Abstract
Objective
Little is known about predictors of recovery from bipolar depression or moderators of treatment response. In the present study we investigated attributional style (a cognitive pattern of explaining the causes of life events) as a predictor of recovery from episodes of bipolar depression and as a moderator of response to psychotherapy for bipolar depression.
Method
106 depressed outpatients with DSM-IV bipolar I or II disorder enrolled in the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) were randomized to intensive psychotherapy for depression (n=62), or collaborative care (n=44), a minimal psychoeducational intervention. The primary outcome was recovery status at each study visit as measured by the Clinical Monitoring Form. Attributional style was measured at baseline using the Attributional Style Questionnaire. Data were collected between 1998 and 2005.
Results
All analyses were by intention to treat. Extreme attributions predicted a lower likelihood of recovery (p=.01, OR=0.93, 95% CI=.88-.98) and longer time until recovery (p<.01, OR=0.96, 95% CI=.93-.99), independent of the effects of initial depression severity. Among individuals with more pessimistic attributional styles, initial depression severity predicted a lower likelihood of recovery (p=.01, OR=0.64, 95% CI=.45-.91) and longer time until recovery (p<.001, OR=0.76, 95% CI=.66-.88). There was no difference in recovery rates between intensive psychotherapy and collaborative care (OR=0.90, 95% CI=0.40-2.01) in the full sample.
Conclusions
These results suggest that extreme, rigid attributions may be associated with a more severe course of depression, and that evaluating attributional style may help clinicians to identify patients who are at risk for experiencing a more severe course of depression.
Bipolar disorder is characterized by periods of depression and/or hypomania/mania, with lengthy periods of residual symptoms prior to recovery1. Individuals with bipolar disorder often experience a highly recurrent course of the disorder2 with impairment in many areas, including cognitive impairment, poorer academic and work achievement, and high rates of suicide3-10. People with bipolar disorder spend substantially more time depressed than being hypomanic or manic11. In particular, depressive symptoms account for much of the illness burden among individuals with bipolar disorder8,12,13.
Attributional style is a cognitive characteristic that has been useful for the understanding of the course of major depression in individuals with unipolar major depressive disorder14,15. Originally developed to apply learned helplessness theory to humans16, pessimistic attributional style is defined as the tendency to attribute the causes of negative events to internal, stable, and global reasons (e.g., “I was fired because I am worthless”), and to attribute the causes of positive events to external, unstable, and specific reasons (e.g., “I received the promotion because I got lucky”)16. Several decades of research has indicated the utility of attributional style in identifying individuals at risk for developing unipolar depression14,15,17,18. In addition, several studies have found that extreme responses on measures of depressive cognition (e.g., indicating “totally agree” or “totally disagree”) predict relapse in unipolar depression19-21. In bipolar disorder, pessimistic attributional style has been found to predict increases in depressive symptoms22, particularly when vulnerable individuals experience life stressors23,24. However, it is unclear whether pessimistic attributional style is associated with longer depressive episodes in bipolar disorder, particularly after accounting for factors likely to be associated with recovery such as psychosocial treatment25 and severity of initial depressive symptoms.
Pharmacotherapy is the first line of treatment for bipolar disorder, but pharmacological treatments often fail to bring patients with bipolar disorder to sustained remission26,27. As a result, several adjunctive psychosocial interventions have been developed to treat bipolar disorder28,29. This includes cognitive-behavioral therapies (CBT)30-38, family-focused treatment (FFT)39,40, and interpersonal and social rhythm therapy (IPSRT)41,42. One of largest randomized controlled treatment trials investigating the efficacy of psychotherapy for depression in bipolar disorder was conducted in the context of the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD)43,25. This study found that FFT, IPSRT, and CBT were all equally effective in decreasing the length of time until recovery from depressive episodes and also improved functioning25,44.
Despite advances in psychotherapeutic and pharmacological28 treatment, many individuals with bipolar disorder recover slowly or not at all .9,45-47 Researchers and clinicians have called for a better understanding of predictors of outcome of bipolar depression, as well as a better understanding of which individuals are likely to benefit from psychotherapy (i.e., moderators of response to treatment)28,48,49. For example, research has indicated that CBT may be more beneficial in patients with bipolar disorder with fewer mood episodes38, whereas IPSRT and FFT may be superior for patients in more acutely ill states or individuals with a more severe course of the disorder28. Although it has been recognized that cognitive style may help identify which individuals may benefit most from psychotherapy28,50,51, to our knowledge, psychotherapy studies in bipolar disorder have neither evaluated cognitive style as a predictor for the duration of mood episodes, nor as a moderator of treatment outcome.
This study evaluated the role of attributional style in predicting recovery from bipolar depression in the context of psychosocial treatment. Specifically, we evaluated the following questions: (1) Does attributional style (including extreme attributions) impact the duration of depressive episodes in bipolar disorder? More specifically, do bipolar patients with pessimistic attributional styles or who make extreme pessimistic attributions for life events take longer to recover from depression? (2) Is there an interaction between attributional style and initial depression severity? Specifically, do patients with negative attributional style and high depression severity take longer to recover to recover from depression? (3) Does attributional style (including extreme attributions) moderate the efficacy of different types of psychotherapy for depression in bipolar disorder? To evaluate these questions we used a sample of depressed bipolar patients who were enrolled in a randomized controlled trial of adjunctive psychotherapy for bipolar depression as part of STEP-BD25.
Method
Study Design and Participants
The 106 study participants (bipolar I (61%) or II (39%)) were drawn from 293 outpatients enrolled in the randomized, controlled clinical trial25 comparing the efficacy of psychotherapy and collaborative care treatment as part of STEP-BD. STEP-BD is a National Institute of Mental Health-sponsored naturalistic multi-center study of the effectiveness of treatments for bipolar disorder46 (for more details about the psychosocial treatment trial, see Miklowitz et al.25). Inclusion criteria for the embedded randomized controlled psychotherapy trial included: (a) being 18 years of age or older, (b) meeting DSM-IV criteria for bipolar I or II disorder and currently (during the prior 2 weeks) meeting criteria for a major depressive episode, (c) current treatment with a mood stabilizer, (d) not currently undergoing psychotherapy or willing to taper non-study psychotherapy sessions to one or fewer per month, (e) speaks English, and (f) being willing and able to give informed consent. Exclusion criteria were requiring immediate treatment for a DSM-IV substance or alcohol use or dependence disorder (excluding nicotine), being pregnant or planning pregnancy in the next year, a history of intolerance, nonresponse, or contraindication to bupropion or paroxetine, or requiring dose changes in antipsychotic medications25. The STEP-BD trial was reviewed and approved by the Human Research Institutional Review Boards of all participating universities.
The subsample of 106 patients from the larger STEP-BD trial had completed a measure of attributional style (the Attributional Style Questionnaire [ASQ]52) prior to the first psychosocial treatment session (see Table 1). This subsample did not differ from the original sample of 293 on any patient characteristics (χ2s<2.15, ts<1.23, ps>.14, N's=246-293) with the exception of the severity of initial depressive symptoms, which were higher in this subsample (t=9.18, p<.001, N=288) and global assessment of functioning scores which were lower in this subsample (t=7.84, p<.001, N=292).
Table 1.
Demographic and Illness Characteristics of 106 Bipolar Depressed Patients.
| Variable | Value |
|---|---|
| Age, mean ± SD | 39.68 ± 11.84 |
| Female sex | 62% |
| Race | |
| Caucasian/White | 94% |
| African American/Black | 5% |
| Asian/Pacific Islander | 0% |
| Other | 1% |
| Hispanic ethnicity | 1% |
| Education >1 year of college | 85% |
| Income < $29,999 | 39% |
| Marital status | |
| Married | 34% |
| Never married | 37% |
| Separated/Divorced | 28% |
| Widowed | 2% |
| Diagnosis | |
| Bipolar I | 61% |
| Bipolar II | 39% |
| >10 Previous depressive episodes | 65% |
| >10 Previous manic episodes | 67% |
| Age at illness onset, mean ± SD | 21.89 ± 10.09 |
| Baseline depression symptoms, mean ± SD | 6.23 ± 2.43 |
| Baseline mania symptoms, mean ± SD | 1.16 ± 1.17 |
| Baseline GAF score, mean ± SD | 55.91 ± 8.59 |
| Medications | |
| Lithium | 34% |
| Atypical antipsychotic | 26% |
| Anticonvulsant | 56% |
| Benzodiazepine | 25% |
| Antidepressants | 46% |
| Stimulants | 1% |
| Valproate | 36% |
| Other mood stabilizers | 28% |
| Medication Load Index74 | 3.64 (1.94) |
| Comorbid diagnoses | |
| Anxiety disorder (current) | 49% |
| Substance abuse/dependence (current) | 13% |
| ADHD (current) | 14% |
| Any lifetime comorbid disorder | 83% |
Note. Data are presented as number (percentage) unless otherwise indicated. Percentages are not always based on 106 patients owing to missing data (see Miklowitz et al., 200725).
Procedures and Outcomes
In STEP-BD patients were diagnosed with bipolar disorder by study psychiatrists using the Affective Disorders Evaluation53,54. A second clinical interviewer verified the results using the Mini-International Neuropsychiatric Interview (version 5.0)55,46. The 106 participants included in the present study were randomly assigned to an intensive psychotherapy (n=62; CBT [n=31], IP SRT [n=20], or FFT [n=11]) or to a Collaborative Care (CC [n=44]) control condition (for more detailed information of these treatments, see Miklowitz et al.25; Otto et al.56; Miklowitz57; Frank58). CC was a minimal psychosocial intervention that consisted of three 50-minute individual sessions conducted within 6 weeks after randomization and included psychoeducation about bipolar disorder and development of a relapse prevention contract. CC was intended to provide a brief version of the most common strategies shown to benefit patients with bipolar disorder57. All intensive psychosocial treatments consisted of up to thirty 50-minute sessions conducted by therapists who received training and supervision from nationally-recognized experts in the specific intensive treatments25.
Measures
Clinical Monitoring Form (CMF)59
As in Miklowitz et al.25, the primary outcome measure in the present study was patients’ clinical recovery status, which was assessed at each visit via the CMF59. The CMF is a well-validated measure of the severity of DSM-IV mood symptoms and clinical status1,25,43,59,60. Clinical status (e.g. recovered) is based on the presence or absence of DSM-IV criteria for episodes of depression or mania/hypomania, with recovered status defined as ≤ 2 moderate symptoms of depression for ≥ 8 of the previous weeks. Initial depression severity was defined as the CMF depressive symptom severity score (sum of the severity of all depression symptoms) at study entry, and could range from 0 to 12. Initial medication types and dosages were also evaluated with the CMF. We also computed a variable representing psychiatric medication load, following the coding system delineated by Phillips et al.61, such that higher values represent greater medication load (Table 1). Each psychiatric medication was given a coding of 1 or 2 depending on the therapeutic dosage61. Total medication load scores ranged from 0 to 8 (Mean=3.64, SD=1.94).
Attributional Style Questionnaire (ASQ)52
Participants rated the perceived cause of six hypothetical negative events and six hypothetical positive events using 7-point Likert scales in terms of internality (due to me vs. due to other people or circumstances), stability (will always be present vs. will never be present), and globality (influences all situations in my life vs. influences only this particular situation). Scores were computed representing attributional style for negative events (Mean=86.39, Median=87, SD=14.49; higher scores indicate more pessimistic attributional style), positive events (Mean=84.85, Median=86, SD=13.20; higher scores indicate more optimistic attributional style), and a difference score indicating the degree of optimistic versus pessimistic attributional styles, computed by subtracting the positive event score from the negative event score (Mean=1.54, Median=2, SD=19.44; higher scores indicate more pessimistic attributional style). Scores on these subscales were comparable with previously-published scores in healthy and depressed samples52, 62.
Because of its utility in predicting recurrence of unipolar depression in previous research19-21, we also computed the number of “extreme” responses (rating of a “1” or “7” on each item), resulting in variables for extreme pessimistic (Mean=5.84, Median=5, SD=4.79), extreme optimistic (Mean=4.64, Median=3, SD=4.80), and total extreme responses (Mean=10.48, Median=9, SD=8.00), with higher scores indicating a greater frequency of extreme responses of each type. Internal consistency for the ASQ was high (α=.76).
Statistical Analysis
To evaluate the effects of attributional style and extreme responses on likelihood of recovery and time until recovery, we conducted logistic regressions and Cox proportional hazards models, respectively. All analyses were by intention to treat. Patients were included until their final assessment point with a maximum of 365 days in the study25 (M=291.78 days, SD=96.51). The proportionality of risk assumption was upheld for all survival analyses. Odds ratios less than one indicate lower likelihood of recovery and greater time until recovery.
To evaluate the incremental ability of attributional style and extreme responses to predict recovery status beyond the effects of treatment or initial depressive symptoms, treatment condition (CC or intensive psychotherapy) and initial depressive symptoms were included in step 1 of the regression models, and ASQ variables in step 2. Prior to evaluating ASQ variables as moderators of treatment effects, we determined whether there were significant effects of treatment condition on likelihood of recovery and time until recovery63.
Results
Incremental Effects of Attributional Style on Recovery from Depression
Demographic and clinical characteristics including psychopharmacological medications, attrition, and treatment completion are shown in Table 1 (for the characteristics of the full sample see Miklowitz et al25). The results of the primary analyses (logistic regression models using attribution scores, psychosocial treatment condition, and initial depression severity to predict recovery, and Cox regression analyses to predict time to recovery) are in Table 2. All analyses had a total sample of N=106 participants. The severity of initial depressive symptoms was not associated with likelihood of recovery (Wald=2.64, OR=0.87, 95% CI=.73-1.03, p=.10, R2=.04), but it was associated with longer time to recovery (Wald=6.57, OR=0.89, 95% CI=.81-.97, p=.01). Higher medication load predicted a lower likelihood of recovery (Wald=4.38, OR=0.80, 95% CI=.64-.99, p=.04, R2=.06), and a greater time to recovery (Wald=11.37, OR=0.80, 95% CI=.70-.91, p<.001). ASQ variables were not significantly associated with initial depressive symptoms (rs<.13, ps>.19) or with medication load (rs<.16, ps ≥.10).
Table 2.
Logistic Regression and Cox Regression Analyses Evaluating Attributional Style and Extreme Responses as Predictors of Likelihood of Recovery and Time until Recovery from Depressiona
| Step | Predictor | B | Wald | OR | p | 95% CI | ΔR2 b, c |
|---|---|---|---|---|---|---|---|
| ASQ Total Score Models | |||||||
| Logistic Regression: Predicting Recovery | |||||||
| 1 | CMF Depressive Sx | -0.14 | 2.47 | 0.87 | .12 | .730-1.035 | .04 |
| Treatment Groupd | 0.02 | <0.01 | 1.02 | .96 | .447-2.332 | ||
| 2 | ASQ Total | >-0.01 | 0.09 | <1.00 | .76 | .976-1.018 | <.01 |
| Cox Regression: Predicting Time Until Recovery | |||||||
| 1 | CMF Depressive Sx | -0.12 | 5.92 | 0.89 | .02 | .812-.978 | |
| Treatment Groupd | 0.05 | 0.04 | 1.05 | .84 | .647-1.714 | ||
| 2 | ASQ Total | <0.01 | 0.01 | 1.00 | .94 | .988-1.011 | <.01 |
| ASQ Extreme Total Models | |||||||
| Logistic Regression: Predicting Recovery | |||||||
| 1 | CMF Depressive Sx | -0.16 | 3.16 | 0.85 | .08 | .715-1.017 | .04 |
| Treatment Groupd | 0.10 | 0.05 | 1.10 | .82 | .470-2.597 | ||
| 2 | ASQ Extreme Total | -0.07 | 6.70 | 0.93 | .01 | .883-.983 | .09 |
| Cox Regression: Predicting Time Until Recovery | |||||||
| 1 | CMF Depressive Sx | -0.13 | 6.87 | 0.88 | .01 | .794-.967 | |
| Treatment Groupd | -0.02 | 0.01 | 0.98 | .92 | .596-1.599 | ||
| 2 | ASQ Extreme Total | -0.05 | 6.86 | 0.96 | .01 | .925-.989 | .07 |
| Models for Interaction between ASQ Total Score and Initial Depressive Symptoms | |||||||
| Logistic Regression: Predicting Recovery | |||||||
| 1 | Treatment Groupd | -0.07 | 0.02 | 0.94 | .88 | .401-2.187 | <.01 |
| 2 | CMF Depressive Sx | -0.19 | 3.59 | 0.83 | .06 | .679-1.007 | .04 |
| ASQ Total | >-.01 | 0.04 | 1.00 | .84 | .975-1.020 | ||
| 3 | CMF Depressive Sx X ASQ Total | -.01 | 3.81 | 0.99 | .05 | .981-.999 | .06 |
| Cox Regression: Predicting Time Until Recovery | |||||||
| 1 | Treatment Groupd | 0.02 | <0.01 | 1.02 | .95 | .621-.1659 | |
| 2 | CMF Depressive Sx | -0.14 | 8.40 | 0.87 | <.01 | .794-.956 | .03 |
| ASQ Total | 0.02 | 2.99 | 1.02 | .84 | .997-1.045 | ||
| 3 | CMF Depressive Sx X ASQ Total | >-0.01 | 4.06 | 0.99 | .04 | .993-.999 | .04 |
| Models for Interaction between ASQ Extreme Total and Initial Depressive Symptoms | |||||||
| Logistic Regression: Predicting Recovery | |||||||
| 1 | Treatment Groupd | 0.08 | 0.03 | 1.08 | .86 | .456-2.549 | <.01 |
| 2 | CMF Depressive Sx | -0.13 | 1.91 | 0.88 | .17 | .725-1.057 | .12 |
| ASQ Extreme Total | -0.08 | 6.83 | 0.93 | .01 | .876-.981 | ||
| 3 | CMF Depressive Sx X ASQ Extreme Total | -0.01 | 0.60 | 0.99 | .44 | .972-1.012 | .01 |
| Cox Regression: Predicting Time Until Recovery | |||||||
| 1 | Treatment Groupd | -0.03 | 0.01 | 0.97 | .92 | .595-1.594 | |
| 2 | CMF Depressive Sx | -0.13 | 6.14 | 0.88 | .01 | .799-.974 | .09 |
| ASQ Extreme Total | -0.05 | 7.16 | 0.95 | .01 | .919-.987 | ||
| 3 | CMF Depressive Sx X ASQ Extreme Total | >-0.01 | 0.56 | 1.00 | .46 | .986-1.006 | .01 |
N = 106.
Change in R2 for logistic regressions represents Nagelkerke R2 change since previous step, an estimate of the increment in variance in the probability of recovery accounted for by the predictors tested since the previous step73.
Change in R2 for Cox regressions represents Cox-Snell R2 change since previous step, an estimate of the relative association between survival and the predictors tested since the previous step76.
Treatment Group = Intensive psychosocial treatment (1) vs. Collaborative Care (0).
Controlling for treatment group (intensive psychotherapy and collaborative care) and initial depressive symptoms, there was no significant effect of ASQ total score on likelihood of recovery or time until recovery (Table 2). However, consistent with our hypotheses, more ASQ total extreme responses were associated with a significantly lower likelihood of recovery and a longer time until recovery (Table 2). This effect was significant for extreme pessimistic responses (Logistic p=.02 and Cox p=.04) as well as for extreme optimistic responses (Logistic p=.04 and Cox p=.03).
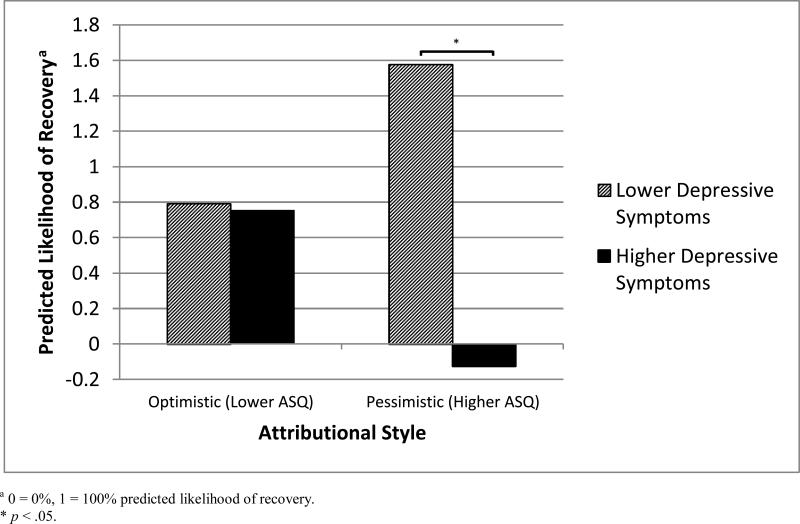
Patients’ ASQ total scores interacted with initial depressive symptoms in predicting likelihood of recovery and time until recovery (Table 2). To probe the nature of these interactions, we centered the ASQ variables and tested the effects of depressive symptoms on recovery at one standard deviation above or below the ASQ means64. Consistent with the hypothesis that initial depressive symptoms had a more severe impact on course of depression among individuals with a negative attributional style, higher initial depressive symptoms were associated with lower likelihood of recovery (Wald=6.25, OR=0.64, 95% CI=.45-.91, p=.01) and greater time until recovery (Wald=14.56, OR=0.76, 95% CI=.66-.88, p<.001) among individuals with more pessimistic attributional styles, but did not predict likelihood of recovery (Wald=0.38, OR=1.09, 95% CI=.83-1.42, p=.54) or time until recovery (Wald=0.04, OR=0.99, 95% CI=.87-1.13, p=.85) among individuals with more optimistic attributional styles.
Effects of Treatment on Recovery from Depression
In contrast with the full sample of 293 patients (see Miklowitz et al.25), there was no significant effect of treatment group in this study's subsample (N = 106) on likelihood of recovery from depression (B=-0.11, Wald=0.07, OR=0.90, p=.79, 95% CI=.40-2.01, R2<.01), or time to recovery (B=-0.10, Wald=0.16, OR=0.91, p=.69, 95% CI=.56-1.47). Per Kraemer et al.63, this precluded the investigation of whether attributional style moderated the effect of psychotherapy compared to collaborative care on recovery. All results remained consistent after controlling for study site, number of psychosocial treatment sessions, bipolar I or II status, age, gender, education, number of lifetime episodes of depression and mania/hypomania, baseline manic symptoms, psychiatric medication load, and age at onset of bipolar disorder.
Discussion
Our results indicated that, among depressed patients with bipolar I or II disorder, extreme pessimistic and extreme optimistic responses predicted a lower likelihood of recovery and a greater time until recovery from depression. These results remained significant when initial depression severity, psychosocial treatment type, and symptoms of mania were included in regression models. We had hypothesized this effect for pessimistic responses; yet the emergence of significant prediction for extreme optimistic responses suggests that it is not simply the negative nature of extreme thoughts that may be important for prediction of recovery in bipolar depression, but the fixity or rigidity of thought, as reflected by greater belief in both positive and negative extreme thoughts.
Cognitive rigidity, typically assessed with neuropsychological tasks, has itself been linked to both disorder onset and a more chronic course of depression65-67. In contrast, being more fluidly aware of the possible inaccuracies of thoughts (metacognitive awareness) is associated with lower relapse into depression68. Our results are in accord with both of these findings and suggest that the presence of extreme cognitions (regardless of valence) may indicate a lower likelihood of recovery from depression in bipolar disorder.
The tendency to make extreme attributions about the causes of life events appears to be associated with a more severe course of bipolar depression. To recover, these individuals may need to overcome not only their depressed mood but also the extreme rigid thought style through which they interpret negative events in their lives, which may serve to maintain depressed mood. Indeed, individuals with a pessimistic attributional style and more severe initial depressive symptoms experienced the worst course of depression, suggesting that the combination of these factors may be associated with a poorer prognosis. These results are consistent with studies that report that a pessimistic attributional style is a risk factors for depressed mood among individuals with bipolar disorder23,24. The present study indicates that pessimistic attributional style, and particularly extreme attributions, may also predict the course of bipolar depression by means of maintaining depressed mood. Thus, evaluating attributional style among patients presenting for treatment for bipolar depression may allow for adapting treatments in order to address these issues. For example, it is possible that bipolar individuals who make extreme attributions would benefit from cognitive restructuring using hypothetical scenarios to help them make more balanced attributions, or from observing their attributions using a mindful, nonjudgmental, decentered approach to their thoughts, as suggested by mindfulness-based treatments for bipolar disorder69-71.
To our knowledge, this study is the first to evaluate cognitive style as a predictor of the course of bipolar depression. We utilized a sample early in the development of a major depressive episode which may be representative of patients with bipolar disorder who are seen for acute care in clinical practice25. Nevertheless, several limitations of the study should be noted. First, only a subsample of participants from the full trial of psychosocial treatments for bipolar depression completed the ASQ, so it is unclear whether these results would extend to the full sample in STEP-BD. In this subsample, intensive psychotherapy was not associated with a more rapid time to recovery from depression, possible because patients in the subsample had more severe initial depressive symptoms and poorer functioning than those in the full sample.25 Second, attributional style was only evaluated at time of randomization, so it was not possible to evaluate whether attributional style changed as a result of treatments condition or in concert with recovery from depression. Third, although our primary outcome measure of recovery from the depressive episode is clinically relevant, other ways of evaluating course of illness (e.g., continued residual mood symptoms, switch to mania, or symptom worsening49) should be evaluated in greater detail in the future.
Fourth, we did not evaluate intervening life events as suggested by vulnerability-stress models of bipolar disorder23,24,72. Evaluating life stress in combination with cognitive vulnerabilities such as attributional style might allow clinicians to predict more precisely which patients are likely to have more severe courses of illness51. In addition, our sample was relatively homogenous in terms of race and socioeconomic status. Finally, the primary findings were characterized by small to medium effect sizes. Nonetheless, even small effects may be clinically relevant when evaluating predictors of recovery from bipolar depression73.
In conclusion, attributional style and extreme attributions for life events may be important predictors of the course of bipolar depression. Future research should examine whether evaluating attributions in the context of life stress23,24,72, as well as attributions for actual (as opposed to hypothetical) negative life events74, allows for better prediction of which individuals take longer to recover from bipolar depression. Finally, more work is needed to determine whether enhancing psychotherapies such as CBT by more deliberately targeting negative or rigid cognitions, or by using cognitive remediation strategies for treating cognitive rigidity75, would improve the course of depression among bipolar individuals undergoing pharmacological treatment.
Figure 1.
Interaction between Attributional Style and Initial Depressive Symptoms Predicting Likelihood of Recovery from Depression.
Acknowledgments
Funding/Support: STEP-BD was funded in part by contract N01MH80001 from the National Institute of Mental Health (Gary Sachs). Support for the development of the psychosocial treatments was provided by grants MH29618 (Ellen Frank), MH43931 (David Miklowitz), and MH55101 (David Miklowitz) from the National Institute of Mental Health and by the National Alliance for Research on Schizophrenia and Depression (David Miklowitz). Jonathan Stange was supported by National Research Service Award F31MH099761 from NIMH. Louisa Sylvia was employed by Massachusetts General Hospital, served as a Consultant for Bracket Global and Clintara, received research support from NIMH, is a former stockholder in Concordant Rater Systems, and has received support from New Harbinger Publishers. Pedro Vieira da Silva Magalhães reports no relevant financial interests. David Miklowitz has received research support or honoraria from NIMH, Brain and Behavior Research Foundation, Danny Alberts Foundation, and Attias Family Foundation; He has received other financial or material support from Guilford Press, and John Wiley and Sons. Michael Otto has served as a consultant for MicroTransponder, Inc. Ellen Frank has served as a consultant for Servier International, and has received other financial or material support from Guilford Press and the American Psychological Association Press. Michael Berk is an employee of Barwon Health, Deakin University; he has received research support from NIH, NHMRC, and CRC Simons; he has received honoraria from Lundbeck, Astrazeneca, Servier, Lilly, and ISBD Korea; he has served as a speaker or on the advisory board for Astrazeneca, Lundbeck, Lilly, and Janssen; and he has received financial or material support from Allen & Unwin and Cambridge University Press. Andrew Nierenberg has received honoraria or travel expenses from: American Society of Clinical Psychopharmacology, Australasian Society for Bipolar Disorder, Bayamon Region Psychiatric Society, San Juan, Puerto Rico, Belvoir Publishing, Boston Center for the Arts, Corcept, CRICO, Dartmouth, Dey Pharma, L.P./Mylan Inc., Israel Society for Biological Psychiatry, John Hopkins University, National Association of Continuing Education, PAI, Pamlabs, Physicians Postgraduate Press, Ridge Diagnostics, Slack Publishing, Sunovion, Teva Pharmaceuticals, University of Florida, University of Michigan, University of New Mexico, University of Miami, University of Wisconsin, Wolters Klower Publishing. Potential consulting honoraria from Astra Zeneca, Bristol Myers Squibb, Forest, Pfizer, Ridge Diagnostics. Potential support of research at MGH through Biogen Idec, Dey Pharmaceuticals, Pamlabs, Shire, and Sunovian. He owns stock options in Appliance Computing, Inc.(MindSite.com) and Brain Cells, Inc. Additional income is possible from Infomedic.com depending on overall revenues of the company but no revenue has been received to date. Through MGH, Dr. Nierenberg is named for copyrights to: the Clinical Positive Affect Scale and the MGH Structured Clinical Interview for the Montgomery Asberg Depression Scale exclusively licensed to the MGH Clinical Trials Network and Institute (CTNI). Thilo Deckersbach was supported in part by a K-23 NIMH Career Award 1K23MH074895-01A2. His research has also been funded by NARSAD, TSA, OCF and Tufts University. He has received honoraria, consultation fees and/or royalties from the MGH Psychiatry Academy, BrainCells Inc., Systems Research and Applications Corporation, Boston University, the Catalan Agency for Health Technology Assessment and Research, the National Association of Social Workers Massachusetts, the Massachusetts Medical Society, Tufts University, NIDA and Oxford University Press. He has also participated in research funded by NIH, NIA, AHRQ, Janssen Pharmaceuticals, The Forest Research Institute, Shire Development Inc., Medtronic, Cyberonics, and Northstar.
References
- 1.Perlis RH, Ostacher MJ, Patel JK, et al. Predictors of recurrence in bipolar disorder: primary outcomes from the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). Am J Psychiatry. 2006;163(2):217–24. doi: 10.1176/appi.ajp.163.2.217. [DOI] [PubMed] [Google Scholar]
- 2.Goldberg JF, Burdick KE, editors. Cognitive dysfunction in bipolar disorder. American Psychiatric Publishing; Washington, DC: 2008. [Google Scholar]
- 3.Murray CJL, Lopez AD. The Global Burden of Disease: A Comprehensive Assessment of Mortality and Disability From Diseases, Injuries, and Risk Factors in 1990 and Projected to 2020. Harvard University Press; Boston: 1996. [Google Scholar]
- 4.Martinez-Aran A, Vieta E, Colom F, et al. Cognitive impairment in euthymic bipolar patients: implications for clinical and functional outcome. Bipolar Disord. 2004;6(3):224–32. doi: 10.1111/j.1399-5618.2004.00111.x. [DOI] [PubMed] [Google Scholar]
- 5.Grant BF, Stinson FS, Dawson DA, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- 6.Angst F, Stassen HH, Clayton PJ, et al. Mortality of patients with mood disorders: Follow-up over 34–38 years. J Affect Disord. 2002;68:167–81. doi: 10.1016/s0165-0327(01)00377-9. [DOI] [PubMed] [Google Scholar]
- 7.Nusslock R, Abramson LY, Harmon-Jones E, et al. A goal-striving life event and the onset of bipolar episodes: Perspective from the behavioral approach system (BAS) dysregulation theory. J Abnorm Psychol. 2007;116:105–15. doi: 10.1037/0021-843X.116.1.105. [DOI] [PubMed] [Google Scholar]
- 8.Kessler RC, Akiskal HS, Ames M, et al. Prevalence and effects of mood disorders on work performance in a nationally representative sample of U.S. workers. Am J Psychiatry. 2006;163(9):1561–8. doi: 10.1176/appi.ajp.163.9.1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goodwin FK, Jamison KR. Manic-depressive illness. Oxford University Press; New York: 1990. [Google Scholar]
- 10.Keck PE, Jr, McElroy SL, Strakowski SM, et al. Factors associated with pharmacologic noncompliance in patients with mania. J Clin Psychiatry. 1996;57:292–7. [PubMed] [Google Scholar]
- 11.De Dios C, Ezquiaga E, Garcia A, Soler B, Vieta E. Time spent with symptoms in a cohort of bipolar disorder outpatients in Spain: a prospective, 18-month follow-up study. J Affect Disord. 2010 Sep;125(1-3):74–81. doi: 10.1016/j.jad.2009.12.006. [DOI] [PubMed] [Google Scholar]
- 12.Rosa AR, Reinares M, Michalak EE, Bonnin CM, Sole B, Franco C, Comes M, Torrent C, Kapczinski F, Vieta E. Functional impairment and disability across mood states in bipolar disorder. Value Health. 2010 Dec;13(8):984–8. doi: 10.1111/j.1524-4733.2010.00768.x. [DOI] [PubMed] [Google Scholar]
- 13.Baldessarini RJ, Salvatore P, Khalsa HM, Gebre-Medhin P, Imaz H, González-Pinto A, Perez J, Cruz N, Maggini C, Tohen M. Morbidity in 303 first-episode bipolar I disorder patients. Bipolar Disord. 2010 May;12(3):264–70. doi: 10.1111/j.1399-5618.2010.00812.x. [DOI] [PubMed] [Google Scholar]
- 14.Alloy LB, Abramson LY, Keyser J, Gerstein RK, Sylvia LG. Negative cognitive style. In: Dobson KS, Dozois DJA, editors. Risk Factors in Depression. Academic Press; New York: 2008. pp. 221–236. [Google Scholar]
- 15.Abela JRZ, Auerbach RP, Seligman MEP. Dispositional pessimism across the lifespan. In: Dobson KS, Dozois DJA, editors. Risk Factors in Depression. Academic Press; New York: 2008. pp. 195–220. [Google Scholar]
- 16.Abramson LY, Seligman ME, Teasdale JD. Learned helplessness in humans: critique and reformulation. J Abnorm Psychol. 1978 Feb;87(1):49–74. [PubMed] [Google Scholar]
- 17.Alloy LB, Abramson LY, Whitehouse WG, Hogan ME, Panzarella C, Rose DT. Prospective incidence of first onsets and recurrences of depression in individuals at high and low cognitive risk for depression. J Abnorm Psychol. 2006 Feb;115(1):145–56. doi: 10.1037/0021-843X.115.1.145. [DOI] [PubMed] [Google Scholar]
- 18.Sweeney PD, Anderson K, Bailey S. Attributional style in depression: a meta-analytic review. J Pers Soc Psychol. 1986 May;50(5):974–91. doi: 10.1037//0022-3514.50.5.974. [DOI] [PubMed] [Google Scholar]
- 19.Teasdale JD, Scott J, Moore RG, Hayhurst H, Pope M, Paykel ES. How does cognitive therapy prevent relapse in residual depression? Evidence from a controlled trial. J Consult Clin Psychol. 2001 Jun;69(3):347–57. doi: 10.1037//0022-006x.69.3.347. [DOI] [PubMed] [Google Scholar]
- 20.Petersen TJ, Feldman G, Harley R, Fresco DM, Graves L, Holmes A, Bogdan R, Papakostas GI, Bohn L, Lury RA, Fava M, Segal ZV. Extreme response style in recurrent and chronically depressed patients: change with antidepressant administration and stability during continuation treatment. J Consult Clin Psychol. 2007 Feb;75(1):145–53. doi: 10.1037/0022-006X.75.1.145. [DOI] [PubMed] [Google Scholar]
- 21.Beevers CG, Keitner GI, Ryan CE, Miller IW. Cognitive predictors of symptom return following depression treatment. J Abnorm Psychol. 2003 Aug;112(3):488–96. doi: 10.1037/0021-843x.112.3.488. [DOI] [PubMed] [Google Scholar]
- 22.Johnson SL, Fingerhut R. Cognitive styles predict the course of bipolar depression, not mania. Journal of Cognitive Psychotherapy: An International Quarterly. 2004;18:149–162. [Google Scholar]
- 23.Reilly-Harrington NA, Alloy LB, Fresco DM, Whitehouse WG. Cognitive styles and life events interact to predict bipolar and unipolar symptomatology. J Abnorm Psychol. 1999 Nov;108(4):567–78. doi: 10.1037//0021-843x.108.4.567. [DOI] [PubMed] [Google Scholar]
- 24.Alloy LB, Reilly-Harrington N, Fresco DM, Whitehouse WG, Zechmeister JS. Cognitive styles and life events in subsyndromal unipolar and bipolar disorders: Stability and prospective prediction of depressive and hypomanic mood swings. J Cog Psychother. 1999;13:21–40. [Google Scholar]
- 25.Miklowitz DJ, Otto MW, Frank E, et al. Psychosocial treatments for bipolar depression: a 1-year randomized trial from the Systematic Treatment Enhancement Program. Arch Gen Psychiatry. 2007a;64(4):419–26. doi: 10.1001/archpsyc.64.4.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gitlin MJ, Swendsen J, Heller TL, et al. Relapse and impairment in bipolar disorder. Am J Psychiatry. 1995;152:1635–40. doi: 10.1176/ajp.152.11.1635. [DOI] [PubMed] [Google Scholar]
- 27.Harel EV, Levkovitz Y. Effectiveness and safety of adjunctive antidepressants in the treatment of bipolar depression: a review. Isr J Psychiatry Relat Sci. 2008;45(2):121–8. [PubMed] [Google Scholar]
- 28.Miklowitz DJ. Adjunctive psychotherapy for bipolar disorder: state of the evidence. Am J Psychiatry. 2008;165(11):1408–19. doi: 10.1176/appi.ajp.2008.08040488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lauder SD, Berk M, Castle DJ, Dodd S, Berk L. The role of psychotherapy in bipolar disorder. Med J Aust. 2010 Aug 16;193(4 Suppl):S31–5. doi: 10.5694/j.1326-5377.2010.tb03895.x. [DOI] [PubMed] [Google Scholar]
- 30.Cochran SD. Preventing medical noncompliance in the outpatient treatment of bipolar affective disorders. J Consult Clin Psychol. 1984 Oct;52(5):873–8. doi: 10.1037//0022-006x.52.5.873. [DOI] [PubMed] [Google Scholar]
- 31.Colom F, Vieta E, Sánchez-Moreno J, Palomino-Otiniano R, Reinares M, Goikolea JM, Benabarre A, Martínez-Arán A. Group psychoeducation for stabilised bipolar disorders: 5-year outcome of a randomised clinical trial. Br J Psychiatry. 2009 Mar;194(3):260–5. doi: 10.1192/bjp.bp.107.040485. [DOI] [PubMed] [Google Scholar]
- 32.Castle D, White C, Chamberlain J, Berk M, Berk L, Lauder S, Murray G, Schweitzer I, Piterman L, Gilbert M. Group-based psychosocial intervention for bipolar disorder: randomised controlled trial. Br J Psychiatry. 2010 May;196(5):383–8. doi: 10.1192/bjp.bp.108.058263. [DOI] [PubMed] [Google Scholar]
- 33.Lam DH, Watkins ER, Hayward P, et al. A randomized controlled study of cognitive therapy for relapse prevention for bipolar affective disorder: outcome of the first year. Arch Gen Psychiatry. 2003;60(2):145–52. doi: 10.1001/archpsyc.60.2.145. [DOI] [PubMed] [Google Scholar]
- 34.Lam DH, Hayward P, Watkins ER, et al. Relapse prevention in patients with bipolar disorder: cognitive therapy outcome after 2 years. Am J Psychiatry. 2005;162(2):324–9. doi: 10.1176/appi.ajp.162.2.324. [DOI] [PubMed] [Google Scholar]
- 35.Otto MW, Reilly-Harrington NA, Kogan JN, Henin A, Knauz RO, Sachs GS. Managing bipolar disorder: A cognitive-behavioral approach (Therapist guide) Oxford University Press; New York: 2009. [Google Scholar]
- 36.Sajatovic M, Davies M, Hrouda DR. Enhancement of treatment adherence among patients with bipolar disorder. Psychiatr Serv. 2004 Mar;55(3):264–9. doi: 10.1176/appi.ps.55.3.264. [DOI] [PubMed] [Google Scholar]
- 37.Scott J, Garland A, Moorhead S. A pilot study of cognitive therapy in bipolar disorders. Psychol Med. 2001;31(3):459–67. doi: 10.1017/s0033291701003373. [DOI] [PubMed] [Google Scholar]
- 38.Scott J, Paykel E, Morriss R, et al. Cognitive-behavioural therapy for severe and recurrent bipolar disorders: randomised controlled trial. Br J Psychiatry. 2006 Apr;188:313–20. doi: 10.1192/bjp.188.4.313. [DOI] [PubMed] [Google Scholar]
- 39.Miklowitz DJ, Simoneau TL, George EL, et al. Family-focused treatment of bipolar disorder: 1-year effects of a psychoeducational program in conjunction with pharmacotherapy. Biol Psychiatry. 2000;48(6):582–92. doi: 10.1016/s0006-3223(00)00931-8. [DOI] [PubMed] [Google Scholar]
- 40.Rea MM, Tompson MC, Miklowitz DJ, et al. Family-focused treatment versus individual treatment for bipolar disorder: results of a randomized clinical trial. J Consult Clin Psychol. 2003;71(3):482–92. doi: 10.1037/0022-006x.71.3.482. [DOI] [PubMed] [Google Scholar]
- 41.Frank E, Swartz HA, Kupfer DJ. Interpersonal and social rhythm therapy: managing the chaos of bipolar disorder. Biol Psychiatry. 2000;48(6):593–604. doi: 10.1016/s0006-3223(00)00969-0. [DOI] [PubMed] [Google Scholar]
- 42.Frank E, Kupfer DJ, Thase ME, et al. Two-year outcomes for interpersonal and social rhythm therapy in individuals with bipolar I disorder. Arch Gen Psychiatry. 2005;62(9):996–1004. doi: 10.1001/archpsyc.62.9.996. [DOI] [PubMed] [Google Scholar]
- 43.Sachs GS, Thase ME, Otto MW, Bauer M, Miklowitz D, Wisniewski SR, Lavori P, Lebowitz B, Rudorfer M, Frank E, Nierenberg AA, Fava M, Bowden C, Ketter T, Marangell L, Calabrese J, Kupfer D, Rosenbaum JF. Rationale, design, and methods of the systematic treatment enhancement program for bipolar disorder (STEP-BD). Biol Psychiatry. 2003 Jun 1;53(11):1028–42. doi: 10.1016/s0006-3223(03)00165-3. [DOI] [PubMed] [Google Scholar]
- 44.Miklowitz DJ, Otto MW, Frank E, et al. Intensive psychosocial intervention enhances functioning in patients with bipolar depression: results from a 9-month randomized controlled trial. Am J Psychiatry. 2007;164(9):1340–7. doi: 10.1176/appi.ajp.2007.07020311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mitchell PB, Malhi GS. Bipolar depression: phenomenological overview and clinical characteristics. Bipolar Disord. 2004 Dec;6(6):530–9. doi: 10.1111/j.1399-5618.2004.00137.x. [DOI] [PubMed] [Google Scholar]
- 46.Sachs GS, Nierenberg AA, Calabrese JR, Marangell LB, Wisniewski SR, Gyulai L, Friedman ES, Bowden CL, Fossey MD, Ostacher MJ, Ketter TA, Patel J, Hauser P, Rapport D, Martinez JM, Allen MH, Miklowitz DJ, Otto MW, Dennehy EB, Thase ME. Effectiveness of adjunctive antidepressant treatment for bipolar depression. N Engl J Med. 2007 Apr 26;356(17):1711–22. doi: 10.1056/NEJMoa064135. [DOI] [PubMed] [Google Scholar]
- 47.Gitlin M. Treatment-resistant bipolar disorder. Mol Psychiatry. 2006 Mar;11(3):227–40. doi: 10.1038/sj.mp.4001793. [DOI] [PubMed] [Google Scholar]
- 48.Treuer T, Tohen M. Predicting the course and outcome of bipolar disorder: a review. Eur Psychiatry. 2010 Oct;25(6):328–33. doi: 10.1016/j.eurpsy.2009.11.012. [DOI] [PubMed] [Google Scholar]
- 49.Berk M, Parker G. The elephant on the couch: side-effects of psychotherapy. Aust N Z J Psychiatry. 2009 Sep;43(9):787–94. doi: 10.1080/00048670903107559. [DOI] [PubMed] [Google Scholar]
- 50.Johnson SL. Life events in bipolar disorder: towards more specific models. Clin Psychol Rev. 2005 Dec;25(8):1008–27. doi: 10.1016/j.cpr.2005.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Miklowitz DJ, Johnson SL. The psychopathology and treatment of bipolar disorder. Annu Rev Clin Psychol. 2006;2:199–235. doi: 10.1146/annurev.clinpsy.2.022305.095332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Peterson C, Semmel A, von Baeyer C, Abramson LY, Metalsky GI, Seligman MEP. The Attributional Style Questionnaire. Cog Ther Res. 1982;6:287–300. [Google Scholar]
- 53.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders. Biometrics Research Department, New York State Psychiatric Institute; New York: 1995. [Google Scholar]
- 54.Sachs GS. Use of clonazepam for bipolar affective disorder. J Clin Psychiatry. 1990;51:31–34. [PubMed] [Google Scholar]
- 55.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(suppl 20):22–33. [PubMed] [Google Scholar]
- 56.Otto MW, Reilly-Harrington NA, Knauz RO, Henin A, Kogan JN, Sachs GS. Managing bipolar disorder: A cognitive behavior treatment program workbook. Oxford University Press; New York: 2008. [Google Scholar]
- 57.Miklowitz DJ. Bipolar Disorder: A family-focused treatment approach. 2nd edition Guilford Press; New York: 2010. [Google Scholar]
- 58.Frank E. Treating bipolar disorder: A clinician's guide to interpersonal and social rhythm therapy. Guilford Press; New York: 2005. [Google Scholar]
- 59.Sachs GS, Guille C, McMurrich SL. A clinical monitoring form for mood disorders. Bipolar Disord. 2002;4:323–327. doi: 10.1034/j.1399-5618.2002.01195.x. [DOI] [PubMed] [Google Scholar]
- 60.Otto MW, Simon NM, Wisniewski SR, Miklowitz DJ, Kogan JN, Reilly-Harrington NA, Frank E, Nierenberg AA, Marangell LB, Sagduyu K, Weiss RD, Miyahara S, Thas ME, Sachs GS, Pollack MH, STEP-BD Investigators Prospective 12-month course of bipolar disorder in out-patients with and without comorbid anxiety disorders. Br J Psychiatry. 2006 Jul;189:20–5.35. doi: 10.1192/bjp.bp.104.007773. [DOI] [PubMed] [Google Scholar]
- 61.Phillips ML, Travis MJ, Fagiolini A, Kupfer DJ. Medication effects in neuroimaging studies of bipolar disorder. Am J Psychiatry. 2008 Mar;165(3):313–20. doi: 10.1176/appi.ajp.2007.07071066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Reilly-Harrington NA, Miklowitz DJ, Otto MW, Frank E, Wisniewski SR, Thase ME, Sachs GS. Dysfunctional attitudes, attributional styles, and phase of illness in bipolar disorder. Cog Ther Res. 2010;34:24–34. [Google Scholar]
- 63.Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Arch Gen Psychiatry. 2002 Oct;59(10):877–83. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- 64.Aiken LS, West SG. Multiple Regression: Testing and interpreting interactions. Sage; Newbury Park, CA: 1991. [Google Scholar]
- 65.Roberts JE, Gilboa E, Gotlib IH. Ruminative response style and vulnerability to episodes of dysphoria: Gender, neuroticism and episode duration. Cog Ther Res. 1998;22:401–23. [Google Scholar]
- 66.Mathews A, MacLeod C. Cognitive vulnerability to emotional disorders. Annu Rev Clin Psychol. 2005;1:167–95. doi: 10.1146/annurev.clinpsy.1.102803.143916. [DOI] [PubMed] [Google Scholar]
- 67.Jaeger J, Berns S, Loftus S, Gonzalez C, Czobor P. Neurocognitive test performance predicts functional recovery from acute exacerbation leading to hospitalization in bipolar disorder. Bipolar Disord. 2007 Feb-Mar;9(1-2):93–102. doi: 10.1111/j.1399-5618.2007.00427.x. [DOI] [PubMed] [Google Scholar]
- 68.Teasdale JD, Moore RG, Hayhurst H, Pope M, Williams S, Segal ZV. Metacognitive awareness and prevention of relapse in depression: empirical evidence. J Consult Clin Psychol. 2002 Apr;70(2):275–87. doi: 10.1037//0022-006x.70.2.275. [DOI] [PubMed] [Google Scholar]
- 69.Williams JM, Alatiq Y, Crane C, Barnhofer T, Fennell MJ, Duggan DS, Hepburn S, Goodwin GM. Mindfulness-based Cognitive Therapy (MBCT) in bipolar disorder: preliminary evaluation of immediate effects on between-episode functioning. J Affect Disord. 2008 Apr;107(1-3):275–9. doi: 10.1016/j.jad.2007.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Deckersbach T, Hölzel BK, Eisner LR, Stange JP, Peckham AD, Dougherty DD, Rauch SL, Lazar S, Nierenberg AA. Mindfulness-based cognitive therapy for nonremitted patients with bipolar disorder. CNS Neurosci Ther. 2012 Feb;18(2):133–41. doi: 10.1111/j.1755-5949.2011.00236.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Miklowitz DJ, Alatiq Y, Goodwin GM, et al. A pilot study of mindfulness-based cognitive therapy for bipolar disorder. Int J Cogn Ther. 2009;2:373–-82. [Google Scholar]
- 72.Alloy LB, Abramson LY, Walshaw PD, Keyser J, Gerstein RK. Adolescent-onset bipolar spectrum disorders: A cognitive vulnerability-stress perspective. In: Miklowitz DJ, Cicchetti D, editors. Understanding bipolar disorder: A developmental psychopathology perspective. Guilford Press; New York: 2010. pp. 282–330. [Google Scholar]
- 73.Strakowski SM. Approaching the challenge of bipolar depression: results from STEP-BD. Am J Psychiatry. 2007 Sep;164(9):1301–3. doi: 10.1176/appi.ajp.2007.07060926. [DOI] [PubMed] [Google Scholar]
- 74.Hankin BL, Fraley RC, Abela JR. Daily depression and cognitions about stress: Evidence for a traitlike depressogenic cognitive style and the prediction of depressive symptoms in a prospective daily diary study. J Pers Soc Psychol. 2005 Apr;88(4):673–85. doi: 10.1037/0022-3514.88.4.673. [DOI] [PubMed] [Google Scholar]
- 75.Deckersbach T, Nierenberg AA, Kessler R, Lund HG, Ametrano RM, Sachs G, Rauch SL, Dougherty D. Cognitive rehabilitation for bipolar disorder: An open trial for employed patients with residual depressive symptoms. CNS Neurosci Ther. 2010 Oct;16(5):298–307. doi: 10.1111/j.1755-5949.2009.00110.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Tabachnik BG, Fidell LS. Using multivariate statistics. 5th ed. Pearson; Boston: 2007. [Google Scholar]