Abstract
Ancillary to decline in cognitive abilities, patients with Alzheimer’s disease (AD) frequently suffer from behavioural and psychological symptoms of dementia (BPSD). Hypothalamic polypeptides such as melanin-concentrating hormone (MCH) and hypocretin-1 (HCRT-1, orexin-A) are promoters of sleep-wake regulation and energy homeostasis and are found to impact on cognitive performance. To investigate the role of MCH and HCRT-1 in AD, cerebrospinal fluid (CSF) levels were measured in 33 patients with AD and 33 healthy subjects (HS) using a fluorescence immunoassay (FIA). A significant main effect of diagnosis (F(1,62) = 8.490, p<0.01) on MCH levels was found between AD (93.76±13.47 pg/mL) and HS (84.65±11.40 pg/mL). MCH correlated with T-tau (r = 0.47; p<0.01) and P-tau (r = 0.404; p<0.05) in the AD but not in the HS. CSF-MCH correlated negatively with MMSE scores in the AD (r = −0.362, p<0.05) and was increased in more severely affected patients (MMSE≤20) compared to HS (p<0.001) and BPSD-positive patients compared to HS (p<0.05). In CSF-HCRT-1, a significant main effect of sex (F(1,31) = 4.400, p<0.05) with elevated levels in females (90.93±17.37 pg/mL vs. 82.73±15.39 pg/mL) was found whereas diagnosis and the sex*diagnosis interaction were not significant. Elevated levels of MCH in patients suffering from AD and correlation with Tau and severity of cognitive impairment point towards an impact of MCH in AD. Gender differences of CSF-HCRT-1 controversially portend a previously reported gender dependence of HCRT-1-regulation. Histochemical and actigraphic explorations are warranted to further elucidate alterations of hypothalamic transmitter regulation in AD.
Introduction
In Alzheimer’s disease (AD) which is predominately characterized by the decline of cognitive abilities in memory, abstraction, orientation and language, cognition-related behavioral and psychological symptoms of dementia (BPSD) frequently occur. These include sleep-wake disturbances with daytime sleepiness and napping, nightly awakening, reduced REM-sleep and increased REM-onset latency, cyclic agitation and deregulation of appetite and weight [1], [2].
The complementary acting transmitters melanin-concentrating hormone (MCH) and hypocretin-1 (HCRT-1; syn. orexin-A) are synthesized in the hypothalamus, a subcortical region where senile plaques and neurofibrillary tangles as ‘hallmarks of dementia’ are to be found [3], [4], [5]. Experimental studies demonstrate that receptors for both peptides are found in areas not only involved in the regulation of wakefulness, circadian rhythmicity and energy homeostasis but also regarded affected in AD, such as the cerebral cortex, cholinergic neurons of the basal forebrain, amygdala, and the brainstem [6], [7], [8], [9], [10], [11]. Animal studies have shown that the activation of MCH neurons leads to improved learning and memory performance (for references see [8]), increased REM sleep [12], [13] increased food and water intake [14] and has anxiogenic effects in mice [15]. Reduction of MCH or blockage of MCH-receptors leads to improved social recognition in rats [16], hyperactivity, leanness, hypermetabolism in mice [17], and has antidepressant effects in animals (for references see [18]).
The infusion of HCRT-1 improves accuracy in demanding attentional tasks in rats [19] and the excitement of neurons of the basal forebrain [20]. In HCRT-deficient narcoleptic patients, the dysregulation of sleep-wake control is featured by worsening in cognitive attentive processing as well as performance in information gathering and memory tasks [21], [22], [23], [24].
While to date no data on MCH levels in AD exist, literature concerning HCRT-1 is heterogenous: whereas immunoreactive neurons in postmortem hypothalami and ventricular cerebrospinal fluid (CSF)-HCRT-1 levels in AD patients were found to be reduced [25], lumbar CSF levels in vivo were unaltered [26], [27], [28]. A regulation of amyloid-beta (Aβ42) by HCRT has been concluded since the infusion of HCRT-1 in animals lead to increased levels of Aβ42 in the brain interstitial fluid. In contrast the infusion of an HCRT-1-antagonist led to a reduction in Aβ42-plaque deposition as shown with microdialysis in mice [29]. Only in AD but not healthy subjects (HS), daily amplitudes of HCRT-1 and Aβ42 correlated [30] whereas levels were not found to correlate in neither AD nor HS [26]. Furthermore in AD, CSF-HCRT-1 levels negatively correlated with the number of daily naps and the total amount of daily nap time [31]. A reduction of HCRT-1-containing neurons [32] and HCRT-1-mediated efflux of acetylcholine in the medial septum [33] with age has been furthermore demonstrated in rats.
The aim of this study was to investigate the CSF levels of MCH and HCRT-1 in patients with AD and HS and the potentially causal relationship between these polypeptides and CSF levels of the AD marker total Tau (T-tau), hyperphosphorylated tau (P-tau) and Aβ42, cognitive performance and behavioral symptoms in AD.
Methods
Subjects
This study was approved by Leipzig University and Saxony Medical Ethics Committee. Patients or, when appointed, proxy provided written informed consent to the appropriation in this clinical study.
33 patients with mild to severe AD and 33 subjects without any psychiatric or neurological disorder (HS) were consecutively recruited to participate in the study. Characteristics of patients and HS such as age, gender, psychotropic medication as well as performances in cognitive tests are depicted in tables 1 and 2. All patients and HS were admitted to the Department of Psychiatry of the University Hospital Leipzig as inpatients. Patients or HS showing any indication of limitation to provide full consent and lacking a proxy were excluded from the study. Patients with AD were admitted in order to clinically explore and diagnose cognitive deficits registered in ambulatory setting. Patients were diagnosed with AD under supervision of a senior specialist in geriatric psychiatry according to Dubois criteria [34]. Diagnostics included history, clinical investigation, neuropsychological testing with the neuropsychological test battery of the Consortium to Establish a Registry for Alzheimer’s Disease (CERAD; [35]), Wechsler Memory Scale-Revision (WMS-R; [36]), clock drawing test [37], and Trail Making Test (TMT; [38]), a MRI head-scan, genotyping of ApoE4 and determination of Aβ42, T-tau and P-tau in the CSF. Patients were only included when no further neurological disturbances were diagnosed by clinical and laboratory investigations. BPSD was categorized into sleep disorder and irritability. Sleep disorder contained sleep onset latency of more than two hours or fragmented sleep with 1 or more periods of awakening for more than half an hour during the in the night before investigation. Irritability included verbal aggression, including curse and abusive formal language recorded by physicians or nursing staff.
Table 1. Subject characteristics.
| AD | HS | |
| N | 33 | 33 |
| Male/female | 11/22 | 19/14 |
| Age in years (±SD) | 73.76 (±8.07) | 52.03 (±17.24)*** |
| MMSE (±SD) | 19.76 (±6.54) | 29.92 (±0.29)*** |
| BMI (±SD) | 24.97 (±4.61) | 27.44 (±5.15) |
| CSF-t-Tau in pg/ml (±SD) | 449.5 (±245.0) | 133.8 (±48.5)*** |
| CSF-pTau in pg/ml (±SD) | 79.2 (±38.8) | 32.6 (±12.0)*** |
| CSF-Amyloid-β-1-42 in pg/ml (±SD) | 633.8 (±290.2) | 1157.3 (±260.6)*** |
| Psychotropic medication n/y | 22/11 | 33/0 |
| Galantamine | 3 | ― |
| Rivastigmine | 4 | ― |
| Memantine | 3 | ― |
| Venlafaxine | 2 | ― |
| Citalopram | 1 | ― |
| Risperidone | 1 | ― |
p<0.001, N = Number, AD = Alzheimer’s Disease, HS = Healthy subjects, N = Number, SD = Standard Deviation, BMI = Body Mass Index.
Table 2. Clinical characteristics of patients with AD.
| Total AD | Male AD | Female AD | |
| N | 33 | 11 | 22 |
| Age (±SD) | 73.76 (±8.07) | 73.36 (±7.02) | 73.95 (±8.71) |
| BMI (±SD) | 24.97 (±4.61) | 24.78 (±5.14) | 24.05 (±4.47) |
| MWT-A (±SD) | 24.46 (±9.25) | 29.38 (±4.47) | 22.28 (±10.06) |
| Education in years (±SD) | 9.20 (±1.54) | 10.1 (±1.79) | 8.75 (±1.21)* |
| MMSE (±SD) | 19.76 (±6.54) | 19.82 (±5.86) | 19.73 (±6.99) |
| TMT-A (±SD) | 123.83 (±74.53) | 107.00 (±82.07) | 125.09 (±75.57) |
| TMT-B (±SD) | 251.96 (±89.71) | 234.13 (±153.41) | 206.42 (±111.63) |
| Clock drawing test (±SD) | 3.61 (±1.65) | 3.44 (±1.94) | 3.68 (±1.55) |
| WMS-Logical Memory-I (±SD) | 6.03 (±5.38) | 8.44 (±6.75) | 5.05 (±4.52) |
| WMS-Logical Memory-D (±SD) | 2.87 (±4.81) | 3.89 (±5.62) | 2.45 (±4.51) |
| Verbal fluency (±SD) | 9.81 (±4.88) | 9.89 (±5.25) | 9.77 (±4.84) |
| MBNT (±SD) | 10.87 (±3.49) | 13.44 (±1.42) | 9.82 (±3.56)** |
| Wordlist learning (±SD) | 9.83 (±5.09) | 10.89 (±4.70) | 9.38 (±5.29) |
| Wordlist recall (±SD) | 4.20 (±13.47) | 2.11 (±1.83) | 5.10 (±16.09) |
| Constructional praxis learning (±SD) | 8.32 (±2.51) | 9.11 (±1.97) | 8.00 (±2.67) |
| Constructional praxis recall (±SD) | 1.71 (±2.037) | 2.89 (±2.21) | 1.23 (±1.79) |
| Apo E4 carriers in % | 65.4 | 77.8 | 58.8 |
p<0.05,
p<0.01, N: Number, SD: Standard Deviation, BMI: Body Mass Index, MWT-A: Mehrfachwahl-Wortschatz-Test A, MMSE: Mini Mental State Examination, TMT: Trail Making Test, Scale Logical Memory- Delayed recall trial, MBNT: Modified Boston, Naming Test, WMS-Logical Memory- I: Wechsler Memory Scale-Logical Memory-Immediate recall trial, WMS-Logical Memory- D: Wechsler Memory Scale-Logical Memory- Delayed recall trial.
HS were recruited from the Clinic of Anesthesiology and Intensive Care Medicine, University Hospital Leipzig and Helios Hospital Borna, prior to elective abdominal or orthopedic surgery. HS showing any signs of neurological or psychiatric disorder in clinical and laboratory investigation or with the medication of psychoactive drugs within the last 30 days were excluded from the study. In order to further survey exclusion criteria, the Structured Clinical Interview Axis I Disorder (SCID; [39]), the Hamilton Depression Rating Scale (HAMD-17; [40]) and the Mini Mental Status Examination (MMSE; [41]) were performed when applicable.
Processing of Neuropeptides
In order to minimize known diurnal variation as a confounding factor which is found for HCRT-1 and assumed for MCH [30], [42], lumbar puncture was performed in a time slot between 00:30 pm and 01:30 pm. Following, samples were immediately aliquoted in non-absorbing polypropylen-tubes of 300 µl. Probes were shock-frozen in fluid N2 and stored in freezers at −80°C until further measurements. For the measurement of MCH we used a fluorescence immunoassay (FIA) with a linear measuring range between 35.0 and 808 pg/mL (Phoenix Pharmaceuticals, Burlingame, US). For the measurement of HCRT-1 we used a fluorescence immunoassay (FIA) with a linear measuring range between 15.2 and 366 pg/mL (Phoenix Pharmaceuticals, Burlingame, US).
Statistical Analysis
The IBM Statistical Package for the Social Sciences (SPSS) program version 20.0 for Windows was used for all statistical analyses. The significance level was set at p<0.05 for all statistical analyses. Univariate ANOVA with post-hoc Bonferroni testing for multiple comparisons was performed for analysis of MCH and HCRT-1 between AD and HS, between sexes, between medicated and unmedicated patients and HS, for patients showing any of the BPSD stated above (BPSD+) and showing no BPSD (BPSD−), in patients with mild severities of AD (MMSE≥21) and moderate to severe severities (MMSE≤20), [43], as well as for detection of interactions between groups and gender. T-test was performed for differences of MCH and HCRT-1 in ApoE4 carriers vs non-carriers, as well as mean differences in scores in cognitive tests and educational level between male and female AD. For bivariate correlation of HCRT-1 and MCH levels and cognitive testing, Pearson’s correlation was performed; for BMI and age, two- tailed analyses of coefficient was performed using Spearman Rho. To assess the accuracy rates of MCH, receiver operating characteristic (ROC) analyses resulting in area under the curve values (AUC) was performed. Sensitivity and specificity was computed for different cut-off scores. The Youden index was used to select optimal cut-off scores.
Results
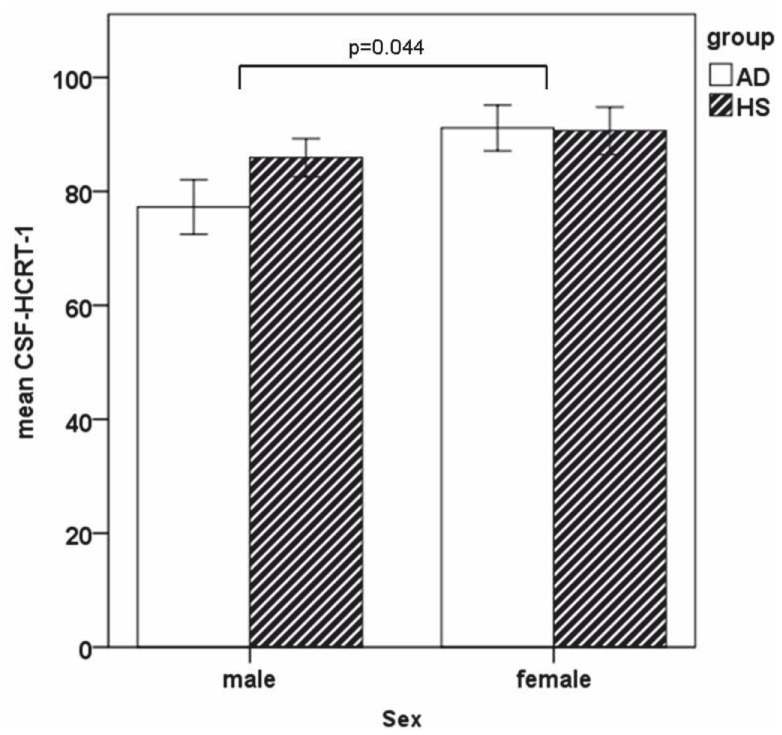
The distributions of CSF-MCH and CSF-HCRT-1 within the groups are depicted in table 3. Regarding MCH, the inferential statistical analyses showed a main effect of diagnosis (F(1,62) = 8.490, p<0.01) (see figure 1), whereas age (F(38,66) = 1.338, p = 0.237), sex (F(1,62) = 0.424, p = 0.517) and diagnosis*age interaction (F(4,66) = 0.957, p = 0.450) and diagnosis*sex interaction (F(1,62) = 1,175, p = 0.283) were not significant. MCH correlated with T-tau (r = 0.47, p<0.01) and P-tau (r = 0.404, p<0.05) in the AD but not in the HS. MCH and Aβ42 were found to weakly correlate in the total group (r = −0.264, p<0.05) but not in separate groups. CSF-MCH levels showed a negative correlation with MMSE scores in AD (r = −0.362, p<0.05) but not in the HS. Of the further cognitive tests performed, negative correlation was found with scores in the TMT-B (r = −0.466; p<0.05). CSF-MCH levels differed between AD with MMSE≤20 (n = 15), AD with MMSE≥21 (n = 18) and HS, (F(2,62) = 6.997, p<0.01) with post-hoc analyses showing higher levels in AD with MMSE≤20 compared to HS (p<0.001). CSF-MCH differed between BPSD+ (n = 14), BPSD− (n = 19) and HS (F(2,63) = 4.623, p<0.05) with post-hoc analyses showing higher levels in BPSD+ compared to HS (p<0.05). CSF-MCH levels also differed between medicated AD (n = 11), drug-naïve AD (n = 22) and HS (F(2,63) = 4.664, p = 0.05), with post-hoc analyses showing higher levels in medicated AD compared to HS (p<0.05). For the differentiation between AD and HS, ROC analyses for controlled values resulted in AUC = 0.713. With a Youden index of 0.39, sensitivity was 67% and specificity 73% for a cut-off value of 90.15 pg/mL.
Table 3. Levels of CSF-MCH and -HCRT-1 in patients with AD and HS.
| CSF-MCH in pg/mL | CSF-HCRT-1 in pg/mL | |||
| AD | HS | AD | HS | |
| Mean (±SD) | 93.76 (±13.47) | 84.65 (±11.40)** | 86.50 (±18.82) | 87.91 (±14.95) |
| Female (±SD) | 94.22 (±14.55) | 81.46 (±12.07)** | 91.12 (±18.75) | 90.62 (±15.61) |
| Male (±SD) | 92.84 (±11.60) | 87.19 (±10.85)a | 77.26 (±15.94) | 85.91 (±14.53)* |
| AD MMSE≥21 (±SD) | 89.52 (±13.53) | 84.65 (±11.40)a | 84.21 (±19.69) | 87.91 (±14.95) |
| AD MMSE≤20 (±SD) | 98.84 (±11.90) | “ *** | 91.08 (±16.89) | “ |
| AD BPSD– (±SD) | 92.42 (±13.30) | “ | 88.00 (±20.37) | “ |
| AD BPSD+ (±SD) | 95.58 (±13.85) | “ * | 84.69 (±17.31) | “ |
| AD Med– (±SD) | 92.58 (±15.54) | “ | 86.96 (±21.43) | “ |
| AD Med+ (±SD) | 96.12 (±15.54) | 84.65 (±11.40)* | 85.88 (±15.34) | 87.91 (±14.95) |
p<0.05;
p<0.01;
p<0.001, AD = Alzheimer’s Disease, HS = Healthy subjects, N = Number, SD = Standard Deviation, AD Med−/+ = AD patients without/with psychotropic medication, MMSE≥21/≤20: Scores in the Mini Mental State Examination higher or equal 21 points or less or equal 20 points, BPSD+/−: presence or absence of behavioral and psychiatric symptoms of dementia.
Figure 1. Mean value of CSF-MCH was elevated in AD when compared to HS.
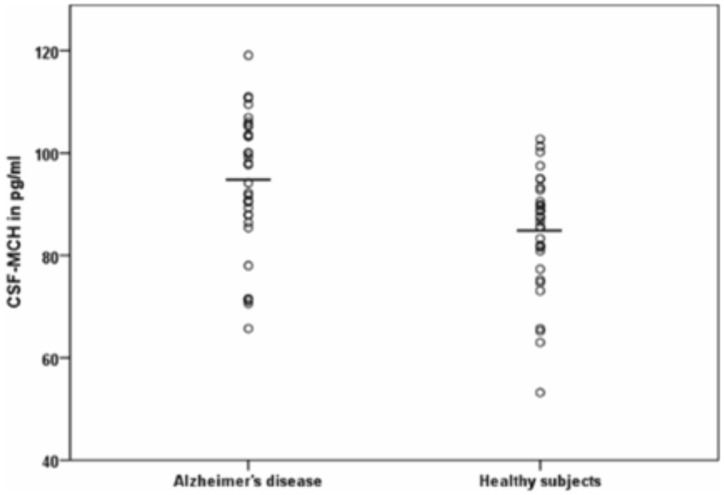
Regarding CSF-HCRT-1, the inferential statistical analyses showed a main effect of sex (F(1,62) = 4.863, p<0.05), whereas diagnosis (F(1,62) = 0.937, p = 0.337), age (F(38,66) = 1.408, p = 0.199), the sex*group (F1,62) = 1.179, p = 0.282) and age*group (F4,66) = 0.858, p = 0.504) interaction did not reach significance (see figure 2). CSF-HCRT-1 did not correlate with the MMSE in the two groups. Among the other cognitive tests performed, significance in the AD was reached with the TMT-A (−0.412, p<0.05). CSF-HCRT-1 did neither differ in means between groups of medicated AD, drug-naïve AD and HS nor between groups of BPSD+, BPSD− and HS. HCRT-1 did not correlate significantly with T-tau, P-Tau or Aβ42. CSF-MCH and CSF-HCRT-1 correlated within the AD group, r = 0.382, p<0.01, but not in the HS. Levels of CSF-MCH and CSF-HCRT-1 did not correlate with age, education levels in school years, MWT-A or BMI, and no differences in means of CSF-MCH or CSF-HCRT-1 depending on the ApoE4 genotype were found.
Figure 2. In HCRT-1, mean differences in gender were found as main effect with reduced levels in males.
Discussion
In the present study, we investigated CSF levels of the hypothalamic polypeptides MCH and HCRT-1 in 33 patients with AD and 33 HS. This, to the best of the authors’ knowledge, first investigation of MCH in AD revealed elevated means in the CSF when compared to HS. To differentiate AD from HS, a moderate sensitivity and specificity was reached with the respective optimal cut-off. Furthermore, levels of CSF-MCH were found to correlate with T-tau and P-tau only in the AD and to be severity- and BPSD-related. An association between CSF levels of MCH and HCRT-1 was found only in AD patients, whereas means of HCRT-1 were not found to differ significantly between AD and HS. Notably, CSF-HCRT-1 levels showed sex- dependence with elevations in females when compared to males.
A couple of findings suggest the regulation of MCH to be altered in AD. Correlations between MCH and Tau, but not for Aβ42, as established marker for the neuropathic formation of neurofibrillary tangles only in AD portend a connection between the parameter. The formation of neurofibrillary tangles in the hypothalamus in AD [5] with its expression of elevated levels of Tau may have impact on the activity of MCH-ergic neurons leading to a, potentially temporary, hypersecretion of MCH. MCH was further linked to severity of the disorder in general since only MMSE and TMT were found to correlate. In line with the regulatory function on sleep-wake regulation MCH was connected to the occurrence of BPSD. Although means of MCH did not show to differ by more than about 10 percent and although levels of MCH between AD and HS were found to overlap in a large proportion of participants which makes it rather useless as diagnostic or differential tool in AD, the finding of elevated means in a neurodegenerative disease is noteworthy. According to our findings and the impact of other chronobiological agents such as melatonin on neurodegenerative symptomatology [44], an explanatory approach may be driven here. Besides the neurodegenerative influence of the formation of neurofibrillary tangles, changes in levels of MCH may depict changes in the MCH-neuron regulation: MCH-receptor (MCH-R) sites are pronounced found in the hippocampus and cortex, vulnerable areas for degeneration in AD. Reduced stimulation or presence of MCH-R leads to a reduced negative feedback and increased high voltage-activated calcium channels in MCH neurons in the LH [45], leading consecutively to higher release of MCH. Supporting a modification of MCH-R in AD, MCH-R deficient mice showed worse cognitive performance and reduced N-methyl D-aspartate (NMDA) receptors in the hippocampus [46]. The positive effects of MCH on performance in learning and memory [47], the potentiation of hippocampal synaptic transmission by infusion of MCH [48] may be affected in AD due to reduced MCH-R availability. By primarily stabilizing REM-sleep phases [6], [12] an indirect effect of MCH on memory abilities has been shown [8]. Patients with AD lack the impact of (REM−) sleep on memory consolidating and synaptic plasticity [49], [50] which may contribute to cognitive impairment [51].
It may be considered if elevated CSF-MCH levels are caused by a temporal release of polypeptides subsequent to cellular apoptosis or necrosis in the LH. However, no short or long-time increase but only a reduction of transmitter levels are found [52] and no correlation between cell loss and CSF-levels could be found for HCRT-1 in AD [25].
In contrast to a previous report [25], we did not find differences in CSF-HCRT-1 between the two groups. Whereas patients in our study suffered from mild to severe AD, samples in the aforementioned were drawn from post-mortal brains. Gerashchenko and colleagues [52] demonstrated that the loss of a high proportion of HCRT-containing neurons leads to significant alterations of CSF-levels, possibly a state of degeneration patients in this study did not yet suffer from.
When performing subgroup analysis, our data showed increased CSF-HCRT-1 in females compared to males. This finding supports a previous report in which female AD patients showed increased levels in CSF-HCRT-1 compared to male AD patients, healthy females and females with DLB [26]. Thereupon, a determining influence of gender in the regulation of CSF-HCRT-1 was postulated. Findings indicating higher incidence of AD in females [53], worse cognitive performance in female mice in a transgene mice model of dementia [54], pronounced impairment of sleep in females [55], the modulation of HCRT-receptor-1 by gonadal steroids [56] and a sexually dimorphic expression of HCRT-1 [57] make further investigation of a gender dependence of HCRT-1 regulation in AD warranted. Contrary to the prior investigations stated in the introduction, we did neither find correlations between HCRT-1 and Tau nor Aβ42 and may therefore not support a link between established pathological cascades and HCRT-1.
When interpreting the results and the use of cut-off scores in clinical practice, several limitations have to be considered. A third of the patients with AD received psychotropic medication that may have had influence on MCH and HCRT-1 neuronal activity. Furthermore, groups differed in age and gender distributions. Though no impact of age and gender in the inferential statistics and no correlations between age and polypeptide levels were found in this nor previous reports [58], [25], these factors as well as the psychotropic medication cannot fully be ruled out to account for the group differences of MCH levels. Since biomarkers in AD have been demonstrated to show characteristic time course [59], further studies have to control for duration of illness. Concerning the objection of BPSD, data from medical records as used here are potentially not of enough accuracy and should be added by established rating scales assessing appetite sleep and behavioral qualities. Moreover, the binary differentiation between presence or absence of any BPSD and no further itemization is potentially of impreciseness.
This report on MCH in patients with AD adds to preclinical studies and may allow further research on the role of the hypothalamus in pathology and occurrence of behavioral disturbances in AD. Future investigations, including repeated MCH/HCRT-1 level measurements in combination with sleep-wake-actigraphy and assessment of sleep by questionnaires, histochemical determinations of MCH in animal and post-mortem tissues are warranted to understand the hypothalamic impact in AD in greater detail.
Funding Statement
These authors have no support or funding to report.
References
- 1. Fernández M, Gobartt AL, Balañá M (2010) Behavioural symptoms in patients with Alzheimer’s disease and their association with cognitive impairment. BMC Neurol 10: 87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. McCurry SM, Ancoli-Israel S (1985) Sleep Dysfunction in Alzheimer’s Disease and Other Dementias. Curr Treat Options Neurol 5: 261–272. [DOI] [PubMed] [Google Scholar]
- 3. McDuff T, Sumi SM (1985) Subcortical degeneration in Alzheimer’s disease. Neurology 35: 123–6. [DOI] [PubMed] [Google Scholar]
- 4. Ogomori K, Kitamoto T, Tateishi J, Sato Y, Suetsugu M (1989) Beta-protein amyloid is widely distributed in the central nervous system of patients with Alzheimer’s disease. Am J Pathol 134: 243–51. [PMC free article] [PubMed] [Google Scholar]
- 5. Simpson J, Yates CM, Watts AG, Fink G (1988) Congo red birefringent structures in the hypothalamus in senile dementia of the Alzheimer type. Neuropathol Appl Neurobiol 14: 381–93. [DOI] [PubMed] [Google Scholar]
- 6. Saper CB, Fuller PM, Pedersen NP, Lu J, Scammell TE (2010) Sleep state switching. Neuron 68: 1023–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hassani OK, Lee MG, Jones BE (2009) Melanin-concentrating hormone neurons discharge in a reciprocal manner to orexin neurons across the sleep-wake cycle. Proc Natl Acad Sci U S A 106: 2418–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Adamantidis A, de Lecea L (2009) A role for Melanin-Concentrating Hormone in learning and memory. Peptides 30: 2066–70. Review. [DOI] [PMC free article] [PubMed]
- 9. Bayer L, Eggermann E, Serafin M, Grivel J, Machard D, et al. (2005) Opposite effects of noradrenaline and acetylcholine upon hypocretin/orexin versus melanin concentrating hormone neurons in rat hypothalamic slices. Neuroscience 130: 807–811. [DOI] [PubMed] [Google Scholar]
- 10. Van den Pol AN, Acuna-Goycolea C, Clark KR, Ghosh PK (2004) Physiological properties of hypothalamic MCH neurons identified with selective expression of reporter gene after recombinant virus infection. Neuron 42: 635–52. [DOI] [PubMed] [Google Scholar]
- 11. Hervieu GJ, Cluderay JE, Harrison D, Meakin J, Maycox P, et al. (2000) The distribution of the mRNA and protein products of the melanin-concentrating hormone (MCH) receptor gene, slc-1, in the central nervous system of the rat. Eur J Neurosci 12: 1194–216. [DOI] [PubMed] [Google Scholar]
- 12.Peyron C, Sapin E, Leger L, Luppi PH, Fort P (2009) Role of the melanin-concentrating hormone neuropeptide in sleep regulation. Peptides 30: 2052–9. Review. [DOI] [PubMed]
- 13. Verret L, Goutagny R, Fort P, Cagnon L, Salvert D, et al. (2003) A role of melanin-concentrating hormone producing neurons in the central regulation of paradoxical sleep. BMC Neurosci 4: 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sakamaki R, Uemoto M, Inui A, Asakawa A, Ueno N, et al. (2005) Melanin-concentrating hormone enhances sucrose intake. Int J Mol Med 15: 1033–9. [PubMed] [Google Scholar]
- 15. Smith DG, Davis RJ, Rorick-Kehn L, Morin M, Witkin JM, et al. (2006) McKinzie DL, Nomikos GG, Gehlert DR. Melanin-concentrating hormone-1 receptor modulates neuroendocrine, behavioral, and corticolimbic neurochemical stress responses in mice. Neuropsychopharmacology 31: 1135–45. [DOI] [PubMed] [Google Scholar]
- 16. Millan MJ, Gobert A, Panayi F, Rivet JM, Dekeyne A, et al. (2008) The melanin-concentrating hormone1 receptor antagonists, SNAP-7941 and GW3430, enhance social recognition and dialysate levels of acetylcholine in the frontal cortex of rats. Int J Neuropsychopharmacol 11: 1105–22. [DOI] [PubMed] [Google Scholar]
- 17. Shimada M, Tritos NA, Lowell BB, Flier JS, Maratos-Flier E (1998) Mice lacking melanin-concentrating hormone are hypophagic and lean. Nature 396: 670–4. [DOI] [PubMed] [Google Scholar]
- 18.Chung S, Parks GS, Lee C, Civelli O (2011) Recent updates on the melanin-concentrating hormone (MCH) and its receptor system: lessons from MCH1R antagonists. J Mol Neurosci 43: 115–21. Review. [DOI] [PMC free article] [PubMed]
- 19. Lambe EK, Olausson P, Horst NK, Taylor JR, Aghajanian GK (2005) Hypocretin and nicotine excite the same thalamocortical synapses in prefrontal cortex: correlation with improved attention in rat. J Neurosci 25: 5225–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Arrigoni E, Mochizuki T, Scammell TE (2010) Activation of the basal forebrain by the orexin/hypocretin neurones. Acta Physiol (Oxf) 198: 223–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Delazer M, Högl B, Zamarian L, Wenter J, Gschliesser V, et al. (2011) Executive functions, information sampling, and decision making in narcolepsy with cataplexy. Neuropsychology 25: 477–87. [DOI] [PubMed] [Google Scholar]
- 22. Naumann A, Daum I (2003) Narcolepsy: pathophysiology and neuropsychological changes. Behav Neurol 14: 89–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Raggi A, Plazzi G, Pennisi G, Tasca D, Ferri R (2011) Cognitive evoked potentials in narcolepsy: a review of the literature. Neurosci Biobehav Rev 35: 1144–53. [DOI] [PubMed] [Google Scholar]
- 24. Gozzi A, Turrini G, Piccoli L, Massagrande M, Amantini D, et al. (2011) Functional magnetic resonance imaging reveals different neural substrates for the effects of orexin-1 and orexin-2 receptor antagonists. PLoS One 6: e16406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Fronczek R, van Geest S, Frölich M, Overeem S, Roelandse FW, et al. (2012) Hypocretin (orexin) loss in Alzheimer’s disease. Neurobiol Aging 33: 1642–50. [DOI] [PubMed] [Google Scholar]
- 26. Wennström M, Londos E, Minthon L, Nielsen HM (2012) Altered CSF Orexin and α-Synuclein Levels in Dementia Patients.J Alzheimers Dis. 29: 125–32. [DOI] [PubMed] [Google Scholar]
- 27. Lessig S, Ubhi K, Galasko D, Adame A, Pham E, et al. (2010) Remidios K, Chang M, Hansen LA, Masliah E. Reduced hypocretin (orexin) levels in dementia with Lewy bodies. Neuroreport 21: 756–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Baumann CR, Hersberger M, Bassetti CL (2006) Hypocretin-1 (orexin A) levels are normal in Huntington’s disease. J Neurol 253: 1232–3. [DOI] [PubMed] [Google Scholar]
- 29. Kang JE, Lim MM, Bateman RJ, Lee JJ, Smyth LP, et al. (2009) Cirrito JR, Fujiki N, Nishino S, Holtzman DM. Amyloid-beta dynamics are regulated by orexin and the sleep-wake cycle. Science 326: 1005–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Slats D, Claassen J, Lammers GJ, Melis RJ, Verbeek MM, et al. (2012) Association between Hypocretin-1 and Amyloid-beta 42 Cerebrospinal Fluid Levels in Alzheimer’s Disease and Healthy Controls. Curr Alzheimer Res. 9: 1119–25. [DOI] [PubMed] [Google Scholar]
- 31. Friedman LF, Zeitzer JM, Lin L, Hoff D, Mignot E, et al. (2007) In Alzheimer disease, increased wake fragmentation found in those with lower hypocretin-1. Neurology 68: 793–4. [DOI] [PubMed] [Google Scholar]
- 32. Kessler BA, Stanley EM, Frederick-Duus D, Fadel J (2011) Age-related loss of orexin/hypocretin neurons. Neuroscience 178: 82–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Stanley EM, Fadel J (2012) Aging-related deficits in orexin/hypocretin modulation of the septohippocampal cholinergic system. Synapse 66: 445–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Dubois B, Feldman HH, Jacova C, Cummings JL, Dekosky ST, et al. (2010) Revising the definition of Alzheimer’s disease: a new lexicon. Lancet Neurol 9: 1118–27. [DOI] [PubMed] [Google Scholar]
- 35. Morris JC, Heyman A, Mohs RC, Hughes JP, van Belle G, et al. (1989) The Consortium to Establish a Registry for Alzheimer’s Disease (CERAD). Part I. Clinical and neuropsychological assessment of Alzheimer’s disease. Neurology 39: 1159–65. [DOI] [PubMed] [Google Scholar]
- 36. Russell EW (1982) Factor analysis of the Revised Wechsler Memory Scale tests in a neuropsychological battery. Percept Mot Skills 54: 971–4. [DOI] [PubMed] [Google Scholar]
- 37. Shulman KI (2000) Clock-drawing: is it the ideal cognitive screening test? Int J Geriatr Psychiatry 15: 548–61. [DOI] [PubMed] [Google Scholar]
- 38.Moses JA Jr (2004). Test review-Comprehensive Trail Making Test (CTMT). Arch Clin Neuropsychol 19: 703–8. Review. [DOI] [PubMed]
- 39.First MB, Spitzer RL, Gibbon M, Williams JBW (1997) Structured Clinical Interview for DSM-IV Axis I disorders (SCID I). New York: Biometric Research Department.
- 40. Hamilton M (1960) A rating scale for depression. J Neurol Neurosurg Psychiatry 23: 56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Burkart M, Heun R, Maier W, Benkert O (1998) Dementia screening in routine clinical practice. A comparative analysis of MMSE, SIDAM and ADAS. Nervenarzt 69: 983–90. [DOI] [PubMed] [Google Scholar]
- 42. Salomon RM, Ripley B, Kennedy JS, Johnson B, Schmidt D, et al. (2003) Diurnal variation of cerebrospinal fluid hypocretin-1 (orexin-A) levels in control and depressed subjects. Biol Psychiatry 54: 96–104. [DOI] [PubMed] [Google Scholar]
- 43.Mungas D (1991) In-office mental status testing: a practical guide. Geriatrics 46: 54–8, 63, 66. [PubMed]
- 44. Cecon E, Markus RP (2011) Relevance of the chronobiological and non-chronobiological actions of melatonin for enhancing therapeutic efficacy in neurodegenerative disorders. Recent Pat Endocr Metab Immune Drug Discov 5: 91–9. [DOI] [PubMed] [Google Scholar]
- 45.Guyon A, Conductier G, Rovere C, Enfissi A, Nahon JL (2009) Melanin-concentrating hormone producing neurons: Activities and modulations. Peptides 30: 2031–9. Review. [DOI] [PubMed]
- 46. Adamantidis A, Thomas E, Foidart A, Tyhon A, Coumans B, et al. (2005) Disrupting the melanin-concentrating hormone receptor 1 in mice leads to cognitive deficits and alterations of NMDA receptor function. Eur J Neurosci (21) 2837–44. [DOI] [PubMed] [Google Scholar]
- 47. Monzon ME, de Souza MM, Izquierdo LA, Izquierdo I, Barros DM, et al. (1999) Melanin-concentrating hormone (MCH) modifies memory retention in rats. Peptides 20: 1517–9. [DOI] [PubMed] [Google Scholar]
- 48. Varas M, Pérez M, Ramírez O, de BarioglioSR (2002) Melanin concentrating hormone increase hippocampal synaptic transmission in the rat. Peptides 23: 151–5. [DOI] [PubMed] [Google Scholar]
- 49.Ellenbogen JM, Payne JD, Stickgold R (2006) The role of sleep in declarative memory consolidation: passive, permissive, active or none? Curr Opin Neurobiol 16: 716–22. Review. [DOI] [PubMed]
- 50. Wang G, Grone B, Colas D, Appelbaum L, Mourrain P (2011) Synaptic plasticity in sleep: learning, homeostasis and disease. Trends Neurosci 34: 452–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Rolls A, Colas D, Adamantidis A, Carter M, Lanre-Amos T, et al. (2011) Optogenetic disruption of sleep continuity impairs memory consolidation. Proc Natl Acad Sci U S A 108: 13305–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Gerashchenko D, Murillo-Rodriguez E, Lin L, Xu M, Hallett L, et al. (2003) Relationship between CSF hypocretin levels and hypocretin neuronal loss. Exp Neurol 184: 1010–6. [DOI] [PubMed] [Google Scholar]
- 53. Gao S, Hendrie HC, Hall KS, Hui S (1998) The relationships between age, sex, and the incidence of dementia and Alzheimer disease: a meta-analysis. Arch Gen Psychiatry 55: 809–15. [DOI] [PubMed] [Google Scholar]
- 54. Clinton LK, Billings LM, Green KN, Caccamo A, Ngo J, et al. (2007) Age-dependent sexual dimorphism in cognition and stress response in the 3xTg-AD mice. Neurobiol Dis 28: 76–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Silva A, Andersen ML, De Mello MT, Bittencourt LR, Peruzzo D, et al. (2008) Tufik S.Gender and age differences in polysomnography findings and sleep complaints of patients referred to a sleep laboratory. Braz J Med Biol Res 41: 1067–75. [DOI] [PubMed] [Google Scholar]
- 56. Silveyra P, Cataldi NI, Lux-Lantos V, Libertun C (2009) Gonadal steroids modulated hypocretin/orexin type-1 receptor expression in a brain region, sex and daytime specific manner. Regul Pept 158: 121–6. [DOI] [PubMed] [Google Scholar]
- 57. Jöhren O, Neidert SJ, Kummer M, Dominiak P (2002) Sexually dimorphic expression of prepro-orexin mRNA in the rat hypothalamus. Peptides 23: 1177–80. [DOI] [PubMed] [Google Scholar]
- 58. Schmidt FM, Arendt E, Steinmetzer A, Bruegel M, Kratzsch J, et al. (2011) CSF-hypocretin-1 levels in patients with major depressive disorder compared to healthy controls. Psychiatry Res 190: 240–243. [DOI] [PubMed] [Google Scholar]
- 59. Jack CR Jr, Knopman DS, Jagust WJ, Shaw LM, Aisen PS, et al. (2010) Hypothetical model of dynamic biomarkers of the Alzheimer’s pathological cascade. Lancet Neurol 9: 119–28. [DOI] [PMC free article] [PubMed] [Google Scholar]