Abstract
This study implemented an innovative new model of delivering a Mindfulness-Based Stress Reduction (MBSR) program that replaces six of the eight traditional in-person sessions with group telephonic sessions (tMBSR) and measured the program's impact on the health and well-being of nurses employed within a large health care organization. As part of a nonrandomized pre–post intervention study, 36 nurses completed measures of health, stress, burnout, self-compassion, serenity, and empathy at three points in time. Between baseline (Time 1) and the end of the 8-week tMBSR intervention (Time 2), participants showed improvement in general health, t(37) = 2.8, p < .01, decreased stress, t(37) = 6.8, p < .001, decreased work burnout, t(37) = 4.0, p < .001, and improvement in several other areas. Improvements were sustained 4 months later (Time 3), and individuals who continued their MBSR practice after the program demonstrated better outcomes than those that did not. Findings suggest that the tMBSR program can be a low cost, feasible, and scalable intervention that shows positive impact on health and well-being, and could allow MBSR to be delivered to employees who are otherwise unable to access traditional, on-site programs.
Keywords: burnout, healthcare, meditation, Mindfulness-Based Stress Reduction (MBSR), nursing, stress
The study team thanks Jeannine Rivet for her support and encouragement of this study, as well as her support of UnitedHealth Group's Center for Nursing Advancement. The authors also wish to acknowledge Terry Pearson from the University of Minnesota Center for Spirituality and Healing who provided the MBSR intervention that we tested in this study. In addition, we wish to acknowledge Crysil Ashcroft and Lisa Ballard, both instrumental to this research in their project coordination roles. Finally, this study could not have been completed without the dedicated participation by members of the UnitedHealth Group nursing community not only in the MBSR sessions, but also in their responses to study questionnaires, and in the feedback they provided about the MBSR program; their contribution is greatly appreciated.
Within the health care industry and beyond, persistent high stress has been shown to be related to negative outcomes in the workplace including personal and professional burnout, absenteeism, lower productivity, lower job satisfaction, and workplace turnover (Erickson & Grove, 2007; Gilboa, Shirom, Fried, & Cooper, 2008; Parker et al., 2003; Zangaro & Soeken, 2007). Although this article focuses on a stress intervention within a health care environment, the problem of stress in the workplace and the proposed intervention is relevant and implementable for a wide variety of industries.
Specific to the health care setting, high employee stress has also demonstrated to be detrimental to the outcomes of patients served (Aiken, Clarke, Sloane, Sochalski, & Silber, 2002; Halm et al., 2005; Scott, Hwang, & Rogers, 2006). Furthermore, nurses serving in nontraditional roles face unique kinds of stress in the workplace. For example, in addition to meeting the needs of sick and dying patients, and coordinating and documenting care across different health care systems, clinical and administrative nurses at companies similar to the one in which this study was conducted face additional pressures tied to working in the highly metrics-driven, productivity-oriented, financially focused work environment of a large corporation. Typical nurse roles in a corporate environment may include direct patient care, either telephonically or in-person, as well as nurse informatics specialist, and nurses designing and running large-scale programs. In these corporate roles, nurses are held to production and financial targets to ensure alignment with business objectives. This may contribute to a mismatch between job requirements and the skills of the employee, which, according to Borkowski (2011), results in job stress, increased absenteeism, tardiness, and turnover leading to lower organizational productivity and profitability. In addition, the nursing profession is predominantly female, and studies on health care workers that explore family–work conflict in relation to stress, burnout, and well-being clearly indicate that those experiencing more stress in and out of work have a greater incidence of anxiety and depressive disorders (Bryant, Fairbrother, & Fenton, 2009; Weinberg & Creed, 2000).
Research also shows that prolonged stress and maladaptive stress responses may result in a number of negative emotional and physical impacts that are well documented. Stress responses may include elevated cortisol levels, which interfere with working memory and information processing; and impaired digestive function, including ulcers, irritable bowel syndrome, and ulcerative colitis (Borkowski, 2011; Irving, Dobkin, & Park, 2009; Jennings, 2008; Larzelere & Jones, 2008). Additionally, stress causes impaired immune response and delayed healing; cardiovascular disease, including hypertension, atherosclerosis, and heart attacks; and a number of psychiatric or social disorders including anxiety, depression, psychosis, sleep disorders, and social impairment (Borkowski, 2011; Jennings, 2008; Larzelere & Jones, 2008).
In addition to these critical concerns related to employee well-being and health, there is also the economic impact to employers to consider. Although estimating the true cost of stress in the workplace is difficult (Goldin, 2004), stress is thought to be related to absenteeism, presenteeism, turnover, direct medical costs, short- and long-term disability, worker's compensation, legal costs, and accidents, and the total cost to U.S. businesses could be as high as $300 billion (American Institute of Stress, n.d.; American Psychological Association, n.d.). One study found that stressed employees are 46% costlier in terms of medical costs alone than nonstressed employees (Goetzel et al., 1998).
MINDFULNESS-BASED STRESS REDUCTION
Mindfulness-Based Stress Reduction (MBSR) was originally created as an 8-week, patient-centered, evidence-based intervention that focuses on teaching mindfulness meditation, breathwork, basic yoga, and other relaxation methods. MBSR was initially developed by Jon Kabat-Zinn at the University of Massachusetts Medical Center in 1979 in an effort to teach patients with chronic medical conditions how to lead fuller and healthier lives. Mindfulness is defined as a self-directed practice for relaxing the body and calming the mind through focusing on present-moment awareness. The emphasis of mindfulness is staying in the present moment, with a nonjudging, nonstriving attitude of acceptance (Kabat-Zinn, 1990; Reibel, Greeson, Brainard, & Rosenzweig, 2001). Mindfulness is cultivated through the practice of meditation (Kabat-Zinn, 2003).
A review of the literature finds that MBSR has repeatedly demonstrated positive impacts on health and well-being in a variety of populations. A meta-analysis of 20 studies in a wide-range of clinical populations found consistent improvements in depression, anxiety, coping style, and quality-of-life measures (Grossman, Niemann, Schmidt, & Walach, 2004). McCarney, Schulz, and Grey (2012) conducted a meta-analysis of 11 studies examining the effectiveness of mindfulness-based therapies in reducing symptoms of depression and reported significant decreases in depression symptomatology. Another meta-analysis of seven controlled trials of healthy participants found that MBSR had a significant impact on stress compared to no treatment (Chiesa & Serretti, 2009). A recent review also outlines evidence to support the impact of mindfulness meditation on many stress-related medical conditions including psoriasis, type 2 diabetes, fibromyalgia, rheumatoid arthritis, and chronic low back pain, as well as reducing stress among individuals with chronic illness (Greeson, 2009). Although many of these studies rely on self-report measures, additional studies have found objective changes in brain activation, immune system response, and changes in the structure and function of the brain involved in memory, learning, and emotion (Davidson, et al., 2003; Hölzel et al., 2011).
Specific to the health care field, a review of 10 studies of the impact of MBSR on health care professionals’ health and wellness found that MBSR consistently reduced stress and anxiety and improved positive affect, while also decreasing emotional exhaustion (Irving et al., 2009). Although there has been limited research involving the impact of MBSR on nurses separate from other health care professionals, studies have found statistically significant improvements in mood and burnout pre- and post-MBSR intervention, and among MBSR intervention groups compared to control groups (Cohen-Katz, Wiley, Capuano, Baker, & Shapiro, 2005; Mackenzie, Poulin, & Seidman-Carlson, 2006). In addition to improved mood and decreased burnout, Frisvold, Lindquist, and McAlpine (2012) reported that nurses completing an MBSR program described in qualitative interviews stronger interpersonal communication, increased self-awareness through becoming more mindful and reflective, improved effectiveness at dealing with stress, and an ability to take hold of their lives. Although the above research has demonstrated that MBSR can reduce stress and burnout, and improve health, other potential benefits from MBSR, including increased serenity, empathy, and self-compassion, are critical to the delivery of health care services in particular, but can also be important factors for those in leadership roles, as well as those in job roles with high customer contact.
Serenity, defined as a learned feeling of inner peace, has been linked to decreased stress and improved general health, and for decades has been recognized as an important component of the nursing profession (Kreitzer, Gross, Waleekhachonolet, Reilly-Spong, & Byrd, 2009; Roberts & Whall, 1996). Knowledge of serenity has also been shown to be related to lower nurse burnout (Sansoucie et al., 2006). Emerging research has demonstrated that serenity is positively related to mindfulness, and that MBSR programs show positive impact on serenity among registered nurses (Penque, 2009) and transplant patients (Sherr, 2010).
Research has demonstrated that empathy plays a critical role in health care practice in terms of providing adequate support and care for patients (Reynolds, Scott, & Austin, 2000), influencing patient satisfaction (Pollak et al., 2011), and being related to patient compliance with clinical recommendations (Hojat et al., 2010). A review of 17 studies of empathy training for nurses concluded that it is possible to increase nurse empathy (Brunero, Lamont, & Coates, 2010), and it has been suggested that empathy could be improved and expanded through strategies that encourage a mindful awareness of the patient as the center of care and moves beyond just feeling empathy to taking empathetic action through support and treatment (Garden, 2009). MBSR has been shown to significantly increase empathy among physicians (Beckman et al., 2012; Krasner et al., 2009), as well as among nursing students (Beddoe & Murphy, 2004), social work students (Gockel, Burton, James, & Bryer, 2012), medical and premedical students (Shapiro, Schwartz, & Bonner, 1998), and within a community sample (Birnie, Speca, & Carlson, 2010).
In some cases, caring for others comes at the expense of caring for the self, and often this continued self-sacrifice can lead to compassion fatigue among helping professionals, especially those exposed to pain, suffering, or trauma (Figley, 2002; Sabo, 2011). Self-compassion, therefore, is a key element to the self-care that needs to be part of therapy and other helping professions (Gilbert, 2006); a lack of that self-compassion has been associated with poorer patient outcomes (Castonguay, Boswell, Constantino, Goldfried, & Hill, 2010). A randomized controlled study of health care professionals found that the group receiving the MBSR intervention reported decreased stress and greater self-compassion than the controls (Shapiro, Astin, Bishop, & Cordova, 2005), and a study of therapists in training found that MBSR program participants showed significantly greater increases in self-compassion compared to cohort controls (Shapiro, Brown, & Biegel, 2007). In a study (Newsome, Waldo, & Gruszka, 2012) that included a group of interprofessional students preparing to enter helping professions (nursing, social work, psychology, counseling, and teaching), a 6-week mindfulness group work intervention resulted in reductions in perceived stress and an increase in self-compassion.
The largest study of mindfulness in the workplace by Wolever et al. (2012) compared a mindfulness-based intervention with therapeutic yoga and with a control group and compared online versus in-person versions of each program. Two hundred thirty-nine employees were enrolled. Compared with the control group, participants in the mind–body interventions showed significantly greater improvements in perceived stress, sleep quality, and heart rate variability. The two delivery mechanisms produced equivalent results. A telehealth mindfulness intervention has also been piloted in a population of military veterans diagnosed with combat-related post-traumatic stress disorder (PTSD). The goal of this pilot study by Niles, Vujanovic, Silberbogen, Seligowski, and Potter (2012) was to determine whether self-reported levels of mindfulness would change over the course of the 8-week program. Results indicated that a brief telehealth intervention was effective in increasing self-reported mindfulness.
The impact of mindfulness on leadership in the workplace has also been the focus of recent studies. Reb, Narayan, and Chaturvedi (2012) hypothesized that supervisors who completed mindfulness would demonstrate increased awareness and attention and that these traits would impact employee well-being and job satisfaction. Two studies using data from supervisors and their subordinates confirmed these predicted relationships.
OBJECTIVE
Previous research has suggested that the traditional 8-week in-person MBSR program can be successfully adapted for use in the workplace and still show significant impact on perceived stress (Klatt, Buckworth, & Malarkey, 2009; Pipe et al., 2009). These prior adaptations have involved shortening the overall length of the program, as well as the amount of meeting and practice time. However, the typical format for MBSR has generally remained classroom based and therefore may still limit participation for telecommuters, employees who travel frequently for business, or other employee or patient populations that could possibly benefit from MBSR but cannot easily attend weekly classroom sessions. There are, therefore, emerging efforts to explore new ways of providing alternatives to these in-person MBSR classes. As noted earlier, a recent study demonstrated that those who participated in a workplace MBSR program showed greater improvement in perceived stress, sleep quality, and heart rhythm coherence (a measure of heart rate variability) than employees randomized to a control group without the program, and that there was no difference in outcomes between MBSR program participants who attended in-person versus online (Wolever et al., 2012).
To add to our knowledge about the viability of alternative deliveries of MBSR, this study tested an innovative, scalable delivery method of MBSR called telephonic MBSR (tMBSR) that was designed to provide access to nurse telecommuters employed at a large multisite health care company. The objective of the study was to measure whether this alternative delivery of MBSR that requires less in-person attendance could positively affect the nurses’ overall health and well-being in key areas research suggests are important to this working population and have been shown to be affected by traditional MBSR programs in prior studies: stress, burnout, general and mental health, serenity, empathy, and self-compassion.
METHOD
Procedure
All study-related procedures were approved by the Institutional Review Board at the University of Minnesota. The target audience for this intervention included nurses employed in a variety of nursing roles in either a Midwest or Southwest location of a large health care company. Following identification of the target nurse population, an e-mail was sent to these 258 nurses inviting them to participate in a one-hour tMBSR informational teleconference call, including a 10-minute meditation session, led by an MBSR instructor. Seventy-two nurses participated in the informational call, and subsequently 58 participants indicated interest in the program and completed a brief online application.
Study enrollment occurred on a first-come, first-serve basis, and the 41 candidates who successfully met eligibility criteria and provided informed consent were enrolled in the study. Eligibility criteria were (a) a hire date of June 1, 2009 or earlier; (b) lack of previous MBSR training; (c) active nurse licensure (participants could be LPNs/LVNs, RNs, or NPs); (d) performance standing (nurses on elevated or final corrective action were not eligible due to attrition risk); and (e) manager support to ensure business continuity requirements were met.
In addition to participating in the tMBSR intervention, study participants were asked to complete baseline, 2-month follow-up, and 4-month follow-up measures (described below) and were offered a gift of low monetary value and continuing education (CE) credits (one contact hour) for each survey completion as compensation for their time. The participants were also given additional CE credits for their participation in the intervention itself, with the number of credits dependent on the number of hours they engaged in MBSR meetings and practice.
Design
The study was designed as a nonrandomized pre–post intervention study, to examine within-group differences in the nurses on measures of health and well-being (described below) administered in the 2 weeks prior to the beginning of the tMBSR intervention period (Time 1), immediately following the 8-week tMBSR intervention period (Time 2), and an additional measure 4 months after the conclusion of the tMBSR program (Time 3). Analyses were run using SAS software, version 9.2 of the SAS system for Windows.
Sample
A total of 41 nurses from a large health care company participated in the tMBSR intervention, of which 36 completed the survey measure at all three time points (see Figure 1 for a complete study flow diagram). Gender, age, education, and job characteristics data were available for each of the participants, though company policy prevented us from obtaining ethnicity information.
FIGURE 1.
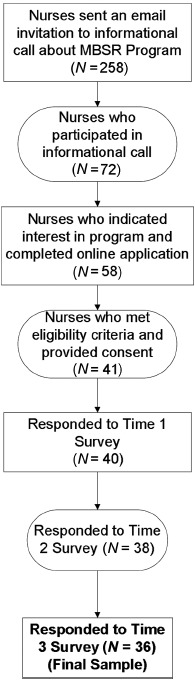
Response rate throughout recruitment and participation in the telephonic Mindfulness-Based Stress Reduction (tMBSR) intervention.
Measures
A consolidated online survey instrument was administered at the three time points and consisted of six measures that have been used widely in the literature and that have demonstrated strong reliability and validity in previous studies. The Perceived Stress Scale is an extensively used measure of stress appraisal, measuring the degree to which individuals perceive their lives as unpredictable and uncontrollable (Cohen, Kamarck, & Mermelstein, 1983), and is a scale that has been used in a prior study of MBSR in a population of health professionals (Shapiro et al., 2005). The Copenhagen Burnout Inventory (CBI) is an instrument that measures burnout in three areas—personal, work, and with clients (Kristensen, Borritz, Valladsen, & Christensen, 2005)—and is a measure that has been used in several studies of nurses and other care providers (e.g., Bourbonnais, et al., 2006). The SF-12v2 Health Survey (SF-12), is a well-known measure of physical and mental health that includes two overall scores (the Physical Component Score [PCS] and the Mental Health Component Score [MCS]) as well as several subscales (Ware, Kosinski, & Keller, 1996). We analyzed the SF-12 using a scoring algorithm coded from the user's manual that is based on the 1998 norms for the U.S. population (Ware, Kosinski, Turner-Bowker, & Gandek, 2002). The Brief Serenity Scale is a relatively new measure of spirituality and well-being that was developed in response to a need for a shorter measure of serenity than previously established measures (Kreitzer et al., 2009), and which has been used in prior studies of the nursing population (Penque, 2009) and MBSR (Gross et al., 2009). The Jefferson Scale of Physician Empathy is designed to measure empathy among physicians, health professionals, and medical students (Hojat et al., 2001), and its use has been validated among nurses (Fields et al., 2004), and nursing students (Ward et al., 2009). The Self-Compassion Scale is a validated, reliable scale designed to measure multiple areas such as self-kindness, isolation, and self-judgment (Neff, 2003) and has been used in a prior study of MBSR in a population of health professionals (Shapiro et al., 2005) as well as in prior studies of self-compassion among nurses (Heffernan, Griffin, McNulty, & Fitzpatrick, 2010; Penque, 2009).
Throughout the tMBSR program, the nurses maintained a detailed log of the amount and type of participation (retreats, teleconferences, and self-practice). In addition, at Time 3, the nurses were also asked “Have you maintained your MBSR practice after completing the formal program?” This question was used to measure the relationship between continued MBSR practice and Time 3 outcomes. Nurses who reported maintaining their MBSR practice were asked to indicate which activities they had maintained, as well as to report the number of hours they maintained their MBSR practice on average per week.
Intervention
The tMBSR intervention was sponsored by a large, multisite health care organization and intervention delivery occurred in partnership with the University of Minnesota's Center for Spirituality & Healing, which maintains MBSR research and training programs. The tMBSR delivery was an innovative blended format of MBSR that combined classroom and telephonic delivery methods, rather than using the in-person only method, as MBSR has traditionally been delivered. The tMBSR program was delivered by an experienced MBSR instructor and involved a full-day in-person retreat on a Saturday at the beginning of the 8-week program, six weekly 1.5-hour group teleconference calls at a regularly scheduled day and time, email contact with the instructor between sessions, and a full-day retreat on a Saturday at the end of the 8-week program. The full-day retreats occurred in a conference room at a business location. During the 8-week course, participants followed a proposed schedule that included (a) guided instruction in mindfulness meditation practices, (b) facilitated group discussion, (c) gentle stretching and yoga, (d) daily work and home assignments, and (e) access to individually tailored instruction and support. Each participant received four guided CDs, a customized workbook, a DVD of yoga instruction, and the book Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness, by Jon Kabat-Zinn (1990). Participants followed a homework schedule of formal and informal practices from the CD, workbook, and DVD, as well as readings from the Full Catastrophe Living for each week. All home practices were 25 to 30 minutes in duration and a recorded sitting meditation with attention on the breath was used on alternating days in Weeks 2 through 4. Throughout the 8-week intervention period the participants maintained a log of the type of home practice they engaged in and the amount of time they spent on each activity.
RESULTS
Demographics
Table 1 shows the demographic and job characteristics of the intervention group who completed surveys at all three time points. One hundred percent of the sample was female with a mean age of 52 and were diverse in terms of education and tenure with the company. The majority of the sample were fulltime employees in exempt, nonsupervisory roles involving patient contact.
Table 1.
Demographic and Job Characteristics of Sample
| % of Total |
||
|---|---|---|
| Sample characteristics | n | N = 36 |
| Job location | ||
| Minnesota | 17 | 47.2% |
| Arizona | 19 | 52.8% |
| Gender | ||
| Female | 36 | 100.0% |
| Age | ||
| Mean age | 52.2 years | |
| Education category | ||
| Non-bachelor's degree | 12 | 38.7% |
| College degree | 9 | 29.0% |
| Postgraduate | 10 | 32.3% |
| Tenure category | ||
| 0–5 Years | 18 | 50.0% |
| 6–10 Years | 7 | 19.4% |
| 11–15 years | 5 | 13.9% |
| 16–20 years | 6 | 16.7% |
| Mean tenure with company | 8.7 years | |
| Median tenure with company | 6.4 years | |
| Job characteristics | ||
| Part-time | 4 | 11.1% |
| Full-time | 32 | 88.9% |
| Telecommuter | 20 | 55.6% |
| Nontelecommuter | 16 | 44.4% |
| Supervisor | 9 | 25.0% |
| Nonsupervisor | 27 | 75.0% |
| Exempt | 32 | 88.9% |
| Nonexempt | 4 | 11.1% |
| Has patient contact | 29 | 80.6% |
| Has no patient contact | 7 | 19.4% |
| Grade level category | ||
| Salary grade under 28 | 23 | 63.9% |
| Salary grade 28+ | 13 | 36.1% |
Amount of tMBSR Participation
Table 2 summarizes the amount and type of nurse participation during the 8-week tMBSR program. Results suggest that there was high engagement in the program, with an average total time participating (including retreats, teleconference, and self-practice) of 50.3 hours. The nurses participated, on average, 13.9 hours in the in-person retreats, out of the total of 16 hours that were offered. Of the 9 possible hours of teleconference practice, the nurses participated for an average of 7.9 hours. The nurses also spent a substantial amount of time practicing on their own, outside of the instructor-led retreats and teleconferences, as reflected in an average of 28.5 hours of self-practice.
Table 2.
Amount of Participation in Telephonic Mindfulness-Based Stress Reduction (tMBSR) Intervention
| Practice elements | M | SD | Maximum | Minimum |
|---|---|---|---|---|
| Mean total hours of practice | 50.3 | 14.6 | 81.1 | 26.6 |
| Mean total hours in in-person retreats | 13.9 | 1.9 | 14.5 | 7.5 |
| Mean total hours in teleconferences | 7.9 | 1.4 | 9.0 | 4.5 |
| Mean total hours in group practice (retreat or teleconference) | 21.8 | 2.5 | 23.5 | 12.0 |
| Mean total hours in self practice | 28.5 | 14.0 | 57.6 | 6.1 |
Impact of MBSR on Health and Wellness Measures
As shown in Table 3, statistically significant improvements were observed for those nurses participating in the tMBSR program on almost every measure from baseline (Time 1) to postintervention (Time 2). These changes were sustained 4 months later (Time 3) and, on some measures, nurses continued to show significant improvement from Time 2 to Time 3.
Table 3.
Impact of Telephonic Mindfulness-Based Stress Reduction (tMBSR) Intervention on Health and Wellness Measures
| Time 1 |
Time 2 |
Time 1 – Time 2 Difference |
Time 3 |
Time 2 – Time 3 Difference |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | n | α | M | SD | M | SD | t | p | M | SD | t | p |
| Perceived Stress Scale | 36 | 0.94 | 20.64 | 7.61 | 12.39 | 5.71 | t(35) = 6.39 | <001 | 12.50 | 5.56 | t(35)=.15 | ns |
| Copenhagen Burnout | ||||||||||||
| Inventory (CBI) | ||||||||||||
| CBI Personal | 36 | 0.91 | 44.56 | 19.74 | 26.27 | 17.48 | t(35) = 5.65 | <.001 | 24.88 | 17.66 | t(35)=.56 | ns |
| CBI Work | 36 | 0.78 | 49.50 | 19.43 | 37.55 | 15.83 | t(35) = 3.88 | <.001 | 32.24 | 14.45 | t(35) = 2.55 | <.05 |
| CBI Client | 34 | 0.89 | 19.49 | 18.05 | 14.22 | 16.12 | t(33) = 2.12 | <.05 | 13.48 | 15.56 | t(33)=.32 | ns |
| SF-12v2 Health Survey | 0.85 | |||||||||||
| General health | 36 | 46.12 | 9.11 | 49.41 | 8.35 | t(35) = 2.58 | <.05 | 50.91 | 7.05 | t(35) = 1.30 | ns | |
| Physical functioning | 36 | 51.69 | 8.07 | 51.46 | 8.56 | t(35)=.18 | ns | 53.13 | 5.54 | t(35)=1.19 | ns | |
| Role physical | 36 | 52.70 | 6.37 | 52.95 | 6.46 | t(35)=.23 | ns | 53.85 | 5.00 | t(35)=.88 | ns | |
| Bodily pain (lack of) | 36 | 49.52 | 8.82 | 51.78 | 6.65 | t(35)=1.85 | ns | 52.35 | 5.71 | t(35)=.53 | ns | |
| Vitality | 36 | 46.91 | 7.75 | 53.34 | 6.56 | t(35) = 4.60 | <.001 | 53.34 | 7.39 | t(35) = .00 | ns | |
| Social functioning | 36 | 45.91 | 10.51 | 52.36 | 6.99 | t(35) = 4.12 | <.001 | 53.20 | 5.40 | t(35) = 1.00 | ns | |
| aRole emotional | 36 | 41.79 | 9.95 | 49.87 | 6.38 | t(35) = 5.56 | <.001 | 51.26 | 6.43 | t(35) = 1.06 | ns | |
| Mental health | 36 | 38.13 | 9.22 | 51.84 | 8.29 | t(35) = 8.12 | <.001 | 51.50 | 6.38 | t(35)=.29 | ns | |
| PCS | 36 | 54.68 | 8.01 | 51.77 | 7.23 | t(35) = 2.65 | <.05 | 53.15 | 5.78 | t(35)=1.27 | ns | |
| MCS | 36 | 38.23 | 10.53 | 51.39 | 7.84 | t(35) = 7.46 | <.001 | 51.49 | 6.25 | t(35)=.08 | ns | |
| Brief Serenity Scale | 36 | 0.94 | 2.75 | 0.61 | 3.69 | 0.65 | t(35) = 8.43 | <.001 | 3.79 | 0.67 | t(35)=1.71 | ns |
| Jefferson Scale of Physician Empathy | 32 | 0.78 | 116.59 | 8.98 | 123.59 | 9.31 | t(31) = 5.17 | <.001 | 123.00 | 10.48 | t(31)=.49 | ns |
| Self-Compassion Scale | ||||||||||||
| Self-kindness | 36 | 0.95 | 2.67 | 0.82 | 3.52 | 0.73 | t(35) = 4.86 | <.001 | 3.70 | 0.69 | t(35) = 2.16 | <.05 |
| Common humanity | 36 | 0.85 | 2.81 | 0.88 | 3.70 | 0.83 | t(35) = 5.84 | <.001 | 3.92 | 0.78 | t(35) = 2.91 | <.01 |
| Mindfulness | 36 | 0.83 | 3.02 | 0.71 | 3.80 | 0.66 | t(35) = 5.57 | <.001 | 3.92 | 0.72 | t(35) = 1.94 | ns |
| Self-judgment | 36 | 0.91 | 3.35 | 0.96 | 2.41 | 0.83 | t(35) = 6.10 | <.001 | 2.30 | 0.90 | t(35)=.95 | ns |
| Isolation | 36 | 0.86 | 2.98 | 1.01 | 2.19 | 0.79 | t(35) = 5.13 | <.001 | 2.02 | 0.83 | t(35) = 1.98 | ns |
| Overidentification | 36 | 0.87 | 3.17 | 1.02 | 2.13 | 0.81 | t(35) = 6.67 | <.001 | 2.01 | 0.76 | t(35) = 1.36 | ns |
| Overall self-compassion | 36 | 0.91 | 2.83 | 0.75 | 3.72 | 0.66 | t(35) = 6.53 | <.001 | 3.87 | 0.66 | t(35) = 2.75 | <.01 |
Note. PCS = Physical Component Score; MCS = Mental Health Component Score.
Perceived Stress
Previous studies of health care professionals (Shapiro et al., 2005) indicates a norm among women in the United States on the Perceived Stress Scale of 13.7 suggesting that the women in this study, demonstrating a baseline mean score of 20.67, were experiencing high levels of stress. As shown in Table 3 and Figure 2, nurses showed significant improvement from Time 1 to Time 2 on perceived stress, with no significant change from Time 2 to Time 3, suggesting the change was maintained over 4 months.
FIGURE 2.
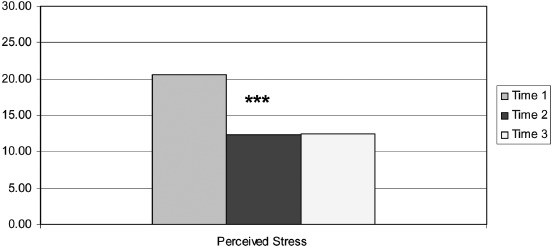
Change in perceived stress as measured by the Perceived Stress Scale from baseline (Time 1) to postintervention (Time 2) to 4-month follow-up (Time 3). ***p < .001. (Color figure available online.)
Burnout
Baseline mean personal and work burnout were comparable to a previous study of health care providers (Bourbonnais et al., 2006). However, client burnout was much higher in the Bourbonnais et al. (2006) study (M = 36.1) compared to our sample (M = 19.49), even when our sample was restricted to just the 28 nurses who had patient contact (M = 21.28). As shown in Table 3 and Figure 3, nurses showed a significant improvement in all three areas of burnout from Time 1 to Time 2 including personal, work, and client. When analyses of the client burnout were restricted to just those nurses who had patient contact, the results were similar, t(27) = 2.5, p = .017. Examining change from Time 2 to Time 3, change was maintained on personal and client burnout. On work burnout, the nurses continued to improve from Time 2 to Time 3, showing a significant decrease over the 4 months after the program.
FIGURE 3.
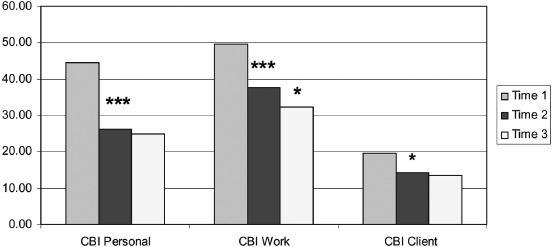
Change in personal, work, and client burnout from baseline (Time 1) to postintervention (Time 2) to 4-month follow-up (Time 3). CBI = Copenhagen Burnout Inventory. *p < .05. ***p < .001. (Color figure available online.)
Health
The norm for the general U.S. population on the SF-12 is represented by a score of 50. As shown in Table 3 and Figure 4, the nurses were above average compared to the general population and did not show significant change over time on the physical functioning, role physical, or bodily pain subscales of the SF-12, and showed a significant decrease in their PCS, but remained above average. However, they did show significant improvement on overall general health, and by Time 3 were above average. They also improved significantly on the vitality subscale from Time 1 to Time 2 and moved from being below average to above average. At Time 1 the women were below average on all mental health aspects of the SF-12, and at Time 2 were scoring above average, with statistically significant improvements on all of the mental health aspects including social functioning, role emotional, mental health, and the overall MCS. There was no significant change from Time 2 to Time 3 on any of the SF-12 measures, suggesting that improvements seen from Time 1 to Time 2 were maintained 4 months later.
FIGURE 4.
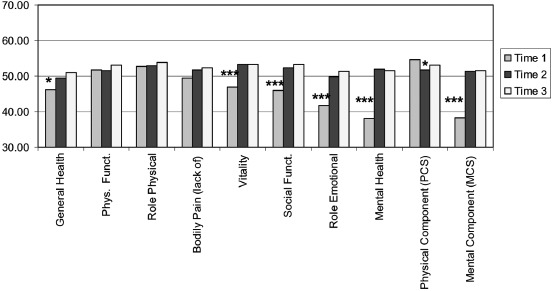
Change in health as measured by the SF12v2 from baseline (Time 1) to postintervention (Time 2) to 4-month follow-up (Time 3). Phys. Funct. = physical functioning; Social Funct. = social functioning; PCS = Physical Component Score; MCS = Mental Health Component Score. *p < .05. ***p < .001. (Color figure available online.)
Serenity
Table 3 shows that at baseline the nurses showed similar serenity scores as previous studies of nurses (Penque, 2009). As shown in Table 3 and Figure 5, nurses showed significant improvement from Time 1 to Time 2 on serenity, with no additional significant change from Time 2 to Time 3, suggesting the change was maintained over 4 months.
FIGURE 5.
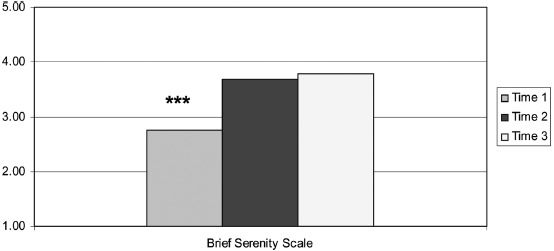
Change in serenity as measured by the Brief Serenity Scale from baseline (Time 1) to postintervention (Time 2) to 4-month follow-up (Time 3). ***p < .001. (Color figure available online.)
Empathy
At baseline, the nurses showed comparable empathy to previous studies of female nurses (Fields et al., 2004). As shown in Table 3 and Figure 6, nurses showed significant improvement from Time 1 to Time 2 on empathy, with no additional change from Time 2 to Time 3, suggesting the change was maintained over 4 months. When analyses of empathy were restricted to just those nurses (n = 28) who had patient contact, the results were similar, t(27) = 4.9, p < .001.
FIGURE 6.
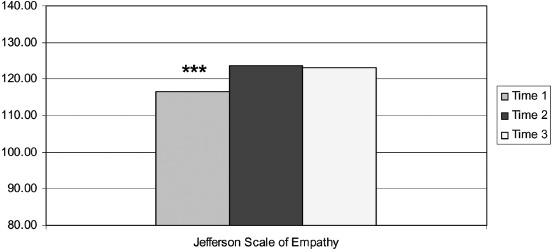
Change in empathy as measured by the Jefferson Scale of Empathy from baseline (Time 1) to postintervention (Time 2) to 4-month follow-up (Time 3). ***p < .001. (Color figure available online.)
Self-compassion
As shown in Table 3, at baseline, the nurses showed mean overall scores and subscale scores on self-compassion that reflected low self-compassion, with scores comparable to or lower than previous studies of nurses (Heffernan et al., 2010; Penque, 2009). As shown in Table 3 and Figure 7, there were significant improvements on all six areas of self-compassion, and in the overall self-compassion score from Time 1 to Time 2. There were significant increases on the three “positive” areas that suggest high self-compassion: self-kindness, common humanity, and mindfulness, and significant decreases on the three “negative” areas that suggest low self-compassion: self- judgment, isolation, and overidentification. Examining differences from Time 2 to Time 3, change was maintained on mindfulness, self-judgment, isolation, and overidentification. However, on self-kindness, common humanity, and overall self-compassion, the nurses continued to show significant improvement from Time 2 to Time 3.
FIGURE 7.
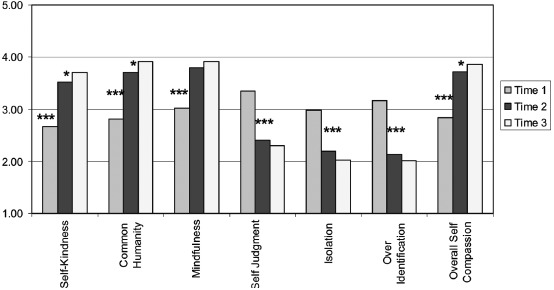
Change in overall self-compassion and its subscales as measured by the Self-Compassion Scale from baseline (Time 1) to postintervention (Time 2) to 4-month follow-up (Time 3). *p < .05. ***p < .001. (Color figure available online.)
Impact of Maintained MBSR Practice on Time 3 Outcomes
At Time 3, 75% (n = 27) of the nurses reported that they had maintained their MBSR practice since completing the program, and the majority reported that they practiced between 1 and 5 hours per week, most commonly practicing the body scan, yoga, and/or meditation. As illustrated in Table 4 and Figure 8, there were several significant differences in Time 3 outcomes between the women who reported at Time 3 that they had maintained their MBSR practice after the program ended (the 4 months between Time 2 and 3), and those who did not. Those who maintained MBSR practice were significantly lower on stress, personal burnout, and work burnout. They were also significantly higher on the SF-12 role emotional subscale, and SF-12 MCS.
Table 4.
Difference in Time 3 Outcomes Between Those Who Maintained Versus Did Not Maintain Mindfulness-Based Stress Reduction (MBSR) Practice
| Maintained MBSRn = 27 | Did not maintain MBSRn = 9 | |||||
|---|---|---|---|---|---|---|
| M | SD | M | SD | t(34) | Significance | |
| Perceived Stress Scale | 10.74 | 4.86 | 17.78 | 4.09 | 3.90 | p < .001 |
| Copenhagen Burnout Inventory (CBI) | ||||||
| CBI Personal | 20.99 | 17.12 | 36.57 | 14.40 | 2.45 | p < .05 |
| CBI Work | 29.10 | 13.93 | 41.67 | 12.24 | 2.41 | p < .05 |
| CBI Client | 11.83 | 16.12 | 18.06 | 13.66 | 1.03 | ns |
| SF-12v2 Health Survey | ||||||
| General health | 52.01 | 7.28 | 47.62 | 5.39 | 1.66 | ns |
| Physical functioning | 53.28 | 5.41 | 52.65 | 6.24 | 0.29 | ns |
| Role physical | 53.93 | 4.75 | 53.59 | 6.00 | 0.17 | ns |
| Bodily pain (lack of) | 52.91 | 5.88 | 50.65 | 5.10 | 1.03 | ns |
| Vitality | 54.46 | 6.24 | 49.99 | 9.78 | 1.61 | ns |
| Social functioning | 53.20 | 5.60 | 53.20 | 5.05 | 0.00 | ns |
| Role emotional | 52.97 | 5.22 | 46.14 | 7.28 | 3.08 | ns |
| Mental health | 52.58 | 6.21 | 48.29 | 6.10 | 1.80 | ns |
| PCS | 53.17 | 5.36 | 53.09 | 7.28 | 0.03 | ns |
| MCS | 52.90 | 5.56 | 47.27 | 6.59 | 2.51 | p < .05 |
| Brief Serenity Scale | 4.02 | 0.58 | 3.09 | 0.38 | 4.47 | p < .001 |
| Jefferson Scale of Physician Empathy | 125.60 | 9.58 | 116.00 | 10.14 | 2.43 | p < .05 |
| Self-Compassion Scale | ||||||
| Self-kindness | 3.88 | 0.67 | 3.17 | 0.45 | 2.96 | p < .01 |
| Common humanity | 4.10 | 0.75 | 3.36 | 0.61 | 2.66 | p < .05 |
| Mindfulness | 4.12 | 0.66 | 3.31 | 0.51 | 3.36 | p < .01 |
| Self-judgment | 2.06 | 0.81 | 3.04 | 0.79 | 3.19 | p < .01 |
| Isolation | 1.79 | 0.76 | 2.72 | 0.64 | 3.28 | p < .01 |
| Overidentification | 1.84 | 0.72 | 2.53 | 0.69 | 2.50 | p < .05 |
| Overall self-compassion | 4.07 | 0.58 | 3.26 | 0.51 | 3.74 | p < .001 |
Note. PCS = Physical Component Score; MCS = Mental Health Component Score.
FIGURE 8.
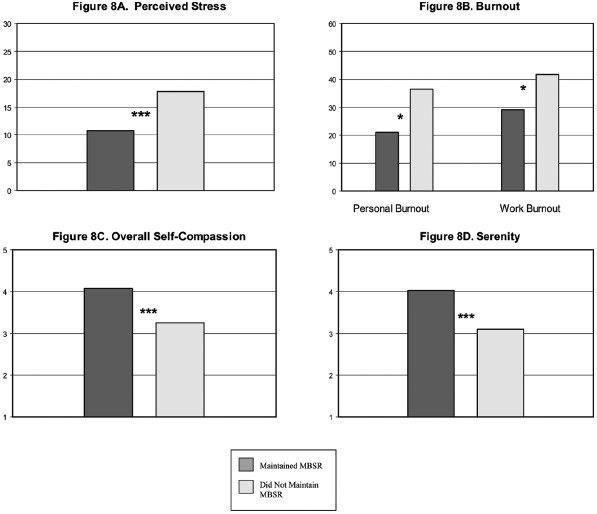
Impact of maintaining Mindfulness-Based Stress Reduction (MBSR) practice after the intervention on 4-month outcomes (Time 3). *p < .05. ***p < .001. (Color figure available online.)
Participants who maintained their MBSR practice were significantly higher on overall self-compassion, as well as all of the positive areas that suggest high self-compassion: self-kindness, common humanity, and mindfulness. They were also significantly lower on all of the negative areas that suggest low self-compassion: self-judgment, isolation, and overidentification. At Time 3 women who maintained their MBSR practice were also significantly higher than those who did not maintain their practice on serenity and empathy.
DISCUSSION
The results of this pilot study suggest that the innovative blended delivery of tMBSR using in-person and telephonic mediums had a positive impact on the nurses’ self-reported health and wellness measures from baseline to postintervention, with all improvements either sustained or showing continued improvement 4 months after the tMBSR intervention, particularly among those who continued to use the MBSR techniques on their own. Similar to other studies showing the positive impact of traditional classroom-based MBSR on health care workers (Cohen-Katz et al., 2005; Galantino, Baime, Mcguire, Szapary, & Farrar, 2005; Mackenzie et al., 2006), nurses who participated in this hybrid tMBSR intervention showed decreased perceived stress and burnout, improved mental health and social functioning, and increased overall general health, as well as significant increases in serenity, empathy, and self-compassion—all important elements to patient care.
Implications to Nursing Practice and Other Service Professions
The positive results realized in this small, pilot study demonstrate that tMBSR may be a desirable, effective, scalable, and affordable intervention to reduce stress and burnout of nurses and other non-nurse employees. Workplace and nonworkplace stress continue to negatively affect the health and well-being of many employees, their productivity, and ultimately the employer's bottom line. This hybrid tMBSR program may prove to be a highly effective intervention to arm employees with the tools and knowledge to improve their physical and mental health and overall effectiveness with patient care, as well as decrease job burnout and turnover; a major problem within the health care professions, particularly nursing, as noted above. Supervisors and managers are ideally positioned to identify opportunities for intervention among their staff, and to serve as positive change agents on behalf of their staff and colleagues. As telecommuting and telehealth become more mainstream, nontraditional mediums for the delivery of health care interventions are needed. The tMBSR pilot shows promise for reaching a telecommuting workforce, as well as employees needing time flexibility given family or dependent care issues, and adds a valuable deployment method to a growing number of options for employers who wish to implement MBSR programs.
Limitations and Lessons Learned
This study did not include a randomized control group who did not receive the tMBSR intervention. Thus, we cannot rule out that the differences observed in the intervention group are a result of regression to the mean, or due to other influences impacting the nurses outside of the tMBSR intervention. Other threats to internal validity include the fact that participants were self-selected, and arguably highly motivated to participate, as demonstrated by their willingness to participate in two full-day retreats on Saturdays, as well as several hours of phone participation and spending time on homework. Without a wait-list control group we cannot rule out the impact individual motivation played in these results. We also did not obtain data from the participants on their previous experience with MBSR or components of MBSR (meditation, yoga, breathwork) which may also have affected participation and outcomes in this study. Additional limitations include the homogeneity of our sample (all female nurses), and the reliance on self-report data that may be subject to respondent bias. We also do not know the role that offering incentives for participation (CE credits) played in the success of our intervention, though the high amount of MBSR practice that continued after the program had ended (and therefore incentives had ended) seems to suggest that these are skills that employees are eager to learn and practice for their own inherent reward.
To address some of these limitations of this study, future research should include a randomized control trial across employees who work in a variety of high-stress roles in the health care industry, including not only nurses, but also customer service representatives and behavioral health intake counselors, and include men and women in these roles. Future research should include, in addition to subjective self-report measures of perceived stress and burnout, objective physiological measures of stress, as well as measures of the impact of the intervention on manager ratings of employee performance, as well as on service delivery in the form of patient and customer ratings of the employees who serve them.
Although engagement among participants was high, as indicated by the high average number of hours of participation in all three methods (in-per-son retreats, teleconferences, and self-practice), we should acknowledge that initial response to the invitation to participate was relatively low (27.9%). We attribute this low receptivity to a general lack of familiarity with the program; the timing of the invitation, which occurred in January, which is usually the busiest time of year for these nurses; and the struggle to articulate the value of a program such as this in manner that can be monetized. Since the time of this study, general awareness about mindfulness has grown as part of the company culture, and with better timing of recruitment, it is likely that response to the invitation would be much higher. Prior to implementing a program such as this, it would be a good idea to provide education about the content and known benefits of MBSR within the workplace, and to be sure to consider the timing of recruitment for the program with other company activity.
Costs incurred by this pilot included fees for the mindfulness instructor, meeting materials, travel costs for the program team, and meals for participants during the two weekend day in-person retreats. Offering the in-person retreats at the worksite eliminated costs for conference room rental and minimized any travel costs for participants. Although the instructor costs were not substantially lower than an 8-week in-person program, because a large component of the program was delivered “virtually,” we did not incur additional meeting room costs and individual travel costs for participant, and thus costs to offer this novel tMBSR program to 40 nurses were lower than the traditional 8-week classroom based format.
It is likely that for some participants, even with the more “user-friendly” telephonic sessions replacing several of the in-person sessions, the time commitment of tMBSR is still too much to fit into their busy schedules. It would therefore be valuable to employers to know the minimal amount of time (frequency of sessions and duration of each session) and amount of each type of delivery method (in-person, telephonic, online, and group vs. self-practice) that is needed to achieve positive outcomes. Given the already busy schedules of nurses and many other employees, there is a need to “explor[e] ways to offer stress management interventions without adding additional time-commitment and strain” (Shapiro et al., 2005, p. 172). Future research is necessary to determine how best to utilize less in-person time, augment with more phone and online technology, and develop communities of practice, all of which would lower the costs and result in an even more approachable program. An additional area of future research is to assess the cost-benefit of the intervention through measures of employee productivity and workforce health care costs.
CONCLUSIONS
These findings are the first to document significant changes in the health and well-being of employees participating in a novel hybrid MBSR program called tMBSR in a corporate environment. There was high receptivity to the program by participating employees, with high levels of engagement and very low attrition. In addition to the measured outcomes, there were additional positive effects on workplace culture conveyed by participants in their comments. Those nurses participating in the program reported that they have begun to utilize new strategies with others in the workplace. Some reported beginning staff meetings with a brief meditation as a mechanism to focus the team and enable dialogue that is more effective. Many participants also reported stopping the reactivity cycle in personal or professional dialogue.
An additional advantage of the tMBSR program to employers is sustain-ability when the program ends. As seen in results from the Time 3 survey at 4 months postprogram completion, those nurses who maintained their MBSR practice between Time 2 and Time 3 showed significantly better outcomes than the nurses who did not maintain their MBSR practice. In addition to their own self-practice, participants were so actively engaged in the program that they requested a mechanism to stay together as a community and to continue their practice after the formal program ended. As a result, optional “drop-in” teleconferences were scheduled for weekday evenings and participants could attend as they desired and their schedules permitted. Participation in these “drop-in” calls was high.
This study contributes to the existing knowledge about the effects of MBSR on health care professionals and demonstrates that a hybrid tMBSR model shows promise as an effective intervention to reduce stress and burnout. The unexpected creation of new, positive relationships in the workplace further supports the impact of the program. Many large organizations stand to benefit from a workplace MBSR intervention and this scalable, novel format is highly approachable for most companies.
With time and intention, we each can use tools such as these to promote mindfulness and increased compassion and engagement to create a culture and work environment that benefits individual employees, those they serve, and the organization as a whole.
REFERENCES
- Aiken L. H., Clarke S. P., Sloane D. M., Sochalski J., Silber J. H. Hospital nurse staffing and patient mortality, nurse burnout, and Job dissatisfaction. Journal of the American Medical Association. 2002;288(16):1987–1993. doi: 10.1001/jama.288.16.1987. [DOI] [PubMed] [Google Scholar]
- American Institute of Stress. Workplace stress. (n.d.). Retrieved from http://www.stress.org/workplace-stress/
- American Psychological Association. Overwhelmed by workplace stress? You're not alone. (n.d.). Retrieved from http://www.apa.org/helpcenter/work-stress.aspx.
- Beckman H. B., Wendland M., Mooney C., Krasner M. S., Quill T. E., Suchman A. L., Epstein R. M. The impact of a program in mindful communication on primary care physicians. Academic Medicine. 2012;87(6):815–819. doi: 10.1097/ACM.0b013e318253d3b2. [DOI] [PubMed] [Google Scholar]
- Beddoe A. E., Murphy S. O. Does mindfulness decrease stress and foster empathy among nursing students? The Journal of Nursing Education. 2004;43(7):305–312. doi: 10.3928/01484834-20040701-07. [DOI] [PubMed] [Google Scholar]
- Birnie K., Speca M., Carlson L. E. Exploring self-compassion and empathy in the context of mindfulness-based stress reduction (MBSR) Stress and Health. 2010;26:359–371. [Google Scholar]
- Borkowski N. Organizational behavior in health care. 2nd ed. Sudbury, MA: Jones and Bartlett Publishers; 2011. [Google Scholar]
- Bourbonnais R., Brisson C., Vinet A., Vézina M, Abdous B., Gaudet M. Effectiveness of a participative intervention on psychosocial work factors to prevent mental health problems in a hospital setting. Occupational and Environmental Medicine. 2006;63:335–342. doi: 10.1136/oem.2004.018077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunero S., Lamont S., Coates M. A review of empathy education in nursing. Nursing Inquiry. 2010;17:65–74. doi: 10.1111/j.1440-1800.2009.00482.x. [DOI] [PubMed] [Google Scholar]
- Bryant C., Fairbrother G., Fenton P. The relative influence of personal and workplace descriptors on stress. British Journal of Nursing. 2000;9(13):876–880. doi: 10.12968/bjon.2000.9.13.5517. [DOI] [PubMed] [Google Scholar]
- Castonguay L. G., Boswell J. F., Constantino M. J., Goldfried M. R., Hill C. E. Training implications of harmful effects of psychological treatments. American Psychologist. 2010;65:34–49. doi: 10.1037/a0017330. [DOI] [PubMed] [Google Scholar]
- Chiesa A., Serretti A. Mindfulness-based stress reduction for stress management in healthy people: A review and meta-analysis. Journal of Alternative Complementary Medicine. 2009;15(5):593–600. doi: 10.1089/acm.2008.0495. [DOI] [PubMed] [Google Scholar]
- Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24:385–396. [PubMed] [Google Scholar]
- Cohen-Katz J., Wiley S., Capuano T., Baker D., Shapiro S. The effects of mindfulness-based stress reduction on nurse stress and burnout. Holistic Nursing Practice. 2005;18(6):303–308. doi: 10.1097/00004650-200411000-00006. [DOI] [PubMed] [Google Scholar]
- Davidson R. J., Kabat-Zinn J., Schumacher J., Rosenkranz M., Muller D., Santorelli S. F., Sheridan J. F. Alterations in brain and immune function produced by mindfulness meditation. Psychosomatic Medicine. 2003;65(4):564–570. doi: 10.1097/01.psy.0000077505.67574.e3. [DOI] [PubMed] [Google Scholar]
- Erickson R., Grove W. Why emotions matter: Age, agitation and burnout among Registered Nurses. Online Journal of Issues in Nursing. 2007;13(1) Retrieved from http://gm6.nursingworld.org/MainMenuCategories/ANAMarketplace/ANAPeriodicals/OJIN/TableofContents/vol132008/No1Jan08/ArticlePreviousTopic/WhyEmotionsMatterAgeAgitationandBurnoutAmongRegisteredNurses.html. [Google Scholar]
- Fields S. K., Hojat M., Gonnella J. S., Mangione S., Kane G., Magee M. Comparisons of nurses and physicians on an operational measure of empathy. Evaluation & the Health Professions. 2004;27:80–94. doi: 10.1177/0163278703261206. [DOI] [PubMed] [Google Scholar]
- Figley C. R. Compassion fatigue: Psychotherapist's chronic lack of self care. Journal of Clinical Psychology. 2002;58:1433–1441. doi: 10.1002/jclp.10090. [DOI] [PubMed] [Google Scholar]
- Frisvold M. H., Lindquist R., McAlpine C. Living life in the balance of mid-life: Lessons learned from mindfulness. Western Journal of Nursing Research. 2012;34(2):265–278. doi: 10.1177/0193945911424171. [DOI] [PubMed] [Google Scholar]
- Galantino M. L., Baime M., Maguire M., Szapary P. O., Farrar J. T. Association of psychological and physiological measures of stress in health-care professionals during an 8-week mindfulness meditation program: Mindfulness in practice. Stress & Health: Journal of the International Society for the Investigation of Stress. 2005;21(4):255–261. [Google Scholar]
- Garden R. Expanding clinical empathy: An activist perspective. Journal of General Internal Medicine. 2009;24:122–125. doi: 10.1007/s11606-008-0849-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert P. Compassion: Conceptualizations, research and use in psychotherapy. New York, NY: Routledge; 2006. [Google Scholar]
- Gilboa S., Shirom A., Fried Y., Cooper C. A meta-analysis of work demand stressors and Job performance: Examining main and moderating effects. Personnel Psychology. 2008;61:227–272. [Google Scholar]
- Gockel A., Burton D., James S., Bryer E. Introducing mindfulness as a self-care and clinical training strategy for beginning social work students. Mindfulness. 2012. pp. 1–11. Retrieved from http://link.springer.com/article/10.1007%2Fs12671-012-0134-1?LI=true#page-1.
- Goetzel R. Z., Anderson D. R., Whitmer R. W., Ozminkowski R. J., Dunn R. L., Wasserman J. The relationship between modifiable health risks and health care expenditures: An analysis of the multi-employer HERO health risk and cost database. Journal of Occupational and Environmental Medicine. 1998;40(10):843–854. doi: 10.1097/00043764-199810000-00003. [DOI] [PubMed] [Google Scholar]
- Goldin R. Counting the costs of stress. STATS: Take a quantitative leap. 2004. Retrieved from http://stats.org/stories/2004/counting_costs_stress_sep23_04.htm.
- Greeson J. M. Mindfulness research update 2008. Complementary Health Practice Review. 2009;14:10–18. doi: 10.1177/1533210108329862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross C. R., Kreitzer M. J., Reilly-Spong M., Winbush N. Y., Schomaker E. K., Thomas W. Mindfulness meditation training to reduce symptom distress in transplant patients: Rationale, design, and experience with a recycled wait-list. Clinical Trials. 2009;6:76–89. doi: 10.1177/1740774508100982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossman P., Niemann L., Schmidt S., Walach H. Mindfulness-based stress reduction and health benefits: A meta-analysis. Journal of Psychosomatic Research. 2004;57:35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- Halm M., Peterson M., Kandels M., Sabo J., Blalock M., Braden R., Topham D. Hospital nurse staffing and patient mortality, emotional exhaustion, and Job dissatisfaction. Clinical Nurse Specialist. 2005;19(5):241–251. doi: 10.1097/00002800-200509000-00007. [DOI] [PubMed] [Google Scholar]
- Heffernan M., Griffin M., McNulty S., Fitzpatrick J. J. Self-compassion and emotional intelligence in nurses. International Journal of Nursing Practice. 2010;16:366–373. doi: 10.1111/j.1440-172X.2010.01853.x. [DOI] [PubMed] [Google Scholar]
- Hojat M., Louis D. Z., Maxwell K., Markham F., Wender R., Gonnella J. S. Patient perceptions of physician empathy, satisfaction with physician, interpersonal trust, and compliance. International Journal for Medical Education. 2010;1:83–87. [Google Scholar]
- Hojat M., Mangione S., Nasca T. J., Cohen M. J., Gonnella J. S., Erdmann J. B., Magee M. The Jefferson Scale of Physician Empathy: Development and preliminary psychometric data. Educational and Psychological Measurement. 2001;61(2):349–365. [Google Scholar]
- Hölzel B. K., Carmody J., Vangel M., Congleton C., Yerramsetti S. M., Gard T., Lazar S. W. Mindfulness practice leads to increases in regional brain gray matter density. Psychiatry Research: Neuroimaging. 2011;191(1):36–43. doi: 10.1016/j.pscychresns.2010.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irving J. A., Dobkin P. L., Park J. Cultivating mindfulness in health care professionals: A review of empirical studies of mindfulness-based stress reduction (MBSR) Complementary Therapies in Clinical Practice. 2009;15:61–66. doi: 10.1016/j.ctcp.2009.01.002. [DOI] [PubMed] [Google Scholar]
- Jennings B. Work stress and burnout among nurses: Role of the work environment and working conditions. In: Hughes R. G., editor. Patient safety and quality: An evidence-based handbook for nurses. Rockville, MD: Agency for Healthcare Research and Quality; 2008. pp. 2–137–2–158. (AHRQ Publication No. 08-0043, pp. Retrieved from http://www.ahrq.gov/qual/nurseshdbk/nurseshdbk.pdf. [PubMed] [Google Scholar]
- Kabat-Zinn J. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. New York, NY: Bantam Dell; 1990. [Google Scholar]
- Kabat-Zinn J. Mindfulness-based interventions in context: Past, present, and future. American Psychological Association. 2003;10(2):146–156. [Google Scholar]
- Klatt M. D., Buckworth J., Malarkey W. B. Effects of low-dose mindfulness-based stress reduction (MBSR-ld) on working adults. Health Education & Behavior: The Official Publication of the Society for Public Health Education. 2009;36(3):601–614. doi: 10.1177/1090198108317627. [DOI] [PubMed] [Google Scholar]
- Krasner M. S., Epstein R. M., Beckman H., Suchman A. L., Chapman B., Mooney C. J., Quill T. E. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. Journal of the American Medical Association. 2009;302:1284–1293. doi: 10.1001/jama.2009.1384. [DOI] [PubMed] [Google Scholar]
- Kreitzer M. J., Gross C. R., Waleekhachonloet O., Reilly-Spong M., Byrd M. The Brief Serenity Scale: A psychometric analysis of a measure of spirituality and well-being. Journal of Holistic Nursing. 2009;27(1):7–16. doi: 10.1177/0898010108327212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kristensen T. S., Borritz M., Villadsen E., Christensen K. B. The Copenhagen Burnout Inventory: A new tool for the assessment of burnout. Work & Stress. 2005;19:192–207. [Google Scholar]
- Larzelere M., Jones G. Stress and health. Primary Care: Clinics in Office Practice. 2008;35:839–856. doi: 10.1016/j.pop.2008.07.011. [DOI] [PubMed] [Google Scholar]
- Mackenzie C. S., Poulin P. A., Seidman-Carlson R. A brief mindfulness-based stress reduction intervention for nurses and nurse aides. Applied Nursing Research. 2006;19:105–109. doi: 10.1016/j.apnr.2005.08.002. [DOI] [PubMed] [Google Scholar]
- McCarney R., Schulz J., Grey R. Effectiveness of mindfulness-based interventions in reducing symptoms of depression: A meta-analysis. European Journal of Psychotherapy & Counseling. 2012;14(3):279–299. [Google Scholar]
- Neff K. D. The development and validation of a scale to measure self-compassion. Self and Identity. 2003;2:223–250. [Google Scholar]
- Newsome S., Waldo M., Gruszka C. Mindfulness group work: Preventing stress and increasing self-compassion among helping professions in training. Journal for Specialists in Group Work. 2012;37(4):297–311. [Google Scholar]
- Niles B. L., Vujanovic A. A., Silberbogen A. K., Seligowski A. V., Potter C. M. Changes in mindfulness following a mindfulness telehealth intervention. Mindfulness. 2012. pp. 1–10. Retrieved from http://link.springer.com/article/10.1007%2Fs12671-012-0130-5?LI=true#page-1.
- Parker C. P., Baltes B. B., Young S. A., Huff J. W., Altmann R. A., Lacost H. A., Roberts J. E. Relationships between psychological climate perceptions and work outcomes: A meta-analytic review. Journal of Organizational Behavior. 2003;24:389–416. [Google Scholar]
- Penque S. Mindfulness based stress reduction effects on registered nurses. 2009. (Unpublished doctoral dissertation). Retrieved from http://conservancy.umn.edu/bitstream/58728/1/Penque_umn_0130E_10859.pdf.
- Pipe T. B., Bortz J. J., Dueck A., Pendergast D., Buchda V., Summers J. Nurse leader mindfulness meditation program for stress management: A randomized controlled trial. Journal of Nursing Administration. 2009;39(3):130–137. doi: 10.1097/NNA.0b013e31819894a0. [DOI] [PubMed] [Google Scholar]
- Pollak K., Alexander S., Tulsky J., Lyna P., Coffman C., Dolor R., Ostbye R. Physician empathy and listening: Associations with patient satisfaction and autonomy. Journal of the American Board of Family Medicine. 2011;24:665–672. doi: 10.3122/jabfm.2011.06.110025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reb J., Narayan J., Chaturvedi S. Leading mindfully: Two studies on the influence of supervisor trait mindfulness on employee well-being and performance. Mindfulness. 2012. pp. 1–10. Retrieved from http://link.springer.com/article/10.1007%2Fs12671-012-0144-z?LI=true#page-1.
- Reibel D. K., Greeson J. M., Brainard G. C., Rosenzweig S. Mindfulness-based stress reduction and health-related quality of life in a heterogeneous patient population. General Hospital Psychiatry. 2001;23(4):183–192. doi: 10.1016/s0163-8343(01)00149-9. [DOI] [PubMed] [Google Scholar]
- Reynolds W., Scott P. A., Austin W. Nursing, empathy and the perception of the moral. Journal of Advanced Nursing. 2000;32(1):235–242. doi: 10.1046/j.1365-2648.2000.01440.x. [DOI] [PubMed] [Google Scholar]
- Roberts K., Whall A. Serenity as a goal for nursing practice. Image: The Journal of Nursing Scholarship. 1996;28(4):359–364. doi: 10.1111/j.1547-5069.1996.tb00388.x. [DOI] [PubMed] [Google Scholar]
- Sabo B. Reflecting on the concept of compassion fatigue. Online Journal of Issues in Nursing. 2011;16(1) doi: 10.3912/OJIN.Vol16No01Man01. Retrieved from http://www.nursingworld.org/MainMenuCategories/ANAMarketplace/ANAPeriodicals/OJIN/TableofContents/Vol-16-2011/No1-Jan-2011/Concept-of-Compassion-Fatigue.aspx. [DOI] [PubMed] [Google Scholar]
- Sansoucie D. A., Steckel A., Messina B. A., Greenfield J., Kealey C., Bratby K., Boughton S. The relationship between serenity and burnout among nurses. 2006, April. Paper presented at the Eastern Nursing Research Society 18th Annual Scientific Sessions, Philadelphia, PA.
- Scott L. D., Hwang W., Rogers A. E. The impact of multiple care giving roles on fatigue, stress, and work performance among hospital staff nurses. Journal of Nursing Administration. 2006;36:86–95. doi: 10.1097/00005110-200602000-00007. [DOI] [PubMed] [Google Scholar]
- Shapiro S. L., Astin J. A., Bishop S. R., Cordova M. Mindfulness-based stress reduction for health care professionals: Results from a randomized trial. International Journal of Stress Management. 2005;12:164–176. [Google Scholar]
- Shapiro S., Brown K. W., Biegel G. Teaching self-care to caregivers: Effects of mindfulness-based stress reduction on the mental health of therapists in training. Training and Education in Professional Psychology. 2007;1:105–115. [Google Scholar]
- Shapiro S. L., Schwartz G. E., Bonner G. Effects of mindfulness-based stress reduction on medical and premedical students. Journal of Behavioral Medicine. 1998;21(6):581–599. doi: 10.1023/a:1018700829825. [DOI] [PubMed] [Google Scholar]
- Sherr L. J. Moderators of the effectiveness of a mindfulness-based stress reduction intervention compared to an active control for solid organ transplant patients. 2010. (Unpublished doctoral dissertation). Retrieved from http://conservancy.umn.edu/bitstream/98006/1/Sherr_umn_0130E_11359.pdf.
- Ward J., Schaal M., Sullivan J., Bowen M. E., Erdmann J. B., Hojat M. Reliability and validity of the Jefferson Scale of Empathy in undergraduate nursing students. Journal of Nursing Measurement. 2009;17(1):73–88. doi: 10.1891/1061-3749.17.1.73. [DOI] [PubMed] [Google Scholar]
- Ware J. E., Jr., Kosinski M., Keller S. D. A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Medical Care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- Ware J., Kosinski M., Turner-Bowker D., Gandek B. SF-12, V2: How to score Version 2 of the SF-12 Health Survey. Lincoln, RI: Quality Metric Incorporated; 2002. [Google Scholar]
- Weinberg A., Creed F. Stress and psychiatric disorder in healthcare professionals and hospital staff. Lancet. 2000;355:533–537. doi: 10.1016/S0140-6736(99)07366-3. [DOI] [PubMed] [Google Scholar]
- Wolever R. Q., Bobinet K. J., McCabe K., Mackenzie E. R., Fekete E., Kusnick C. A., Baime M. Effective and viable mind-body stress reduction in the workplace: A randomized controlled trial. Journal of Occupational Health Psychology. 2012;17(2):246–258. doi: 10.1037/a0027278. [DOI] [PubMed] [Google Scholar]
- Zangaro G. A., Soeken K. L. A meta-analysis of studies of nurses’ Job satisfaction. Research in Nursing & Health. 2007;30(4):445–458. doi: 10.1002/nur.20202. [DOI] [PubMed] [Google Scholar]


