Abstract
Delirium is the most common neuropsychiatric complication seen in patients with cancer, and it is associated with significant morbidity and mortality. Increased health care costs, prolonged hospital stays, and long-term cognitive decline are other well-recognized adverse outcomes of delirium. Improved recognition of delirium and early treatment are important in diminishing such morbidity. There has been an increasing number of studies published in the literature over the last 10 years regarding delirium treatment as well as prevention. Antipsychotics, cholinesterase inhibitors, and alpha-2 agonists are the three groups of medications that have been studied in randomized controlled trials in different patient populations. In patients with cancer, the evidence is most clearly supportive of short-term, low-dose use of antipsychotics for controlling the symptoms of delirium, with close monitoring for possible adverse effects, especially in older patients with multiple medical comorbidities. Nonpharmacologic interventions also appear to have a beneficial role in the treatment of patients with cancer who have or are at risk for delirium. This article presents evidence-based recommendations based on the results of pharmacologic and nonpharmacologic studies of the treatment and prevention of delirium.
INTRODUCTION
Delirium is the most common and often serious neuropsychiatric complication seen in patients with cancer. It is well-recognized that delirium is associated with increased morbidity and mortality, increased length of hospitalization, higher health care costs, and significant distress in patients, family members, and professional caregivers.1–4 The presence of delirium can interfere with the recognition and control of physical and psychological symptoms such as pain.5,6 Delirium is often under-recognized or misdiagnosed in patients with cancer; even when recognized, it frequently goes untreated or is inappropriately treated. Clinicians who care for patients with cancer must be able to diagnose delirium accurately, undertake appropriate assessment of etiologies, and understand the risks and benefits of the pharmacologic and nonpharmacologic interventions currently available for managing delirium. This article reviews the best evidence available for pharmacologic and nonpharmacologic management of delirium in patients with cancer.
DELIRIUM PREVALENCE, ETIOLOGY, AND PATHOPHYSIOLOGY
The prevalence of delirium in cancer ranges from 10% to 30% in hospitalized patients and up to 85% in terminally ill patients with cancer.7 Among patients undergoing myeloablative hematopoietic stem-cell transplantation, delirium has been found to occur in up to 50% of patients during the 4 weeks after conditioning and stem-cell infusion.8 Delirium is caused by a significant physiologic disturbance, usually involving multiple medical etiologies among patients with cancer, including infections, organ failure, and adverse effects of medication.9–12 In patients with cancer, delirium can result either from the direct effects of cancer on the CNS (eg, metastatic brain lesions) or from indirect CNS effects of the disease or treatments (eg, medications, electrolyte imbalance, dehydration, major organ failure, infection, vascular complications, or paraneoplastic syndromes).7–13 Chemotherapeutic immunotherapeutic agents (eg, vincristine, corticosteroids, and interferon) and medications used in supportive care (eg, opioids, antiemetics, and benzodiazepines) may precipitate delirium in patients with cancer.7–13 Use of opioids and cognitive, liver, or renal impairment have been identified as major risk factors for delirium in patients with advanced cancer and in patients undergoing hematopoietic stem-cell transplantation.8–10 Despite many different etiologies, symptoms of delirium are largely stereotypical with a set of core symptoms. It appears that this diversity of physiologic disturbances translates into a common clinical expression that may relate to dysfunction of a final common pathway primarily involving the prefrontal cortex, posterior parietal cortex, and anteromedial thalamus, with an imbalance in the neurotransmitters acetylcholine and dopamine.14–16
DELIRIUM ASSESSMENT: DIAGNOSTIC FEATURES AND PHENOMENOLOGY
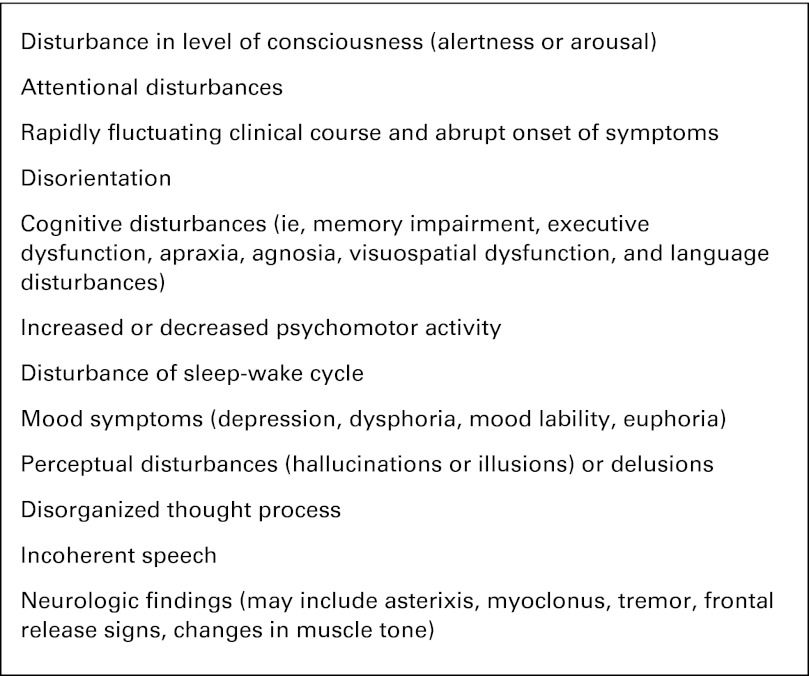
Delirium is characterized by an abrupt onset of disturbances of consciousness (ie, arousal), attention, cognition, and perception that fluctuate over the course of the day.7 The clinical features of delirium are numerous and include a variety of neuropsychiatric symptoms that are also common to other psychiatric disorders, such as depression, cognitive disturbances, and psychotic symptoms (Fig 1).7,13,17 Clinically, the diagnostic gold standard for delirium is the clinician's assessment using Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR) criteria.18
Fig 1.
Clinical features of delirium in patients with cancer. Adapted from Breitbart and Alici.7
Several delirium assessment tools, including the Memorial Delirium Assessment Scale (MDAS),19 the Delirium Rating Scale-Revised 98 (DRS-R-98),20 and the Confusion Assessment Method (CAM),21 have been validated in patients with cancer and are used to maximize diagnostic precision for clinical and research purposes and to assess delirium severity.19–22
Cognitive impairment was found to be the most common symptom noted in phenomenology studies.23 Three clinical subtypes of delirium based on psychomotor behavior and level of arousal have been described: the hyperactive (or hyperalert) subtype, the hypoactive (or hypoalert or hypoaroused) subtype, and a mixed subtype with alternating features of each.24 The hypoactive subtype is characterized by psychomotor retardation, lethargy, and reduced awareness of surroundings.24 The hyperactive subtype is commonly characterized by restlessness, agitation, hypervigilance, hallucinations, and delusions.24 A recent phenomenology study showed that although perceptual disturbances and delusions were more prevalent in hyperactive (70.2% and 78.7%, respectively) than in hypoactive (50.9% and 43.4%, respectively) delirium, the prevalence of perceptual disturbances and delusions in hypoactive delirium was much higher than previously reported and is deserving of clinical attention and intervention.17 There is evidence suggesting that the subtypes of delirium may be related to different causes and may have different treatment responses and prognosis.23–27 Hypoactive delirium has generally been found to be due to hypoxia, metabolic disturbances, or hepatic encephalopathies.24 Hyperactive delirium is correlated with alcohol and drug withdrawal, drug intoxication, or adverse effects of medication.24 The hypoactive subtype of delirium is associated with higher mortality risk compared with hyperactive delirium24,28 (see Pharmacologic Interventions in the Treatment of Delirium for a description of the differences in treatment responses).
DELIRIUM ASSESSMENT: DIAGNOSTIC WORKUP
The diagnostic workup of delirium should include an assessment of potentially reversible causes of delirium.13,29 The clinician should obtain a detailed history from family and staff of the patient's baseline mental status and verify the current fluctuating mental status.13 It is important to inquire about alcohol or other substance use disorders in hospitalized patients with cancer to be able to recognize and appropriately treat delirium associated with alcohol or other substance-induced withdrawal symptoms.7,13 Medications that could contribute to delirium should be reviewed, particularly opioid analgesics, benzodiazepines, and anticholinergic drugs, in the elderly and in the terminally ill.7,13,29,30 Predisposing delirium risk factors should be reviewed in detail, including old age, physical frailty, multiple medical comorbidities, dementia, admission to the hospital with infection or dehydration, visual impairment, deafness, polypharmacy, renal impairment, and malnutrition.3 A screen of laboratory parameters will allow assessment of the possible role of metabolic abnormalities, such as hypercalcemia, and other problems, such as hypoxia or disseminated intravascular coagulation.7,13,29 In some instances, an EEG (to rule out seizures), brain imaging studies (to rule out brain metastases, intracranial bleeding, or ischemia), or lumbar puncture (to rule out leptomeningeal carcinomatosis or meningitis) may be appropriate.7,13
TREATMENT OF DELIRIUM IN PATIENTS WITH CANCER
The standard approach to treating delirium in patients with cancer, even in those with advanced disease, includes a search for underlying causes, correction of those factors, and concurrent management of the symptoms of delirium (by using both pharmacologic and nonpharmacologic strategies).13 Modifiable predisposing risk factors (eg, visual impairment, malnutrition, dehydration, and polypharmacy) should be identified and corrected diligently.3 Treatment of the symptoms of delirium should be initiated before, or in concert with, a diagnostic assessment of the etiologies to minimize distress to patients, staff, and family members.7,13 The desired and often achievable outcome is a patient who is awake, alert, calm, comfortable, not in pain, cognitively intact, not psychotic, and communicating coherently with family and staff.7 In the terminally ill patient who develops delirium in the last days of life, the management of delirium is unique, presenting several dilemmas, and the desired clinical outcome may be significantly altered by the dying process.7 The goal of care in the terminally ill may shift to providing comfort through the judicious use of sedatives, even at the expense of alertness.7
Pharmacologic Interventions in the Treatment of Delirium
Treatment with psychotropic medications is often necessary to control the symptoms of delirium in patients with cancer. Antipsychotics, cholinesterase inhibitors, and alpha-2 agonists represent the main classes of medications studied in the treatment and prevention of delirium. No medication has been approved by the US Food and Drug Administration (FDA) for treatment or prevention of delirium to date.
Antipsychotics.
Formerly known as neuroleptics, antipsychotics are a group of medications primarily indicated for schizophrenia, bipolar disorder, and other mood disorders. The mechanisms by which these drugs ameliorate disturbances of thought and affect in psychotic states are not fully understood, but presumably they act by blocking the postsynaptic mesolimbic dopamine receptors. Typical (conventional or first-generation) and atypical (second-generation) antipsychotics differ in their effects on the different dopamine and serotonin receptor subtypes. Typical antipsychotics are traditionally known to be associated with a higher incidence of extrapyramidal adverse effects because of their effects on the striatal dopamine D2 receptors. Atypical antipsychotics have lower affinity and occupancy for the dopaminergic receptors and a high degree of occupancy of the serotoninergic receptors. Conversely, atypical antipsychotics (ie, risperidone, olanzapine, quetiapine, ziprasidone, and aripiprazole) have been associated with weight gain (appetite-stimulating effects are sometimes a benefit in cachectic patients with cancer) and metabolic syndrome but significantly less risk for extrapyramidal adverse effects.
Antipsychotic medications: Review of the efficacy of antipsychotics in the treatment of delirium.
There have been case reports, case series, retrospective chart reviews, open-label trials, randomized controlled comparison trials and, most recently, placebo-controlled trials with both typical and atypical antipsychotics in the treatment of delirium.25–27,31–42 Study populations primarily include general medically ill patients, postoperative patients, and patients in intensive care unit (ICU) settings; only a few focus specifically on populations of patients with cancer. Table 1 presents a summary of the open-label and randomized controlled trials with antipsychotics in the treatment of patients with cancer who have delirium and was based on a comprehensive search of PubMed by using the search terms “delirium,” “cancer,” “treatment,” and “antipsychotic” from 1960 through November 2011. Almost a dozen open-label and a total of five randomized controlled studies have been conducted with antipsychotics in nononcology settings; a review of those studies can be found elsewhere.31,43
Table 1.
Open-Label and RCTs of Antipsychotics in Treatment of Delirium in Patients With Cancer
| Trial Type | Intervention | Mean Dose (SD) and Duration | Results | Comments |
|---|---|---|---|---|
| Open-label | ||||
| Breitbart et al26 | Open-label trial of hospitalized patients (n = 79) with advanced cancer with delirium who were treated with olanzapine. | Average starting dose was in the 2.5-5 mg range, and patients were given up to 20 mg/d olanzapine. | Olanzapine was effective in resolving delirium in 76% of patients with no incidence of extrapyramidal adverse effects. The mean MDAS scores declined from 19.85 to 10.78 in 7 days. | Sedation was the most common adverse effect. Factors found to be significantly associated with poorer response to olanzapine for treatment of delirium were age older than 70 years, history of dementia, and hypoactive delirium. |
| Kim et al42 | Open-label trial of patients (n = 12; most with leukemia) with delirium who were treated with quetiapine. | Average dose was 93.75 mg. Mean duration for stabilization was 5.91 days. Quetiapine dose was tapered down about 1 month after discharge from the hospital. | The DRS scores declined from 18.25 to 8.00. | None of the patients experienced any Parkinsonian adverse effects; sedation and vivid dreaming were the only reported adverse effects. |
| Elsayem et al40 | Open-label trial of patients (n = 24) with advanced cancer with delirium who were treated with subcutaneous olanzapine. | Patients received olanzapine 5 mg subcutaneously every 8 hours for 3 days and continued with haloperidol for breakthrough agitation. | Efficacy was achieved in nine patients (37.5%). Subcutaneous olanzapine was well tolerated in the treatment of delirium. | No injection site toxicity was observed after 167 injections. Probable adverse effects were observed in four patients (severe hypotension [blood pressure < 90/50 mmHg], paradoxical agitation, diabetes insipidus, and seizure). |
| Boettger et al25 | Prospective, case-matched control comparison trial of patients with cancer who had delirium and were treated with aripiprazole (n = 21) v haloperidol (n = 21). | Mean aripiprazole dose was 15.2 mg at study entry and 18.3 mg at the end. Mean haloperidol dose was 4.9 mg at study entry and 5.5 mg at the end. | Over the course of treatment, MDAS scores improved from 18.1 to 8.3 for aripiprazole and 19.9 to 6.8 for haloperidol. The delirium resolution rate was 76.2% for aripiprazole and 76.2% for haloperidol. | There were no significant differences in treatment results between aripiprazole and haloperidol for patients with cancer with either hypoactive or hyperactive subtypes of delirium. However, there was a trend for poor response to aripiprazole among patients with hyperactive delirium. Treatment with haloperidol resulted in more extrapyramidal adverse effects. |
| Randomized controlled | ||||
| Breitbart et al27 | Double-blind RCT of terminally ill patients with AIDS with delirium who were treated with haloperidol (n = 11), chlorpromazine (n = 13), or lorazepam (n = 6). | 1.4 (1.2) mg/d haloperidol, 36 (18.4) mg/d chlorpromazine, 4.6 (4.7) mg/d lorazepam for up to 6 days. | DRS scores significantly improved in haloperidol and chlorpromazine groups (P < .05). No significant extrapyramidal symptoms were observed. | Lorazepam group was discontinued early because of worsening of delirium symptoms. |
| Hu et al35 | Double-blind RCT of hospitalized patients with delirium who were treated with olanzapine (n = 75), intramuscular haloperidol (n = 72), or oral placebo (n = 29). | 4.5 (4) mg/d olanzapine, 7 (2.3) mg/d haloperidol, and placebo for 7 days. | The improvement in DRS scores was significantly higher in the olanzapine (72%) and haloperidol (70%) groups v placebo (29.7%; P < .01). Increased rates of extrapyramidal symptoms were observed in the haloperidol group. | Comparison of oral olanzapine and oral placebo with intramuscular haloperidol hinders the quality of double-blind study design. |
| Kim et al41 | A randomized, single-blind clinical trial of mostly oncology patients with delirium comparing the effectiveness of treatment with risperidone (n = 17) and olanzapine (n = 15). | Study period: 7 days. Mean starting dose was 0.6 (0.2) mg/d risperidone and 1.8 (0.6) mg/d olanzapine. Mean dose at last observation was 0.9 (0.6) mg/d risperidone and 2.4 (1.7) mg/d olanzapine. | Significant within-group improvements in the DRS-R-98 scores over time were observed in both treatment groups; the response (defined as a 50% reduction in the DRS-R-98 scores) rates did not differ significantly between the two groups (risperidone group: 64.7%; olanzapine group: 73.3%). | The response to risperidone was significantly poorer in patients age 70 years or older compared with those younger than age 70 years. There was no significant difference in the safety profiles, including extrapyramidal symptoms, between the two groups. |
Abbreviations: DRS, Delirium Rating Scale; DRS-R-98, DRS-Revised 98; MDAS, Memorial Delirium Assessment Scale; RCT, randomized controlled trial; SD, standard deviation.
Despite the growing number of studies with antipsychotics for the treatment of the symptoms of delirium, there are several limitations to the published studies that should be taken into account. Retrospective studies are clearly limited in the accurate assessment of treatment efficacy and adverse effects. Open-label study designs are also of limited value in that selection bias cannot be ruled out. Common problems in most delirium trials include small sample size, heterogeneous samples, lack of systematic assessment of adverse effects, lack of use of valid adverse effect rating scales, lack of differentiation between subtypes of delirium, and the lack of controls for use of additional psychotropic agents as needed. Placebo-controlled randomized trials in the treatment of delirium should also be interpreted with caution.37–39 Although some were well-conducted studies and used validated and reliable delirium screening tools, others involved too few patients to reliably detect differences between treatment arms for important clinical outcomes, such as delirium resolution, mortality, or hospital length of stay.
Antipsychotic medications: Review of the adverse effects of antipsychotics.
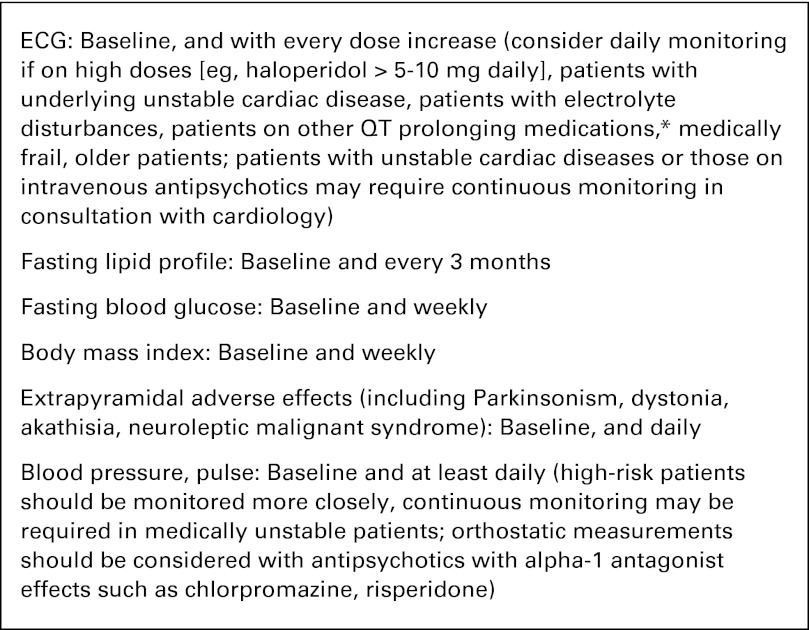
Important considerations in starting treatment with any antipsychotic for delirium should include risk of extrapyramidal adverse effects, sedation, anticholinergic adverse effects, cardiac arrhythmias, and possible drug-drug interactions (Fig 2). Despite its widespread use, especially in postoperative patients and in ICU settings, there is an FDA warning on the risk of QTc prolongation and torsades de pointes with the use of intravenous haloperidol. Therefore, monitoring QTc intervals at least daily among medically ill patients receiving intravenous haloperidol has become the standard clinical practice.47 The FDA has issued a black box warning of increased risk of death when antipsychotics are used to treat elderly patients with dementia-related psychoses. Initial warning for atypical antipsychotics was based on a meta-analysis by Schneider et al48 of 17 placebo-controlled trials involving patients with dementia. The risk of death in patients treated with atypical antipsychotic agents was 1.6 to 1.7 times greater than in those who received placebo. Most deaths were associated with cardiovascular disease or infection. A second retrospective study of nearly 23,000 older patients found higher mortality rates associated with typical than with atypical antipsychotics—whether or not the patients had dementia.49 This finding has led to an extension of the FDA warning for typical antipsychotics.50 Caution is advised when using antipsychotic medications especially in elderly patients with dementia. A retrospective case-control analysis of 326 elderly hospitalized patients with delirium at an acute care community hospital compared risk of mortality among patients who received an antipsychotic versus those who did not; it showed that of the 111 patients who received an antipsychotic, a total of 16 patients died during that hospitalization. The odds ratio (OR) of association between antipsychotic use and death was 1.53 (95% CI, 0.83 to 2.80) in univariate and 1.61 (95% CI, 0.88 to 2.96) in multivariate analysis. The researchers concluded that among elderly medical inpatients with delirium, administration of antipsychotics was not associated with a statistically significant increased risk of mortality.51 However, larger studies are needed to clarify this conclusion.
Fig 2.
Recommendations on monitoring patients with cancer who have delirium for antipsychotic adverse effects. Recommendations are based on the Consensus Development Conference on antipsychotic drugs and obesity and diabetes.44 (*) The risk of QT prolongation is directly correlated with higher antipsychotic doses, with parenteral formulations (eg, intravenous haloperidol) of antipsychotics, and with certain medications (eg, ziprasidone, thioridazine).45 In individual patients, an absolute QTc interval of 500 ms or an increase of 60 ms (or more than 20%) from baseline is regarded as indicating an increased risk of torsades des pointes.46 Discontinuation of the antipsychotic and a consultation with a cardiologist should be considered, especially if there is continued need for the use of antipsychotics.
It is important to recognize that antipsychotics have complex mechanisms of action, mostly affecting multiple neurotransmitter systems that can lead to unwanted adverse effects. Therefore, the benefits of initiating antipsychotic treatment for delirium should be weighed against risks associated with their use.
Antipsychotic medications: Evidence-based recommendations for the use of antipsychotics in the treatment of delirium.
The American Psychiatric Association (APA) practice guidelines published in 1999 recommended the use of antipsychotics as the first-line pharmacologic option in the treatment of symptoms of delirium.13
A 2004 Cochrane review on drug therapy for delirium in the terminally ill33 concluded that haloperidol was the most suitable medication for the treatment of patients with delirium near the end of life, with chlorpromazine being an acceptable alternative. A 2007 Cochrane review comparing the efficacy and the incidence of adverse effects between haloperidol and atypical antipsychotics concluded that, like haloperidol, selected atypical antipsychotics (risperidone and olanzapine) were effective in managing delirium.32 Haloperidol doses greater than 4.5 mg/d resulted in increased rates of extrapyramidal symptoms compared with the atypical antipsychotics, but low-dose haloperidol (ie, < 3.5 mg/d) was not shown to result in a greater frequency of extrapyramidal adverse effects.32,34,35
Despite the limitations noted for antipsychotic medication trials in the treatment of deliriumin the Antipsychotic Medications: Review of the Efficacy of Antipsychotics in the Treatment of Delirium section, the evidence to date suggests that antipsychotic medications are effective in improving or resolving the symptoms of delirium in populations of medically ill patients and those with cancer.
Our review supports the recommendations of the APA guidelines13 for the management of delirium in that low-dose haloperidol (ie, 1 to 2 mg orally every 4 hours as needed or 0.25 to 0.5 mg orally every 4 hours for the elderly) continues to be the first-line agent for treatment of symptoms of delirium. Our review also supports the Cochrane review32 conclusion that atypical antipsychotics (eg, olanzapine and risperidone) should be considered as effective alternatives to haloperidol, particularly in patients who are sensitive to or intolerant of haloperidol. None of the antipsychotics were found to be superior when compared with others in the treatment of delirium symptoms, and there is evidence for efficacy in the improvement of the symptoms of delirium for the following atypical antipsychotics: olanzapine, risperidone, aripiprazole, and quetiapine. Evidence suggests that the subtypes of delirium may have different treatment responses. A randomized controlled trial of haloperidol and chlorpromazine found that both medications were equally effective in hypoactive and hyperactive subtypes of delirium.27 However, two open-label trials showed different treatment responses to different antipsychotics. In one open-label trial,26 the hypoactive subtype was associated with poorer treatment response to olanzapine. Another open-label study25 suggested that the hypoactive subtype of delirium was associated with better response to treatment with aripiprazole. Table 2 presents a list of the antipsychotic medications and dosages recommended for use in the treatment of delirium.
Table 2.
Antipsychotic Medications Used Clinically in the Treatment of Delirium*
| Medication | Dose Range | Route of Administration | Adverse Effects | Comments |
|---|---|---|---|---|
| Typical antipsychotics | ||||
| Haloperidol | 0.5-2 mg every 2 to 12 hours | PO, IV, IM, SC | Extrapyramidal adverse effects can occur at higher doses. Monitor QT interval on ECG. | Remains the gold standard therapy for delirium. May add lorazepam (0.5-1 mg every 2 to 4 hours) for agitated patients. |
| Chlorpromazine | 12.5-50 mg every 4 to 6 hours | PO, IV, IM, SC, PR | More sedating and anticholinergic adverse effects compared with haloperidol. Monitor blood pressure for hypotension. More suitable for use in ICU settings for closer monitoring of blood pressure. | May be preferred in agitated patients because of its sedative effect. |
| Atypical antipsychotics | ||||
| Olanzapine | 2.5-5 mg every 12 to 24 hours | PO,† IM | Sedation is the main dose-limiting adverse effect in short-term use. | Older age, pre-existing dementia, and hypoactive subtype of delirium have been associated with poor response. |
| Risperidone | 0.25-1 mg every 12 to 24 hours | PO† | Extrapyramidal adverse effects can occur with doses > 6 mg/d. Orthostatic hypotension. | May be associated with orthostatic hypotension. |
| Quetiapine | 12.5-100 mg every 12 to 24 hours | PO | Sedation, orthostatic hypotension. | Sedating effects may be helpful in patients with sleep-wake cycle disturbance. |
| Ziprasidone | 10-40 mg every 12 to 24 hours | PO, IM | Monitor QT interval on ECG. | The literature on QT prolongation with ziprasidone makes it the least preferred agent in the medically ill. |
| Aripiprazole | 5-30 mg every 24 hours | PO,† IM | Monitor for akathisia. | Evidence is limited. Might be more efficacious in patients with hypoactive subtype than the hyperactive subtype. |
Abbreviations: ICU, intensive care unit; IM, intramuscular; IV, intravenous; PO, oral; PR, per rectum; SC, subcutaneous.
Adapted from Breitbart and Alici.7
Risperidone, olanzapine, and aripiprazole are available in orally disintegrating tablets.
Psychostimulants.
Some clinicians have suggested that the hypoactive subtype of delirium may respond to psychostimulants such as methylphenidate or combinations of antipsychotics and psychostimulants or antipsychotics and wakefulness agents such as modafinil.7,52–54 Studies of the use of psychostimulants in treating delirium are limited to case reports and one open-label study52–54 that are supportive of their use in terminally ill patients with cancer with no significant adverse events.
Psychostimulants: Evidence-based recommendations for the use of psychostimulants in the treatment of delirium.
In the absence of further evidence, psychostimulants cannot be recommended at this time for the treatment of patients with cancer who have delirium. The risks of precipitating agitation and exacerbating psychotic symptoms should be carefully evaluated when psychostimulants are considered in the treatment of the hypoactive subtype of delirium in patients with cancer.
Cholinesterase inhibitors.
Impaired cholinergic function has been implicated as one of the final common pathways in the neuropathogenesis of delirium.15 Despite case reports of beneficial effects of donepezil and rivastigmine, a 2008 Cochrane review55 concluded that there is currently no evidence from controlled trials supporting the use of cholinesterase inhibitors in the treatment of delirium.
A small, double-blind, placebo-controlled trial that used rivastigmine to treat patients with delirium in general hospital settings failed to show any differences between rivastigmine and placebo groups in the duration of delirium.56 A recent European multicenter double-blind study57 in ICUs comparing rivastigmine and placebo for the treatment of delirium was stopped prematurely because of increased mortality in the rivastigmine group. No common cause of mortality could be identified among patients who died while being given rivastigmine.
Cholinesterase inhibitors: Evidence-based recommendations for the use of cholinesterase inhibitors in the treatment of delirium.
The use of cholinesterase inhibitors in delirium have not been studied in patients with cancer. On the basis of the existing evidence from general hospital and ICU settings, cholinesterase inhibitors cannot be recommended in the treatment of delirium.
Pharmacologic Interventions in the Prevention of Delirium
Given the high occurrence rates, high health care costs, and increased morbidity and mortality associated with delirium, effective strategies that prevent delirium should be a high priority for treating patients with cancer. Several researchers studied both pharmacologic and nonpharmacologic interventions in the prevention of delirium among older patient populations, particularly in surgical and ICU settings.58–70 However, there have been no delirium prevention trials with any of the pharmacologic agents in oncology settings to date. Antipsychotics, cholinesterase inhibitors, melatonin, and dexmedetomidine have been studied in the prevention of delirium in randomized controlled delirium prevention studies conducted in different settings.58,59,63–70
Evidence-based recommendations for the use of pharmacologic interventions in the prevention of delirium.
A 2007 Cochrane review61 of delirium prevention studies in different patient populations concluded that the evidence on effectiveness of interventions to prevent delirium was sparse; therefore, no recommendations could be made regarding the use of pharmacologic interventions for prevention of delirium. The following is a summary of the findings of the delirium prevention studies conducted in noncancer postoperative and ICU settings.
Antipsychotics.
A randomized controlled prevention trial66 with low-dose haloperidol found that it was not effective in reducing delirium incidence; however, it was shown to decrease delirium severity and duration. A delirium prevention trial67 among postoperative patients was suggestive of a decrease in delirium incidence with the prophylactic use of olanzapine; however, increase in the severity and duration of delirium with olanzapine in that study raised concerns. The positive results (decrease in delirium incidence) of a prevention trial with risperidone were reported to be imprecise in a deliberate review of delirium trials.68,69
Antipsychotics: Cholinesterase inhibitors.
Cholinesterase inhibitors were not found to be effective in reducing delirium incidence or severity on the basis of evidence from three different placebo-controlled prevention trials with donepezil and rivastigmine.58,59,70
Antipsychotics: Melatonin.
Melatonin has been suggested to play a role in the treatment of delirium through direct antioxidant and anti-inflammatory activity, in addition to its effects on the sleep-wake cycle. A small randomized, double-blind, placebo-controlled study65 suggested that low-dose melatonin (0.5 mg) administered nightly to elderly patients admitted to acute care units may represent a potential protective agent against development of delirium.
Antipsychotics: Alpha-2 agonists.
Dexmedetomidine, is a selective alpha-2 adrenergic receptor agonist that is indicated in the United States for the sedation of mechanically ventilated adult patients in ICU settings and in nonintubated adult patients before and/or during surgery and other procedures. Clinical trials with dexmedetomidine have shown mixed results for the prevention and treatment of delirium in the ICU setting.63,64 The potential use of dexmedetomidine in the palliative care population has been considered for the prevention and treatment of delirium and enhancing analgesia.71 However, to the best of our knowledge, there have not been any studies with dexmedetomidine in palliative care settings. It is important to note that none of the pharmacologic agents were studied specifically in patients with cancer in the prevention of delirium; therefore, no recommendations could be made regarding use of these medications in the prevention of delirium in oncology settings.
Nonpharmacologic Management of Delirium
Here, we review several nonpharmacologic intervention trials on the treatment and prevention of delirium among older patients in general medical and surgical settings.
Nonpharmacologic intervention studies on the treatment of delirium.
Two randomized trials that used systematic detection of delirium, geriatrician consultations, and a geriatric nurse specialist72,73 did not show a difference in mortality, functioning, discharge location, delirium duration, or length of hospital stays. A minor difference was noted in delirium severity. A multicomponent directed management trial of 174 geriatric patients with delirium74 failed to show any difference in mortality, length of stay, or rates of institutionalization, but delirium severity was lower in the intervention group. In an observational study of 148 patients with delirium,75 the use of a delirium room, described as a specialized restraint-free room with 24-hour nursing, was associated with improved functioning, and equal length of stay and mortality when those patients were compared with patients without delirium. Low implementation rates of all the components of the interventions were identified as the main limiting factor in interpreting the study results in a majority of the nonpharmacologic treatment trials.
Nonpharmacologic interventions for the prevention of delirium.
Several researchers have studied nonpharmacologic interventions in the prevention of delirium.60–62,76,77 Although only one such study by Gagnon et al78 conducted in patients with cancer demonstrated no benefit, several studies among hospitalized geriatric populations have shown promise.
Inouye et al60 studied the effectiveness of a multicomponent intervention for the prevention of delirium among patients age 70 years or older who had been admitted to the general medicine service at a teaching hospital. The intervention consisted of standardized protocols for the management of six risk factors for delirium: cognitive impairment, sleep deprivation, immobility, visual impairment, hearing impairment, and dehydration. Delirium was the primary outcome and was assessed daily until discharge. Of the 852 patients studied, delirium developed in 9.9% of the intervention group compared with 15.0% of the usual care group (matched OR, 0.60; 95% CI, 0.39 to 0.92). The total number of days with delirium (105 v 161 days; P = .02) and the total number of delirium episodes (62 v 90 episodes; P = .03) were significantly lower in the intervention group. However, the severity of delirium and recurrence rates were not significantly different. Intervention was associated with significant improvement in the degree of cognitive impairment among patients who had cognitive impairment at admission and a reduction in the rate of use of sleep medications among all patients. On the basis of the study findings, researchers concluded that primary prevention of delirium was probably the most effective treatment strategy. A randomized controlled trial of proactive geriatric consultations—making recommendations for nonpharmacologic interventions—in a population of patients undergoing surgery for hip fracture was found to be the only effective intervention in reducing incidence (32% v 50%) and severity of delirium.62
The applicability of a multicomponent intervention to prevent delirium in patients with cancer has been studied by Gagnon et al.78 A cohort of 1,516 patients was followed from admission to death at seven palliative care centers. In two of these centers, routine care included a delirium preventive intervention that targeted physicians (written notice on selective delirium risk factors and inquest on intended medication changes), patients, and their families (orientation to time and place, information about early delirium symptoms). Delirium frequency and severity were compared between patients at the intervention (n = 674) and usual care (n = 842) centers based on thrice daily symptom assessments with the Confusion Rating Scale. The overall rate of adherence to the intervention was 89.7%. The incidence of delirium was 49.1% in the intervention group compared with 43.9% in the usual care group (OR, 1.23; P = .045). When confounding variables were controlled for, no difference was observed between the intervention and the usual care groups in delirium incidence (OR, 0.94; P = .66), delirium severity (1.83 v 1.92; P = .07), total days in delirium (4.57 v 3.57 days; P = .63), or duration of first delirium episode (2.9 v 2.1 days; P = .96). Researchers concluded that a simple multicomponent preventive intervention was ineffective in reducing delirium incidence or severity among patients with cancer who were receiving end-of-life care.
Evidence-based recommendations for the use of nonpharmacologic interventions in the treatment and prevention of delirium.
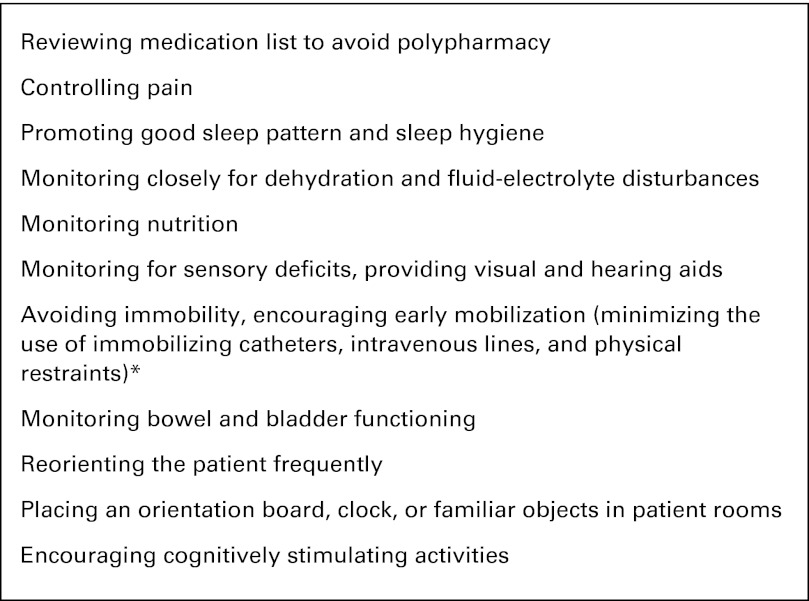
Nonpharmacologic and supportive therapies play an essential role in the treatment and prevention of delirium in patients with cancer. Assessment and modification of key clinical factors that may precipitate delirium for persons at risk for delirium, including cognitive impairment or disorientation, dehydration, constipation, hypoxia, infection, immobility or limited mobility, several medications, pain, poor nutrition, sensory impairment, and sleep disturbance, constitute the main components of nonpharmacologic intervention trials.
Although these interventions were not found to have any beneficial effects on mortality or health-related quality of life when compared with usual care, there is evidence that they result in faster improvement of delirium and slower deterioration in cognition especially among older patients with delirium in general hospital settings.72–75 Prevention trials60–62,76,77 yielded more encouraging results in reducing delirium incidence and decreasing delirium duration and severity in geriatric patient populations. The study effect sizes suggested statistically significant reductions in delirium incidence of about one third with multicomponent interventions.69 There was an inconsistent effect on reduction in hospital stay and no statistically significant effects on discharge to long-term care facilities, mortality, or duration and severity of delirium.69 Figure 3 is a summary of nonpharmacologic interventions used in the delirium treatment and prevention trials described in the Nonpharmacologic Management of Delirium section.
Fig 3.
Summary of nonpharmacologic interventions used in the prevention and treatment of delirium.60–62,69,72–77 (*) Physical restraints should be avoided both in patients who are at risk for developing delirium and in those who have delirium. The use of physical restraints has been identified as an independent risk factor for delirium persistence at the time of hospital discharge (Inouye, et al: Arch Intern Med 167:1406-1413, 2007). Restraint-free care should be the standard of care for prevention and treatment of delirium among cancer patients.
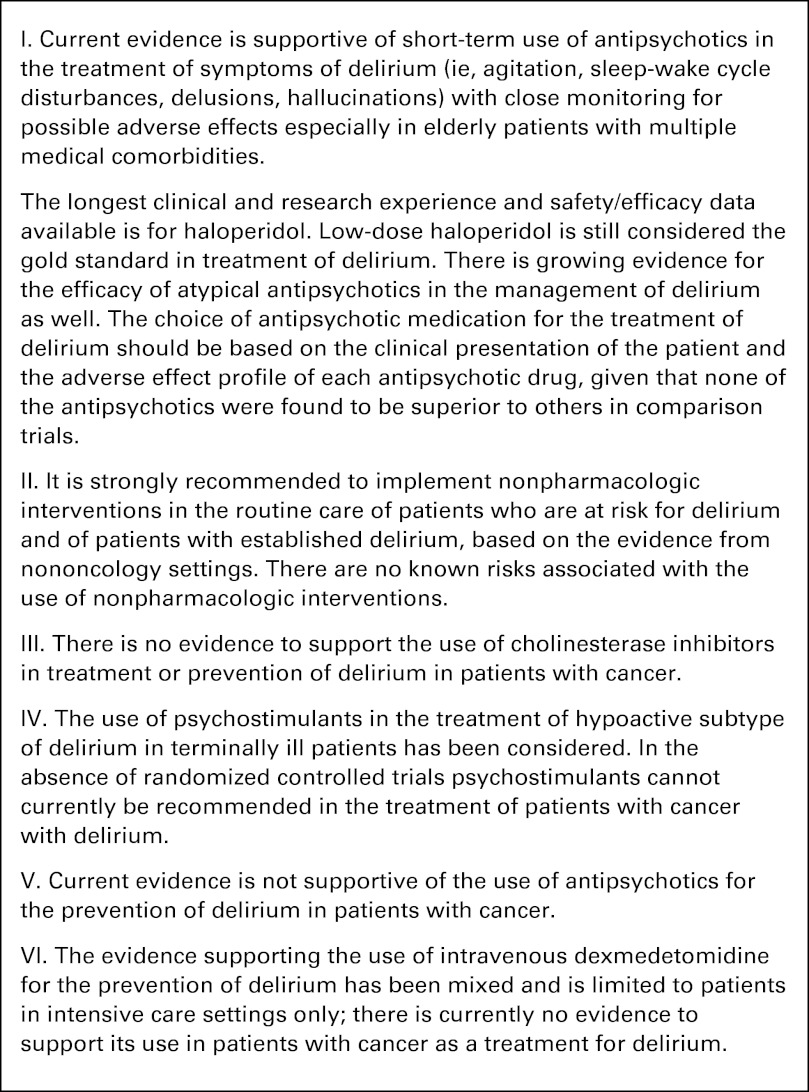
In conclusion, oncologists commonly encounter delirium as a major complication of cancer and its treatments, particularly among hospitalized patients with cancer. Proper assessment, diagnosis, and management of delirium are essential in improving quality of life and minimizing morbidity in patients with cancer. Figure 4 is a summary of the evidence-based management recommendations for patients with cancer who have or are at risk for delirium. The current evidence supports the use of pharmacologic agents to control symptoms of delirium, with the best evidence demonstrating efficacy for antipsychotics—low-dose haloperidol being the gold standard treatment for patients with cancer who have delirium. Current evidence does not support the use of psychostimulants or cholinesterase inhibitors for the treatment or prevention of delirium. Nonpharmacologic prevention strategies such as multicomponent intervention with multidisciplinary, educational, and proactive management of patients at risk for delirium are supported by the evidence-based literature in general hospital settings, especially among older patients. Evidence is not as strong for the use of nonpharmacologic interventions to minimize the morbidity of the symptoms of delirium. Although they may not be effective in controlling delirium symptoms, the use of nonpharmacologic interventions in patients with cancer who have delirium is recommended when feasible. There are no known risks associated with the use of nonpharmacologic interventions in patients who have delirium. The cost-effectiveness of these measures remains to be determined. Clinicians should try every possible measure to alleviate the well-documented patient, family, and caregiver distress associated with delirium in the oncology wards. The prophylactic use of antipsychotics, alpha-2 agonists, and melatonin in the prevention of delirium is one of the more interesting new frontiers of delirium management, and the evidence to date suggests some promise for olanzapine, risperidone, and melatonin in nononcology settings. The use of alpha-2 agonists in the prevention of delirium has shown mixed results in ICU settings. Larger, well-designed, placebo-controlled trials are required for any prophylactic drug recommendations to be made in patients with cancer who are at risk for delirium.
Fig 4.
Evidence-based management recommendations for patients with cancer with delirium.
Footnotes
Authors' disclosures of potential conflicts of interest and author contributions are found at the end of this article.
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The author(s) indicated no potential conflicts of interest.
AUTHOR CONTRIBUTIONS
Manuscript writing: All authors
Final approval of manuscript: All authors
REFERENCES
- 1.Breitbart W, Gibson C, Tremblay A. The delirium experience: Delirium recall and delirium-related distress in hospitalized patients with cancer, their spouses/caregivers, and their nurses. Psychosomatics. 2002;43:183–194. doi: 10.1176/appi.psy.43.3.183. [DOI] [PubMed] [Google Scholar]
- 2.Morita T, Hirai K, Sakaguchi Y, et al. Family-perceived distress from delirium-related symptoms of terminally ill cancer patients. Psychosomatics. 2004;45:107–113. doi: 10.1176/appi.psy.45.2.107. [DOI] [PubMed] [Google Scholar]
- 3.Inouye SK. Delirium in older persons. N Engl J Med. 2006;354:1157–1165. doi: 10.1056/NEJMra052321. [DOI] [PubMed] [Google Scholar]
- 4.Witlox J, Kalisvaart KJ, de Jonghe JF, et al. Cerebrospinal fluid β-amyloid and tau are not associated with risk of delirium: A prospective cohort study in older adults with hip fracture. J Am Geriatr Soc. 2011;59:1260–1267. doi: 10.1111/j.1532-5415.2011.03482.x. [DOI] [PubMed] [Google Scholar]
- 5.Bruera E, Fainsinger RL, Miller MJ, et al. The assessment of pain intensity in patients with cognitive failure: A preliminary report. J Pain Symptom Manage. 1992;7:267–270. doi: 10.1016/0885-3924(92)90060-u. [DOI] [PubMed] [Google Scholar]
- 6.Gagnon B, Lawlor PG, Mancini IL, et al. The impact of delirium on the circadian distribution of breakthrough analgesia in advanced cancer patients. J Pain Symptom Manage. 2001;22:826–833. doi: 10.1016/s0885-3924(01)00339-6. [DOI] [PubMed] [Google Scholar]
- 7.Breitbart W, Alici Y. Agitation and delirium at the end of life: “We couldn't manage him.”. JAMA. 2008;300:2898–2910. doi: 10.1001/jama.2008.885. [DOI] [PubMed] [Google Scholar]
- 8.Fann JR, Roth-Roemer S, Burington BE, et al. Delirium in patients undergoing hematopoietic stem cell transplantation. Cancer. 2002;95:1971–1981. doi: 10.1002/cncr.10889. [DOI] [PubMed] [Google Scholar]
- 9.Gaudreau JD, Gagnon P, Harel F, et al. Psychoactive medications and risk of delirium in hospitalized cancer patients. J Clin Oncol. 2005;23:6712–6718. doi: 10.1200/JCO.2005.05.140. [DOI] [PubMed] [Google Scholar]
- 10.Lawlor PG, Gagnon B, Mancini IL, et al. Occurrence, causes, and outcome of delirium in patients with advanced cancer: A prospective study. Arch Intern Med. 2000;160:786–794. doi: 10.1001/archinte.160.6.786. [DOI] [PubMed] [Google Scholar]
- 11.Morita T, Tei Y, Tsunoda J, et al. Underlying pathologies and their associations with clinical features in terminal delirium of cancer patients. J Pain Symptom Manage. 2001;22:997–1006. doi: 10.1016/s0885-3924(01)00360-8. [DOI] [PubMed] [Google Scholar]
- 12.Spiller JA, Keen JC. Hypoactive delirium: Assessing the extent of the problem for inpatient specialist palliative care. Palliat Med. 2006;20:17–23. doi: 10.1191/0269216306pm1097oa. [DOI] [PubMed] [Google Scholar]
- 13.Practice guideline for the treatment of patients with delirium: American Psychiatric Association. Am J Psychiatry. 1999;156:1–20. No authors listed. [PubMed] [Google Scholar]
- 14.Trzepacz PT, Sclabassi RJ, Van Thiel DH. Delirium: A subcortical phenomenon? J Neuropsychiatry Clin Neurosci. 1989;1:283–290. doi: 10.1176/jnp.1.3.283. [DOI] [PubMed] [Google Scholar]
- 15.Trzepacz PT. Is there a final common neural pathway in delirium? Focus on acetylcholine and dopamine. Semin Clin Neuropsychiatry. 2000;5:132–148. doi: 10.153/SCNP00500132. [DOI] [PubMed] [Google Scholar]
- 16.Maldonado JR. Pathoetiological model of delirium: A comprehensive understanding of the neurobiology of delirium and an evidence-based approach to prevention and treatment. Crit Care Clin. 2008;24:789–856. doi: 10.1016/j.ccc.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 17.Boettger S, Breitbart W. Phenomenology of the subtypes of delirium: Phenomenological differences between hyperactive and hypoactive delirium. Palliat Support Care. 2011;9:129–135. doi: 10.1017/S1478951510000672. [DOI] [PubMed] [Google Scholar]
- 18.American Psychiatric Association. Washington, DC: American Psychiatric Association Press; 2000. Diagnostic and Statistical Manual of Mental Disorders DSM-IV-TR (ed 4; Text Revision) [Google Scholar]
- 19.Breitbart W, Rosenfeld B, Roth A, et al. The Memorial Delirium Assessment Scale. J Pain Symptom Manage. 1997;13:128–137. doi: 10.1016/s0885-3924(96)00316-8. [DOI] [PubMed] [Google Scholar]
- 20.Trzepacz PT, Mittal D, Torres R, et al. Validation of the Delirium Rating Scale-revised-98: Comparison with the delirium rating scale and the cognitive test for delirium. J Neuropsychiatry Clin Neurosci. 2001;13:229–242. doi: 10.1176/jnp.13.2.229. [DOI] [PubMed] [Google Scholar]
- 21.Inouye SK, van Dyck CH, Alessi CA, et al. Clarifying confusion: The confusion assessment method—A new method for the detection of delirium. Ann Intern Med. 1990;113:941–948. doi: 10.7326/0003-4819-113-12-941. [DOI] [PubMed] [Google Scholar]
- 22.Smith MJ, Breitbart WS, Platt MM. A critique of instruments and methods to detect, diagnose, and rate delirium. J Pain Symptom Manage. 1994;10:35–77. doi: 10.1016/0885-3924(94)00066-T. [DOI] [PubMed] [Google Scholar]
- 23.Meagher DJ, Moran M, Raju B, et al. Motor symptoms in 100 patients with delirium versus control subjects: Comparison of subtyping methods. Psychosomatics. 2008;49:300–308. doi: 10.1176/appi.psy.49.4.300. [DOI] [PubMed] [Google Scholar]
- 24.Stagno D, Gibson C, Breitbart W. The delirium subtypes: A review of prevalence, phenomenology, pathophysiology, and treatment response. Palliat Support Care. 2004;2:171–179. doi: 10.1017/s1478951504040234. [DOI] [PubMed] [Google Scholar]
- 25.Boettger S, Friedlander M, Breitbart W, et al. Aripiprazole and haloperidol in the treatment of delirium. Aust N Z J Psychiatry. 2011;45:477–482. doi: 10.3109/00048674.2011.543411. [DOI] [PubMed] [Google Scholar]
- 26.Breitbart W, Tremblay A, Gibson C. An open trial of olanzapine for the treatment of delirium in hospitalized cancer patients. Psychosomatics. 2002;43:175–182. doi: 10.1176/appi.psy.43.3.175. [DOI] [PubMed] [Google Scholar]
- 27.Breitbart W, Marotta R, Platt MM, et al. A double-blind trial of haloperidol, chlorpromazine, and lorazepam in the treatment of delirium in hospitalized AIDS patients. Am J Psychiatry. 1996;153:231–237. doi: 10.1176/ajp.153.2.231. [DOI] [PubMed] [Google Scholar]
- 28.Kiely DK, Jones RN, Bergmann MA, et al. Association between psychomotor activity delirium subtypes and mortality among newly admitted post-acute facility patients. J Gerontol A Biol Sci Med Sci. 2007;62:174–179. doi: 10.1093/gerona/62.2.174. [DOI] [PubMed] [Google Scholar]
- 29.National Comprehensive Cancer Network Distress Management Panel Members. National Comprehensive Cancer Network (v. 1.2011) distress management—NCCN practice guidelines in oncology. http://www.nccn.org/professionals/physician_gls/pdf/distress.pdf. [DOI] [PMC free article] [PubMed]
- 30.Agar M, Currow D, Plummer J, et al. Changes in anticholinergic load from regular prescribed medications in palliative care as death approaches. Palliat Med. 2009;23:257–265. doi: 10.1177/0269216309102528. [DOI] [PubMed] [Google Scholar]
- 31.Boettger S, Breitbart W. Atypical antipsychotics in the management of delirium: A review of the empirical literature. Palliat Support Care. 2005;3:227–237. doi: 10.1017/s1478951505050352. [DOI] [PubMed] [Google Scholar]
- 32.Lonergan E, Britton AM, Luxenberg J, et al. Antipsychotics for delirium. Cochrane Database Syst Rev. 2007;2:CD005594. doi: 10.1002/14651858.CD005594.pub2. [DOI] [PubMed] [Google Scholar]
- 33.Jackson KC, Lipman AG. Drug therapy for delirium in terminally ill patients. Cochrane Database Syst Rev. 2004;2:CD004770. doi: 10.1002/14651858.CD004770. [DOI] [PubMed] [Google Scholar]
- 34.Han CS, Kim YK. A double-blind trial of risperidone and haloperidol for the treatment of delirium. Psychosomatics. 2004;45:297–301. doi: 10.1016/S0033-3182(04)70170-X. [DOI] [PubMed] [Google Scholar]
- 35.Hu H, Deng W, Yang H. A prospective random control study: Comparison of olanzapine and haloperidol in senile delirium. Chongqing Med J. 2004;8:1234–1237. [Google Scholar]
- 36.Grover S, Kumar V, Chakrabarti S. Comparative efficacy study of haloperidol, olanzapine and risperidone in delirium. J Psychosom Res. 2011;71:277–281. doi: 10.1016/j.jpsychores.2011.01.019. [DOI] [PubMed] [Google Scholar]
- 37.Girard TD, Pandharipande PP, Carson SS, et al. Feasibility, efficacy, and safety of antipsychotics for intensive care unit delirium: The MIND randomized, placebo-controlled trial. Crit Care Med. 2010;38:428–437. doi: 10.1097/ccm.0b013e3181c58715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Devlin JW, Roberts RJ, Fong JJ, et al. Efficacy and safety of quetiapine in critically ill patients with delirium: A prospective, multicenter, randomized, double-blind, placebo-controlled pilot study. Crit Care Med. 2010;38:419–427. doi: 10.1097/CCM.0b013e3181b9e302. [DOI] [PubMed] [Google Scholar]
- 39.Tahir TA, Eeles E, Karapareddy V, et al. A randomized controlled trial of quetiapine versus placebo in the treatment of delirium. J Psychosom Res. 2010;69:485–490. doi: 10.1016/j.jpsychores.2010.05.006. [DOI] [PubMed] [Google Scholar]
- 40.Elsayem A, Bush SH, Munsell MF, et al. Subcutaneous olanzapine for hyperactive or mixed delirium in patients with advanced cancer: A preliminary study. J Pain Symptom Manage. 2010;40:774–782. doi: 10.1016/j.jpainsymman.2010.02.017. [DOI] [PubMed] [Google Scholar]
- 41.Kim SW, Yoo JA, Lee SY, et al. Risperidone versus olanzapine for the treatment of delirium. Hum Psychopharmacol. 2010;25:298–302. doi: 10.1002/hup.1117. [DOI] [PubMed] [Google Scholar]
- 42.Kim KY, Bader GM, Kotlyar V, et al. Treatment of delirium in older adults with quetiapine. J Geriatr Psychiatry Neurol. 2003;16:29–31. doi: 10.1177/0891988702250533. [DOI] [PubMed] [Google Scholar]
- 43.Flaherty JH. The evaluation and management of delirium among older persons. Med Clin North Am. 2011;95:555–577. doi: 10.1016/j.mcna.2011.02.005. [DOI] [PubMed] [Google Scholar]
- 44.American Diabetes Association. American Psychiatric Association. American Association of Clinical Endocrinologists et al. Consensus development conference on antipsychotic drugs and obesity and diabetes. Diabetes Care. 2004;27:596–601. doi: 10.2337/diacare.27.2.596. [DOI] [PubMed] [Google Scholar]
- 45.Harrigan EP, Miceli JJ, Anziano R, et al. A randomized evaluation of the effects of six antipsychotic agents on QTc, in the absence and presence of metabolic inhibition. J Clin Psychopharmacol. 2004;24:62–69. doi: 10.1097/01.jcp.0000104913.75206.62. [DOI] [PubMed] [Google Scholar]
- 46.Haddad PM, Anderson IM. Antipsychotic-related QTc prolongation, torsade de pointes and sudden death. Drugs. 2002;62:1649–1671. doi: 10.2165/00003495-200262110-00006. [DOI] [PubMed] [Google Scholar]
- 47.US Food and Drug Administration. Information for healthcare professionals: Haloperidol (marketed as Haldol, Haldol Decanoate and Haldol Lactate) http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/DrugSafetyInformationforHeathcareProfessionals/ucm085203.htm.
- 48.Schneider LS, Dagerman KS, Insel P. Risk of death with atypical antipsychotic drug treatment for dementia: Meta-analysis of randomized placebo-controlled trials. JAMA. 2005;294:1934–1943. doi: 10.1001/jama.294.15.1934. [DOI] [PubMed] [Google Scholar]
- 49.Wang PS, Schneeweiss S, Avorn J, et al. Risk of death in elderly users of conventional vs atypical antipsychotic medications. N Engl J Med. 2005;353:2335–2341. doi: 10.1056/NEJMoa052827. [DOI] [PubMed] [Google Scholar]
- 50.US Food and Drug Administration. Information for healthcare professionals: Conventional Antipsychotics. http://www.fda.gov/drugs/drugsafety/postmarketdrugsafetyinformationforpatientsandproviders/ucm124830.htm.
- 51.Elie M, Boss K, Cole MG, et al. A retrospective, exploratory, secondary analysis of the association between antipsychotic use and mortality in elderly patients with delirium. Int Psychogeriatr. 2009;21:588–592. doi: 10.1017/S1041610209008977. [DOI] [PubMed] [Google Scholar]
- 52.Gagnon B, Low G, Schreier G. Methylphenidate hydrochloride improves cognitive function in patients with advanced cancer and hypoactive delirium: A prospective clinical study. J Psychiatry Neurosci. 2005;30:100–107. [PMC free article] [PubMed] [Google Scholar]
- 53.Keen JC, Brown D. Psychostimulants and delirium in patients receiving palliative care. Palliat Support Care. 2004;2:199–202. doi: 10.1017/s147895150404026x. [DOI] [PubMed] [Google Scholar]
- 54.Morita T, Otani H, Tsunoda J, et al. Successful palliation of hypoactive delirium due to multi-organ failure by oral methylphenidate. Support Care Cancer. 2000;8:134–137. doi: 10.1007/s005200050028. [DOI] [PubMed] [Google Scholar]
- 55.Overshott R, Karim S, Burns A. Cholinesterase inhibitors for delirium. Cochrane Database Syst Rev. 2008;1:CD005317. doi: 10.1002/14651858.CD005317.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Overshott R, Vernon M, Morris J, et al. Rivastigmine in the treatment of delirium in older people: A pilot study. Int Psychogeriatr. 2010;22:812–818. doi: 10.1017/S1041610209991359. [DOI] [PubMed] [Google Scholar]
- 57.van Eijk MM, Roes KC, Honing ML, et al. Effect of rivastigmine as an adjunct to usual care with haloperidol on duration of delirium and mortality in critically ill patients: A multicentre, double-blind, placebo-controlled randomised trial. Lancet. 2010;376:1829–1837. doi: 10.1016/S0140-6736(10)61855-7. [DOI] [PubMed] [Google Scholar]
- 58.Liptzin B, Laki A, Garb JL, et al. Donepezil in the prevention and treatment of post-surgical delirium. Am J Geriatr Psychiatry. 2005;13:1100–1106. doi: 10.1176/appi.ajgp.13.12.1100. [DOI] [PubMed] [Google Scholar]
- 59.Sampson EL, Raven PR, Ndhlovu PN, et al. A randomized, double-blind, placebo-controlled trial of donepezil hydrochloride (Aricept) for reducing the incidence of postoperative delirium after elective total hip replacement. Int J Geriatr Psychiatry. 2007;22:343–349. doi: 10.1002/gps.1679. [DOI] [PubMed] [Google Scholar]
- 60.Inouye SK, Bogardus ST, Jr, Charpentier PA, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999;340:669–766. doi: 10.1056/NEJM199903043400901. [DOI] [PubMed] [Google Scholar]
- 61.Siddiqi N, Stockdale R, Britton AM, et al. Interventions for preventing delirium in hospitalised patients. Cochrane Database Syst Rev. 2007;2:CD005563. doi: 10.1002/14651858.CD005563.pub2. [DOI] [PubMed] [Google Scholar]
- 62.Marcantonio ER, Flacker JM, Wright RJ, et al. Reducing delirium after hip fracture: A randomized trial. J Am Geriatr Soc. 2001;49:516–522. doi: 10.1046/j.1532-5415.2001.49108.x. [DOI] [PubMed] [Google Scholar]
- 63.Pandharipande PP, Sanders RD, Girard TD, et al. Effect of dexmedetomidine versus lorazepam on outcome in patients with sepsis: An a priori-designed analysis of the MENDS randomized controlled trial. Crit Care. 2010;14:R38. doi: 10.1186/cc8916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Riker RR, Shehabi Y, Bokesch PM, et al. Dexmedetomidine vs midazolam for sedation of critically ill patients: A randomized trial. JAMA. 2009;301:489–499. doi: 10.1001/jama.2009.56. [DOI] [PubMed] [Google Scholar]
- 65.Al-Aama T, Brymer C, Gutmanis I, et al. Melatonin decreases delirium in elderly patients: A randomized, placebo-controlled trial. Int J Geriatr Psychiatry. 2011;26:687–694. doi: 10.1002/gps.2582. [DOI] [PubMed] [Google Scholar]
- 66.Kalisvaart KJ, de Jonghe JF, Bogaards MJ, et al. Haloperidol prophylaxis for elderly hip-surgery patients at risk for delirium: A randomized placebo-controlled study. J Am Geriatr Soc. 2005;53:1658–1666. doi: 10.1111/j.1532-5415.2005.53503.x. [DOI] [PubMed] [Google Scholar]
- 67.Larsen KA, Kelly SE, Stern TA, et al. Administration of olanzapine to prevent postoperative delirium in elderly joint-replacement patients: A randomized, controlled trial. Psychosomatics. 2010;51:409–418. doi: 10.1176/appi.psy.51.5.409. [DOI] [PubMed] [Google Scholar]
- 68.Prakanrattana U, Prapaitrakool S. Efficacy of risperidone for prevention of postoperative delirium in cardiac surgery. Anaesth Intensive Care. 2007;35:714–719. doi: 10.1177/0310057X0703500509. [DOI] [PubMed] [Google Scholar]
- 69.National Institute for Health and Clinical Excellence. Delirium: Diagnosis, prevention and management (NICE clinical guideline 103) 2010. Jul, www.nice.org.uk/nicemedia/live/13060/49909/49909.pdf.
- 70.Gamberini M, Bolliger D, Lurati Buse GA, et al. Rivastigmine for the prevention of postoperative delirium in elderly patients undergoing elective cardiac surgery: A randomized controlled trial. Crit Care Med. 2009;37:1762–1768. doi: 10.1097/CCM.0b013e31819da780. [DOI] [PubMed] [Google Scholar]
- 71.Prommer E. Review article: Dexmedetomidine: Does it have potential in palliative medicine? Am J Hosp Palliat Care. 2011;28:276–283. doi: 10.1177/1049909110389804. [DOI] [PubMed] [Google Scholar]
- 72.Cole MG, Primeau FJ, Bailey RF, et al. Systematic intervention for elderly inpatients with delirium: A randomized trial. CMAJ. 1994;151:965–970. [PMC free article] [PubMed] [Google Scholar]
- 73.Cole MG, McCusker J, Bellavance F, et al. Systematic detection and multidisciplinary care of delirium in older medical inpatients: A randomized trial. CMAJ. 2002;167:753–759. [PMC free article] [PubMed] [Google Scholar]
- 74.Pitkälä KH, Laurila JV, Strandberg TE, et al. Multicomponent geriatric intervention for elderly inpatients with delirium: A randomized, controlled trial. J Gerontol A Biol Sci Med Sci. 2006;61:176–181. doi: 10.1093/gerona/61.2.176. [DOI] [PubMed] [Google Scholar]
- 75.Flaherty JH, Steele DK, Chibnall JT, et al. An ACE unit with a delirium room may improve function and equalize length of stay among older delirious medical inpatients. J Gerontol A Biol Sci Med Sci. 2010;65:1387–1392. doi: 10.1093/gerona/glq136. [DOI] [PubMed] [Google Scholar]
- 76.Pitkala KH, Laurila JV, Strandberg TE, et al. Multicomponent geriatric intervention for elderly inpatients with delirium: Effects on costs and health-related quality of life. J Gerontol A Biol Sci Med Sci. 2008;63:56–61. doi: 10.1093/gerona/63.1.56. [DOI] [PubMed] [Google Scholar]
- 77.Milisen K, Lemiengre J, Braes T, et al. Multicomponent intervention strategies for managing delirium in hospitalized older people: Systematic review. J Adv Nurs. 2005;52:79–90. doi: 10.1111/j.1365-2648.2005.03557.x. [DOI] [PubMed] [Google Scholar]
- 78.Gagnon P, Allard P, Gagnon B, et al. Delirium prevention in terminal cancer: Assessment of a multicomponent intervention. Psychooncology. 2012;21:187–194. doi: 10.1002/pon.1881. [DOI] [PubMed] [Google Scholar]