Abstract
The fear and stigma associated with Postpartum Depression (PPD) is a major challenge in the treatment of this disease. Our goal is to develop innovative methods of screening women for the symptoms of PPD to facilitate referral and treatment. This study explores the efficacy of the Internet in reaching out to postpartum women in the convenience and privacy of their own homes, particularly those in rural and underserved areas.
An exploratory study design was used to explore the feasibility and acceptability of online screening for PPD with postpartum women in the first 2–3 months after delivery (N=18). In the first phase, a focus group was conducted with a small group of postpartum women; the second phase consisted of individual interviews of postpartum women in their homes; and in phase three, 10 women participated in the on-line screening intervention. Postpartum depression was measured using an online version of the Edinburgh Postnatal Depression Scale (EPDS) a well-established instrument with reported alpha reliabilities (0.81–0.88) across studies and concurrent validity demonstrated using the gold standard, DSM IV criteria for depression interview. Qualitative data collected from all the participants were also analyzed.
The sample included women age 18–29; 70% White/Caucasian, 50% low income, and the majority living in rural areas. The EPDS scores ranged from 0–13 (mean 8.0; SD 4.76). Participants described the online PPD screening process as easy, straightforward and personalized and provided additional suggestions for improvement.
Online Screening and Referral for Postpartum Depression: An Exploratory Study
An estimated 9 to 16 percent of child bearing women are affected by Postpartum Depression (PPD), with a 41 percent incidence rate among women who already have experienced PPD in a previous pregnancy. Postpartum depression is the diagnosis of depressive disorder during the postpartum period, and while not specifically listed in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) (American Psychiatric Association, 2000), symptoms of postpartum onset major depressive disorder are similar to general mood disorders but may also include anxiety, maternal preoccupation with infant well-being, and intrusive thoughts. PPD is a serious mental health problem characterized by a prolonged period of emotional disturbance which accompanies the increased and critical responsibilities of caring for a newborn infant. PPD could result in serious consequences for both mother and infant, such as maternal incapacity to provide optimal care to the infant and compromising infant attachment and child development (Ensminger, Hanson, Riley, & Juon, 2003; Grace, Evindar, & Stewart, 2003).
Despite such consequences for women and infants, research on postpartum depression has shown that the disorder is both under-diagnosed and undertreated by healthcare providers with more than half of PPD cases going undiagnosed. A recent study in England found little evidence that health care providers were using established criteria to assess maternal mental health needs (Lees, 2009). In a large, multi-site study of 298 family practice physicians in the United States, only 12 physicians were routinely screening for postpartum depression using a valid tool (Seehusen, Baldwin, Runkle, & Clark, 2005). In a study by Kim et al. (2009), 95% of obstetrics providers overestimated their screening rates with 67% inaccurately believing that had achieved universal screening (Kim et al., 2009). Providers who were uninvolved in their own office-based PPD screening program had lower screening rates (3%) than those who were active in the in-office screening process (59%). Goodman & Tyer-Viola (2008) found that the majority of women who screened positive during the study had not been identified as at risk for PPD during pregnancy or postpartum (Goodman & Tyer-Viola, 2010).
In addition to provider challenges, the women themselves may resist treatment (Russell, 2006). It is not unusual for women to feel shame and embarrassment about their feelings and be reluctant to admit to symptoms of postpartum depression (Amankwaa, 2003; Ugarriza, 2004). Thus even referred women may be hesitant to seek counseling or treatment (Edwards & Timmons, 2005; Marcus, 2009; McGarry, Kim, Sheng, Egger, & Baksh, 2009). In a study by Flynn (2009) concerns about the stigma associated with PPD resulted in only 35.6% of the women who were referred for treatment, actually participating (Flynn, Henshaw, O'Mahen, & Forman, 2009). Sword, et al. (2008) found that women and their family members and friends, as well as their healthcare professionals tended to normalize symptoms and attribute them to external factors, again suggesting a general lack of knowledge about the etiology, warning signs, timing, screening, and referral of postpartum depression. At the same time, the women expressed a strong preference for treatment in the privacy of the obstetric clinic or in the home (Sword, Busser, Ganann, McMillan, & Swinton, 2008). These findings speak to the need for accurate information and counseling about depression severity, safety, and treatment options, presented in a systematic and comprehensive manner as part of the protocol for pregnancy, childbirth and postpartum management. In addition, accurate screening and referral must be confidential and properly timed.
The internet has become a promising clinical tool for assisting patients to assess their physical and mental health. It is widely used as a source of education, screening, and treatment for many different psychological disorders, including major depressive disorder (Houston et al., 2001; Tate & Zabinsky, 2004). Currently, accurate information about postpartum depression on the internet is comparatively limited (Le, Perry, & Sheng, 2009) but providing accurate information and confidential screening for all pregnant and postpartum women via the internet holds great promise as an innovative solution to address PPD.
Research over the past decade has established that online questionnaires produce information that is as accurate (Buchanan, 2002) or even more accurate (Skårderud, 2003) as traditional paper and pencil questionnaires suggesting its usefulness for detecting symptoms of psychological disorders in general and PPD in particular. According to Skarderud, there is less pressure for the patient’s response to be affected by face to face interactions. Online questions also are able to capture more ethnically diverse participants compared to in-person inquiries, allowing the results to be applied more broadly (Le et al., 2009)
The Study
An exploratory study to assess the feasibility of on-line screening for PPD was conducted in the southern United States among low-risk women who delivered in a comprehensive health science center in 2010. The purpose was to (1) test the efficacy of on-line assessment of PPD and (2) identify women’s responses to online self-screening for postpartum depression in preparation for a larger study. The long-term goal is to test the usefulness of online screening as a vehicle to achieve more comprehensive identification, assessment, referral and treatment for PPD.
Methods
Institutional review board approval was obtained prior to data collection. Participants were initially recruited from a local hospital postpartum unit 24–72 hours after delivery. To be eligible for the study, mothers: (1) were over the age of 18; (2) were able to read English; and (3) had just delivered a healthy infant. Research assistants introduced the study and invited women to participate, then conducted the informed consent process. All participants completed a demographic questionnaire on a laptop computer in the hospital and later self-administered the EDPS 2–3 months after the birth of their infant. The computer was able to instantly provide individualized results of the PPD screening (EDPS score and interpretation) and referral information to each participant. This time frame was chosen because PPD can occur anytime in the first year after delivery but peak incidence appears to be two to three months after delivery (Beeghly et al., 2002; Gaynes et al., 2005).
A descriptive mixed-mode study design was used to explore the feasibility of online screening for PPD using the Edinburgh Postnatal Depression Scale (EPDS) in a convenience sample (N=18) of healthy volunteers that included postpartum women in the first 2–3 months after delivery. An online version of the EPDS scale was used. The EPDS first developed by Cox, Holden & Sagovsky (1987), evaluates emotional distress in the postpartum period and includes items on anxiety, crying, and self-harm. Scoring: The 10 items are rated on a 0–3 point Likert-scale, including reverse-coded items. Total scores range from 0 to 30, with higher scores indicating PPD. The cut off score ≥ 10 is a positive screen for minor or major depression (J. L. Cox & Holden, 2007). Cut off scores of 12/13 have been used for postpartum depression screening (Chaudron et al., 2010; M. C. Logsdon & Myers, 2010). The EPDS is written at a 3rd grade reading level, has been translated into many languages, and is available in the public domain. It is one of the most widely used instruments for PPD screening. Definitive diagnosis of PPD still requires further specialized assessment by a trained health care provider.
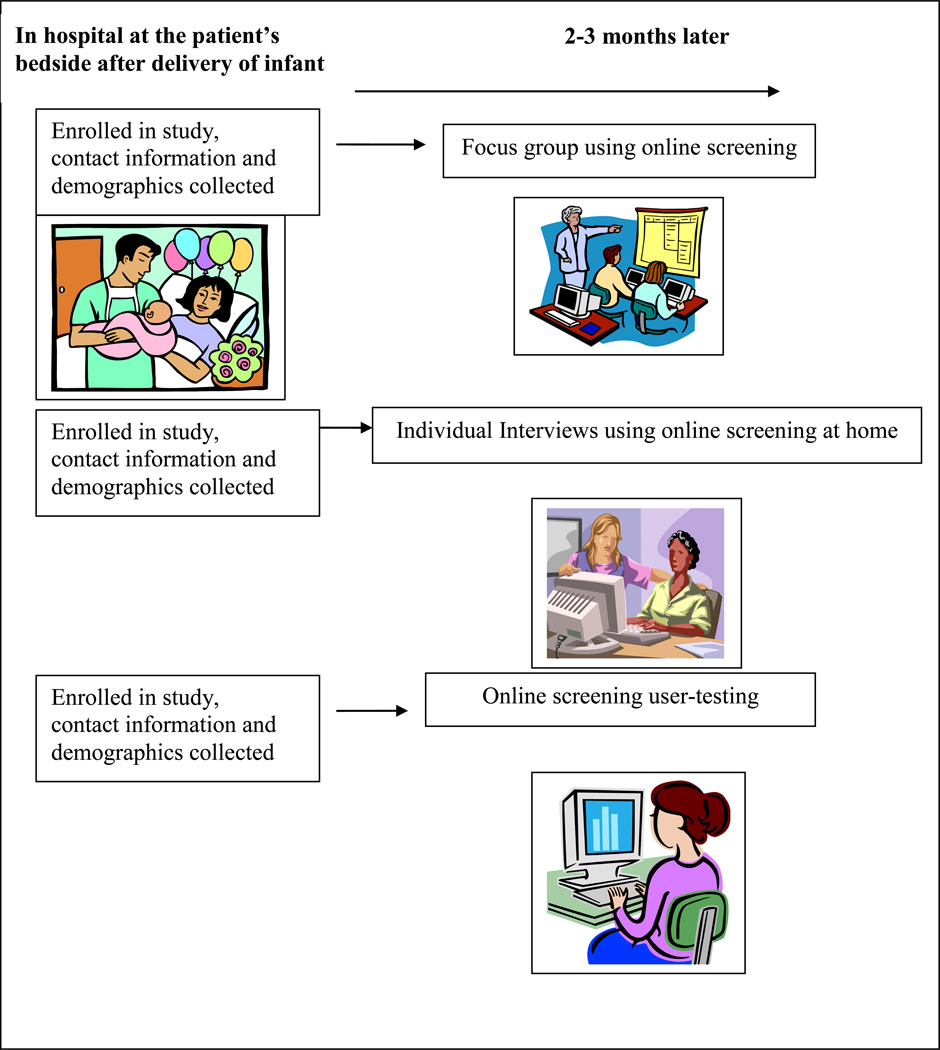
To test feasibility, this study was conducted in three phases. In Phase 1, we conducted a focus group with a small group of healthy postpartum women; in Phase 2, we conducted individual interviews with five different healthy postpartum women; and in Phase 3, we conducted online user-testing with 10 other healthy postpartum women (see Figure 1).
Figure 1.
Model of study: Pilot study of online screening for postpartum depression (PPD)
Phase 1 Focus Group
Ten low-risk postpartum women were invited to participate in a focus group; three women actually showed up for the focus group. The focus group met approximately three months after delivery, lasted two hours, and met in a hospital conference room where participants were observed directly and their comments were audio and video-recorded and then transcribed verbatim. Six major topic areas were explored: (1) the look, feel and approach of the online screening, (2) the ease of navigating through the online screening, (3) the clarity of the instructions and individual questions, (4) the presentation of EDPS results, (5) the helpfulness of postpartum depression information provided, and (6) the participants’ access to computers and ability to complete the online screening either in their own home or other convenient location. We also asked for any other suggestions or comments. These data were analyzed and used to construct changes in the online screening for the next phase.
Phase 2 Home Interviews
In the next phase of the study, five individual interviews were completed in the homes of participants approximately three months after delivery and lasted approximately 30 minutes and were audio-recorded. To ascertain the advantages of private versus group context for obtaining the richest data, we interviewed some women in a group setting and some at home, privately. We also wanted to know if women were able to access the online survey from their home computers with ease. The same semi-structured interview guide was used with the goal of eliciting perceptions of the experience of online self-screening for PPD.
Phase 3 User-Testing of Intervention
Finally, for the last phase of the study, we conducted online user-testing. Data were collected from an additional group of 10 women at two distinct time points: (1) one to two days after delivery and (2) three months after delivery. In the first data collection period, the ten participants were enrolled prior to discharge from the hospital. They entered their own demographic data into a laptop computer which we provided at the bedside. Approximately three months later, the same group of participants received an email with a link to the online survey so that they could self-administer PPD screening at home. One reminder e-mail was sent along with a token incentive ($10.00 gift certificate). Each participant who completed the survey received an individualized EPDS score and interpretation information. During the online user-testing, respondents were able to type in answers to several open-ended questions regarding their experience at the end of online screening and these were also included for content analysis.
Referral and Safety Plan
All participants were given information about PPD plus contact information for local and national resources. If a participant reported feelings of severe depression/emotional distress, feelings of harm to self or others, we were ready to evaluate and refer them to a health care provider for further assessment and support per the study Safety Plan. In this study, only one participant reported an EPDS score >13 and was currently receiving treatment.
Data Analysis
Demographic characteristics, EDPS scores, response rates, and psychometric properties were examined using a standard statistical program (SPSS, version 19.0). To facilitate a qualitative analysis, we began by entering transcripts of raw data into a software program (NVIVO, QSR International). The research team further refined codes from these data, based on common themes we identified relevant to the research questions (e.g., the experience of online self-screening and suggestions for improvement). An iterative process was used to compare results until agreement was reached on code definitions. The credibility of the study analysis was enhanced by detailed data from in-depth interviews, rigorous code development, the group consensus process and the involvement of researchers with varying professional backgrounds in psychology, nursing, and perinatal health.
Results
Demographic characteristics
Table 1 presents demographic characteristics of the 18 participants. These women ranged in age from 18–29; the majority lived in rural communities, half were low income (defined as annual household income less than $30,000/year), the majority were white/Caucasian and married. All reported that they had email and internet access.
Table 1.
Characteristics of the Sample (N = 18)
| N | ||
|---|---|---|
| Age Range | 18–29 years old | |
| Race | ||
| White/Caucasian | 13 | |
| African American | 4 | |
| Other/unknown | 1 | |
| Education Level | ||
| High School | 10 | |
| College | 8 | |
| Marital status | ||
| Unmarried | 9 | |
| Married | 9 | |
| Socio Economic Status | ||
| Low income | 9 | |
| Rural/Urban | ||
| Rural | 11 | |
| Urban | 8 | |
| Email/Internet access | 18 |
Depression scores and instrument analysis
The EPDS scores among study participants ranged from 0–13 (mean 8.0; SD 4.76). The online version of the EPDS used in this study demonstrated good internal consistency (cronbach’s α =0.81). In this study, participants completed the online version of the EPDS in 2 minutes or less.
The response rate for the user-test group was a 50% (5/10). Responses came in fairly quickly. After receiving an email prompt to complete the screening, participants completed the online screening within average of 6 days (range: 7 minutes – 12 days). No significant differences were found when comparing demographics of responders to non-responders in this sample.
Qualitative Data Analysis
The qualitative data from the focus group and individual interviews with women in their homes, revealed four main themes: (1) the postpartum experience; (2) ease and acceptability of online survey for PPD; (3) identification of resources and help-seeking behaviors, and; (4) suggestions for improvement.
- The postpartum experience;“A huge thing I think is not just what type of birth you had on the surface, but how do you feel about it? Do you feel traumatized by the birth that you had? Do you feel that you were a failure somehow in the birth that you had? Do you have something like you wanted to breast feed, but weren’t able to. That’s huge as to how she feels she’s doing as a mother.”“The last two weeks don’t compare to awhile ago when I was, I mean, I know emotionally I’m in a completely different [better] place than I was a month ago”“I’d say [the first] six weeks was a really rough time for me”“There has been lots of worrying.”
- Ease and acceptability of online screening for PPD;“I thought it was pretty easy”“I’m breastfeeding while I’m clicking [completing online screening]”“Great non-intimidating venue”
- Identification of resources and help-seeking behaviors:“You’re not going to want to just be on the phone, like, yeah I’m suffering from postpartum depression, who do I talk to? You want someone who is expecting the call, like that’s why that person is there and you’re not just blurting it out to anybody who answers the phone.”
- Suggestions for improvement“It seems like a lot of the times the partner, husband, or boyfriend would notice this and be more proactive. I don’t know if maybe there would be some way to reach out to them also as a way for them to get help for the mother when they are noticing that something is not right and she’s not able to take the initiative to deal with it. That might help.”
Interestingly, none of the participants sought further information and resources within the online materials that came with the screening. They did not click on any links to go beyond the current web page. One participant suggested sending educational information and resources in a separate follow-up email.
Discussion
Reliability and validity
The online version of the EPDS used in this study demonstrated good internal consistency (α = 0.81), similar to what has been reported in other studies using an online version of the EPDS (0.87)(Le et al., 2009) and is congruent with reliability estimates from the EPDS in traditional paper and pencil format (0.81–0.88) (Dennis, 2004; M. C. Logsdon, Wisner, Hanusa, & Phillips, 2003) (M. C. Logsdon et al., 2003). The mean (mean 8.0; SD 4.76) and range (0–13) of EPDS scores in this small sample were similar to the scores reported in larger samples (mean 7.8)( Reichenheim, Moraes, Oliveira, & Lobato, 2011)
Social desirability or acceptable response bias can be an issue when asking questions about sensitive topics. Mothers may be reluctant to admit to depressive symptoms for fear of stigma or fear that their baby could be removed from them. However, some research has shown that computerized or online surveys actually decrease participants’ their inclination to give a socially-desirable response and may allow for more honest answers due to a sense of privacy and lack of perceived judgment (Estes et al., 2010).
Response Rates
According to a review of the literature by Dillman and colleagues, typical response rates for internet surveys range from 50–65%. The response rate for this exploratory study falls within that range. Additional strategies that may help improve web survey response rates include: Pre-survey notice, pre-paid token incentives, personalized email, and follow-up contacts, each with a tailored appeal (Dillman, Smyth, & Christian, 2009).
Feasibility and Accessibility
Based on the qualitative data from this exploratory study, online screening for PPD appeared to be feasible and acceptable for most participants. Taking a family centered approach may help improve the process. Partners and family members could be included in the email contact and online screening. In fact, partners may benefit from screening too. Emerging research suggests that fathers can also suffer for depression after delivery; they may also be in the best position to recognize symptoms for themselves or in their partner (Nazareth, 2011; Paulson & Bazemore, 2010). Providing information to the entire family can help mobilize resources for those in need. This is especially important because it may be difficult to motivate the depressed person to take action on their own.
An interesting finding in this study was the failure of any participants to seek out further information or resources available with the online screening. Promoting help seeking remains a challenge in the treatment of PPD and depression in general (Barney, Griffiths, Jorm & Christensen, 2006). Creative interventions pairing social media and face-to-face counseling in a multi-stage process may be helpful. Improving knowledge and availability of services is important (Golberstein, Eisenberg & Gollust, 2008). Further research targeted at the referral and help seeking process after PPD screening is needed with larger, more diverse samples of women with a range of mild, moderate and severe symptoms.
The ability to perform the screening multiple times in the postpartum period is critical due to the fact that PPD can occur anytime in the first year after delivery. This type of online screening can be offered multiple times, but it will still not capture all women. Other forms of screening in other settings will continue to be necessary. Screening should continue to take place in pediatric offices, emergency departments, and anywhere families with new children are seen (Drake, E. & Coolidge, G., 2010; Earls & Committee on Psychosocial Aspects of Child and Family Health American Academy of Pediatrics, 2010).
Methodological considerations
This exploratory study with nested qualitative methods was under-powered for statistical significance but the qualitative data was rich and provided valuable information for the exploratory purpose of this study. All women who participated in this study reported that online screening was accessible and helpful, thus the results from this study are promising and suggest that further research could be conducted with larger samples using online screening. Further research is clearly needed to refine the referral process after screening, monitor treatment engagement rates, and measure health outcomes.
Conclusion
In light of the recent Institute of Medicine (IOM) report on depression in parents (National Research Council and Institute of Medicine, 2009) and The Joint Commission (JCAHO) patient safety goals calling for increased depression screening and suicide risk evaluation, this method of online screening may become a viable and useful option to help meet those requirements as one part of a comprehensive screening, referral and treatment plan. It may also be possible to cluster additional screening, such as partner violence, parenting stress, or self-efficacy along with online PPD screening.
Acknowledgments
Source of Support/Acknowledgements: NIH-NINR grant P20NR009009, Rural Health Care Research Center, University of Virginia School of Nursing, Postpartum Support International (PSI), Susan Hickman Research Award
Contributor Information
Emily Drake, University of Virginia School of Nursing.
Erica Gustavson, University of Virginia School of Nursing.
Emily Kinsey, University of Virginia School of Medicine.
References
- Amankwaa L. Postpartum depression among african-american women. Issues in Mental Health Nursing. 2003;24:297–316. doi: 10.1080/01612840305283. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic criteria from DSM-IV-TR. Washington, DC: The Association; 2000. [Google Scholar]
- Barney LJ, Griffiths KM, Jorm AF, Christensen H. Stigma about depression and its impact on help-seeking intentions. Australian & New Zealand Journal of Psychiatry. 2006;40(1):51–54. doi: 10.1080/j.1440-1614.2006.01741.x. [DOI] [PubMed] [Google Scholar]
- Beeghly M, Weinberg MK, Olson KL, Kernan H, Riley J, Tronick EZ. Stability and change in level of maternal depressive symptomatology during the first postpartum year. Journal of Affective Disorders. 2002;71(1–3):169–180. doi: 10.1016/s0165-0327(01)00409-8. [DOI] [PubMed] [Google Scholar]
- Buchanan T. Online assessment: Desirable or dangerous? Professional Psychology-Research and Practice. 2002;33(2):148–154. [Google Scholar]
- Chaudron LH, Szilagyi PG, Tang W, Anson E, Talbot NL, Wadkins HI, Wisner KL. Accuracy of depression screening tools for identifying postpartum depression among urban mothers. Pediatrics. 2010;125(3):e609–e617. doi: 10.1542/peds.2008-3261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox JL, Holden JM. Perinatal mental health: A guide to the edinburgh postnatal depression scale. Glasgow, UK: Royal College of Psychiatrists; 2007. [Google Scholar]
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. development of the 10-item edinburgh postnatal depression scale. British Journal of Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Dennis CL. Can we identify mothers at risk for postpartum depression in the immediate postpartum period using the edinburgh postnatal depression scale? Journal of Affective Disorders. 2004;78(2Using Smart Source Parsing Feb):163–169. doi: 10.1016/s0165-0327(02)00299-9. [DOI] [PubMed] [Google Scholar]
- Dillman D, Smyth J, Christian M. Internet, mail, and mixed-mode surveys: The tailored design method. 3rd Ed. ed. Hoboken, NJ: Wiley; 2009. [Google Scholar]
- Drake E, Coolidge G. Postpartum depression: Don’t let patients suffer in silence. American Nurse Today. 2010;Vol 5(No. 12):1–5. [Google Scholar]
- Earls MF Committee on Psychosocial Aspects of Child and Family Health American Academy of,Pediatrics. Incorporating recognition and management of perinatal and postpartum depression into pediatric practice. Pediatrics. 2010;126(5):1032–1039. doi: 10.1542/peds.2010-2348. [DOI] [PubMed] [Google Scholar]
- Edwards E, Timmons S. A qualitative study of stigma among women suffering postnatal illness. Journal of Mental Health. 2005;14(5):471–481. [Google Scholar]
- Ensminger M, Hanson S, Riley A, Juon H. Maternal psychological distress: Adult sons' and daughters' mental health and educational attainment. Journal of the American Academy of Child & Adolescent Psychiatry. 2003;42:1108–1115. doi: 10.1097/01.CHI.0000070261.24125.F8. [DOI] [PubMed] [Google Scholar]
- Estes LJ, Lloyd LE, Teti M, Raja S, Bowleg L, Allgood KL, Glick N. Perceptions of audio computer-assisted self-interviewing (ACASI) among women in an HIV-positive prevention program. PLoS ONE [Electronic Resource] 2010;5(2):e9149. doi: 10.1371/journal.pone.0009149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flynn H, Henshaw E, O'Mahen H, Forman J. Patient perspectives on improving the depression referral processes in obstetrics settings: A qualitative study. General Hospital Psychiatry. 2009;32:9–16. doi: 10.1016/j.genhosppsych.2009.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaynes B, Gavin N, Melzer-Brody S, Lohr K, Swinson T, Gartlehner G, Miller W. Perinatal depression: Prevalence, screening accuracy, and screening outcomes. Rockville, MD: 2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golberstein E, Eisenberg D, Gollust SE. Perceived stigma and mental health care seeking. Psychiatric Services. 2008;59(4):392–399. doi: 10.1176/ps.2008.59.4.392. [DOI] [PubMed] [Google Scholar]
- Goodman J, Tyer-Viola L. Detection, treatment, and referral of perinatal depression and anxiety by obstetrical providers. Journal of Women's Health. 2010;19(3):477–490. doi: 10.1089/jwh.2008.1352. [DOI] [PubMed] [Google Scholar]
- Grace S, Evindar A, Stewart D. The effect of postpartum depression on child cognitive development and behavior: A review and critical analysis of the literature. Archives of Women's Mental Health. 2003;6(4):263– 274. doi: 10.1007/s00737-003-0024-6. [DOI] [PubMed] [Google Scholar]
- Houston T, Cooper L, Vu H, Kahn J, Toser J, Ford D. Screening the public for depression through the internet. Psychiatric Services. 2001;52(3):362–367. doi: 10.1176/appi.ps.52.3.362. [DOI] [PubMed] [Google Scholar]
- Kim JJ, La Porte LM, Adams MG, Gordon TE, Kuendig JM, Silver RK. Obstetric care provider engagement in a perinatal depression screening program. Archives of Women's Mental Health. 2009;12(3):167–172. doi: 10.1007/s00737-009-0057-6. [DOI] [PubMed] [Google Scholar]
- Le H, Perry D, Sheng X. Using the internet to screen for postpartum depression. Maternal and Child Health Journal. 2009;13:213–221. doi: 10.1007/s10995-008-0322-8. [DOI] [PubMed] [Google Scholar]
- Lees S. Professionals' knowledge of perinatal mental health care. Mental Health Practice. 2009;13(9):24–27. [Google Scholar]
- Logsdon MC, Myers JA. Comparative performance of two depression screening instruments in adolescent mothers. Journal of Women's Health (15409996) 2010;19(6):1123–1128. doi: 10.1089/jwh.2009.1511. [DOI] [PubMed] [Google Scholar]
- Logsdon MC, Wisner K, Hanusa BH, Phillips A. Role functioning and symptom remission in women with postpartum depression after antidepressant treatment. Archives of Psychiatric Nursing. 2003;17(6):276–283. doi: 10.1053/j.apnu.2003.10.004. [DOI] [PubMed] [Google Scholar]
- Marcus SM. Depression during pregnancy: Rates, risks and consequences--motherisk update 2008. Canadian Journal of Clinical Pharmacology/Journal Canadien De Pharmacologie Clinique. 2009;16(1):e15–e22. [PubMed] [Google Scholar]
- McGarry J, Kim H, Sheng X, Egger M, Baksh L. Postpartum depression and help-seeking behavior. Journal of Midwifery & Women's Health. 2009;54(1):50–56. doi: 10.1016/j.jmwh.2008.07.003. [DOI] [PubMed] [Google Scholar]
- Nazareth I. Should men be screened and treated for postnatal depression? Expert Review of Neurotherapeutics. 2011;11(1):1–3. doi: 10.1586/ern.10.183. [DOI] [PubMed] [Google Scholar]
- Paulson JF, Bazemore SD. Prenatal and postpartum depression in fathers and its association with maternal depression: A meta-analysis. JAMA. 2010;303(19):1961–1969. doi: 10.1001/jama.2010.605. [DOI] [PubMed] [Google Scholar]
- Reichenheim ME, Moraes CL, Oliveira AS, Lobato G. Revisiting the dimensional structure of the edinburgh postnatal depression scale (EPDS): Empirical evidence for a general factor. BMC Medical Research Methodology. 2011;11:93. doi: 10.1186/1471-2288-11-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell S. Barriers to care in postnatal depression. Community Practitioner. 2006;79(4):110–111. [PubMed] [Google Scholar]
- Seehusen D, Baldwin L, Runkle G, Clark G. Are family physicians appropriately screening for postpartum depression? Journal of the American Board of Family Medicine. 2005;18(2):104–112. doi: 10.3122/jabfm.18.2.104. [DOI] [PubMed] [Google Scholar]
- Skårderud F. Sh@me in cyberspace. relationships without faces: The E-media and eating disorders. European Eating Disorders Review. 2003;11(3):155–169. [Google Scholar]
- Sword W, Busser D, Ganann R, McMillan T, Swinton M. Women's care-seeking experiences after referral for postpartum depression. Qualitative Health Research. 2008;18(9):1161–1173. doi: 10.1177/1049732308321736. [DOI] [PubMed] [Google Scholar]
- Tate D, Zabinsky M. Computer and internet applications for psychological treatment: Update for clinicians. Journal of Clinical Psychology. 2004;33(2):209–220. doi: 10.1002/jclp.10247. [DOI] [PubMed] [Google Scholar]
- Ugarriza D. Group therapy and its barriers for women suffering from post-natal depression. Archives of Psychiatric Nursing. 2004;18(2):39–48. doi: 10.1053/j.apnu.2004.01.002. [DOI] [PubMed] [Google Scholar]