Abstract
Ecological momentary assessment (EMA) data suggest that global negative affect (NA) increases prior to and decreases following episodes of binge eating and purging, providing support for the affect regulation model of BN. The current study examined whether facets of NA are differentially related to bulimic behaviors. Women with bulimia nervosa (BN; n = 133) completed a 2-week EMA protocol. Momentary assessments of 4 facets of NA (Fear, Guilt, Hostility, and Sadness) were derived from the PANAS subscales. Trajectories of the NA facets were modeled prior to and following binge-only, purge-only, and binge/purge events. Fear, Guilt, Hostility, and Sadness increased prior to and decreased following binge-only and binge/purge events. The same results were found for purge-only events, with the exception that Hostility did not increase significantly prior to purging. Notably, ratings of Guilt were higher than those of Fear, Hostility, and Sadness at the time of binge-only and binge/purge events. Furthermore, post hoc analyses demonstrate that Guilt increased prior to and decreased following the 3 behavior types, even after controlling for Fear, Hostility, and Sadness. These results provide further support for the affect regulation model of BN and also suggest that guilt may be particularly important to the pathology of BN.
Keywords: bulimia nervosa, negative affect, ecological momentary assessment, affect regulation, guilt
Bulimia nervosa (BN) is characterized by recurrent binge eating (BE), defined as eating an unusually large amount of food with a sense of loss of control, and the use of compensatory behaviors such as self-induced vomiting (American Psychiatric Association [APA], 2000). Bulimic symptoms are relatively common in adults and adolescents (e.g., Hoek, 2006) and are associated with serious medical and psychiatric problems, along with increased risk of mortality (e.g., Crow et al., 2009). Although several promising treatments for BN have been identified, the majority of patients remain symptomatic after receiving treatment (e.g., Agras, Crow, et al., 2000). The development of innovative treatments for BN will depend in large part on research efforts to delineate the mechanisms with which bulimic symptoms are maintained over time.
The affect regulation model proposes one possible mechanism by which bulimic symptoms are maintained (Polivy & Herman, 1993). This model posits that BE and purging function to mitigate negative emotional states and that these behaviors are maintained through negative reinforcement. Evidence supporting the affect regulation model relies on data that demonstrate both high levels of NA prior to bulimic behaviors and a decrease in NA following these behaviors. Overall, there is robust evidence that NA is elevated prior to both BE and purging. For example, ecological momentary assessment (EMA) data suggest that BE is more likely to occur on days characterized by stable high NA or increasing NA (Crosby et al., 2009). Furthermore, a recent meta-analysis of EMA data found that NA ratings prior to BE were higher than average ratings of NA (ES = .63) and NA ratings prior to regular eating (ES = .68; Haedt-Matt & Keel, 2011). Perhaps most compelling are data from an EMA study that used multilevel modeling to illustrate that NA increases over the 4 hours prior to bulimic behaviors (Smyth et al., 2007). In contrast, the evidence that NA decreases after bulimic behaviors is less consistent. The above-referenced meta-analysis found that NA ratings made after BE were higher than those made before BE (ES = .50; Haedt-Matt & Keel, 2011). However, results from a recent EMA study found that NA decreased significantly over the 4 hours following bulimic behaviors (Smyth et al., 2007). It is possible that the inconsistent findings are due to differences in the statistical methodology used by each study; the meta-analysis compared NA ratings made at two single time points, whereas the EMA study modeled the trajectory of NA over 4 hours using all available data.
One limitation of the current literature on the affect regulation model of BN is that NA is a broad construct that encompasses many types of emotional experiences (e.g., depression, anxiety). Determining whether bulimic behaviors are related to NA in general or to a particular facet of NA (e.g., depression) is particularly important to treatment development, because it has the potential to determine the content and focus of new interventions. Six previous investigations have compared facets of NA at different time points in relation to episodes of BE in women with BN (Corstorphine, Waller, Ohanian, & Baker, 2006; Elmore & de Castro, 1990; Hetherington, Altemus, Nelson, Bernat, & Gold, 1994; Johnson & Larson, 1982; Kaye, Gwirtsman, George, Weiss, & Jimerson, 1986; Powell & Thelen, 1996). The most common facets of NA examined were depression, anxiety, anger, and guilt. The most common comparisons were immediately prior to BE versus immediately after BE and immediately after BE versus some point in time after BE (which varied between studies). The results of the six studies are relatively inconsistent, both within (e.g., comparing the trajectories of depression and anxiety within a single study) and between studies (e.g., comparing the trajectory of depression across studies; see Table 1).
Table 1.
Changes in Facets of Negative Affect During and After Episodes of Binge Eating
| Study | N | Length | Depression
|
Anxiety
|
Anger/frustration
|
Guilt
|
||||
|---|---|---|---|---|---|---|---|---|---|---|
| Prebinge to postbinge | After binge | Prebinge to postbinge | After binge | Prebinge to postbinge | After binge | Prebinge to postbinge | After binge | |||
| Elmore & Castro (1990) | 19 | 7 days | Increase | — | Decrease | — | — | — | — | — |
| Corstorphine et al. (2006) | 23 | 7 days | No change | No change | Increase | No change | No change | No change | Increase | No change |
| Hetherington et al. (1994) | 10 | 7 days | Increase | Increase | Decrease | Decrease | — | — | — | — |
| Johnson & Larson (1982) | 15 | 7 days | — | Increase | — | — | — | Decrease | — | Decrease |
| Kaye et al. (1986) | 12 | 1 day | No change | No change | Decrease | Decrease | — | — | — | — |
| Powell & Thelen (1996) | 22 | 6 days | No change | Decrease | No change | Decrease | No change | No change | — | — |
These inconsistencies are notable; however, Table 1 highlights several possible explanations for the discrepancies. First, each study examines multiple facets of NA, each of which could follow a different trajectory in relation to bulimic behaviors (e.g., depression could increase prior to and decrease after BE, whereas anxiety could decrease prior to and increase after BE). Although facets of NA are often highly correlated and load onto a higher-order factor (global NA), findings from these previous investigations appear to provide preliminary support for this hypothesis. Second, it is also important to note that BN is characterized by both BE and compensatory behaviors, which are often, but not always linked (Agras, Walsh, Fairburn, Wilson, & Kraemer, 2000). Thus, another possibility is that BE and compensatory behaviors may be differentially related to NA, but unfortunately, previous investigators have not distinguished these behaviors in their analyses. Third, there were notable discrepancies between the studies with regard to the time at which affect was measured (e.g., an hour after BE, immediately after purging). Thus, the inconsistencies in the trajectories of NA between the studies could be due to differences in the time frames being assessed.
Another possible explanation for the inconsistent findings with regard to the relationship between facets of NA and bulimic behaviors in previous investigations relates not only to when NA was assessed, but also to how it was assessed. It is important to note that these previous investigations are strengthened by the use of EMA rather than retrospective recall data. Whereas retrospective recall requires participants to remember events that occurred in the past, EMA allows for the assessment of events in real time. Thus, EMA data are less likely to be influenced by biases common to retrospective recall, including current mood (Teasdale & Fogarty, 1979), retroactive reconstruction, and effort after meaning (Stone & Shiffman, 1994). However, a limitation of these studies, and a possible explanation for the inconsistent findings, is that they collected EMA data using paper-and-pencil assessments, which cannot be time stamped. Without a time stamp, it cannot be guaranteed that participants completed ratings of NA at the specified times, which means that the temporal relationship between assessments cannot be validated. Previous research has demonstrated that participants’ reported compliance with paper-and-pencil EMA (90%) vastly overestimates their actual compliance (10%; Stone, Shiffman, Schwartz, Broderick, & Huffor, 2003). A second limitation of the investigations described above is that these studies characterized the temporal relationship between affect and behavior by comparing affect ratings at single time points in relation to bulimic behaviors (e.g., “prebinge” vs. “postbinge”). Although a comparison of means analysis can demonstrate whether there is a statistically significant difference between the magnitude of affect at those time points, this type of analysis cannot provide any information about the trajectory of affect between those time points.
In summary, previous investigations suggest that facets of NA could be differentially related to bulimic behaviors. These results have important implications for our understanding of maintenance mechanisms of BN (e.g., bulimic behaviors may effectively reduce anxiety but not depression) and subsequently could influence the focus of future treatments (e.g., anxiety management). Unfortunately, conclusions about the role of facets of NA in BN are premature given the methodological limitations of previous investigations. The objective of the current study was to examine whether facets of NA are differentially related to bulimic behaviors using a rigorous methodology. First, we specifically distinguished among binge-only, purge-only, and binge/purge events to examine whether these behaviors are differentially related to NA. Second, we collected time-stamped EMA data using palm-top computers to know exactly when assessments of affect were made in relation to bulimic behaviors. Finally, we analyzed all data points using multivariate modeling to examine the trajectory of affect in relation to bulimic behaviors. On the basis of the current literature, we expected to find that all facets of NA will increase prior to all three types of bulimic behaviors (i.e., binge-only, purge-only, and binge/purge events) and that the four facets of NA will follow different trajectories after the occurrence of the behaviors.
Method
Participants
Data were collected from 133 adult women who met Diagnostic and Statistical Manual of Mental Disorders (4th ed., text rev.; DSM–IV–TR; APA, 2000) criteria for BN. Participants were excluded from the study if they were under 18 years of age or men. Participants ranged in age from 18 to 55 years, with a mean age of 25.3 ± 7.6 years. Most participants were Caucasian (95.5%), currently employed (73.3%), and had never been married (63.9%). Lifetime rates of Axis I disorders were 87.0% for mood disorders, 59.5% for anxiety disorders, and 54.2% for substance dependence. All participants were at least 85% of ideal body weight (mean body mass index [BMI] = 23.9 ± 5.2). Detailed descriptions of participants’ demographic data, symptom severity, and rates of co-occurring psychopathology have been previously reported (Crosby et al., 2009; Smyth et al., 2007).
Measures
Structured Clinical Interview for DSM–IV Axis I Disorders, Patient Edition (SCID–I/P)
The SCID–I/P (First, Spitzer, Gibbon, & Williams, 1995) is a semistructured interview that measures Axis I psychopathology. The SCID–I/P was administered by a trained doctoral-level psychologist and was used to establish lifetime history of Axis I disorders. The Eating Disorder module of the SCID–I/P was used to determine whether participants met current DSM–IV criteria for BN. All interviews were audiotaped, and interrater reliability was calculated on 25 cases from the sample. The kappa coefficient for current DSM–IV BN diagnosis was 1.0.
Positive and Negative Affect States (PANAS)
The PANAS (Watson, Clark, & Tellegen, 1988) measures two general dimensions of affect (i.e., positive and negative) as well as facets of affect (e.g., fear, joviality). Eleven items from the PANAS were chosen to assess momentary NA: afraid, lonely, irritable, ashamed, angry, disgusted, nervous, dissatisfied with self, jittery, sad, and angry with self. Participants were asked to rate the extent to which they currently felt these emotions on a 5-point Likert scale, ranging from 1 (not at all) to 5 (extremely). The internal consistency of this abbreviated NA scale (α = .92) was consistent with the internal consistency of the full NA scale when assessed at the momentary level (range of αs = .85–.91; Watson & Clark, 1994).
Eating Disorder Checklist
Participants were asked to indicate whenever they engaged in BE, self-induced vomiting, laxative misuse, or diuretic misuse. These behaviors could be recorded either immediately after they occurred or during the next signaled recording. Participants were not asked to provide EMA assessment ratings during behaviors. Participants were provided with standard definitions of BE (“an amount of food that you consider excessive, or an amount of food that other people would consider excessive, with an associated loss of control or the feeling of being compelled to eat”) as well as examples of what constituted objectively large amounts of food. In the current analyses, self-induced vomiting, laxative misuse, and diuretic misuse were combined to form a single variable representing purging.
Procedure
This study was approved by the Institutional Review Boards of the University of North Dakota and MeritCare Hospital (Fargo, ND). Participants were recruited through clinical, community, and campus advertisements. Interested participants were initially screened over the phone for inclusion and exclusion criteria. Eligible participants were scheduled for an informational meeting during which they received information about the study and provided written informed consent. Participants completed two assessment visits (approximately 3– 4 hr total) during which they completed a larger battery of assessments including semistructured interviews, self-report questionnaires, and an electrolyte screening to ensure medical stability. Only those measures used for the current study have been described above; please refer to Smyth et al. (2007) for the full battery of assessments.
After baseline assessments, eligible participants were given palm-top computers to complete EMA assessments over the course of the next 2 weeks. The EMA assessment protocol implemented three types of daily self-report methods: (1) signal-contingent recording, (2) interval-contingent recording, and (3) event-contingent recording. With regard to the signal-contingent recording, participants were signaled by the palm-top computer to complete EMA assessment ratings at six semi-random times throughout the day. These signals occurred semirandomly, but were all within ±20 min of each of six “anchor” times distributed evenly throughout the day: 8:30 a.m., 11:10 a.m., 1:50 p.m., 4:30 p.m., 7:10 p.m., and 9:50 p.m. With regard to interval-contingent recording, participants were instructed to complete EMA assessment ratings at the end of each day. Finally, with regard to event-contingent recording, participants were instructed to provide EMA assessment ratings immediately following the occurrence of predetermined behaviors (e.g., BE). During each recording, participants completed the PANAS and Eating Disorder Checklist. Participants received $200 for completing the 2-week assessment period and were given a $50 bonus for completing at least 85% of assessments within 45 min of the palm-top signal. For additional detail regarding the procedure, please refer to Smyth et al. (2007).
Statistical Methods
Confirmatory factor analysis
A two-level confirmatory factor analysis with random intercept was performed with EMA data to evaluate the factor structure of the PANAS negative scale. Model fit was evaluated using the confirmatory fit index (CFI), the Tucker–Lewis index (TLI), the root-mean-square error of approximation (RMSEA), and the standard root-mean-square residual (SRMR). Analyses were performed using Mplus version 6.11 (Muthén & Muthén, 1998 –2004). To examine whether the model varied over the 2-week period, we included time as a covariate.
Within-day analyses
To examine the temporal relationship between facets of NA and bulimic behaviors, we modeled the pre- and postevent trajectories of each facet of NA separately using piecewise linear, quadratic, and cubic functions centered on the time at which each of the following behaviors occurred: BE unaccompanied by purging (binge only), purging unaccompanied by BE (purge only), and BE and purging that occurred in combination (binge/purge). Multilevel models included linear functions (i.e., hours prior to event, hours following event), which reflected the rate of change in affect prior to and following bulimic behaviors; quadratic functions (i.e., [hours prior to event]2, [hours following event]2), which reflected the acceleration in rate of affect change prior to and following bulimic behaviors; and cubic functions (i.e., [hours prior to event]3, [hours following event]3), which reflected either further acceleration or dampening of the acceleration in rate of affect change. When more than one behavior was reported in a single day, only the first behavior was used to avoid confounding the relationship between antecedent and consequent mood ratings in relation to the multiple bulimic behaviors that occurred throughout any one day. Additionally, if subsequent behaviors occurred within the 4-hr time frame following the first behavior, only affect ratings made after the first behavior and prior to the subsequent behavior were included in the postevent analyses.
Results
Participants’ compliance with completing signal-contingent ratings was good (average = 86%; median = 90%). Participants’ timeliness was also good; the majority of signal-contingent ratings were made within 5 min, and 75% were made within 20 min. Analyses were based on observations of 1088 binge-only, 2117 purge-only, and 2727 binge/purge events.
Confirmatory Factor Analysis
The CFA indicated that the best-fitting model was a four-factor solution (RMSEA = .029; CFI = .943; TLI = .917; SRMR within = .033; SRMR between = .053) that replicated the results of the original factor analysis (Watson & Clark, 1994), with one exception. The current CFA indicated that the Disgust item loaded onto the Guilt factor, whereas the original factor analysis found that Disgust loaded most highly onto the Hostility factor (see Table 2). However, it should be noted that in the original factor analysis, Disgust loaded onto both the Guilt and Hostility factors. The Cronbach’s alphas of the four abbreviated lower-order NA subscales were .80 (Fear), .89 (Guilt), .79 (Hostility), and .81 (Sadness), demonstrating good internal consistency. Model estimates from the CFA demonstrated significant, moderate associations among the four factors (see Table 3), which was expected, given that they represent subfactors of a global NA scale. Finally, Factor × Time interactions were not significant, indicating that the model structure did not vary over the 2-week assessment period.
Table 2.
Within-Level Model Results for Two-Level Confirmatory Factor Analysis
| Factor/descriptor | Est. | SE | Two-tailed p value |
|---|---|---|---|
| Fear | |||
| Afraid | 1.00 | 0.00 | 999.00 |
| Nervous | 1.25 | 0.08 | <.001 |
| Jittery | 0.99 | 0.08 | <.001 |
| Guilt | |||
| Ashamed | 1.00 | 0.00 | 999.00 |
| Angry at self | 1.15 | 0.04 | <.001 |
| Dissatisfied with self | 0.82 | 0.05 | <.001 |
| Disgust | 1.06 | 0.04 | <.001 |
| Hostility | |||
| Angry | 1.00 | 0.00 | 999.00 |
| Irritable | 0.91 | 0.04 | <.001 |
| Sadness | |||
| Sad | 1.00 | 0.00 | 999.00 |
| Lonely | 0.75 | 0.03 | <.001 |
Note. Est. = estimate; SE = standard error.
Table 3.
Model Estimates of the Association Between Factors
| Factor | Est. | SE | Two-tailed p value |
|---|---|---|---|
| Fear with | |||
| Guilt | 0.23 | 0.03 | <.001 |
| Hostility | 0.22 | 0.03 | <.001 |
| Sadness | 0.23 | 0.03 | <.001 |
| Guilt with | |||
| Hostility | 0.36 | 0.03 | <.001 |
| Sadness | 0.42 | 0.03 | <.001 |
| Hostility with | |||
| Sadness | 0.35 | 0.03 | <.001 |
Note. Est. = estimate; SE = standard error.
Within-Day Analyses
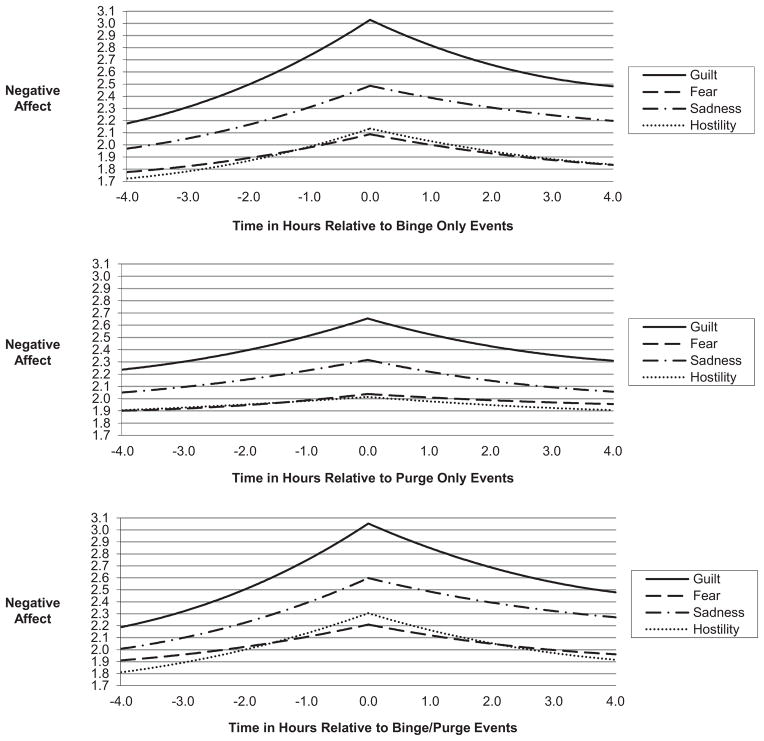
The results of the within-day analyses are provided in Table 4 and illustrated in Figure 1 using data estimated by the linear, quadratic, and cubic coefficients. The data indicate that there was a significant change in trajectory, reflecting the association between NA and time anchored on the time at which the behavior occurred, for all four facets of NA before and after binge-only and binge/purge events. In other words, all four facets of NA increased prior to and decreased following binge-only and binge/purge events (all ps < .001; see Table 4). The same results were found for purge-only events (all ps < .05; see Table 4), with the exception that Hostility did not increase significantly prior to purging. Of note, nonoverlapping confidence intervals suggest that for binge-only and binge/purge events, the magnitude of Guilt at the intercept point1 was higher than the magnitudes of Sadness, Fear, and Hostility (see Table 5). To further examine the unique effects of each facet of NA, we repeated the within-day analyses described above, this time examining each facet of NA individually while using the other three facets of NA as covariates. Despite significant associations among the four facets of NA, the post hoc analyses indicated that Guilt still increased prior to and decreased after all three types of behaviors, even after controlling for Fear, Hostility, and Sadness (all ps < .001). In contrast, the effects for Fear, Hostility, and Sadness washed out when controlling for the other facets of NA.
Table 4.
Within-Day Multilevel Models for Bulimic Behaviors
| Variable | Fear
|
Guilt
|
Hostility
|
Sadness
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Est. | SE | t | Est. | SE | t | Est. | SE | t | Est. | SE | t | |
| Binge-Only | ||||||||||||
| Intercept | 2.09 | .10 | −20.76*** | 3.03 | .10 | 29.32*** | 2.13 | .09 | 22.88*** | 2.49 | .11 | 22.84*** |
| Hours prior to event | 0.12 | .02 | 05.13*** | 0.32 | .03 | 11.43*** | 0.17 | .03 | 5.63*** | 0.20 | .03 | 6.59*** |
| (Hours prior to event)2 | 0.01 | .00 | 03.53*** | 0.03 | .00 | 7.50*** | 0.02 | .00 | 4.26*** | 0.02 | .00 | 4.17*** |
| (Hours prior to event)3 | 0.00 | .00 | 02.51* | 0.00 | .00 | 4.82*** | 0.00 | .00 | 3.00** | 0.00 | .00 | 2.59* |
| Hours following event | −0.22 | .05 | −4.82*** | −0.56 | .05 | −10.30*** | −0.28 | .06 | −4.97*** | −0.30 | .06 | −5.36*** |
| (Hours following event)2 | −0.00 | .01 | −0.55 | −0.00 | .01 | −0.69 | −0.01 | .01 | −0.99 | −0.01 | .01 | −1.07 |
| (Hours following event)3 | −0.00 | .00 | −1.88 | −0.00 | .00 | −4.76*** | −0.00 | .00 | −2.14* | −0.00 | .00 | −1.86 |
| Purge-Only | ||||||||||||
| Intercept | 2.04 | .08 | 23.65*** | 2.66 | .09 | 28.22*** | 2.01 | .08 | 24.46*** | 2.32 | .10 | 23.23*** |
| Hours prior to event | 0.06 | .02 | 03.41*** | 0.16 | .02 | 8.16*** | 0.04 | .02 | 1.76 | 0.10 | .02 | 4.71*** |
| (Hours prior to event)2 | 0.01 | .00 | 02.51* | 0.02 | .00 | 5.28*** | 0.00 | .00 | 0.65 | 0.01 | .00 | 2.67** |
| (Hours prior to event)3 | 0.00 | .00 | 02.16* | 0.00 | .00 | 3.28** | 0.00 | .00 | 0.13 | 0.00 | .00 | 1.12 |
| Hours following event | −0.09 | .03 | −2.93** | −0.31 | .04 | −8.69*** | −0.07 | .04 | −2.09* | −0.21 | .04 | −5.61*** |
| (Hours following event)2 | −0.00 | .00 | −0.98 | −0.00 | .00 | −0.06 | −0.00 | .00 | −0.26 | −0.01 | .00 | −1.18 |
| (Hours following event)3 | −0.00 | .00 | −1.83 | −0.00 | .00 | −4.61*** | −0.00 | .00 | −0.48 | −0.00 | .00 | −2.86** |
| Binge/Purge | ||||||||||||
| Intercept | 2.21 | .09 | 25.50*** | 3.05 | .09 | 33.03*** | 2.31 | .08 | 30.01*** | 2.60 | .09 | 27.43*** |
| Hours prior to event | 0.11 | .01 | 7.73*** | 0.34 | .02 | 18.24*** | 0.18 | .02 | 9.89*** | 0.23 | .02 | 11.58*** |
| (Hours prior to event)2 | 0.01 | .00 | 4.93*** | 0.03 | .00 | 12.08*** | 0.02 | .00 | 6.02*** | 0.02 | .00 | 7.50*** |
| (Hours prior to event)3 | 0.00 | .00 | 3.25** | 0.00 | .00 | 8.25*** | 0.00 | .00 | 3.48** | 0.00 | .00 | 5.06*** |
| Hours following event | −0.21 | .03 | −8.27*** | −0.57 | .03 | −17.25*** | −0.34 | .03 | −10.44*** | −0.35 | .03 | −10.18*** |
| (Hours following event)2 | −0.00 | .00 | −0.22 | −0.01 | .00 | −3.53*** | −0.00 | .00 | −0.05 | −0.01 | .00 | −2.58* |
| (Hours following event)3 | −0.00 | .00 | −3.79*** | −0.00 | .00 | −7.87*** | −0.00 | .00 | −4.94*** | −0.00 | .00 | −4.69*** |
Note. Est. = estimate; SE = standard error.
p < .05.
p < .01.
p < .001.
Figure 1.
Level of lower-order negative affect subscales over time in relation to binge-only, purge-only, and binge/purge events.
Table 5.
Magnitudes of Fear, Guilt, Hostility, and Sadness at the Intercept Point
| Behavior | Intercept | 95% CI |
|---|---|---|
| Binge only | ||
| Fear | 2.09 | 1.89, 2.29 |
| Guilt | 3.03 | 2.83, 3.24 |
| Hostility | 2.13 | 1.95, 2.32 |
| Sadness | 2.49 | 2.27, 2.70 |
| Purge only | ||
| Fear | 2.04 | 1.87, 2.21 |
| Guilt | 2.66 | 2.47, 2.84 |
| Hostility | 2.01 | 1.85, 2.18 |
| Sadness | 2.32 | 2.19, 2.52 |
| Binge/purge | ||
| Fear | 2.21 | 2.04, 2.38 |
| Guilt | 3.05 | 2.87, 3.23 |
| Hostility | 2.31 | 2.15, 2.46 |
| Sadness | 2.60 | 2.41, 2.79 |
Note. CI = confidence interval.
Discussion
The objective of this study was to examine whether facets of NA are differentially related to bulimic behaviors. Overall, there was a relatively consistent temporal relationship between the four facets of NA and bulimic behaviors, with the facets of NA increasing prior to and decreasing following all three types of bulimic behaviors. These data provide additional support for the affect regulation model of BN and indicate that both BE and purging function to mitigate individual facets of NA, regardless of whether the behaviors occur alone or in combination. Although there was a significant decrease in Hostility after purge-only events, there was no significant change in the trajectory of Hostility prior to purge-only events. These data may suggest that although purging may be reinforced by reductions in hostility, fluctuations in hostility do not necessarily precipitate episodes of purging. Of particular interest are the findings that Guilt was higher than the other facets of NA and that Guilt was the only facet of NA that retained significant linear effects before and after bulimic behaviors when controlling for the other facets of NA. These data provide preliminary evidence that guilt may be particularly important to the pathology of BN and the maintenance of bulimic behaviors. For example, one explanation for these findings may be that the primary function of bulimic behaviors is to regulate guilt specifically, and any observed decreases in the other facets of NA following bulimic behaviors may be unintended consequences of those behaviors.
Also of interest is the finding that guilt decreased significantly after binge-only events, which seems counterintuitive given that historically, BE has been thought to be associated with feelings of guilt, self-deprecation, and disgust (American Psychiatric Association [APA], 2012; Polivy & Herman, 1993). However, inherent in this notion is that the feelings of guilt are specifically related to the binge itself and/or potential implications of the binge on shape/weight. It is notable that the item content of the Guilt subscale is relatively vague (e.g., dissatisfied with self), which means that the context for the feelings of guilt cannot be identified with these data. It is possible that the feelings of guilt reported by participants in this study were not related to eating events or shape and weight, but were related to interpersonal events or general self-concept instead. Determining the context of the guilt (e.g., guilt related to interpersonal events, body image, dietary rules, self-concept) could help delineate the role of guilt in maintaining bulimic symptoms and may be particularly important for treatment providers as it could implicate a specific target for treatment.
This study had several strengths. First, it is the first EMA study to examine the relationship between facets of NA and bulimic behaviors with time-stamped assessments, which improve both the reliability and validity of the data. Second, modeling the relationship between NA and bulimic behaviors using all data points provides a more comprehensive illustration of the relationship between NA and bulimic behaviors than does comparing two data points. Third, binge-only, purge-only, and binge/purge behaviors were examined separately, providing the opportunity to examine the relationship between affect and each type of behavior. Finally, participants were not seeking treatment, and the sample size was substantially larger than those of previous investigations, both of which increase the generalizability of the findings.
Several limitations of the current study should be noted. Importantly, the four lower-order subscales of the PANAS were created using a subset of the original items. However, the factor structure and internal consistencies of the four subscales used in the current study were consistent with the full subscales. Second, although BE was defined for all participants, all eating episodes were self-rated as either binge or nonbinge episodes by the participants. Given that research suggests that lay definitions of BE are characterized primarily by the presence of loss of control irrespective of the quantity of food consumed (Beglin & Fairburn, 1992), it is possible that the current data are more suggestive of the relationship between NA and loss of control eating (in which the amount of food consumed may or may not have been large by clinical assessment). Third, although these data illustrate the relationship between facets of NA and individual bulimic behaviors over an 8-hr period, it is possible that the temporal relationship between NA and bulimic behaviors may differ over longer periods of time (e.g., days, weeks) or when multiple bulimic behavior events occur during the same day. Fourth, only adult women were included in the current study; therefore, it is unclear whether these results generalize to men or adolescents. Finally, these data are descriptive and do not necessarily provide explanations for the observed findings. In summary, these data provide additional support for the affect regulation model and suggest that guilt may be particularly important to the pathology of BN. Additional research (e.g., to identify the context of guilt, to examine the relationship between affect and behavior over longer periods of time or when sequential bulimic behaviors occur) is needed to further understand how facets of NA contribute to the pathology of BN.
Acknowledgments
This research was supported by Grants R01 MH59674 and T32 MH082761-01 from the National Institute of Mental Health.
Footnotes
The intercept point represents the time at which the behavior occurred.
Contributor Information
Kelly C. Berg, Department of Psychiatry, University of Minnesota
Ross D. Crosby, Neuropsychiatric Research Institute, Department of Clinical Neuroscience, University of North Dakota School of Medicine and Health Sciences
Li Cao, Neuropsychiatric Research Institute, Department of Clinical Neuroscience, University of North Dakota School of Medicine and Health Sciences.
Carol B. Peterson, Department of Psychiatry, University of Minnesota
Scott G. Engel, Neuropsychiatric Research Institute, Department of Clinical Neuroscience, University of North Dakota School of Medicine and Health Sciences
James E. Mitchell, Neuropsychiatric Research Institute, Department of Clinical Neuroscience, University of North Dakota School of Medicine and Health Sciences
Stephen A. Wonderlich, Neuropsychiatric Research Institute, Department of Clinical Neuroscience, University of North Dakota School of Medicine and Health Sciences
References
- Agras WS, Crow SJ, Halmi KA, Mitchell JE, Wilson GT, Kraemer HD. Outcome predictors for the cognitive behavior treatment of bulimia nervosa: Data from a multisite study. American Journal of Psychiatry. 2000;157:1302–1308. doi: 10.1176/appi.ajp.157.8.1302. [DOI] [PubMed] [Google Scholar]
- Agras WS, Walsh BT, Fairburn CG, Wilson GT, Kraemer HC. A multicenter comparison of cognitive–behavioral therapy and interpersonal psychotherapy for bulimia nervosa. Archives of General Psychiatry. 2000;57:459–466. doi: 10.1001/archpsyc.57.5.459. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association [APA] DSM–IV–TR. 4. Washington, DC: Author; 2000. Diagnostic and statistical manual of mental disorders. text rev.; [Google Scholar]
- American Psychiatric Association [APA] DSM–5 development. 2012 Retrieved from www.dsm5.org.
- Beglin SJ, Fairburn CG. What is meant by the term “binge”? American Journal of Psychiatry. 1992;149:123–124. doi: 10.1176/ajp.149.1.123. [DOI] [PubMed] [Google Scholar]
- Corstorphine E, Waller G, Ohanian V, Baker M. Changes in internal states across the binge–vomit cycle in bulimia nervosa. Journal of Nervous and Mental Disease. 2006;194:446–449. doi: 10.1097/01.nmd.0000221303.64098.23. [DOI] [PubMed] [Google Scholar]
- Crosby RD, Wonderlich SA, Engel SG, Simmonich H, Smyth J, Mitchell JE. Daily mood patterns and bulimic behaviors in the natural environment. Behavior Research and Therapy. 2009;47:181–188. doi: 10.1016/j.brat.2008.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crow SJ, Peterson CB, Swanson SA, Raymond NC, Specker S, Eckert ED, Mitchell JE. Increased mortality in bulimia nervosa and other eating disorders. American Journal of Psychiatry. 2009;166:1342–1346. doi: 10.1176/appi.ajp.2009.09020247. [DOI] [PubMed] [Google Scholar]
- Elmore DK, de Castro JM. Self-rated moods and hunger in relation to spontaneous eating behavior in bulimics, recovered bulimics, and normals. International Journal of Eating Disorders. 1990;9:179–190. doi: 10.1002/1098-108X(199003)9:2<179::AID-EAT2260090207>3.0.CO;2-O. [DOI] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured clinical interview for the DSM–IV axis I disorders—patient edition (SCID–I/P, version 2) New York, NY: New York State Psychiatric Institute, Biometrics Research Department; 1995. [Google Scholar]
- Haedt-Matt AA, Keel PK. Revisiting the affect regulation model of binge eating: A meta-analysis of studies using ecological momentary assessment. Psychological Bulletin. 2011;137:660–681. doi: 10.1037/a0023660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hetherington MM, Altemus M, Nelson ML, Bernat AS, Gold PW. Eating behavior in bulimia nervosa: Multiple meal analyses. American Journal of Clinical Nutrition. 1994;60:864–873. doi: 10.1093/ajcn/60.6.864. [DOI] [PubMed] [Google Scholar]
- Hoek HW. Incidence, prevalence, and mortality of anorexia and other eating disorders. Current Opinion in Psychiatry. 2006;19:389–394. doi: 10.1097/01.yco.0000228759.95237.78. [DOI] [PubMed] [Google Scholar]
- Johnson C, Larson R. Bulimia: An analysis of moods and behavior. Psychosomatic Medicine. 1982;44:341. doi: 10.1097/00006842-198209000-00003. [DOI] [PubMed] [Google Scholar]
- Kaye WH, Gwirtsman HE, George DT, Weiss SR, Jimerson DC. Relationship of mood alterations to bingeing behaviour in bulimia. British Journal of Psychiatry. 1986;149:479–485. doi: 10.1192/bjp.149.4.479. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus (version 6.1) [Computer software] Los Angeles, CA: Muthén & Muthén; 1998–2004. [Google Scholar]
- Polivy J, Herman CP. Etiology of binge eating: Psychological mechanisms. In: Fairburn CG, Wilson GT, editors. Binge eating: Nature, assessment, and treatment. New York, NY: Guilford Press; 1993. pp. 173–205. [Google Scholar]
- Powell AL, Thelen MH. Emotions and cognitions associated with bingeing and weight control behavior in bulimia. Journal of Psychosomatic Research. 1996;40:317–328. doi: 10.1016/0022-3999(95)00641-9. [DOI] [PubMed] [Google Scholar]
- Smyth JM, Wonderlich SA, Heron KE, Sliwinski MJ, Crosby RD, Mitchell JE, Engel SG. Daily and momentary mood and stress are associated with binge eating and vomiting in bulimia nervosa patients in the natural environment. Journal of Consulting and Clinical Psychology. 2007;75:629–638. doi: 10.1037/0022-006X.75.4.629. [DOI] [PubMed] [Google Scholar]
- Stone AA, Shiffman S. Ecological momentary assessment (EMA) in behavioral medicine. Annals of Behavioral Medicine. 1994;16:199–202. [Google Scholar]
- Stone AA, Shiffman S, Schwartz JE, Broderick JE, Huffor MR. Patient compliance with electronic and paper diaries. Controlled Clinical Trials. 2003;24:182–199. doi: 10.1016/S0197-2456(02)00320-3. [DOI] [PubMed] [Google Scholar]
- Teasdale JD, Fogarty SJ. Differential effects of induced mood on retrieval of pleasant and unpleasant events from episodic memory. Journal of Abnormal Psychology. 1979;88:248–257. doi: 10.1037/0021-843X.88.3.248. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA. The PANAS–X: Manual for the positive and negative affect schedule—expanded form. Iowa City, IA: University of Iowa; 1994. [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037/0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]