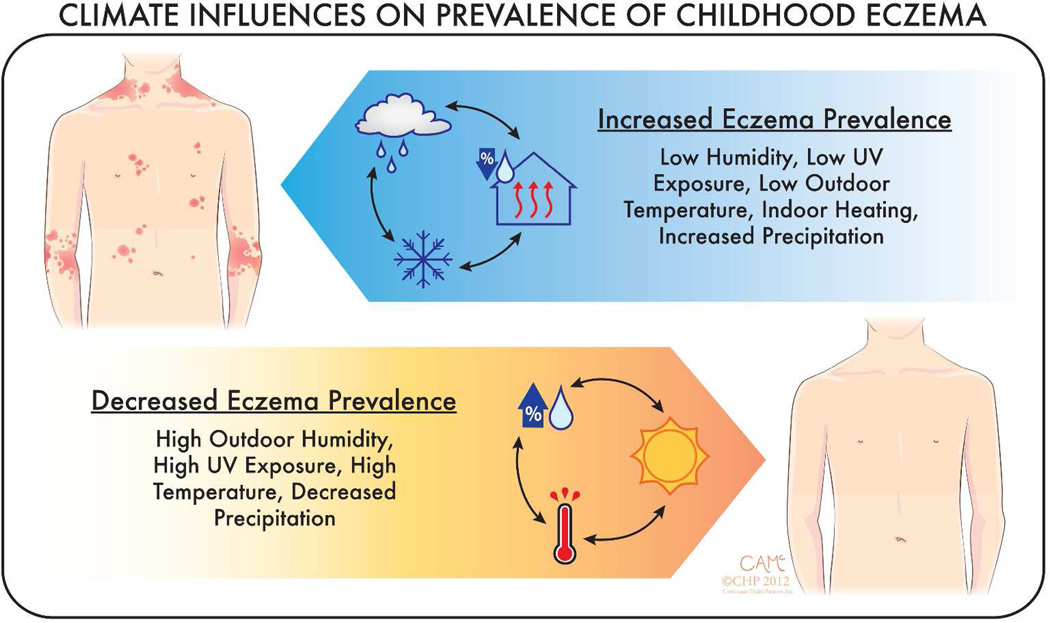
The present study found that outdoor climate conditions influence the prevalence of pediatric eczema in the United States. Specifically, significantly lower eczema prevalence was found in areas with: higher relative humidity, higher UV index, higher mean temperatures, lower precipitation and fewer days needing heat (summarized in Figure 1). The higher prevalence of eczema observed under certain climatic conditions may be attributed to the environmental triggering of subclinical disease in predisposed children. Moreover, climate factors likely also aggravate eczema resulting in chronic disease and/or flares.
Figure 1.
Climate influences on prevalence of childhood eczema. Lower eczema prevalence was found in areas with higher relative humidity, higher UV index, higher mean temperatures, lower precipitation and less indoor heating.
The results of this study have a number of potential clinical implications. First, children with a predisposition for AD, such as those with filaggrin mutations, appear to have a higher risk for AD when exposed to certain climate factors. Our data show climate factors impact upon AD during all seasons, which suggests that they have a cumulative effect across multiple months or seasons in driving eczema. This underscores the importance of continuous use of proper skin care for the prevention and maintenance management of disease. Finally, these data may be incorporated into patient education by encouraging patients and parents to lower the indoor heating by a few degrees, spend more time outdoors and perhaps increase indoor humidity.
Humidity
The protective effects of outdoor relative humidity against eczema observed in the present study are consistent with a previous study of Spanish schoolchildren that found similar findings in relation to outdoor humidity (Suarez-Varela et al., 2008). In contrast, a study of children from International Study of Asthma and Allergies in Childhood (ISAAC) found that eczema prevalence was negatively associated with indoor relative humidity, but not outdoor relative humidity or altitude (Weiland et al., 2004). A possible explanation for the conflicting findings related to outdoor humidity is that climate factors in that study were obtained from data averaged over years to decades and published 12 years prior to the study (Pearce and Smith, 1984). Those results represent long term climate trends and not short term weather patterns that may be more likely to influence eczema prevalence. In contrast, climate factors evaluated in the present study were focused to the 1–2 years preceding questionnaire. Of note, monthly relative humidity was not consistently available for each state, which precluded determining the effects of seasonal humidity on AD prevalence.
It is likely that higher humidity protects against eczema by improving skin barrier function. Several murine studies demonstrated the harmful effects of low humidity on cellular pathways related to eczema. Prolonged exposure of mice to a dry environment resulted in increased epidermal DNA synthesis and epidermal hyperplasia (Denda et al., 1998) and higher epidermal expression of interleukin 1-alpha (Ashida et al., 2001), which were more pronounced after barrier disruption by tape stripping. Transfer of mice from a humid to dry environment resulted in a transient increase of trans-epidermal water loss and epidermal proliferation and altered distribution of lamellar bodies within strata- granulosum and corneum (Sato et al., 2002). Together, these studies suggest that higher relative humidity may improve skin barrier function and is associated with decreased eczema prevalence.. Future prospective studies are warranted to verify this point.
HDD
The present study demonstrates an association between increased HDD in all seasons and eczema prevalence. We hypothesize that the harmful effects of increased HDD on eczema are likely secondary to decreased indoor humidity from heating. This is consistent with the previous finding of an inverse association between eczema prevalence and indoor relative humidity (Weiland et al., 2004).
Temperature
The protective effects of higher temperature against eczema observed in the present study are consistent with a previous study of children from the International Study of Asthma and Allergies in Childhood (ISAAC), which found that eczema prevalence was negatively associated with mean annual temperature (Weiland et al., 2004). It is unknown whether the protective effects of temperature against eczema are related to direct effects on skin. Another possibility, as mentioned above, is that lower temperature would result in greater use of indoor heating and ultimately lower indoor humidity.
UV
The present study found that higher UV levels are associated with lower prevalence of eczema, while increased stratospheric ozone levels are associated with a higher prevalence of eczema. Monthly UV levels were not consistently available for each state, which precluded determining the effects of seasonal UV levels on eczema prevalence. Previous studies demonstrated increased respiratory and atopic disorders with increased tropospheric ozone levels (Jones, 1998; Lee et al., 2010; Schwartz, 1996; Sole et al., 2007). Other studies found an association between increased ozone levels and hospital admissions for AD and asthma (Lee et al., 2010; Schwartz, 1996). A study of a Brazilian cohort from the ISAAC Phase 3 study found an association of increased ozone with increased flexural eczema in São Paulo West, but not in 3 other cities (Sole et al., 2007). All of these studies examined the effects of tropospheric ozone which is generally regarded as potentially harmful/toxic, whereas stratospheric ozone has protective effects via filtering of ultraviolet B and C radiation 19. Ultraviolet B radiation (UVB) stimulates cutaneous synthesis of pre-vitamin D from 7-dehydrocholesterol. In fact, low serum vitamin D levels have been found in patients with AD and other atopic disorders, and vitamin D deficiency is hypothesized to contribute toward atopic disease (Frieri and Valluri, 2011; Peroni et al., 2011; Vahavihu et al., 2010). UVB also induces cutaneous photo-immunosuppression that may have both harmful effects, e.g. photoaging and carcinogenesis, and beneficial effects, e.g. suppression of inflammatory disorders (Norval and Halliday, 2011). Thus, it is possible that higher stratospheric ozone levels result in increased filtering of ultraviolet B radiation and ultimately less vitamin D synthesis and/or photo-immuno-suppression of AD.
Precipitation
The harmful effects of increased amounts of precipitation observed in the present study are likely related to decreased issued UV levels from increased cloudiness and more time spent indoors exposed to indoor heating and low relative humidity. Another possibility is that damp weather promotes the growth of molds and/or dust mites that might aggravate the disease in some cases.
Combined climate factors
Since many climate variables are correlated with each other, we also analyzed the effects of the most dominant combinations of climate variables in the US and found that residence in a state with combined high temperature, low HDD and high issued UV index was protective against eczema. While residence in a location with higher relative humidity is overall protective against eczema (see above), residence in a state with high humidity combined with high precipitation and low UV index, which are risk factors for eczema, was actually associated with increased eczema prevalence. We hypothesize that areas with rainy climate have decreased UV exposure from cloudiness and more time indoors exposed to low indoor humidity from heating.
Strengths and limitations
This study has several strengths, including being prospective, population-based, having a well-powered sample size of children with and without eczema (post-hoc power analysis of 93.8% for n=79667 subjects after exclusion criteria, assuming 10% baseline eczema probability, alpha=0.01 and ability to detect OR≥1.1), and the use of principal components analysis to examine patterns of climate variables not otherwise identified in univariate analyses. This study has potential limitations. Eczema was defined using self-report by parental questionnaire. The NSCH question for eczema asked about “eczema or any other kind of skin allergy”. This rather broad question may result in overestimates of prevalence for AD per se by inclusion of other entities such as allergic contact dermatitis but such entities are relatively uncommon compared to AD in pediatric age groups. NSCH only recorded the state of residence, but not city or county. Thus, climate variables used in the study had to be limited to statewide values, which may result in decreased accuracy of estimates of eczema odds. This study conducted at the crude geographical level of the state is subject to the ‘ecological fallacy” (Piantadosi et al., 1988). It should therefore be interpreted at the group level by state and cannot be interpreted at the individual level.
Conclusions
In conclusion, this study provides evidence of climate influences on the prevalence of eczema, including humidity, UV exposure, temperature, indoor heating and precipitation. In particular, combined high UV exposure and temperature appear to have protective effects specific to eczema, whereas combined high humidity and precipitation are associated with more eczema.
Methods
Data sources
National Survey of children’s Health (NSCH)
We used data from the 2007 NSCH survey of 91,642 households, which was designed to estimate the prevalence of various child health issues including physical, emotional, and behavioral factors. The NSCH was sponsored by the Maternal and Child Health Bureau and the U.S. Department of Health and Human Services. The National Center for Health Statistics conducted using the State and Local Area Integrated Telephone Survey (SLAITS) program with a goal of >1,800 subjects per state. The telephone numbers were chosen at random, followed by identification of the households with one or more children under the age of 18. Subsequently, one child was randomly selected for interview. The survey results were weighted to represent the population of non-institutionalized children nationally and in each state. Using the data from U.S. Bureau of the Census, weights were adjusted for age, sex, race, ethnicity, household size, and educational attainment of the most educated household member to provide a dataset that was more representative of each state’s population of non-institutionalized children less than 18 years of age. The National Center for Health Statistics of Center for Diseases Control and Prevention oversaw sampling and telephone interviews. Verbal informed consent was obtained before interview.
Climate variables
Relative humidity
Seasonal and annual statewide mean values of relative humidity (%) were downloaded from National Oceanic & Atmospheric Administration (NOAA), National Climate Data Center (NCDC) at http://www7.ncdc.noaa.gov/CDO/dataproduct. Relative humidity is a measure of water vapor in the air that is dependent on both the air temperature and pressure.
UV index, stratospheric ozone levels and probability of clear skies
To determine the effects of UV radiation on eczema prevalence, monthly and annual statewide mean values of clear sky and issued UV indices, stratospheric ozone levels (parts per billion) and percent probability of clear skies were downloaded from the NOAA, National Weather Service, Climate Prediction Center at ftp://ftp.cpc.ncep.noaa.gov/long/uv/cities. The issued UV index accounts for the cloud effects on UV transmission, while the clear sky UV index does not. UV index exposure has been categorized by the World Health Organization as low (0–2), moderate (3–5), high (6–7), very high (8– 10), and extreme (≥11). For more information about UV indices, please refer to http://www.cpc.ncep.noaa.gov/products/stratosphere/uv_index/uv_information.shtml. Since the stratospheric ozone layer filters all UVC and the majority of UVB radiation, we studied stratospheric ozone levels as a marker of UV exposure.
Temperature and Heating degree days (HDD)
Monthly and annual statewide mean values of temperatures (Degrees Fahrenheit to 10ths) and HDD (whole number) were downloaded from the NOAA, NCDC at ftp://ftp.ncdc.noaa.gov/pub/data/cirs/. Temperatures were corrected for “time-bias” as per the method of Karl et al. (Karl, 1986). Time-bias correction adjusts the mean temperature values over a 24-hour period from each individual station to coincide with the calendar day. HDD is a statewide population-weighted measure of energy demand to heat indoor structures by one degree for one day using a baseline temperature of 65 degrees Fahrenheit. For example, a value of 3 would mean that the outdoor temperature that day would require buildings to use enough energy to heat their buildings by 3 degrees.
Eczema prevalence
Prevalence of eczema, the primary outcome of the study, was determined using the NSCH question, “During the past 12 months, have you been told by a doctor or other health professional that (child) had eczema or any kind of skin allergy?” This is referred to as eczema throughout the manuscript. To limit the effect that healthcare access may have on the results, we excluded all subjects who responded “none” or “don’t know” to the question, “How many times did (child) see a doctor, nurse, or other health care provider for preventive medical care such as a physical exam or well-child checkup in the past 12 months?”.
Data processing and statistical methods
All data processing and statistical analyses were performed in SAS version 9.2. The above mentioned climate variables were limited to 2006–2007 and were chosen for each subject of the NSCH by the current state of residence. In scenarios where there were climate observations for multiple cities within a state, the mean value of all the cities was used. Mean annual values for variables was used for statistical modeling.
Analyses of survey responses were performed using SURVEY procedures. Univariate and multivariate associations were tested by logistic regression. The dependent binary variable was eczema and the independent variables included the abovementioned climate factors tested individually in univariate models. Age, sex, race/ethnicity, and household income were included in multivariate models because of significant confounding and/or effect modification. Complete data analysis was performed, i.e. subjects with missing data were excluded. Linear interaction terms between age, sex, race/ethnicity, and household income were tested and included in the final models if significant (P<0.05). All population estimates were determined using the predefined sampling weights for the NSCH.
Relative humidity, UV index, temperature, and HDD were highly correlated. Therefore, principal component analysis (PCA) with varimax rotation was used to estimate the combined effects of these climate variables (Kaiser, 1958). PCA was used to determine the best combination and weighting of climate variables in order to best explain how they are correlated. Factors were retained if eigenvalue >1, proportion of variance accounted for >10% and loading value >0.4. Retained factors represent the dominant combinations of these climate variables occurring in the US. Logistic regression was then performed using factor scores from the retained factors to determine the odds of eczema under these common climate conditions.
Correction for multiple dependent tests (k = 65) with the approaches of Benjamini and Hochberg (Benjamini and Hochberg, 1995) yielded a critical P-value of 0.023.
Supplementary Material
Acknowledgments
We would like to thank Courtney A McKenna, Continuum Health Partners for her design of Figure 1.
Funding Support: This project was supported in part by a Mentored Patient-oriented Research Career Development Award (K23)–award number K23AR057486 from the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health.
Abbreviations used
- CI
confidence interval
- OR
odds ratio
- aOR
adjusted odds ratio
Footnotes
Manuscript authorship: JI Silverberg, J Hanifin and E Simpson
Data analysis and interpretation: JI Silverberg, J Hanifin and E Simpson
Statistical analysis: JI Silverberg
Financial disclosures: None.
Conflicts of Interest: The authors report no conflicts of interest.
Bibliography
- [Accessed April 8, 2012]; < http://www.ozonelayer.noaa.gov/science/basics.htm>.
- Ashida Y, Ogo M, Denda M. Epidermal interleukin-1 alpha generation is amplified at low humidity: implications for the pathogenesis of inflammatory dermatoses. Br J Dermatol. 2001;144:238–243. doi: 10.1046/j.1365-2133.2001.04007.x. [DOI] [PubMed] [Google Scholar]
- Benjamini Y, Hochberg Y. Controlling the false discovery rate - a practical and powerful approach to multiple testing. J R Stat Soc Series B Stat Methodol. 1995;57:289–300. [Google Scholar]
- Chernosky ME. Pruritic skin disease and summer air conditioning. JAMA. 1962;179:1005–1010. doi: 10.1001/jama.1962.03050130009003. [DOI] [PubMed] [Google Scholar]
- Denda M, Sato J, Tsuchiya T, Elias PM, Feingold KR. Low humidity stimulates epidermal DNA synthesis and amplifies the hyperproliferative response to barrier disruption: implication for seasonal exacerbations of inflammatory dermatoses. J Invest Dermatol. 1998;111:873–878. doi: 10.1046/j.1523-1747.1998.00364.x. [DOI] [PubMed] [Google Scholar]
- Frieri M, Valluri A. Vitamin D deficiency as a risk factor for allergic disorders and immune mechanisms. Allergy Asthma Proc. 2011;32:438–444. doi: 10.2500/aap.2011.32.3485. [DOI] [PubMed] [Google Scholar]
- Gaul LE, Underwood GB. Relation of dew point and barometric pressure to chapping of normal skin. J Invest Dermatol. 1952;19:9–19. doi: 10.1038/jid.1952.61. [DOI] [PubMed] [Google Scholar]
- Jones AP. Asthma and domestic air quality. Soc Sci Med. 1998;47:755–764. doi: 10.1016/s0277-9536(98)00151-8. [DOI] [PubMed] [Google Scholar]
- Kabir Z, Manning PJ, Holohan J, Goodman PG, Clancy L. Prevalence of symptoms of severe asthma and allergies in Irish school children: an ISAAC protocol study, 1995&3x02013;2007. International journal of environmental research and public health. 2011;8:3192–3201. doi: 10.3390/ijerph8083192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaiser H. The varimax criterion for analytic rotation in factor analysis. Psychometrika. 1958;23:187–200. [Google Scholar]
- Karl TR, Williams Claude N, Young Pamela J, Wendland Wayne M. A Model to Estimate the Time of Observation Bias Associated With Monthly Mean Maximum, Minimum and Mean Temperatures for the United States. Journal of Climate and Applied Meteorology. 1986 [Google Scholar]
- Langan SM, Bourke JF, Silcocks P, Williams HC. An exploratory prospective observational study of environmental factors exacerbating atopic eczema in children. Br J Dermatol. 2006;154:979–980. doi: 10.1111/j.1365-2133.2006.07153.x. [DOI] [PubMed] [Google Scholar]
- Lee JT, Cho YS, Son JY. Relationship between ambient ozone concentrations and daily hospital admissions for childhood asthma/atopic dermatitis in two cities of Korea during 2004–2005. Int J Environ Health Res. 2010;20:1–11. doi: 10.1080/09603120903254033. [DOI] [PubMed] [Google Scholar]
- Norval M, Halliday GM. The consequences of UV-induced immunosuppression for human health. Photochem Photobiol. 2011;87:965–977. doi: 10.1111/j.1751-1097.2011.00969.x. [DOI] [PubMed] [Google Scholar]
- Pearce EA, Smith CG. The Times Books world weather guide : a city-by-city guide that will enable you to forecast the weather you can expect in any part of the world at any time of the year. New York, N.Y.: Times Books; 1984. p. 480. [Google Scholar]
- Peroni DG, Piacentini GL, Cametti E, Chinellato I, Boner AL. Correlation between serum 25-hydroxyvitamin D levels and severity of atopic dermatitis in children. Br J Dermatol. 2011;164:1078–1082. doi: 10.1111/j.1365-2133.2010.10147.x. [DOI] [PubMed] [Google Scholar]
- Piantadosi S, Byar DP, Green SB. The ecological fallacy. Am J Epidemiol. 1988;127:893–904. doi: 10.1093/oxfordjournals.aje.a114892. [DOI] [PubMed] [Google Scholar]
- Rajka G. Atopic dermatitis Correlation of environmental factors with frequency. Int J Dermatol. 1986;25:301–304. doi: 10.1111/j.1365-4362.1986.tb02249.x. [DOI] [PubMed] [Google Scholar]
- Rycroft RJ, Smith WD. Low humidity occupational dermatoses. Contact Dermatitis. 1980;6:488–492. doi: 10.1111/j.1600-0536.1980.tb05572.x. [DOI] [PubMed] [Google Scholar]
- Sato J, Denda M, Chang S, Elias PM, Feingold KR. Abrupt decreases in environmental humidity induce abnormalities in permeability barrier homeostasis. J Invest Dermatol. 2002;119:900–904. doi: 10.1046/j.1523-1747.2002.00589.x. [DOI] [PubMed] [Google Scholar]
- Schwartz J. Air pollution and hospital admissions for respiratory disease. Epidemiology. 1996;7:20–28. doi: 10.1097/00001648-199601000-00005. [DOI] [PubMed] [Google Scholar]
- Selnes A, Nystad W, Bolle R, Lund E. Diverging prevalence trends of atopic disorders in Norwegian children. Results from three cross-sectional studies. Allergy. 2005;60:894–899. doi: 10.1111/j.1398-9995.2005.00797.x. [DOI] [PubMed] [Google Scholar]
- Sole D, Camelo-Nunes IC, Wandalsen GF, Pastorino AC, Jacob CM, Gonzalez C, et al. Prevalence of symptoms of asthma, rhinitis, and atopic eczema in Brazilian adolescents related to exposure to gaseous air pollutants and socioeconomic status. J Investig Allergol Clin Immunol. 2007;17:6–13. [PubMed] [Google Scholar]
- Suarez-Varela MM, Garcia-Marcos Alvarez L, Kogan MD, Gonzalez AL, Gimeno AM, Aguinaga Ontoso I, et al. Climate and prevalence of atopic eczema in 6- to 7-year-old school children in Spain. ISAAC phase III. Int J Biometeorol. 2008;52:833–840. doi: 10.1007/s00484-008-0177-0. [DOI] [PubMed] [Google Scholar]
- Vahavihu K, Ala-Houhala M, Peric M, Karisola P, Kautiainen H, Hasan T, et al. Narrowband ultraviolet B treatment improves vitamin D balance and alters antimicrobial peptide expression in skin lesions of psoriasis and atopic dermatitis. Br J Dermatol. 2010;163:321–328. doi: 10.1111/j.1365-2133.2010.09767.x. [DOI] [PubMed] [Google Scholar]
- Weiland SK, Husing A, Strachan DP, Rzehak P, Pearce N. Climate and the prevalence of symptoms of asthma, allergic rhinitis, and atopic eczema in children. Occup Environ Med. 2004;61:609–615. doi: 10.1136/oem.2002.006809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wuthrich B. Clinical aspects, epidemiology, and prognosis of atopic dermatitis. Ann Allergy Asthma Immunol. 1999;83:464–470. doi: 10.1016/S1081-1206(10)62852-9. [DOI] [PubMed] [Google Scholar]
- Wuthrich B, Schmid-Grendelmeier P. The atopic eczema/dermatitis syndrome. Epidemiology, natural course, and immunology of the IgE-associated ("extrinsic") and the nonallergic ("intrinsic") AEDS. J Investig Allergol Clin Immunol. 2003;13:1–5. [PubMed] [Google Scholar]
- Zar HJ, Ehrlich RI, Workman L, Weinberg EG. The changing prevalence of asthma, allergic rhinitis and atopic eczema in African adolescents from 1995 to 2002. Pediatr Allergy Immunol. 2007;18:560–565. doi: 10.1111/j.1399-3038.2007.00554.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.