Introduction
As populations continue to grow and age, there will be increasing demand for acute curative services responsive to life-threatening emergencies, acute exacerbation of chronic illnesses and many routine health problems that nevertheless require prompt action. Emergency interventions and services should be integrated with primary care and public health measures to complete and strengthen health systems. This paper focuses on acute care within that context. First, we draw on standard World Health Organization (WHO) terminology to propose working terms to define “acute care”. Second, we highlight the fragmentation of service delivery that results from not adopting the proposed definition. Third, we show the potential contribution of acute care to integrated health systems designed to reduce all-cause morbidity and mortality. Finally, we propose key steps to further the development of acute care that leaders, researchers and health workers, who are the people responsible for maintaining strong national health systems, should consider taking.
Defining acute care
Clear definitions of health systems and services are required to create a common language to encourage discussion and help focus system development efforts. Health systems include all organizations, institutions and resources “whose primary purpose is to promote, restore and/or maintain health”.1 Health services are “aimed at contributing to improved health or to the diagnosis, treatment and rehabilitation of sick people”, and they can be viewed from several perspectives: (i) as actions to organize the inputs necessary for the provision of effective interventions; (ii) as inclusive of promotion, prevention, cure, rehabilitation and palliation efforts, and (iii) as oriented towards either individuals or populations.1,2
Acute care must also be clearly defined. Standard medical definitions for acuity emphasize the singular attribute of time pressure.3 Acute services therefore include all promotive, preventive, curative, rehabilitative or palliative actions, whether oriented towards individuals or populations, whose primary purpose is to improve health and whose effectiveness largely depends on time-sensitive and, frequently, rapid intervention.
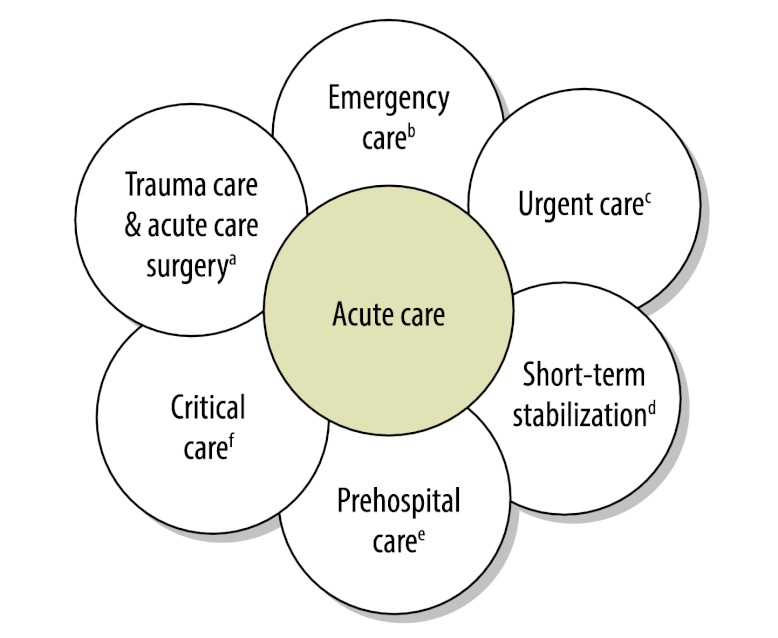
Many individually-oriented services have optimal delivery times. As a group, acute curative services are the most time-sensitive, regardless of disease entity. However, to date, acute care has been poorly defined and inadequately supported in most developing health systems. A reasonable working definition of acute care would include the most time-sensitive, individually-oriented diagnostic and curative actions whose primary purpose is to improve health. A proposed definition of acute care includes the health system components, or care delivery platforms, used to treat sudden, often unexpected, urgent or emergent episodes of injury and illness that can lead to death or disability without rapid intervention. The term acute care encompasses a range of clinical health-care functions, including emergency medicine, trauma care, pre-hospital emergency care, acute care surgery, critical care, urgent care and short-term inpatient stabilization (Fig. 1).
Fig. 1.
Domains in acute care
a Treatment of individuals with acute surgical needs, such as life-threatening injuries, acute appendicitis or strangulated hernias.
b Treatment of individuals with acute life- or limb-threatening medical and potentially surgical needs, such as acute myocardial infarctions or acute cerebrovascular accidents, or evaluation of patients with abdominal pain.
c Ambulatory care in a facility delivering medical care outside a hospital emergency department, usually on an unscheduled, walk-in basis. Examples include evaluation of an injured ankle or fever in a child.
d Treatment of individuals with acute needs before delivery of definitive treatment. Examples include administering intravenous fluids to a critically injured patient before transfer to an operating room.
e Care provided in the community until the patient arrives at a formal health-care facility capable of giving definitive care. Examples include delivery of care by ambulance personnel or evaluation of acute health problems by local health-care providers.
f The specialized care of patients whose conditions are life-threatening and who require comprehensive care and constant monitoring, usually in intensive care units. Examples are patients with severe respiratory problems requiring endotracheal intubation and patients with seizures caused by cerebral malaria.
Fragmented health system and services
In 2007, WHO highlighted the need to strengthen health systems, but precise definitions and objectives, especially with regard to the delivery of health services, often remain elusive.4 Priority health problems are on consensus lists that countries normally develop with input from international organizations. Health services are then oriented towards preventing and controlling these priority health problems. One important component that has yet to be adequately elucidated within these processes is the influence of time on the implementation and success of interventions. Preventive strategies primarily focus on reducing the probability of incident cases through interventions that decrease the risk of developing a disease. The sooner prevention efforts begin, the sooner incidence falls. On the other hand, curative strategies reduce the probability of disability or death among existing cases. The relative priority assigned to curative interventions is driven by how time-sensitive and effective the interventions are, as well as by cost. However, in the case of curative services, the relationship between time and effectiveness varies, which makes it important to get the patient to the right place at the right time for the right intervention. Failure to consider the time component of curative services produces fragmentation through poor coordination of care and the imprecise application of clinical interventions, such as delays in treating sepsis with antibiotics leading to death or disability. Fragmented care reduces the number of disability-adjusted life years (DALYs) that can be averted with a given set of resources.
The contribution of acute care
As a clinical service, acute care responds to immediately life- or limb-threatening health conditions, regardless of their ultimate cause. Thus, acute care necessarily supports progress towards strong health systems (horizontal approach) rather than from patchwork efforts that may improve outcomes for specific conditions but not the overall functioning of the health system (vertical programmes). Notably, many of the material, consumable and human resources required to implement acute care platforms are the same as those needed in traditional “disease-centred” programmes. Additionally, it is important to dispel common misperceptions about acute care, such as believing it to be the same as ambulance transport or fundamentally reliant on high technology. On the contrary, excellent acute care is driven by a temporal element – i.e. responding to immediate threats to life or limb – and involves a redistribution of resources to minimize impending death and disability. The integration of acute care with preventive and primary care completes a health-care system paradigm that fully encompasses all essential aspects of health care delivery.
The predominant conceptual framework divides health problems into communicable diseases, noncommunicable diseases and injuries. The current global discussion concerning noncommunicable diseases illustrates how care can be fragmented when the time sensitivity of curative interventions is ignored. Of the 57 million deaths in the world in 2008, 36 million (63%) were caused by noncommunicable diseases.5 A substantial and increasing proportion of the global deaths from noncommunicable diseases and injuries occurs in low- and middle-income countries undergoing the epidemiologic transition.6 Strategies for addressing morbidity and mortality from noncommunicable diseases have focused almost exclusively on prevention and primary care. For instance, the recently published Prevention and control of noncommunicable diseases: guidelines for primary health care in low-resource settings offers guidelines for the management of diabetes.7 However, only the three final points refer to time-sensitive measures, even though a condition such as diabetic ketoacidosis can be acutely life-threatening. The essential contribution of acute care towards reducing the growing burden of disease and injuries has been woefully underestimated.
Acute care plays a vital role in the prevention of death and disability. Primary care is not positioned, and is frequently unable, to assume this role. Within health systems, acute care also serves as an entry point to health care for individuals with emergent and urgent conditions. A strict definition of acute care will allow the development of metrics for the evaluation of acute care services, the assessment of the disease burden addressed by these services, and the articulation of goals for the advancement of acute care in low- and middle-income countries.8 The separate and currently fragmented specialty areas grouped under acute care have been largely unable to spark growth in their respective clinical domains at the international level. This is partly because of lack of appropriate metrics and coordination of health service delivery. Understanding acute care as an integrated care platform allows these splintered areas to move forward with a single agenda as a unified front.
Key next steps
Many simple, effective and inexpensive acute care interventions can be life-saving, often within the first 24 hours. Among them are those that are provided at basic surgery wards in district hospitals offering treatment for trauma, high-risk pregnancy and other common surgical conditions.9,10 Discussion surrounding acute care is moving forward owing to visionary efforts such as the formation in 2009 of the African Federation for Emergency Medicine and the Academic Emergency Medicine Consensus Conference (devoted to “Global health and emergency care: a research agenda”), scheduled for May 2013. Still, several important steps need to be taken to further the development of acute care. They include:
Creating an acute care service delivery model for low- and middle-income countries that will function in parallel with preventive and primary services. These acute care services will address both life-threatening and limb-threatening problems as well as exacerbations of priority noncommunicable diseases.
Improving coordination between deliverers of acute care services, such as emergency physicians, surgeons and obstetricians, to deliver critical acute care services efficiently and effectively.
Developing research methods to quantify the burden of acute care diseases and injuries, including health economics and cost-effectiveness components, to justify integrating acute care within health systems.
Holding national and international discussions to encourage better integration of acute care within local and national health systems.
This paper is a call to action for leaders, policy-makers and academics to acknowledge the key contribution of acute care systems towards the care of patients with communicable and non-communicable conditions and injuries. However, the creation of such acute care systems should not be used as a pretext for diverting resources to the construction of poorly-resourced and ill-managed health facilities. Aligning key players, both within countries and across them, to support the development of the best mix of acute and preventive services needed to address the growing disease burden is an urgent priority for health systems and society.
Acknowledgements
The authors thank Linda J Kesselring for her valuable assistance.
Funding:
JM Hirshon received funding from the National Institutes of Health Fogarty International Center (Grant 5D43TW007296).
Competing interests:
None declared.
References
- 1.World Health Organization [Internet]. Health systems strengthening glossary. Geneva: WHO; 2013. Available from: http://www.who.int/healthsystems/hss_glossary/en/index5.html [accessed 25 January 2013].
- 2.Terminology: glossary of technical terms on the economics and finance of health services Geneva: World Health Organization, Regional Office for Europe; 1998. Available from: http://www.euro.who.int/__data/assets/pdf_file/0014/102173/E69927.pdf [accessed 25 January 2013].
- 3.Oxford Dictionaries Online [Internet]. Oxford English dictionary. Oxford: Oxford University Press; 2013. Available from: http://oxforddictionaries.com/definition/english/acute?q=acutectionaries.com/ [accessed 25 January 2013].
- 4.Everybody’s business: strengthening health systems to improve health outcomes: WHO’s framework for action Geneva: World Health Organization; 2007. Available from: www.who.int/healthsystems/strategy/everybodys_business.pdf [accessed 25 January 2013].
- 5.Report of the Secretary-General on the prevention and control of non-communicable diseases New York: United Nations General Assembly; 2011 (Document A/66/83). Available from: http://www.un.org/en/ga/president/65/issues/ncdiseases.shtml [accessed 25 January 2013].
- 6.Global status report on noncommunicable diseases 2010 Geneva: World Health Organization; 2011. Available from: www.who.int/nmh/publications/ncd_report2010/en/index.html [accessed 25 January 2013].
- 7.Prevention and control of noncommunicable diseases: guidelines for primary health care in low resource settings Geneva: World Health Organization; 2012. Available from: http://www.who.int/nmh/publications/phc2012/en/index.html [accessed 25 January 2013]. [PubMed]
- 8.Hsia R, Razzak J, Tsai AC, Hirshon JM. Placing emergency care on the global agenda. Ann Emerg Med. 2010;56:142–9. doi: 10.1016/j.annemergmed.2010.01.013. [DOI] [PubMed] [Google Scholar]
- 9.Laxminarayan R, Chow J, Shahid-Salles SA. Chapter 2. Intervention cost-effectiveness: overview of main messages. In: Jamison DT, Breman JG, Measham AR, Alleyne G, Claeson M, Evans DB, et al., editors. Disease control priorities in developing countries 2nd edition. Washington: World Bank; 2006. Available from: http://www.ncbi.nlm.nih.gov/books/NBK11728/ [accessed 24 January 2013].
- 10.Jamison DT, Breman JG, Measham AR, Alleyne G, Claeson M, Evans DB, et al., editors. Priorities in health Washington: World Bank; 2006. Available from: http://www.ncbi.nlm.nih.gov/books/NBK10257/ [accessed 24 January 2013].