Abstract
As treatment for stroke has improved, individuals are living longer with the effects of a stroke. The resulting long-term impairment can affect both survivors’ of stroke (SS) and their caregivers’ (CG) health related quality of life (HRQOL). Few studies have examined the HRQOL of SS and their CG greater than two years post stroke. SS and their spousal CG (n=30 dyads) who had previously completed a 12-month study following discharge from inpatient rehabilitation were assessed at 3–5 years post stroke. Health related quality of life (HRQOL) and related outcomes were measured for SS and CG. Data from baseline to 12 months were used in conjunction with data from the present study. Linear mixed models were used to analyze the change in repeated measures over time. Multiple linear regression was used to analyze the relationship of generic HRQOL to related psychosocial outcomes. SS were an average of 4.68 years post stroke. The mean age for SS and CG was 70.8 and 64.9 years, respectively. The majority of SS were male (80%) and non-Hispanic white (70%). Among SS, depression decreased from baseline to 12 months (p=0.04) but increased from 12 months to end of follow-up (p=0.003). CG depression decreased from baseline to all time points (p=0.015). Stroke-specific HRQOL showed statistically significant (p < 0.03) decreases between 12 months and end of follow-up. Increased number of illnesses and older age were associated with CG lower physical HRQOL score (p=0.004). Higher depression was associated with lower mental HRQOL score for both CG and SS (p= 0.003 & p=0.011, respectively). SS and CG continue to experience negative stroke related health outcomes for many years after the initial stroke; some of these outcomes even worsen over time. These findings illustrate the need for ongoing psychological and medical evaluation for both long-term SS and CG. Development and testing of targeted behavioral interventions are also warranted.
Keywords: stroke, health-related quality of life, long-term survivors of stroke, spousal caregivers
INTRODUCTION
Stroke is a chronic, disabling condition affecting millions of people (Roger, et al., 2012). The co-morbidities and life-style changes associated with stroke can put substantial burden on survivors of stroke, and their caregivers, which ultimately can affect both of their health-related quality of life (HRQOL). HRQOL encompasses the physical, functional, psychological and social dimensions of health (de Haan, Aaronson, Limbur, Hewer, & van Crevel, 1992). While there has been considerable discussion in the stroke rehabilitation literature on what constitutes quality of life after a stroke and how it is measured during the acute and rehabilitative phases of recovery up to one year post stroke (Geyh, Kollertis, Grimby, & Stucki, 2007; Kwok, et al., 2006; Olsson, Secrest & Zeller, 2007; Soderfeldt, & Samuelsson, 1996; White, et al., 2007), limited attention has been given to the natural history of HRQOL in both long-term survivors of stroke and family caregivers greater than 2 years after a stroke.
Researchers have often studied survivors of stroke or caregivers in isolation from each other. The Auckland Stroke Study found that, when compared to the general population, survivors of stroke six years post stroke scored lower on physical functioning and general health as measured by the SF-36, a measure of generic HRQOL (Hackett, Duncan, Anderson, Broad, & Bonita, 2000). Findings from the North East Melbourne Stroke Incidence Study have been reported on survivors of stroke at 2, 5 and 7 years post stroke; 20–25% of survivors of stroke reported very low HRQOL at all three time points (Sturm, et al., 2004; Paul, et al., 2005; Leach, Gall, Dewey, Macdonell & Thrift, 2011). Additionally, a ten year follow-up study of the South London Stroke Registry reported physical domain HRQOL scores, as measured by the SF-12, to remain relatively stable from 3 months to 10 years post stroke while mental domain HRQOL scores varied over time (Wolfe, et al., 2011).
Similar to survivors of stroke, it has been suggested that HRQOL may decline over time for family caregivers (White, Mayo, Hanley, & Wood-Dauphinee, 2003). Despite the call for caregivers of survivors of stroke to be included in longitudinal research of HRQOL (Hopman & Verner, 2003; Lim & Zebrack, 2004), little has been reported in the literature regarding the long-term HRQOL of caregivers of survivors of stroke. However, HRQOL of family caregivers more than 2 years post-stroke has been reported in a few studies (Bluvol & Ford-Gilboe, 2004; McPherson, Wilson, Chyurlia, & Leclerc, 2011; Morimoto, Schreiner, & Asano, 2003). A cross-sectional study of Canadian survivors of stroke and their spousal or committed partner caregivers who were on average 2.5 years post stroke found caregivers to have higher quality of life than survivors of stroke as measured by the Reintegration to Normal Living Index, which was used as a proxy for quality of life (Bluvol & Ford-Gilboe, 2004). Conversely, among a sample of Japanese caregivers and survivors of stroke, only 42.3% of caregivers reported “good” HRQOL as measured by the SF-12 while 63% of survivors of stroke reported “good” HRQOL (Morimoto, et al., 2003). A separate study of Canadian survivors of stroke and their caregivers found HRQOL of caregivers to be moderately correlated with HRQOL of survivors of stroke (McPherson, et al., 2011). While these studies have included measures of HRQOL for both survivors of stroke and caregivers, all of these studies have been cross-sectional studies making it impossible to know the change in HRQOL and related outcomes for caregivers over time.
Previous research has demonstrated that depressive symptoms among survivors of stroke and their spouses are frequent and associated with decreased HRQOL (Kong & Yang, 2006; Sturm et al., 2004). Not only is depression in survivors of stroke common immediately after stroke, but it has been shown to persist over time (van de Port, Kwakkel, Bruin, & Lindeman, 2007) with risk of occurrence being similar for those in early, mid and late stages of stroke recovery (Hackett, Yapa, Parag, & Anderson, 2005). Likewise, depressive symptoms among spouses of survivors of stroke have been reported across the stages of stroke recovery (Berg, Palomäki, Lönnqvist, Lehtihalmes, & Kaste, 2005; Visser-Meily, et al., 2009). Spouses of survivors of stroke have shown decreases in depression initially (Berg, et al., 2005; Visser-Meily, et al., 2009) but an increase in depression at three years post stroke (Visser-Meily, et al., 2009).
The combination of loss, prolonged distress and depression, and physical demands of caregiving have resulted in caregiver burden and decreased caregiver quality of life (Visser-Meily, Post, Schepers, & Lindeman, 2005). A study of survivors of stroke and caregivers at 3 months and 1 year post stroke found caregiver burden to be inversely correlated with caregiver quality of life and positively correlated with increased patient disability, anxiety and depression (McCullagh, Brigstocke, Donaldson, & Kalra, 2005). The cross-sectional study of caregivers of Japanese survivors of stroke mentioned above also found increased caregiver burden to be associated with decreased HRQOL, especially mental health. Although 22% of these caregivers had been in their caregiving role for greater than 5 years, the majority (57.9%) of these caregivers had been providing care for less than 2 years (Morimoto, et al., 2003). While studies have shown an association between caregiver burden and HRQOL (Morimoto, et al., 2003; McCullagh, et al., 2005), these studies have not been longitudinal studies of caregiver burden and HRQOL greater than 2 years post stroke.
While caregiving can be stressful, it can also be rewarding for the caregiver and care receiver. One positive aspect of the caregiving relationship, mutuality, is the shared pleasure that the caregiver and care receiver derive from the caregiving relationship (Archbold, Stewart, Greenlick, & Harvath, 1990). Increased mutuality has been found to be positively associated with improved caregiver and patient reported outcomes (Archbold, et al., 1990; Kneeshaw, Considine, & Jennings, 1999; Lyons, Sayer, Archbold, Hornbrook, & Stewart, 2007) while lower mutuality has been related to negative caregiving outcomes (Halm & Bakas, 2007). Little research has been done on the association between mutuality and HRQOL. In a study of persons with Parkinson’s disease and their spousal caregivers, increased mutuality was associated with increased mental health quality of life, as measured by the SF-12, of caregivers. No association was found for mutuality and physical quality of life for caregivers or persons with Parkinson’s disease (Tanji et al., 2008). Mutuality has also been associated with both survivors’ of stroke and their spousal caregivers’ life satisfaction (Ostwald, Godwin, & Cron, 2009).
As mortality rates from stroke decline, individuals are increasingly likely to live with serious disability which can greatly impact their well-being (Clarke, Marshall, Black, & Colantonio, 2002), including their HRQOL, depression, burden and mutuality. Research on the caregiving process has demonstrated that many factors influence HRQOL for both the survivors of stroke and the family caregivers. The purpose of this study was to measure HRQOL, and its related determinants, in long-term survivors of stroke and their spousal caregivers who were more than 2 years post stroke.
METHODS
This study evaluated health related quality of life (HRQOL) in a sample of long-term survivors of stroke and caregivers who had previously completed an interventional study referred to as Committed to Assisting with Recovery after Stroke (CAReS) (Sharon K. Ostwald, PI, R01NR05316). CAReS was an intervention that provided survivors of stroke and their spousal caregivers with education, skills training, counseling, and referrals to community agencies. CAReS enrolled 159 survivors of stroke and their spousal caregivers from 2001 to 2005; CAReS participants were followed for a one year period after the survivor of stroke was discharged from an inpatient setting. Survivors of stroke who participated in the CAReS study had to be at least 50 years of age, have a diagnosis of stroke and be discharged home with a spouse or committed partner. The couple had to live within 50 miles of the Texas Medical Center, speak English, and be able to be reached by telephone. Neither member of the couple could have a major illness that greatly impacted their life (i.e., dementia, advanced cancer, hepatic or renal failure or fractured lower extremity) or a life expectancy of 6 months or less. CAReS was approved by the University’s Institutional Review Board (IRB) and by the IRB’s of the facilities from which the participants were recruited.
Sample Recruitment
CAReS participants were eligible to participate in the present study if they had completed 12 months of the CAReS study and if both members of the couple were still living in the home. Persons meeting the inclusion criteria were sent a letter explaining the study and asking if they were interested in participating. Follow-up phone calls were conducted to assess interest. If the couple was interested in participating in the study, the project coordinator scheduled an in-person interview. Signed informed consent was obtained prior to data collection.
Data Collection
Data were collected at one time point (which was greater than two years post stroke) in the couple’s home by a trained data collector. Data were entered into a database and double checked for accuracy. Changes in either the stroke survivor’s or caregiver’s health information were updated at the time of data collection. Data collected for this study were then merged with data previously collected in the CAReS study. The following instruments were used to measure the dyad’s HRQOL and related outcomes.
Instruments
The Short Form Health Survey (SF- 36) questionnaire was used to measure the HRQOL of both the survivor of stroke and the caregiver. Widely used in studies on disease burden and illness, the SF-36 was created to assess health status in clinical settings and health research studies (Ware & Sherbourne, 1992). The 36-item survey measures eight concepts including: limitations in physical activities due to health issues, limitations in social activities due to emotional or physical issues, limitations in normal role activities due to physical health issues, bodily pain, general mental health (well-being and psychological distress), limitations in normal role activities due to emotional problems, vitality (fatigue and energy), and general health perceptions. The eight concepts form two summary measures: Physical and Mental Health. Respondents score each item on either a three or five-point Likert-type scale. Reliability estimates from numerous studies have shown the SF-36 to have high validity and reliability (Ware, 2010).
The Stroke Impact Scale (SIS) version 3.0 (Duncan, Bode, Min Lai, & Perera, 2003) was used to measure stroke-specific quality of life among the survivors of stroke in the study. Developed to assess changes over time in disabilities, handicaps, and impairments, the 59-item assessment has eight domains: mobility(9), memory and thinking(7), emotion(9), communication(7), social participation(8), instrumental and physical activities of daily living(10), strength(4), and hand function (5). Individuals respond on a five point Likert-type scale. Three items have reverse scoring. Domains are scored by dividing the difference of the actual raw score and the lowest possible score by the possible raw score range. A higher score indicates better reported HRQOL. The SIS has been found to be a valid and reliable instrument (Duncan, et al., 2003).
The Geriatric Depression Scale (GDS) short-form, used to assess symptoms of depression for both members of the couple, is a 15 question survey developed first by Yesavage and colleagues (1983) to measure depression in the elderly population. Questions are answered with a “Yes” or “No”; five of the questions are reverse scored. A reported score of 0–4 indicates normal mental status, 5–8 denotes mild depression, 9–11 denotes moderate depression, and 12–15 denotes severe depression. Testing showed that the GDS has 89% specificity and 92% sensitivity while a validation study showed that both the long (30-question) and short form of the GDS were able to differentiate depressed from non-depressed adults with a high correlation score (r= .84, p <.001) (Sheikh & Yesavage, 1986).
Mutuality is defined as the ability that caregivers have to find gratification when providing care and to feel reciprocated emotion or appreciation by the care receiver. Mutuality was assessed for both the survivor of stroke and caregiver using the Mutuality Scale (Archbold, et al., 1990). The questionnaire was part of the Family Caregiving Inventory and has 15-items on a 5-point Likert scale with a score range from 0–60. A higher score indicates a more positive relationship between the caregiver and care receiver. High validity and reliability greater than 0.90 has been reported when tested during two different time measurements (Archbold, et al., 1990).
The Zarit Burden interview (ZBI) is one of the most commonly used questionnaires to assess burden among caregivers of elderly, cognitively impaired adults. The 22-item questionnaire is a revision of the original 29-item survey. Respondents answer questions on a 4 point Likert-type scale. Scoring on the ZBI 22-item version ranges from 0–88. Those with a score of 0–21 implied little or no burden, 21–40 implied mild to moderate burden, 41–60 implied moderate to severe burden, and 61–88 implied severe burden (Zarit, Orr, & Zarit, 1985). The ZBI 22-item questionnaire has been reported as having good reliability (Chronbach’s α =0.88) (Bedard, et al., 2001).
Data Analysis
Descriptive statistics were generated to check for potential errors and to examine the distribution of the instrument scores. Descriptive and inferential statistics were computed on participants’ demographic, health-related quality of life and associated variables to describe characteristics of the study sample. Time from stroke was calculated as the difference in the date of data collection in the present study and baseline visit of the parent study. Level of significance for all statistical tests was set at 0.05.
The mean scores for long-term survivors of stroke and spousal caregivers on the physical component summary (PCS) and mental component summary (MCS) of the SF-36 were compared to normative means published in the SF-36 scoring manual (Ware, Kosinski, & Dewey, 2000). The one sample t-test was used to compare the survivors’ of stoke mean scores to normative means for the 65–74 age group, the predominant age group for survivors of stroke in this study. Mean scores for the spousal caregivers were also compared to normative means with the one sample t-test. Normative scores for the 55–64 age group were used for the latter comparison, as this was the predominant age group for the caregivers in this study.
Repeated measures analysis was used to determine participants’ change over time on the SIS, GDS, Mutuality, and Burden scales. Specifically, linear mixed models (Brown & Prescott, 2006) were used to analyze the change in scale/subscale scores over time, with one model developed for each scale/subscale. The ‘days since stroke’ variable was included in the models as a covariate to assess its effects on the change in the above mentioned variables over time.
Multiple linear regression (Kleinbaum, Kupper, & Muller, 1988) was used to analyze the relationship of participants’ HRQOL in the present study to depression, mutuality, number of illnesses, age, ethnicity and SES. Separate models were analyzed using PCS and MCS scores on the SF-36 as dependent variables.
RESULTS
Thirty couples were interviewed for this study. The majority of survivors of stroke in this study were male (80%, n=24) (Table 1). The mean age was 70.8 and 64.9 years for survivors of stroke and caregivers, respectively. Approximately one third of the sample was an ethnic minority as represented by African American (15%) and Hispanic (15%) individuals. The average number of years since stroke was 4.68 (SD = .91, Range= 2.95–6.29).
Table 1.
Descriptive Statistics of Caregiver and Stroke Survivor Demographics
| Variable | Caregiver (n=30) | Stroke Survivor (n=30) | ||||
|---|---|---|---|---|---|---|
| X̅ | SD | Range | X̅ | SD | Range | |
| Age | 64.9 | 9.8 | 51.5–88.6 | 70.8 | 9.4 | 53.2–88.1 |
| Number of Illnesses | 2.08 | 1.57 | 0–6 | 3.72 | 1.89 | 0–7 |
| n | % | n | % | |||
| Gender | ||||||
| Male | 6 | 20 | 24 | 80 | ||
| Female | 24 | 80 | 6 | 20 | ||
| Race | ||||||
| African American | 5 | 16.7 | 5 | 16.7 | ||
| Hispanic | 6 | 20 | 5 | 16.7 | ||
| Non-Hispanic White | 19 | 63.3 | 20 | 66.7 | ||
Caregivers and survivors of stroke were both found to have significant changes in health-related outcomes over time (Table 2). Both caregivers and survivors of stroke had significant changes in depression from baseline to an average of 4.68 years post stroke. Among survivors of stroke, depression was found to decrease from baseline to 12 months (p=0.043) but to increase from 12 months to end of follow-up (p=0.003). Caregivers’ depression decreased from baseline to all time points (p=0.015). Survivors’ of stroke mutuality showed no statistically significant change over time while caregivers’ mutuality approached statistical significance and lessened over time (p=0.056). Caregivers’ burden did not significantly change over time.
Table 2.
Caregiver and Stroke Survivor Average Score on Study Variables over Time
| Variable | Baseline | 3 Months | 6 Months | 9 Months | 12 Months | >2 Years |
|---|---|---|---|---|---|---|
| Caregiver | ||||||
| Depression a | 3.30 | 2.67 | 2.67 | 2.33 | 2.20 | 2.50 |
| Mutuality | 3.31 | -- | 3.25 | -- | 3.21 | 3.03 |
| Burden | 24.53 | 22.17 | 22.20 | 20.83 | 22.30 | 24.53 |
| Stroke Survivor | ||||||
| Depression c | 3.30 | 3.07 | 2.57 | 3.13 | 2.37 | 3.73 |
| Mutuality | 3.59 | -- | 3.41 | -- | 3.44 | 3.45 |
| SIS Emotion b,c | 78.47 | 79.23 | 81.53 | 79.73 | 81.50 | 72.48 |
| SIS Communication c | 83.53 | 90.27 | 86.93 | 85.97 | 91.48 | 82.45 |
| SIS Memory b,c | 79.87 | 81.80 | 85.33 | 86.17 | 87.62 | 71.57 |
| SIS Physical a,c | 50.20 | 62.70 | 68.77 | 66.87 | 66.48 | 61.13 |
| SIS Social Participation a,c | 46.93 | 67.27 | 70.17 | 70.30 | 75.07 | 60.21 |
significant (p<.05) improvement from baseline to last time point
significant (p<.05) worsening from baseline to last time point
significant (p<.05) worsening from 12 Months to last time point
Long-term survivors of stroke had significantly lower scores for than the age matched community dwelling general population using the SF-36 (Table 3), a generic HRQOL measure. Survivors of stroke reported significantly lower scores on the domains of physical functioning, role physical, general health, social functioning, and role emotional as well as on both the physical and mental summary scales. Conversely, for caregiver physical and mental HRQOL, no statistically significant differences were seen between the age matched, community dwelling general population and spousal caregivers.
Table 3.
Comparison of Caregivers and Stroke Survivors to Normative Population Means on the SF-36
| CG |
SS |
|||||
|---|---|---|---|---|---|---|
| Domain | U.S. Pop 55–64 |
Mean | p-value | U.S. Pop 65–74 |
Mean | p-value |
| Physical Functioning | 47.56 | 47.49 | .970 | 44.46 | 35.01 | <.001 |
| Role Physical | 48.32 | 48.85 | .733 | 45.52 | 33.33 | <.001 |
| Bodily Pain | 48.41 | 48.79 | .799 | 47.81 | 45.37 | .261 |
| General Health | 49.08 | 50.38 | .519 | 48.40 | 44.27 | .021 |
| Vitality | 51.17 | 51.26 | .960 | 51.58 | 50.93 | .657 |
| Social Functioning | 49.93 | 51.77 | .192 | 50.08 | 42.63 | .001 |
| Role Emotional | 49.79 | 45.51 | .054 | 48.63 | 36.03 | <.001 |
| Mental Health | 51.25 | 50.48 | .657 | 52.7 | 48.9 | .061 |
| Physical Summary | 47.44 | 49.71 | .091 | 44.70 | 38.25 | .002 |
| Mental Summary | 51.71 | 50.21 | .373 | 53.17 | 47.69 | .012 |
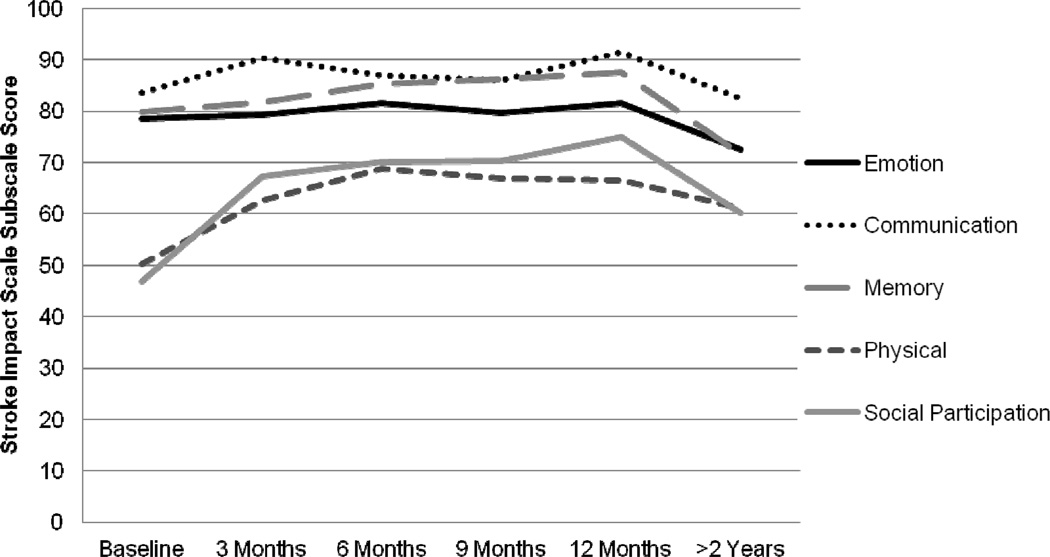
Regarding stroke-specific quality of life, survivors of stroke had significant decreases from baseline to end of follow-up on the SIS subscales of emotion (p=0.043), and memory (p=0.017), but significant increases on the SIS subscales of physical (p<0.0001) and social participation (p=0.003). However, survivors’ of stroke HRQOL showed statistically significant decreases between 12 months and end of follow-up on all SIS subscales (physical (p=0.024), communication (p=0.001), emotion (p=0.003), memory (p<0.0001), and social participation (p=0.001)). (Table 2, Figure 1)
Figure 1.
Changes in Stroke Impact Scale Subscales Over Time
The multiple linear regression analysis showed illness, age and depression to be associated with generic HRQOL (as measured by the SF-36). For caregivers, increased number of illnesses and older age were associated with lower physical HRQOL score (F=7.30, p=0.004). Higher depression was associated with lower mental HRQOL score for both caregivers and survivors of stroke (F=10.97, p= 0.003 & F=7.65, p=0.011, respectively).
DISCUSSION
Our study found survivors of stroke to have significant changes over time in their HRQOL. Similar to those in the Aukland Stroke Study (Hackett, et al., 2000), survivors of stroke reported lower generic HRQOL than age-matched controls on all domains of the SF-36 other than bodily pain, vitality and mental health. While the generic HRQOL reported on survivors of stroke in the South London Stroke Registry remained relatively stable on the HRQOL physical domain and varied over time on the HRQOL mental domain (Wolfe, et al., 2011), our study found the disease-specific HRQOL (SIS) scores for the survivor of stroke to overall trend downwards for emotion and memory but to increase overall in physical and social participation. These overall trends capture the trajectory from baseline to the end of follow-up. However, when the stroke specific HRQOL was examined from 12 months post stroke to the end of follow-up, survivors’ of stroke were found to have significant decreases in all domains (emotion, communication, memory, physical and social participation). This indicates that the survivors’ stroke specific HRQOL worsened after the first year post stroke.
Caregivers had no significant differences in generic HRQOL when compared to age-matched controls. This is incongruent with the findings reported by McPherson and colleagues (2011) who reported that Canadian, partner caregivers of survivors of stroke had lower HQROL on all domains of the SF-36 as compared to the normative population. Perhaps this is due to the differences in time from stroke; McPherson and colleagues (2011) reported their caregivers to be an average of 2.6 years from the stroke event while the caregivers in the present study were an average of 4.8 years post stroke.
Caregivers and survivors of stroke also had significant changes overtime in their HRQOL-related outcomes. Caregivers’ depression decreased over time while survivors’ of stroke depression decreased from baseline to 12 months but then increased after 12 months. The continued presence of stroke survivor depression is congruent with previously reported studies (van de Port, et al, 2007; Hackett, et al., 2005). Survivors’ of stroke perception of the caregiving relationship (mutuality) did not change over time but caregivers’ mutuality did trend towards getting worse over time. Additionally, caregiver burden did not significantly change over time; this is notable because it shows that caregivers had the same amount of burden, on average, at baseline as they did years after their loved one’s stroke. Despite the continued presence of caregiver burden and their worsening perception of the caregiving relationship, caregivers’ depression decreased overtime.
This study does have limitations. First, as this study had a small sample size, caution must be used when applying these findings; generalizability is limited to older, predominately male survivors of stroke and their spousal caregivers in Southeast Texas. Additionally, age associated changes may account for some of the negative findings, such as increased depression (Mirowsky & Ross, 1992) at the later time point for survivors of stroke or the association between increased illness and lower physical HRQOL among caregivers. Also, because the inclusion criteria for both the parent study and the present study required survivors of stroke to be living in their own home during the study, persons who were sicker, and may have possibly had decreased quality of life were excluded. While this study was able to measure the change in HRQOL for survivors of stroke over time and the HRQOL-related outcomes of caregivers over time, we were unable to report on the change in HRQOL of caregivers over time.
Despite these limitations, this study has important implications. Both survivors of stroke and their caregivers continue to experience negative health related outcomes for many years after the initial stroke; some of these outcomes even worsen over time. This study highlights the need for ongoing psychological and medical evaluation for both long-term survivors of stroke and their caregivers. While no significant differences were seen with spousal caregivers in terms of HRQOL in this study, additional study is necessary in that caring for survivors of stroke with continued poor HRQOL may impact other indicators of mental and physical health in this population. As such, large, longitudinal studies, and the development and testing of targeted behavioral and medical interventions for survivors of stroke and their caregivers are warranted.
Nurses caring for long-term survivors of stroke and their caregivers should be aware of the continued impact of the stroke on an individual’s health related quality of life and related psychological wellbeing. Nurses should assess both survivors of stroke and their caregivers for signs of depression, burden and other indicators of psychological distress and make appropriate mental health referrals when necessary. This study also highlights the need for nurses, practicing in a variety of acute and chronic healthcare settings, to educate survivors of stroke and their caregivers about signs and symptoms of depression and burden, and to provide them with information regarding helpful and accessible community resources.
SUMMARY
Stroke often results in serious physical, cognitive and emotional disability for survivors as well as greatly impacting their caregivers. Research has most often focused on the acute and rehabilitative aspects of health care following a stroke. In comparison, very little longitudinal research has been conducted to understand how stroke impacts a survivor’s life long term. Research is needed to elucidate the types of interventions and the best intervals of their delivery to improve the survivor’s quality of life and ability to live a productive life in the community. In addition, even less longitudinal research exists on the long term impact of caregiving on the spouses and family members of survivors of stroke. Little attention has been given to what correlates with a high quality of life, especially for spousal caregivers, and what interventions might help to avoid caregiver burn-out over a long caregiving career. Further study is necessary so that effective, long-term interventions can be developed for both survivors of stroke and their caregivers.
Acknowledgments
This study was supported by grants from the Rehabilitation Nursing Foundation (J. Wasserman, P.I.) and the National Institutes of Nursing Research, National Institutes of Health (S.K. Ostwald, P.I., NR035316).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No conflicts of interest to declare.
Disclaimer: Dr. Wasserman’s participation in this project occurred during her tenure at the University of Texas Health Science Center at Houston, School of Nursing and does not reflect the views of the National Institutes of Health or the United States Government.
REFERENCES
- Archbold PG, Stewart BJ, Greenlick MR, Harvath T. Mutuality and preparedness as predictors of caregiver role strain. Research in Nursing & Health. 1990;13(6):375–384. doi: 10.1002/nur.4770130605. [DOI] [PubMed] [Google Scholar]
- Bédard M, Mollow DW, Squire L, Dubois S, Lever JA, O'Donnell M. The Zarit Burden Interview: A New Short Version and Screening Version. Gerontologist. 2001;41(5):652–657. doi: 10.1093/geront/41.5.652. [DOI] [PubMed] [Google Scholar]
- Berg A, Palomäki H, Lönnqvist J, Lehtihalmes M, Kaste M. Depression among caregivers of stroke survivors. Stroke. 2005;36(3):639–643. doi: 10.1161/01.STR.0000155690.04697.c0. [DOI] [PubMed] [Google Scholar]
- Bluvol A, Ford-Gilboe M. Hope, health work and quality of life in families of stroke survivors. Journal of Advanced Nursing. 2004;48(4):322–332. doi: 10.1111/j.1365-2648.2004.03004.x. [DOI] [PubMed] [Google Scholar]
- Brown H, Prescott R. Applied mixed models in medicine. 2nd ed. Hoboken, NJ: John Wiley & Sons; 2006. [Google Scholar]
- Clarke P, Marshall V, Black SE, Colantonio A. Well-being after stroke in Canadian seniors: Findings from the Canadian Study of Health and Aging. Stroke. 2002;33(4):1016–1021. doi: 10.1161/01.str.0000013066.24300.f9. [DOI] [PubMed] [Google Scholar]
- de Haan R, Aaronson N, Limbur M, Hewer RL, van Crevel H. Measuring quality of life in stroke. Stroke. 1993;24:320–327. doi: 10.1161/01.str.24.2.320. [DOI] [PubMed] [Google Scholar]
- Duncan PW, Bode RK, Min Lai S, Perera S. Rasch analysis of a new stroke-specific outcome scale: the Stroke Impact Scale. Archives of Physical Medicine and Rehabilitation. 2003;84(7):950–963. doi: 10.1016/s0003-9993(03)00035-2. [DOI] [PubMed] [Google Scholar]
- Geyh S, Kollertis B, Grimby G, Stucki G. Content comparison of health-related quality of life measures used in stroke based on the international classification of functioning, disability and health (ICF): a systematic review. Quality of Life Research. 2007;16(5):833–851. doi: 10.1007/s11136-007-9174-8. [DOI] [PubMed] [Google Scholar]
- Hackett ML, Duncan JR, Anderson CS, Broad JB, Bonita R. Health-related quality of life among long-term survivors of stroke: results from the Auckland Stroke Study, 1991–1992. Stroke. 2000;31(2):440–447. doi: 10.1161/01.str.31.2.440. [DOI] [PubMed] [Google Scholar]
- Hackett ML, Yapa C, Parag V, Anderson CS. Frequency of depression after stroke: A systematic review of observational studies. Stroke. 2005;36(6):1330–1340. doi: 10.1161/01.STR.0000165928.19135.35. [DOI] [PubMed] [Google Scholar]
- Halm MA, Bakas T. Factors associated with caregiver depressive symptoms, outcomes, and perceived physical health after coronary artery bypass surgery. Journal of Cardiovascular Nursing. 2007;22(6):508–515. doi: 10.1097/01.JCN.0000297388.21626.6c. [DOI] [PubMed] [Google Scholar]
- Hopman WM, Verner J. Quality of life during and after inpatient stroke rehabilitation. Stroke. 2003;34(3):801–805. doi: 10.1161/01.STR.0000057978.15397.6F. [DOI] [PubMed] [Google Scholar]
- Kleinbaum DG, Kupper LL, Muller KE. Applied regression analysis and other multivariable methods. 2nd ed. Belmont, CA: Duxbury Press; 1988. [Google Scholar]
- Kneeshaw MF, Considine RM, Jennings J. Mutuality and preparedness of family caregivers for elderly women after bypass surgery. Applied Nursing Research. 1999;12(3):128–135. doi: 10.1016/s0897-1897(99)80034-2. [DOI] [PubMed] [Google Scholar]
- Kong KH, Yang SY. Health-related quality of life among chronic stroke survivors attending a rehabilitation clinic. Singapore Medical Journal. 2006;47(3):213–218. [PubMed] [Google Scholar]
- Kwok T, Lo RS, Wong E, Wai-Kwong T, Mok V, Kai-Sing W. Quality of life of stroke survivors: A 1-year follow-up study. Archives of Physical Medicine and Rehabilitation. 2006;87(9):1177–1182. doi: 10.1016/j.apmr.2006.05.015. [DOI] [PubMed] [Google Scholar]
- Leach MJ, Gall SL, Dewey HM, Macdonell RA, Thrift AG. Factors associated with quality of life in 7-year survivors of stroke. Journal of Neurology, Neurosurgery and Psychiatry. 2011;82(12):1365–1371. doi: 10.1136/jnnp.2010.234765. [DOI] [PubMed] [Google Scholar]
- Lim JW, Zebrack B. Caring for family members with chronic physical illness: A critical review of caregiver literature. Health & Quality of Life Outcomes. 2004;2:50. doi: 10.1186/1477-7525-2-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyons KS, Sayer AG, Archbold PG, Hornbrook MC, Stewart BJ. The enduring and contextual effects of physical health and depression on care-dyad mutuality. Research in Nursing & Health. 2007;30(1):84–98. doi: 10.1002/nur.20165. [DOI] [PubMed] [Google Scholar]
- McCullagh E, Brigstocke G, Donaldson N, Kalra L. Determinants of caregiving burden and quality of life in caregivers of stroke patients. Stroke. 2005;36:2181–2186. doi: 10.1161/01.STR.0000181755.23914.53. [DOI] [PubMed] [Google Scholar]
- McPherson CJ, Wilson KG, Chyurlia L, Leclerc C. The caregiving relationship and quality of life among partners of stroke survivors: a cross-sectional study. Health and Quality of Life Outcomes. 2011;9(29) doi: 10.1186/1477-7525-9-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mirowsky J, Ross CE. Age and depression. Journal of Health and Social Behavior. 1992;33:187–205. [PubMed] [Google Scholar]
- Morimoto T, Schreiner AS, Asano H. Caregiver burden and health-related quality of life among Japanese stroke caregivers. Age & Ageing. 2003;32(2):218–223. doi: 10.1093/ageing/32.2.218. [DOI] [PubMed] [Google Scholar]
- Olsson GB, Soderfeldt B, Samuelsson M. Life satisfaction in persons with lacunar infarction--a comparative analysis of two measures of life satisfaction. International Journal of Rehabilitation Research. 1996;19(4):321–325. [PubMed] [Google Scholar]
- Ostwald SK, Godwin KM, Cron S. Predictors of life satisfaction in stroke survivors and spousal caregivers twelve to twenty-four months post discharge from inpatient rehabilitation. Rehabilitation Nursing. 2009;34(4):160–167. 174. doi: 10.1002/j.2048-7940.2009.tb00272.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paul SL, Sturm JW, Dewey HM, Donnan GA, Macdonell RA, Thrift AG. Long-term outcome in the North East Melbourne Stroke Incidence Study: Predictors of quality of life at 5 years after stroke. Stroke. 2005;36(10):2082–2086. doi: 10.1161/01.STR.0000183621.32045.31. [DOI] [PubMed] [Google Scholar]
- Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Turner MB on behalf of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation. 2012;125:e2–e220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Secrest JA, Zeller R. The relationship of continuity and discontinuity, functional ability, depression, and quality of life over time in stroke survivors. Rehabilitation Nursing. 2007;32(4):158–164. doi: 10.1002/j.2048-7940.2007.tb00170.x. [DOI] [PubMed] [Google Scholar]
- Sheikh JI, Yesavage JA. Geriatric depression scale (GDS). Recent evidence and development of a shorter version. In: Brink TL, editor. Clinical gerontology: A guide to assessment and intervention. NY: The Haworth Press, Inc.; 1986. pp. 165–173. [Google Scholar]
- Sturm JW, Donnan GA, Dewey HM, Macdonnell RA, Gilligan AK, Srikanth V, Thrift AG. Quality of life after stroke: the North East Melbourne stroke incidence study (NEMESIS) Stroke. 2004;35(10):2340–2345. doi: 10.1161/01.STR.0000141977.18520.3b. [DOI] [PubMed] [Google Scholar]
- Tanji H, Anderson KE, Gruber-Baldini AL, Fishman PS, Reich SG, Weiner WJ, Shulman LM. Mutuality of the marital relationship in Parkinson’s disease. Movement Disorders. 2008;23(13):1843–1849. doi: 10.1002/mds.22089. [DOI] [PubMed] [Google Scholar]
- van de Port IG, Kwakkel G, Bruin M, Lindeman E. Determinants of depression in chronic stroke: A prospective cohort study. Disability & Rehabilitation. 2007;29(5):353–358. doi: 10.1080/09638280600787047. [DOI] [PubMed] [Google Scholar]
- Visser-Meily A, Post M, Schepers V, Lindeman E. Spouses’ quality of life 1 year after stroke: prediction at the start of clinical rehabilitation. Cerebrovascular Diseases. 2005;20:443–448. doi: 10.1159/000088983. [DOI] [PubMed] [Google Scholar]
- Visser-Meily A, Post M, van de Port I, Maas C, Forstberg-Wärleby G, Lindeman E. Psychosocial functioning of spouses of patients with stroke from initial inpatient rehabilitation to 3 years post stroke: course and relations with coping strategies. Stroke. 2009;40(4):1399–1404. doi: 10.1161/STROKEAHA.108.516682. [DOI] [PubMed] [Google Scholar]
- Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): Conceptual framework and item selection. Medical Care. 1992;30:479–483. [PubMed] [Google Scholar]
- Ware JE, Kosinski M, Dewey JE. How to score version 2 of the SF-36. Health Survey. Lincoln, RI: Quality Metric Incorporated; 2000. [Google Scholar]
- Ware JE. SF-36 Health Survey Update. 2010. From http://www.sf-36.org/tools/sf36.shtml. [DOI] [PubMed] [Google Scholar]
- White CL, Mayo N, Hanley JA, Wood-Dauhpinee S. Evolution of the caregiving experience in the initial 2 years following stroke. Research in Nursing & Health. 2003;26(3):177–189. doi: 10.1002/nur.10084. [DOI] [PubMed] [Google Scholar]
- White JH, Alston MK, Marquez JL, Sweetapple AL, Pollack MR, Attia J, Levi, C.R,. Whyte S. Community-dwelling stroke survivors: function is not the whole story with quality of life. Archives of Physical Medicine & Rehabilitation. 2007;88(9):1140–1146. doi: 10.1016/j.apmr.2007.06.003. [DOI] [PubMed] [Google Scholar]
- Wolfe CDA, Crichton SL, Heuschmann PU, McKevitt CJ, Toschke AM, Grieve AP, Rudd AG. Estimates of outcomes up to ten years after stroke: analysis from the prospective South London Stroke Register. PLoS Medicine. 2011;8(5):e1001033. doi: 10.1371/journal.pmed.1001033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey MB, Leirer VO. Development and validation of a geriatric depression screening scale: A preliminary report. Journal of Psychiatric Research. 1983;17:37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]
- Zarit S, Orr N, Zarit J. The Hidden Victims of Alzheimer's Disease: Families under Stress. New York: University Press; 1985. [Google Scholar]