Summary
This paper reviews the philosophical origins, current scientific evidence, and clinical promise of yoga and mindfulness as complementary therapies for addiction. Historically, there are eight elements of yoga that, together, comprise ethical principles & practices for living a meaningful, purposeful, moral and self-disciplined life. Traditional yoga practices, including postures and meditation, direct attention towards one’s health, while acknowledging the spiritual aspects of one’s nature. Mindfulness derives from ancient Buddhist philosophy, and mindfulness meditation practices, such as gentle Hatha yoga and mindful breathing, are increasingly integrated into secular health care settings. Current theoretical models suggest that the skills, insights, and self-awareness learned through yoga and mindfulness practice can target multiple psychological, neural, physiological, and behavioral processes implicated in addiction and relapse. A small but growing number of well-designed clinical trials and experimental laboratory studies on smoking, alcohol dependence, and illicit substance use support the clinical effectiveness and hypothesized mechanisms of action underlying mindfulness-based interventions for treating addiction. Because very few studies have been conducted on the specific role of yoga in treating or preventing addiction, we propose a conceptual model to inform future studies on outcomes and possible mechanisms. Additional research is also needed to better understand what types of yoga and mindfulness-based interventions work best for what types of addiction, what types of patients, and under what conditions. Overall, current findings increasingly support yoga and mindfulness as promising complementary therapies for treating and preventing addictive behaviors.
Introduction
According to the World Health Organization, the global burden of disease attributable to alcohol and illicit drug abuse amounts to over 5% of the total burden of disease and the harmful use of alcohol claims 2.5 million lives per year.1 There is growing concern regarding substance use disorders as relapse rates continue to remain as high as 80-95% in the first year after alcohol or tobacco cessation.2-3 Although conventional methods for relapse prevention can be somewhat successful, complementary therapies like yoga and mindfulness meditation are increasingly recognized for their ability to enhance recovery from addiction, in part by targeting stress-related cognitions, emotions, and behavioral urges such as craving.4-8
A systematic review conducted in 2009 concluded that although there was promising preliminary evidence for the safety and clinical efficacy of mindfulness meditation training for substance use disorders, conclusive data were lacking due to poor trial quality and other methodological concerns like small sample sizes.9 We are not aware of a review that has specifically addressed yoga as a potential complementary therapy for treating addiction or helping to prevent relapse. The specific objective of this paper, therefore, is to examine the current theoretical and empirical basis for yoga and mindfulness meditation as part of an integrative approach for treating and preventing the most common and costly addictions, namely smoking, alcohol dependence and illicit substance use.
We first describe the philosophy of yoga, with a focus on the ways in which yogic breathing, postures, meditation, concentration, and moral and ethical foundations can increase resilience to stress and decrease vulnerability to addiction. We next discuss the relationship between addiction and stress as a conceptual foundation for how yoga and mindfulness may help treat or preempt addictive behaviors, including associated patterns of thinking, emotional processing, physiology, and behavior. Then, we present three exemplary lines of converging clinical research that point to promising clinical outcomes and potentially shared mechanisms of therapeutic change. We conclude by presenting a conceptual model that highlights the clinical utility of integrating traditional elements of Ashtang yoga and mindfulness meditation as a way to break the vicious cycle of stress, negative emotions, craving, drug seeking behavior, and withdrawal.
Philosophy of Yoga
The Hindu philosophy of Yoga as outlined by sage Patanjali in second century B.C is based on the eight limbs of Ashtang yoga, comprised of yamas (ethical disciplines), niyamas (individual observances), asana (posture), pranayama (breath control), pratyahara (withdrawal of senses), dharana (concentration), dhyana (meditation), and samadhi (self-realization or enlightenment).10 Contrary to popular Western beliefs and modernization, the ancient practice of yoga involves more than just the asanas (postures) or dhyana (meditation). These eight limbs are comprised of ethical principles for living a meaningful and purposeful life; serving as a prescription for moral and ethical conduct and self-discipline, they direct attention towards one’s health while acknowledging the spiritual aspects of one’s nature.11
In the Western scientific literature, yoga is a general term that encompasses breathing techniques, postures, strengthening exercises, and meditation.12 The most common forms of yoga practiced in the West are the physical postures and the breathing practices of Hatha yoga and meditation.13 Hatha yoga is further categorized the Iyengar, Kundalini, Bikram, Ananda, Vivnoya and Anusara style.14 The breathing techniques of Hatha yoga focus on conscious prolongation of inhalation, breath retention and exhalation.11 Although there is focus on breath-work, and meditation is a component to Hatha yoga, Hatha yoga is more physical in nature than the other various forms of yoga.15 For example, asanas are physical postures which stretch and strengthen different parts of the body, massaging and bringing fresh blood to the internal organs while rejuvenating the nervous system and lubricating the joints, muscles and ligaments.16 Practitioners scan their bodies to become aware of stiff muscles, which they can then loosen until the posture is correctly attained.17 The abdominal breathing technique and focus of awareness onto the body are the mental component, with the focus of awareness to the present asana and physical experience helping to center the self in the present moment.17 This kind of present-focused sensory awareness resonates with the Buddhist philosophy of mindfulness meditation, which is the foundation of a secular, widely available course known as Mindfulness-Based Stress Reduction (MBSR).18
A more meditative form of yoga is called the Raja yoga or “Union by mental mastery.”17 According to Swami Vivekananda, the term “Raja yoga” means the method of mental concentration which involves the ability to check and bring the mind under control through the practice of the eight steps described by the sage Patanjali in his text “Yoga Sutras”.19 One of these steps is Pranayama or breath control. The three sorts of motion of Pranayama are, one by which we draw the breath in, another by which we throw it out, and the third action in which the breath is held in the lungs, or stopped from entering the lungs.19 Pranayama is known to increase parasympathetic tone, decrease sympathetic tone, improve cardiovascular and respiratory functions, decrease the effects of stress and strain on the body, and improve physical and mental health.20-22
Integrated yoga practice traditionally involves meditation, exercise and spiritual teaching; the integrated form was found to be more beneficial for physical, psychological and spiritual well-being than yoga practiced primarily as a form of exercise.23 Smith23 also reported that cortisol levels decreased by approximately 31% in people who practiced integrative yoga as compared to those who practiced yoga as a form of physical exercise. This study suggests that practicing yoga with the intention that it is part of one’s spirituality may be related to better outcomes.
Meditation is the art of efficient and adaptive management of neurobehavioral energy, with total engagement or disengagement of conscious mental processes and sensory awareness, depending on the type of meditation practice. Meditation practice can be generally categorized as either open monitoring or focused attention.24 In both of these states, one can experience spontaneous, unitive being without a sense of ego, memory, or time.25 The relaxation response achieved after yoga may confer the ability to face situations in a relaxed state of mind and perform tasks with greater ease and effortlessness.26 This concept is reflected in the secular teachings of mindfulness meditation in academic, medical, and clinical settings in Western countries, including the United States, Canada, and the United Kingdom.27-30
In addition to cultivating present-focused attention, increased sensory awareness, enhanced concentration, and physiological relaxation, yoga and mindfulness meditation can also shift one’s concept and understanding of the self. When the mind is undirected and assumes its original unmodified state, the self is expressed as a narrative, self-centered experience.31 Modern neuroscience has identified the functional neuroanatomy of the tendency to narrowly focus on oneself under natural, mind wandering conditions; these neural substrates have been termed the “default mode network” (DMN).32 The DMN is comprised of a group of functionally connected brain regions spanning several cortices, including the prefrontal, parietal, and temporal cortices, as well as the anterior cingulate cortex, and several subcortical regions including the amygdala and hippocampus, among others.32 Neuroimaging research has recently shown that hypoactive prefrontal activation coupled with hyperactive limbic system activation represents altered DMN function that could serve as a brain-based biomarker for vulnerability to mental disorders, including depression and substance abuse.33-36 Some of the latest clinical and mechanistic research on the DMN has demonstrated that DMN activity is modifiable through meditation practice. Specifically, yoga meditation has been associated with greater functional connectivity between the DMN and other distributed brain networks involved in attention, self-referential processing, and affective responses, and mindfulness meditation has been shown to increase somatosensory processing, decrease cognitive elaboration associated with the narrative self, and diminish emotional reactivity in the limbic system.37-40
The latest contemplative neuroscience data, therefore, show that yoga meditation and mindfulness meditation– both of which engage sensory, non-conceptual awareness – can target multiple brain regions, and the functional connections between them, that subserve addictive behaviors. Thus, yoga and mindfulness meditation, which were developed thousands of years ago, are increasingly recognized as a form of mind-body medicine that can potentially address the physical, psychological, and spiritual aspects pertinent to addiction.26
Addiction and Stress
The global burden of disease attributable to alcohol and illicit drug use amounts to over 5% of the total burden of disease.41 Around 27 million people worldwide suffer from severe drug problems with a prevalence of about 2 percent in the U.S.42 Tobacco consumption was responsible for 100 million deaths in the last century and despite intense efforts over the last 2 decades to control tobacco use, 1.2 billion individuals continue to smoke.42 The 12 month rate of relapse following alcohol or tobacco cessation attempts is usually 80-95%; therefore, preventing relapse or minimizing its extent is a pre-requisite for any attempt to facilitate successful, long-term changes in addictive behavior.2-3, 42
Stress is the subjective experience of negative emotional states coupled with physiological activation that often produces uncomfortable physical sensations, including muscle tension, elevated heart rate and blood pressure, and gastrointestinal distress.43-44 In the context of smoking, for example, symptoms such as perceived stress, negative affect, and physical symptoms of withdrawal have been shown to increase the individual’s risk for relapse.45 Relapse usually occurs within the first week of quitting and is preceded by increases in withdrawal symptoms, including craving for cigarettes, distress and reductions in positive affect.46 Stress is also known to precipitate alcohol relapse, through a constellation of interrelated cognitive, emotional, physiological, and behavioral mechanisms.47 Some of these mechanisms include attentional bias toward alcohol-related cues, thought suppression, poor emotion regulation skills, and emotional reactivity leading to habitual drug-seeking behavior.47
Conventional behavioral approaches to relapse prevention aim to address numerous determinants of relapse, including (a) physical symptoms of withdrawal, (b) cognitive processes like craving, self-efficacy, outcome expectancies, and motivation, (c) coping behaviors, including adaptive and maladaptive coping styles, (d) emotional states, including how to self-regulate positive and negative affect, (e) interpersonal dynamics, including peer pressure and relationship conflict, and (f) situational or contextual factors that cue or elicit cravings.7 As reviewed by others, meditative approaches are now being developed as complementary therapies to augment conventional treatment by directly targeting mindless, automatic mental and behavioral processes, like craving, through cultivating greater mindfulness.8, 35, 48
The following section briefly describes three current exemplary clinical research programs. Each program integrates theory-driven models of addiction and methodologically rigorous science, with real-world practice implications for meditation and yoga as potential complementary therapies.
I. Mindfulness-Based Relapse Prevention for Alcohol and Illicit Substance Abuse
Mindfulness-Based Relapse Prevention (MBRP) is an 8-week, group-based, psychoeducational intervention that combines traditional cognitive-behavioral relapse prevention strategies with meditation training and mindful movement. The primary goal of MBRP is to help patients tolerate uncomfortable states, like craving, and to experience difficult emotions, like anger or fear, without automatically reacting.48 MBRP, which is delivered after intensive stabilization of substance use, is informed by the standard, 8-week Mindfulness-Based Stress Reduction (MBSR) program originally developed by Kabat-Zinn.27 The original MBSR program was designed to help patients with chronic pain and other chronic health conditions face stress, pain & illness with greater awareness, skill, and compassion.18
Whereas the original MBSR program includes 6 weeks of Hatha yoga, the MBRP program teaches “mindful movement” only once, in Session 5 (Sarah Bowen, personal communication, November 26, 2012). In the MBRP model, mindful movement includes light stretching and other basic, gentle movements. Each movement is guided with physical safety and respect for the body at the forefront, and patients are instructed to stay with the movement as it happening, observing physical sensations of moving and stretching, while also noticing striving, thoughts, and judgments about the body. In MBRP, formal asanas are not taught because instructors are typically not trained in yoga, clients recovering from addiction often have physical limitations that preclude performing traditional asanas, and formal yoga can be seen as inaccessible.
A recently published efficacy trial on 168 adults with substance use disorders found that MBRP, compared to a treatment-as-usual control group, resulted in significantly lower rates of substance use at 2-month follow-up.49 Moreover, the trial found that decreased substance use following MBRP could be explained by a weakened association between depressive symptoms and craving. These findings provided empirical support for training in mindfulness meditation and mindful movement in targeting known cognitive-affective risk mechanisms underlying relapse. Because other research has established that areas of the brain implicated in the pathophysiology of addiction, such as the prefrontal cortex and amygdala, can be influenced by mindfulness training, it is plausible that meditation and mindful movement or yoga could complement conventional care by mitigating the highly conditioned chain of cognitive, emotional, and physiological processes known to predict relapse of addictive behavior.48 Insofar as greater mindfulness mediates reduced craving following MBRP50, it is important to note that home meditation between sessions, along with a strong therapeutic alliance between participants and the group instructors, are important predictors of initial increases in mindfulness after the 8-week MBRP program. 51
II. Mindfulness Training for Smoking Cessation
Brewer and colleagues have developed a well-conceived conceptual model that proposes how mindfulness training, without yoga, could target shared psychological and neurobiological processes that cut across substance use disorders and depression.35-36 Similar to the theoretical model underlying MBRP, mindfulness training for smoking cessation hypothesizes a number of interrelated therapeutic mechanisms. These mechanisms include regulating attention, cultivating an attitude of acceptance & non-judgment, and developing a specific set of meta-cognitive skills characterized by the ability to observe and discriminate one’s inner experience of thoughts, feelings, and physical sensations with a sense of equanimity. Together, these core mindfulness skills and perspectives are expected to support smokers in quitting by helping them decrease avoidance, tolerate unpleasant withdrawal symptoms, and unlearn highly conditioned stimulus-response patterns by deliberately observing yet not reacting to impermanent feelings of stress or discomfort. A recently published trial on a group of 88 smokers found that eight sessions of mindfulness training, delivered twice per week over four weeks, resulted in greater reduction in cigarette use compared to the widely used American Lung Association Freedom From Smoking program, with a significantly better abstinence rate 17-weeks after the training ended.52 Those results extended promising pilot data from Davis and colleagues, who reported a 56% biologically confirmed abstinence rate six weeks after study participants quit smoking toward the end of a slightly modified, 8-week MBSR course tailored for smokers.53 The results of a prior treatment development study by Brewer and colleagues suggested that mindfulness training, compared to conventional cognitive-behavioral therapy (CBT), specifically reduced psychological and physiological reactivity to stress provocation.54 Similar to results from the MBRP observational study reported above51, the pre-post observational study of MBSR to aid smoking cessation also found a significant positive correlation between compliance with home meditation practice and smoking abstinence.53 One RCT on Vinyasa style yoga as a complementary therapy for smoking cessation is currently underway; that trial is comparing yoga (1-hr/wk) to a contact-control wellness program (1-hr/wk) that does not include yoga.45 Both yoga and the wellness control groups will also receive group-based cognitive behavioral therapy (CBT) for smoking cessation, delivered separate to the different study arms. Finally, there is also some initial evidence that mindfulness-based coping appears to produce equivalent effects on reducing smoking compared to suppression-based coping, but with additional beneficial effects on other salient psychological outcomes linked to quitting and relapse, including lower levels of negative affect, depressive symptoms, and self-reported nicotine dependence.55
III. Mindfulness Oriented Recovery Enhancement
Mindfulness Oriented Recovery Enhancement (MORE) is a 10-session, group-based, psychoeducational intervention designed by Garland to disrupt cognitive, affective, and physiological mechanisms implicated in alcohol dependence.56-57 As noted by Garland57, MORE is adapted from the Mindfulness-Based Cognitive Therapy (MBCT) for Depression treatment manual58, tailored for addiction. Although MORE does not include yoga, it does include most other mindfulness meditation practices that are typically included as part of MBSR and MBCT, including mindful breathing, body scan, mindfulness of perceptions & sensations, mindful walking, and compassion meditation (loving-kindness, or metta). Like MBRP and mindfulness training for smoking cessation, MORE also includes a focus on meditative approaches to coping with cravings (e.g., “urge surfing”), as well as education & training about how to identify and skillfully change, or mindfully let be, mental processes like thought suppression, aversion, and attachment – all of which are theoretically and phenomenologically part of alcohol dependence and other forms of addiction.47 A novel aspect of MORE is that, unlike MBSR or its off-shoots like MBRP, MORE does explicitly address spirituality. Specifically, MORE participants, in Session 9, discuss interdependence, meaning, and spirituality, and engage in a guided meditation on interdependence. Thus, MORE directly provides some training in self-transcendence – a possible psychological mechanism of mindfulness training.59
A pilot RCT of 37 alcohol dependent adults from a residential therapeutic community who completed the MORE program found that, compared to an evidence-based support group, MORE produced a number of superior outcomes, including reduced stress and thought suppression, increased physiological recovery from alcohol cues indexed by heart rate variability during a laboratory task, and decreased alcohol attentional bias.56 Garland is now working to replicate and extend the outcomes & underlying mechanisms of MORE in patients with chronic pain who are at risk for prescription opioid dependence.60
Finally, one new clinical study on autonomic changes during several distinct forms of ancient yoga meditation found that the greatest reduction of sympathetic nervous system (SNS) activity and the greatest activation of parasympathetic nervous system (PNS) activity occurred during the state of effortless meditation (dhyana).61 This finding is relevant because modern theories of mindfulness training, as described above, presume that practitioners will learn to better self-regulate stress physiology, largely mediated by the SNS, and the relaxation response, primarily meditated by the vagus nerve and PNS. Additionally, most mindfulness-based interventions offered in health care settings today emphasize cultivating receptive awareness (also known as open monitoring, or mindful awareness), with somewhat less emphasis given to prolonged periods of deeply focused, single-pointed concentration.
In summary, the ancient philosophies of yoga and mindfulness as applied to addiction are supported by recent scientific evidence from well-designed clinical trials and experimental laboratory paradigms. Exemplary research across multiple research programs now demonstrates that mindfulness-based interventions can target clinically relevant measures of psychological, biological, and behavioral functioning, all of which are implicated in the pathophysiology of addiction.
Since the three models described above do not include traditional yoga practice, the possible benefit of yoga for addiction remains to be studied. In order to guide future research, we propose a theoretical model that integrates traditional yoga practice with current knowledge of addiction.
Yoga, Mindfulness, and Addiction – A Union of Mind, Body and Spirit
Yoga and mindfulness teachings share a fundamental belief in “mindful” awareness of experiences and emotions as they arise, without having to change them. Addictions are born as a result of “mindless” states involving escapist attitudes, automatic thinking, emotional reactivity and social isolation. The sense of loss and emptiness that occurs with addiction is often filled by nicotine, alcohol or other substances and the loss-addiction cycle develops. Figure 2 integrates current theory and scientific knowledge to illustrate how practicing traditional elements of yoga and mindfulness at any point in the vicious cycle of substance use can help steady attention, strengthen concentration, enhance emotion regulation, and facilitate personal & spiritual growth through self-observation. Whereas simply doing yoga postures (asanas) or practicing meditation (dhyana) or breath control (pranayama) alone can help regulate stress and unhook people from substance use impulses in the moment, we propose that optimal treatment and prevention outcomes may come from utilizing the full system of adaptive attitudes, perspectives, and self-regulation skills embodied by traditional Hatha yoga (Ashtang yoga) and mindfulness meditation. Future studies may benefit from exploring whether yoga as part of a spiritual practice may produce better outcomes than practicing yoga and meditation in a secular form.
Figure 2.
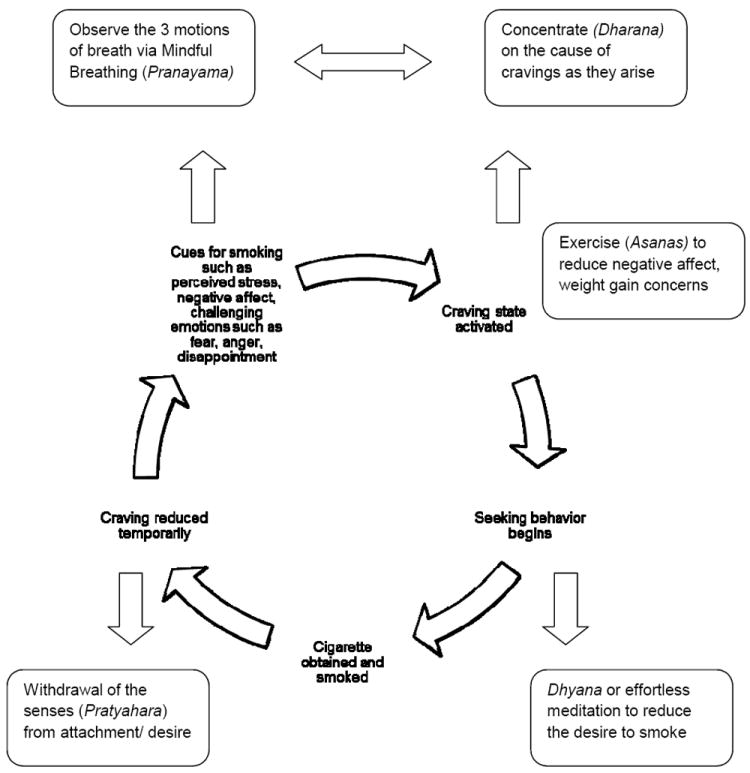
Application of Ashtang Yoga to the Vicious Cycle of Craving, Smoking and Withdrawal
Although clinical trial quality and experimental tests of therapeutic mechanisms have improved since a systematic review was published in 20099, this literature still has a number of gaps & limitations. For instance, a key criterion to qualify as an empirically supported behavioral treatment is that initial findings, typically published by treatment developers, need to be replicated by independent researchers, using the same experimental design, patient sample, and intervention that was used in the initial trial.62 In addition, the specific therapeutic value of yoga – as a whole system (Figure 1), or as stand-alone elements – in accounting for treatment outcomes and hypothesized mechanisms is unclear. Finally, what kinds of patients, with what types(s) of addiction are most likely to benefit from yoga and mindfulness training? Are there gender differences in perceived credibility and/or treatment response? Are treatment effects consistent or disparate across other demographic subgroups, including age, race, ethnicity, level of education, and/or religious beliefs? Can the clinical response to yoga or mindfulness-based interventions for addiction treatment and recovery be predicted, in part, by patient preferences or the level of positive expectancy (placebo effect)? Similarly, does pursuing yoga or meditation as a form of spiritual growth influence outcomes or underlying mechanisms of therapeutic change compared to viewing these practices solely as stress reduction or relaxation techniques? Answers to these kinds of questions will continue to grow the evidence-base for yoga and mindfulness as complementary therapies for treating addiction and preventing relapse in an era of increasingly “personalized” medicine.
Figure 1.
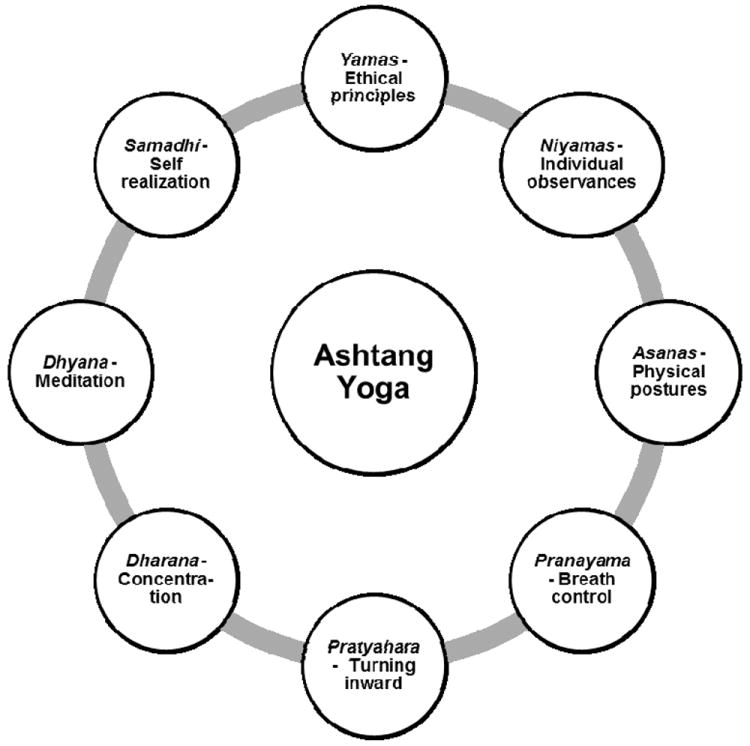
Eight Elements of Ashtang Yoga
Finally, in learning yoga, it is possible that some persons with addiction could become addicted to their guru (teacher). From the perspective of traditional yoga, however, the purpose of the “Guru” is to plant the seeds of knowledge into the minds of the students, rather than insist that his/her students accept their teachings blindly63. On the contrary, the aim of traditional yoga is to look inward (Pratyahara) and to recognize the “Guru” within oneself when cravings arise, being mindful of this state as it develops. Because yoga intends to develop insight and inner resources for coping effectively with stress, upsetting emotions, cravings, and impulses, the Yogic philosophy offers a holistic approach to addictions – an approach that could be integrated with conventional therapies.
In conclusion, mindfulness-based interventions, some of which include yoga, have sound conceptual underpinnings and growing empirical support for enhancing addiction treatment, prevention, and recovery. Future studies are needed to better understand individual differences in treatment response, and to test whether underlying psychological, biological, and behavioral mechanisms are shared or distinct across different types of addiction. Considering the state of the science and the philosophical origins of yoga and mindfulness64, we propose that a whole-system approach (Figure 2) can be used to break the cycle of stress, negative emotions, and addictive behavior by creating a sense of self-awareness, self-control, and self-realization.
Table 1.
Core Qualities of Mindlessness vs. Mindfulness
| Mindlessness | Mindfulness |
|---|---|
| Scattered attention | Steady attention |
| Automatic | Deliberate intention |
| Reactivity | Equanimity |
| Lack of awareness | Rooted in awareness |
| Escape the present | Inhabit the present |
| Self | Non-self |
| Thinking mode | Sensory mode |
| Habitual | Chosen |
| Harsh judgments & criticism | Non-judging & compassionate |
| Isolation | Connection |
Acknowledgments
JMG was supported in preparing this manuscript by Grant No. R00 AT004945 from the National Center for Complementary & Alternative Medicine (NCCAM). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health (NIH).
Footnotes
Conflict of interest statement: None declared
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.World Health Organization (WHO), Global Health Observatory (GHO) [8/31/2012]; Available at: http://www.who.int/gho/substance_abuse/en/index.html.
- 2.Brandon TH, Vidrine JI, Litvin EB. Relapse and relapse prevention. Annu Rev Clin Psychol. 2007;3:257–284. doi: 10.1146/annurev.clinpsy.3.022806.091455. [DOI] [PubMed] [Google Scholar]
- 3.Miller WR, Westerberg VS, Harris RJ, Tonigan JS. What prevents relapse? Prospective testing of antecedent models. Addiction. 1996;91(Suppl):S155–172. [PubMed] [Google Scholar]
- 4.Dakwar E, Levin FR. The emerging role of meditation in addressing psychiatric illness, with a focus on substance use disorders. Harv Rev Psychiatry. 2009;17(4):254–267. doi: 10.1080/10673220903149135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fortney L, Taylor M. Meditation in medical practice: A review of the evidence and practice. Prim Care Clin Office Pract. 2010;37(1):81–90. doi: 10.1016/j.pop.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 6.Marcus MT, Zgierska A. Mindfulness-Based Therapies for Substance Use Disorders: Part 1. Subst Abus. 2009;30(4):263. doi: 10.1080/08897070903250027. Editorial. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Witkiewitz K, Marlatt GA. Relapse Prevention for Alcohol and Drug Problems: That Was Zen, This Is Tao. American Psychologist. 2004;59(4):224–235. doi: 10.1037/0003-066X.59.4.224. [DOI] [PubMed] [Google Scholar]
- 8.Witkiewitz K, Marlatt GA, Walker D. Mindfulness-Based Relapse Prevention for alcohol and substance use disorders. Journal of Cognitive Psychotherapy. 2005;19(3):211–228. [Google Scholar]
- 9.Zgierska A, Rabago D, Chawla N, Kushner K, Koehler R, Marlatt GA. Mindfulness meditation for substance use disorders: A systematic review. Subst Abus. 2009;30(4):266–294. doi: 10.1080/08897070903250019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bonura KB. The psychological benefits of yoga practice for older adults: evidence and guidelines. Int J Yoga Therap. 2011;(21):129–42. [PubMed] [Google Scholar]
- 11.Woodyard C. Exploring the therapeutic effects of yoga and its ability to increase quality of life. Int J Yoga. 2011;4(2):49–54. doi: 10.4103/0973-6131.85485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ospina MB, Bond K, Karkhaneh M, et al. Meditation practices for health: The state of the research. Evid Rep Technol Assess. 2007;(155):1–263. [PMC free article] [PubMed] [Google Scholar]
- 13.Collins C. Yoga: intuition, preventive medicine, and treatment. J Obstet Gynecol Neonatal Nurs. 1998;27(5):563–8. doi: 10.1111/j.1552-6909.1998.tb02623.x. [DOI] [PubMed] [Google Scholar]
- 14.Li AW, Goldsmith CW. The effects of yoga on anxiety and stress. Altern Med Rev. 2012;17:21–35. [PubMed] [Google Scholar]
- 15.Iyenger BKS. Light on Yoga: Yoga Dipika. New York, NY: Schocken Books, Inc.; 2001. [Google Scholar]
- 16.Arora S, Bhattacharjee J. Modulation of immune responses in stress by Yoga. Int J Yoga. 2008;1(2):45–55. doi: 10.4103/0973-6131.43541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brisbon NM, Lowery GA. Mindfulness and levels of stress: A comparison of beginner and advanced Hatha yoga practitioners. J Relig Health. 2011;50(4):931–41. doi: 10.1007/s10943-009-9305-3. [DOI] [PubMed] [Google Scholar]
- 18.Kabat-Zinn J. Mindfulness-based interventions in context: Past, present and future. Clin Psychol Sci Prac. 2003;10(2):144–156. [Google Scholar]
- 19.Vivekananda S. Raja Yoga. Calcutta, India: Advaita Ashram; 1947. p. 232. [Google Scholar]
- 20.Bhargava R, Gogate MG, Mascarenhas JF. Autonomic responses to breath holding and its variations following pranayama. Indian J Physiol Pharmacol. 1988;42:257–64. [PubMed] [Google Scholar]
- 21.Telles S, Nagarathna R, Nagendra HR. Breathing through a particular nostril can alter metabolism and autonomic activities. Indian J Physiol Pharmacol. 1994;38:133–7. [PubMed] [Google Scholar]
- 22.Mohan, Saravanane C, Surange SG, Thombre DP, Chakrabarthy AS. Effect of yoga type breathing on heart rate and cardiac axis of normal subjects. Indian J Physiol Pharmacol. 1986;30:334–40. [PubMed] [Google Scholar]
- 23.Smith JA, Greer T, Sheets T, Watson S. Is there more to exercise than Yoga? Alternative Therapies. 2011;17(3):22–29. [PubMed] [Google Scholar]
- 24.Lutz A, Slagter HA, Dunne JD, Davidson RJ. Attention regulation and monitoring in meditation. Trends Cogn Sci. 2008;12(4):163–169. doi: 10.1016/j.tics.2008.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Deshmukh VD. Neuroscience of meditation. The Scientific World Journal. 2006;6:275–289. doi: 10.1100/tsw.2006.353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Narasimhan L, Nagarathna R, Nagendra H. Effect of integrated yogic practices on positive and negative emotions in healthy adults. International Journal of Yoga. 2011;4(1):13–9. doi: 10.4103/0973-6131.78174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. Gen Hosp Psychiatry. 1982;4(1):33–47. doi: 10.1016/0163-8343(82)90026-3. [DOI] [PubMed] [Google Scholar]
- 28.Carlson LE, Speca M, Faris P, Patel KD. One year pre-post intervention follow-up of psychological, immune, endocrine and blood pressure outcomes of mindfulness-based stress reduction (MBSR) in breast and prostate cancer outpatients. Brain Behav Immun. 2007;21(8):1038–49. doi: 10.1016/j.bbi.2007.04.002. [DOI] [PubMed] [Google Scholar]
- 29.Segal ZV, Bieling P, Young T, et al. Antidepressant monotherapy vs sequential pharmacotherapy and mindfulness-based cognitive therapy, or placebo, for relapse prophylaxis in recurrent depression. Arch Gen Psychiatry. 2010;67(12):1256–64. doi: 10.1001/archgenpsychiatry.2010.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Teasdale JD, Segal ZV, Williams JMG. How does cognitive therapy prevent depressive relapse and why should attentional control (mindfulness) training help? Behav Res Ther. 1995;33:25–39. doi: 10.1016/0005-7967(94)e0011-7. [DOI] [PubMed] [Google Scholar]
- 31.Deshmukh VD. Presence: The Key to Mental Excellence. Jacksonville, FL: Sunanda V Deshmukh; 1999. [Google Scholar]
- 32.Sheline YI, Barch DM, Price JL, et al. The default mode network and self-referential processes in depression. Proc Natl Acad Sci U S A. 2009;106(6):1942–7. doi: 10.1073/pnas.0812686106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Farb NAS, Segal ZV, Anderson AK. Towards a neuroimaging biomarker of depression vulnerability. Translational Neurosci. 2011;2(4):281–292. [Google Scholar]
- 34.Farb NA, Segal ZV, Anderson AK. The mindful brain and emotion regulation in mood disorders. Can J Psychiatry. 2012;57(2):70–7. doi: 10.1177/070674371205700203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brewer JA, Elwafi HM, Davis JH. Craving to Quit: Psychological Models and Neurobiological Mechanisms of Mindfulness Training as Treatment for Addictions. Psychol Addict Behav. 2012 May 28; doi: 10.1037/a0028490. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brewer JA, Bowen S, Smith JT, Marlatt GA, Potenza MN. Mindfulness-based treatments for co-occurring depression and substance use disorders: what can we learn from the brain? Addiction. 2010;105(10):1698–706. doi: 10.1111/j.1360-0443.2009.02890.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brewer JA, Worhunsky PD, Gray JR, Tang YY, Weber J, Kober H. Meditation experience is associated with default mode network activity and connectivity. Proc Natl Acad Sci U S A. 2011;108(50):20254–9. doi: 10.1073/pnas.1112029108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Farb NA, Anderson AK, Mayberg H, Bean J, McKeon D, Segal ZV. Minding one’s emotions: Mindfulness training alters the neural expression of sadness. Emotion. 2010;10(1):25–33. doi: 10.1037/a0017151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Froeliger BE, Garland EL, Modlin LA, McClernon FJ. Neurocognitive correlates of the effects of yoga meditation practice on emotion and cognition: a pilot study. Front Integr Neurosci. 2012;6:48. doi: 10.3389/fnint.2012.00048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hasenkamp W, Wilson-Mendenhall CD, Duncan E, Barsalou LW. Mind wandering and attention during focused meditation: a fine-grained temporal analysis of fluctuating cognitive states. Neuroimage. 2012;59(1):750–60. doi: 10.1016/j.neuroimage.2011.07.008. [DOI] [PubMed] [Google Scholar]
- 41.World Health Organization (WHO) [9/1/2012];Management of Substance Abuse: Resources for the prevention and treatment of substance use disorders. http://www.who.int/substance_abuse/en/
- 42.Kuehn BM. WHO Documents Worldwide Need for Better Drug Abuse Treatment—and Access to It. JAMA. 2012;308(5):442–443. doi: 10.1001/jama.2012.8882. [DOI] [PubMed] [Google Scholar]
- 43.Kochupillai V, Kumar P, Singh D, Aggarwal D, Bhardwaj N, et al. Effect of rhythmic breathing (Sudarshan kriya and pranayam) on immune functions and tobacco addiction. Ann N Y Acad Sci. 2005;1056:242–252. doi: 10.1196/annals.1352.039. [DOI] [PubMed] [Google Scholar]
- 44.Hendershot CS, Witkiewitz K, George WH, Marlatt GA. Relapse prevention for addictive behaviors. Substance abuse treatment, prevention and policy. 2011;6:17. doi: 10.1186/1747-597X-6-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bock, et al. Yoga as a complementary treatment for smoking cessation: rationale, study design and participant characteristics of the Quitting-in-Balance study. BMC Complementary and Alternative Medicine. 2010;10:14. doi: 10.1186/1472-6882-10-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Al’absi M, Hatsukami D, Davis GL, Wittmers LE. Prospective examination of effects of smoking abstinence on cortisol and withdrawal symptoms as predictors of early smoking relapse. Drug Alcohol Depend. 2004;73(3):267–78. doi: 10.1016/j.drugalcdep.2003.10.014. [DOI] [PubMed] [Google Scholar]
- 47.Garland EL, Boettiger CA, Howard MO. Targeting cognitive-affective risk mechanisms in stress-precipitated alcohol dependence: an integrated, biopsychosocial model of automaticity, allostasis, and addiction. Med Hypotheses. 2011;76(5):745–54. doi: 10.1016/j.mehy.2011.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Witkiewitz K, Lustyk MK, Bowen S. Retraining the Addicted Brain: A Review of Hypothesized Neurobiological Mechanisms of Mindfulness-Based Relapse Prevention. Psychol Addict Behav. 2012 doi: 10.1037/a0029258. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Witkiewitz K, Bowen S. Depression, craving, and substance use following a randomized trial of mindfulness-based relapse prevention. J Consult Clin Psychol. 2010;78(3):362–74. doi: 10.1037/a0019172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Witkiewitz K, Bowen S, Douglas H, Hsu SH. Mindfulness-based relapse prevention for substance craving. Addict Behav. 2012 doi: 10.1016/j.addbeh.2012.04.001. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bowen S, Kurz AS. Between-session practice and therapeutic alliance as predictors of mindfulness after mindfulness-based relapse prevention. J Clin Psychol. 2012;68(3):236–45. doi: 10.1002/jclp.20855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Brewer JA, Mallik S, Babuscio TA, et al. Mindfulness training for smoking cessation: results from a randomized controlled trial. Drug Alcohol Depend. 2011;119(1-2):72–80. doi: 10.1016/j.drugalcdep.2011.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Davis JM, Fleming MF, Bonus KA, Baker TB. A pilot study on mindfulness based stress reduction for smokers. BMC Complement Altern Med. 2007;7:2. doi: 10.1186/1472-6882-7-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Brewer JA, Sinha R, Chen JA, et al. Mindfulness training and stress reactivity in substance abuse: results from a randomized, controlled stage I pilot study. Subst Abus. 2009;30(4):306–17. doi: 10.1080/08897070903250241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rogojanski J, Vettese LC, Antony MM. Coping with cigarette cravings: Comparison of suppression versus mindfulness-based strategies. Mindfulness. 2011;2(1):14–26. [Google Scholar]
- 56.Garland EL, Gaylord SA, Boettiger CA, Howard MO. Mindfulness training modifies cognitive, affective, and physiological mechanisms implicated in alcohol dependence: results of a randomized controlled pilot trial. J Psychoactive Drugs. 2010;42(2):177–92. doi: 10.1080/02791072.2010.10400690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Garland EL. Mindfulness-oriented recovery enhancement. Washington, DC: NASW Press; 2012. [Google Scholar]
- 58.Segal ZV, Williams JMG, Teasdale J. Mindfulness-Based Cognitive Therapy for Depression: A New Approach to Preventing Relapse. New York, NY: The Guilford Press; 2002. [Google Scholar]
- 59.Greeson JM, Webber DM, Smoski MJ, Brantley JG, Ekblad AG, Suarez EC, Wolever RQ. Changes in spirituality partly explain health-related quality of life outcomes after Mindfulness-Based Stress Reduction. J Behav Med. 2011;34(6):508–18. doi: 10.1007/s10865-011-9332-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.National Institutes of Health RePORTER. [9/10/2012]; Available at: ( http://clinicaltrials.gov/ct2/show/NCT01505101)
- 61.Telles S, Raghavendra BR, Naveen KV, Manjunath NK, Kumar S, Subramanya P. Changes in Autonomic Variables Following Two Meditative States Described in Yoga Texts. J Altern Complement Med. 2012 doi: 10.1089/acm.2011.0282. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chambless DL, Ollendick TH. Empircally supported psychological interventions: controversies and evidence. Annu Rev Psychol. 2001;52:685–716. doi: 10.1146/annurev.psych.52.1.685. [DOI] [PubMed] [Google Scholar]
- 63.Swami Vishnu-devananda . The Complete Illustrated Book of Yoga. New York, NY: Harmony Books; 1988. p. 5. [Google Scholar]
- 64.Marlatt GA. Buddhist philosophy and the treatment of addictive behavior. Cogn Behav Pract. 2002;9:44–50. [Google Scholar]


