Abstract
Currently, pay lines for NIH grants are at a historical low. In this climate of fierce competition knowledge about the funding situation in a small field like Radiation Oncology becomes very important for career planning and recruitment of faculty. Unfortunately, this data cannot be easily extracted from the NIH s database because it does not discriminate between Radiology and Radiation Oncology Departments.
At the start of fiscal year 2013, we extracted records for 952 individual grants, which were active at the time of analysis from the NIH database. Proposals originating from Radiation Oncology Departments were identified manually. Descriptive statistics were generated using the JMP statistical software package.
Our analysis identified 197 grants in Radiation Oncology. These proposals came from 134 individual investigators in 43 academic institutions. The majority of the grants (118) were awarded to PIs at the Full Professor level and 122 PIs held a PhD degree. In 79% of the grants the research topic fell into the field of Biology, in 13 % into the field of Medical Physics. Only 7.6% of the proposals were clinical investigations.
Our data suggests that the field of Radiation Oncology is underfunded by the NIH, and that the current level of support does not match the relevance of Radiation Oncology for cancer patients or the potential of its academic work force.
Keywords: NIH, Radiation Oncology, funding
Introduction
Biomedical funding in the United States has changed dramatically since 1998. While the direct costs requested from the National Institute of Health (NIH) for investigator-initiated research project grants increased from $4.4 billion in fiscal year (FY) 1998 to more than $13 billion in fiscal year 2011, the funds awarded increased only from $1 billion to $2 billion. Only a small portion of this sharp increase in requested funds is caused by an increased number of applications per principal investigator (PI), the main reason being the increasing size of the biomedical workforce (source:http://nexus.od.nih.gov/all/2012/08/09/more-applications-many-more-applicants/).
In this environment of fierce competition, an overall knowledge of the funding rate in a small field like Radiation Oncology/Biology/Physics becomes crucial. Such information would provide guidance to residency applicants for career planning purposes and support departments in recruiting new faculty. In the analysis described here we have attempted to break down the numbers of NIH support as it pertains to Radiation Oncology/Biology/Physics. However, the NIH database merges data for Radiation Oncology/Biology/Physics with data for Radiology, thus making it difficult to distinguish between NIH funding for Radiation versus Radiology Departments. Therefore, in order to get a clearer picture of the NIH funding landscape in Radiation Oncology/Biology/Physics, we decided to manually extract the funding information for Radiation Oncology/Biology/Physics from the NIH database, and analyze the data to better understand the distribution of NIH grants and awards across institutions.
Methods
The NIH database (1) was queried. The search was limited to grants awarded to PIs in academic departments listed as Radiation-Diagnostic/Oncology. Affiliation of individual PIs to radiation oncology departments and/or association of the research topic with radiation oncology/biology/physics were verified using Internet search engines and the project description provided by the PI. For non-disclosed reasons, some institutions (e.g. Harvard University, Mayo Clinic, and Memorial Sloan Kettering) do not list an academic department in their applications. These institutions were left out because the search would have had to rely on PI names listed on the website of these institutions, which may or may not reflect the current body of faculty in a department correctly. Career levels, academic degrees, and the field of study for each investigator were queried from the homepages of the individual institutions.
Descriptive statistics were obtained using the JMP statistical software package (SAS; version 10).
Results
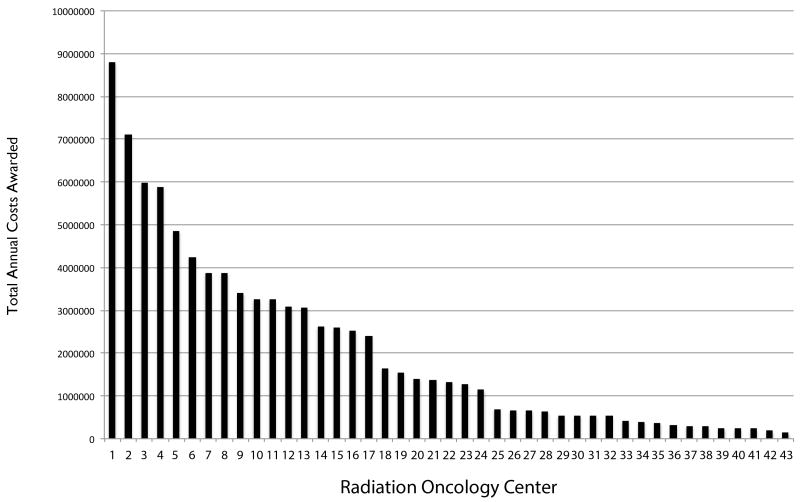
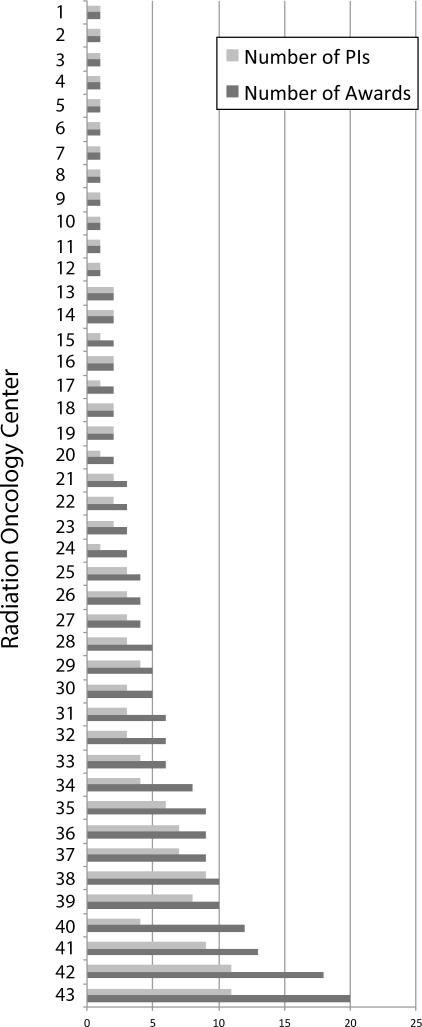
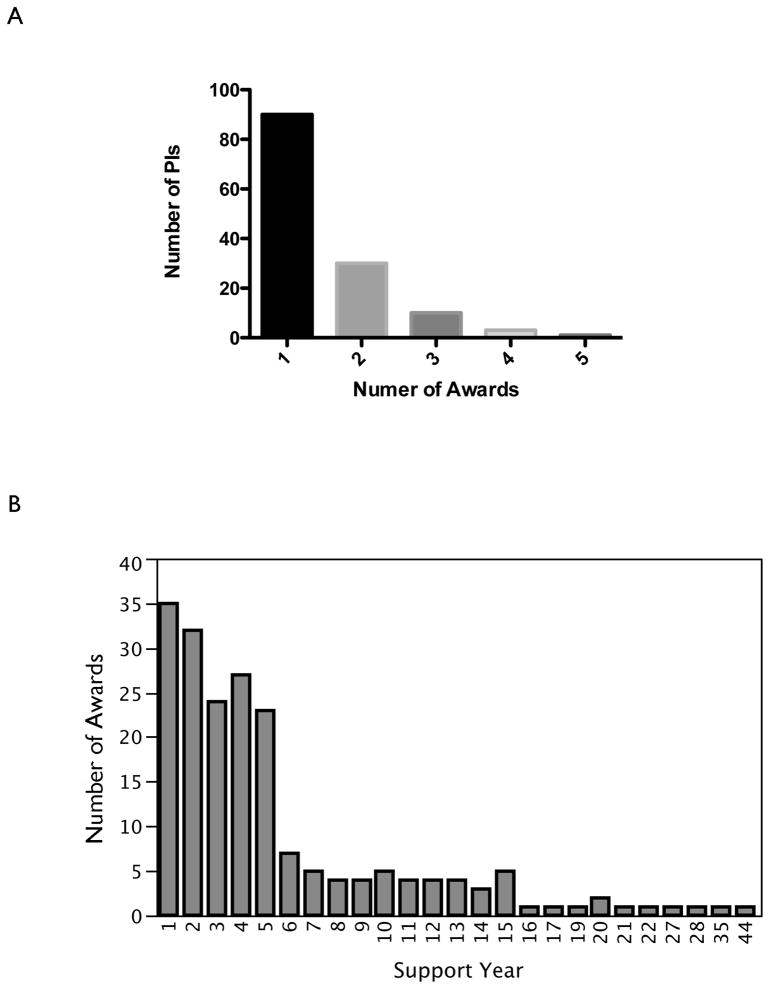
The query resulted in 952 individual awards, active 10 days after the start of the FY 2013. From these 952 awards, 197 were identified as Radiation Oncology/Biology/Physics-related projects. The 197 projects came from 43 academic institutions, all located inside the United States (Figure 1A/B). These projects were awarded to 134 individual investigators, which results in an average of 1.47 awards per investigator (1 award: n=90 (67.2%); 2 awards: n=30 (22.4%); 3 awards: n=10 (7.5%); 4 awards: n=3 (2.2%); 5 awards: n=1 (0.7%)) (Figure 2A). 141 (71.6%) of all awards were in year 1–5 of their funding cycle. 56 (28.4%) awards had been renewed 1–4 times and were in funding year 6–25 (Figure 2B). 89 (70.1%) of all R01 awards were in year 1 to 5 of their funding period, 20 (15.7%) in year 6–10, 12 (9.4%) in year 11–15, 3 (2.4%) in year 16–20 and year 21–25 each.
Figure 1.
(A) Ranking of U.S. Radiation Oncology centers based on total active funding from the NIH at the beginning of fiscal year 2013.
(B) Number of NIH awards and number of PIs per institution at the beginning of fiscal year 2013
Figure 2.
Distribution of PIs in Radiation Research with 1 to 5 NIH awards. A) A total of 134 individual investigators were awarded 197 grants, resulting in an average of 1.47 awards per investigator (1 award: n=90 (67.2%); 2 awards: n=30 (22.4%); 3 awards: n=10 (7.5%); 4 awards: n=3 (2.2%); 5 awards: n=1 (0.7%))
(B) Distribution of the current funding year for all active awards at the beginning of fiscal year 2013.
141 (71.6%) of all awards were in year 1–5 of their funding cycle.
PhDs were the largest group of investigators funded by NIH, with a total of 122 PIs, followed by MD/PhDs (48) and MDs (23). In addition, four PIs held a DVM, a DVM/PhD, Ed.D., or a MSEE CCE degree.
The PIs of 118 grants were at the level of Full Professor, in 49 grants at the level of Associate Professor, and 27 PIs were at the level of an Assistant Professor at the time of the analysis. Three PIs held a position as a lecturer, postdoc, or senior research scientist.
The majority of grants were awarded to Radiation Biology (n=156, 79.2%), 26 (13.2%) awards had a Physics topic, and only 15 (7.6%) awards were clinical investigations. In projects related to radiation biology 98 (62.8%) PIs held a Ph.D., 45 (29.2%) a MD/PhD, 11 (7.1%) a MD degree, and 2 (1.3%) a DVM or DVM/PhD degree. Projects related to medical physics, were led by 23 (88.5%) PIs holding a PhD, 1 (3.8%) a MD/PhD, 1 (3.8%) an Engineering and 1 a (3.8%) Dosimetry degree. Out 15 PIs of the clinical projects, 12 (80%) held a MD, 2 (13.3%) a MD/PhD and 1 (6.7%) a PhD degree.
Only 18 institutions had 3 or more investigators with active NIH funding with an average of 1.52 (range 1 to 3) grants per investigator. The NIH-funded research program of 25 institutions relied on 1 or 2 investigators.
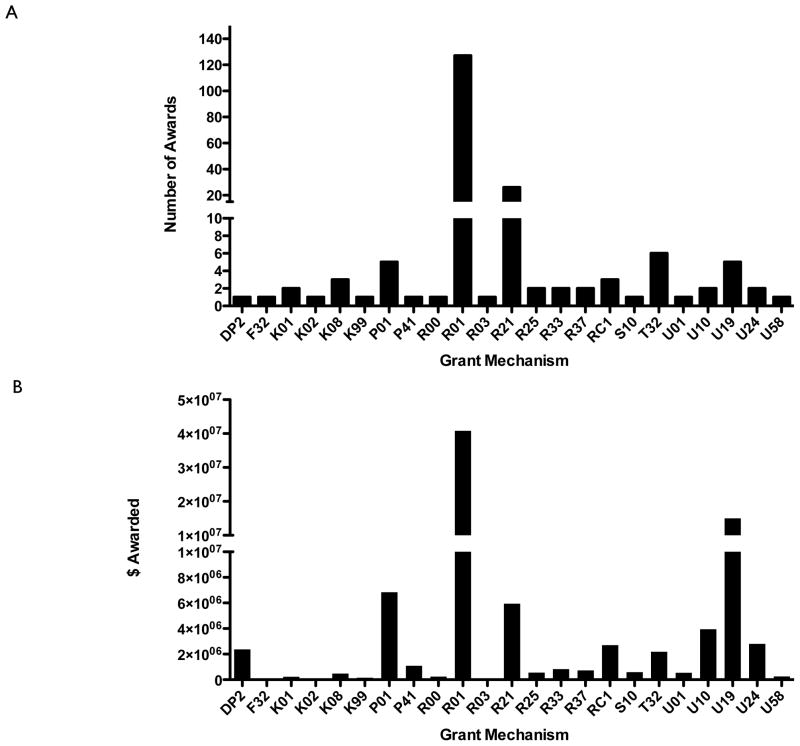
The total amount of active NIH funding for Radiation Oncology/Biology/Physics projects for FY 2013 was $ 85,511,067 (direct plus indirect costs) with an average award size of $449,294 +/− $537,065.5. The majority of awards were granted through the R01 (n=126) and R21 (n=26) funding mechanisms (Figure 3A). More than two thirds (76.9%) of the monetary NIH support granted for radiation research was awarded through the R01 (46.1%), U19 (16.4%), P01 (7.7%) and R21 (6.7%) funding mechanisms (Figure 3B). Administrative supplements were granted for 5 awards (one K01, one P01, two R01s, one U24). A total of 22 (11.2%) applications were funded after resubmissions (A1). A list with the description of the different grant types awarded to radiation oncology departments is given in Table 1.
Figure 3.
Distribution of all awards between the different award mechanisms (A) and total annual costs (B). More than two thirds (76.9%) of the NIH support granted for radiation research was awarded under the P01, R01, R21, and U19 mechanisms.
Table 1.
Grant types awarded to Radiation Oncology Departments
| Funding Mechanism | Title | Description |
|---|---|---|
| DP2 | NIH Director’s New Innovator Awards | To support highly innovative research projects by new investigators in all areas of biomedical and behavioral research. |
| F32 | Postdoctoral Individual National Research Service Award | To provide postdoctoral research training to individuals to broaden their scientific background and extend their potential for research in specified health-related areas. |
| K01 | Research Scientist Development Award-Research & Training | For support of a scientist, committed to research, in need of both advanced research training and additional experience. |
| K02 | Research Scientist Development Award-Research | For support of a scientist, committed to research, in need of additional experience. |
| K08 | Clinical Investigator Award | To provide the opportunity for promising medical scientists with demonstrated aptitude to develop into independent investigators, or for faculty members to pursue research aspects of categorical areas applicable to the awarding unit, and aid in filling the academic faculty gap in these shortage areas within health profession’s institutions of the country. |
| K99 | Career Transition Award | To support the initial phase of a Career/Research Transition award program that provides 1–2 years of mentored support for highly motivated, advanced postdoctoral research scientists. |
| P01 | Research Program Projects | For the support of a broadly based, multidisciplinary, often long-term research program, which has a specific major objective or a basic theme. A program project generally involves the organized efforts of relatively large groups, members of which are conducting research projects designed to elucidate the various aspects or components of this objective. Each research project is usually under the leadership of an established investigator. |
| P41 | Biotechnology Resource Grants | To support biotechnology resources available to all qualified investigators without regard to the scientific disciplines or disease orientations of their research activities or specifically directed to a categorical program area. |
| R00 | Research Transition Award | To support the second phase of a Career/Research Transition award program that provides 1–3 years of independent research support (R00) contingent on securing an independent research position. |
| R01 | Research Project | To support a discrete, specified, circumscribed project to be performed by the named investigator(s) in an area representing his specific interest and competencies. |
| R03 | Small Research Grants | To provide research support specifically limited in time and amount for studies in categorical program areas. |
| R21 | Exploratory/Developmental Grants | To encourage the development of new research activities in categorical program areas. |
| R25 | Education Projects | For support to develop and/or implement a program as it relates to a category in one or more of the areas of education, information, training, technical assistance, coordination, or evaluation. |
| R33 | Exploratory/Developmental Grants Phase II | The R33 award is to provide a second phase for the support for innovative exploratory and development research activities initiated under the R21 mechanism. |
| R37 | Method to Extend Research in Time (MERIT) Award | To provide long-term grant support to investigators whose research competence and productivity are distinctly superior and who are highly likely to continue to perform in an outstanding manner. |
| RC1 | NIH Challenge Grants and Partnerships Program | NIH Challenge Grants in Health and Science Research |
| S10 | Biomedical Research Support Shared Instrumentation Grants | To make available to institutions with a high concentration of NIH extramural research awards, research instruments which will be used on a shared basis. |
| T32 | Institutional National Research Service Award | To enable institutions to make National Research Service Awards to individuals selected by them for predoctoral and postdoctoral research training in specified shortage areas. |
| U01 | Research Project--Cooperative Agreements | To support a discrete, specified, circumscribed project to be performed by the named investigator(s) in an area representing his specific interest and competencies. |
| U10 | Cooperative Clinical Research--Cooperative Agreements | To support clinical evaluation of various methods of therapy and/or prevention in specific disease areas. |
| U19 | Research Program--Cooperative Agreements | To support a research program of multiple projects directed toward a specific major objective, basic theme or program goal, requiring a broadly based, multidisciplinary and often long-term approach. |
| U24 | Resource-Related Research Projects--Cooperative Agreements | To support research projects contributing to improvement of the capability of resources to serve biomedical research. |
| U58 | Chronic Disease Control Cooperative Agreement | In cooperation with State and local public health agencies and other public or private organizations to assist in controlling and preventing chronic diseases. |
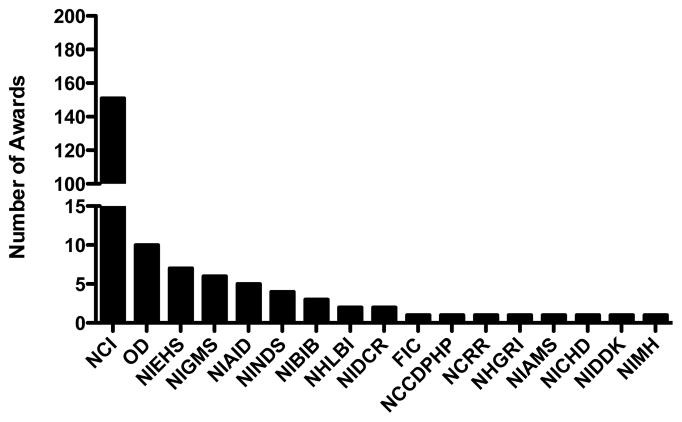
151 (76.7%) grants were awarded by the National Cancer Institute (NCI), 10 (5.1%) by the Office of the Direct (OD), 7 (3.6%) by the National Institute of Environmental Health Sciences (NIEHS), 6 (3%) by the National Institute of General Medical Sciences (NIGMS), 5 (2.5%) by the National Institute of Allergy and Infectious Diseases (NIAID), 4 (2%) by the National Institute of Neurological Disorders and Stroke (NINDS), 3 (1.5%) by the National Institute of Biomedical Imaging and Bioengineering (NIBIB), 2 each (1%) by the National Heart, Lung, and Blood Institute (NHLBI) and the National Institute of Dental and Craniofacial Research (NIDCR), and 1 (0.5%) each by the Fogarty International Center (FIC), the National Center for Chronic Disease Prevention and Health Promotion (NCCDPHP), the National Center for Research Resources (NCRR), the National Human Genome Research Institute (NHGRI), the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), the National Institute of Child Health and Human Development (NICHD), the National Institute of Diabetes and Digestive and Kidney (NIDDK) and the National Institute of Mental Health (NIMH) (Figure 4).
Figure 4.
Distribution of all Awards In Radiation by NIH Institution
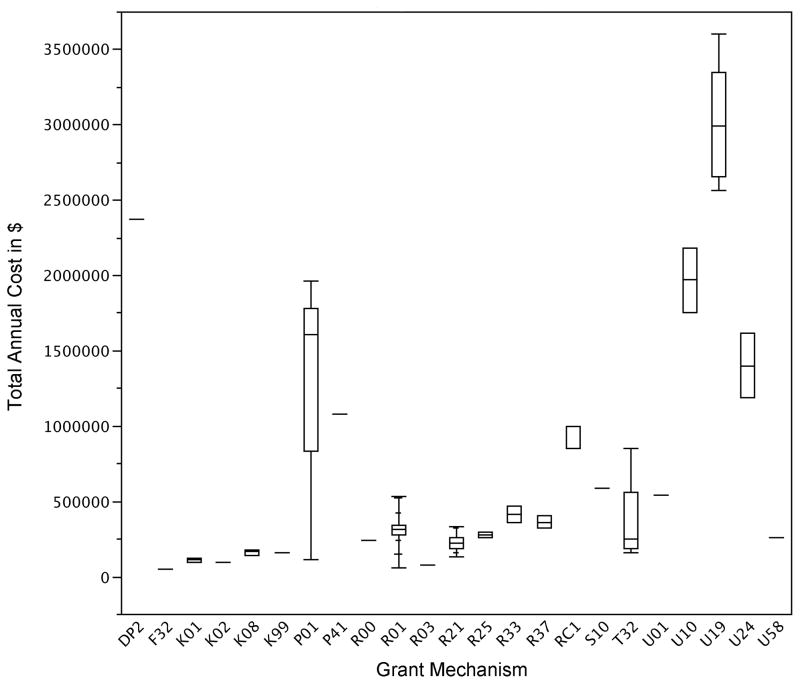
The average award size for R01s was $321,204 (n=127, +/− $282,705 (SD)), for U19s $2,999,389 (n=5, +/− $2,656,449.5 (SD)), for P01s $1,368,512 (n=5, +/− $835,452 (SD)), and $228,744 for R21s (n=26, +/− $188,538 (SD)) (Figure 5).
Figure 5.
Average total annual costs of grants awarded to Radiation Research at the beginning of fiscal year 2013 by award mechanism.
R01 and R21
60 (30.5%) of all grants were awarded through the Radiation Therapeutics and Biology Study Section (RTB) study section. 54 (90%) out of these 60 applications were submitted under the R01 funding mechanism (including one supplement). 74 (37.5%) awards resulted from review through special emphasis panels, out of which 31 (41.9%) where R01 applications. This indicates that at least 33% of all R01 application in Radiation Oncology/Biology/Physics were awarded through study sections other than RTB.
In the RTB Study Section five (9.4%) R01s and one R21 applications were awarded as A1 applications (applications that had been previously reviewed, revised and resubmitted), while 10 (16.1%) of the 62 R01 parent applications awarded through study sections other than RTB were awarded as A1 applications. Only a total of 4 (15.4 %) out of 26 R21 applications were awarded through the RTB study section.
Individual Training Grants
At the time of the analysis one F32, two K01 (Mentored Research Scientist Development Award, NCI participates), one K02 (Independent Scientist Award, NCI does not participate), three K08 (Mentored Clinical Scientist Development Award, NCI participates), one K99 and one R00 were active (Pathway to Independence Award, NCI participates).
Center Grants
We identified one active DP2 award, five P01 grants (four parent grants and 1 supplement), one P41 award, six T32 awards (including 1 supplement), one U01 award, one U10 award, five U19 awards, two U24 awards (including 1 supplement) and one U58 award. The T32 awards covered Cancer Prevention, Postdoctoral Education in Radiation Science, Radiation Biology and Free Radicals, and Radiation Oncology Translational Research.
Discussion
As of December 2012 the Accreditation Council for Graduate Medical Education (ACGME) listed 87 academic programs in Radiation Oncology (2). Academic Radiation Oncology Departments are in general small departments relative to other departments within the medical school with a relatively small body of faculty. However, it was surprising that only 43 (49.4%) of all accredited academic programs in Radiation Oncology have an active research program that is supported by NIH grants, considering that Radiation Oncology academic departments have, for a number of years, attracted the top tier of medical school graduates with the highest percentage of MD/PhDs into its residency programs (3).
A study in 2009 investigating the scholarly productivity of 78 academic programs in Radiation Oncology identified 826 radiation oncology physician-scientists in 2007, not including physicists and basic science researchers (4), and it is likely that this number did increase over the last five years. With 134 PIs including physicians, physicists, and biologists in Radiation Oncology funded by the NIH at the time of the current analysis it appears that only about 1 in 10 of all faculty in academic Radiation Oncology programs currently receives NIH research support. The NIH currently supports investigators with $30.9 billion annually through more than 50,000 grants with an estimated $5.4 billion spent on cancer in FY2013. This suggests that less than 0.3% of NIH-funded principal investigators are working in the field of radiation oncology, and radiation oncology secures only 1.6% of the funding provided for cancer research by the NIH.
Even though there is no clear definition of a critical mass for research groups, it is obvious that very small groups are constantly at risk of losing all NIH support through mobility or retirement of faculty and an increasingly difficult funding environment. In 25 (53.7%) of the institutions, the NIH-funded research program could be considered unstable with only 1 or 2 faculty carrying the program. 11 institutions had 3 or 4 NIH funded investigators, and only 7 institutions had more than 5 NIH funded investigators, with 4 of these programs ranking within the top ten in total funding.
The majority of support from the NIH for radiation research projects was awarded under the R01 funding mechanism. Only 30% of all R01s had been awarded as competitive renewals. Given the current initial administrative cuts to R01s, combined with additional annual reductions and limitation of the annual budget of renewal applications based on the annual budget of the previous award s last year budget, competitive renewal application rates will most likely drop even further, thus jeopardizing the establishment of long-term programs. At the time of the analysis only 26 R21 awards were active. This may be in part due to the fact that until recently the NCI did not offer funding for investigator-initiated projects under this mechanism. Now, with the NCI participating in this program the number of R21s may rise in the near future.
The relatively low number of grants (60) awarded after review by the RTB study section may have several reasons: First, RTB does not exclusively review radiation oncology proposals. Second, radiation oncology is a small field and with the small number of PIs in radiation oncology currently funded by the NIH, conflicts of interest occur frequently and many applications are reviewed by Special Emphasis Panels.
It was concerning to find only 9 active career development awards, 3 of which were K08 (Mentored Clinical Scientist Development Award). Given the consistently top-ranking medical school graduates with advanced degrees in radiation oncology residency programs one would expect that this group would be highly competitive when applying for K08 awards.
The recent addition of Centers for Medical Countermeasures Against Radiation (CMCRs) has boosted radiation research in the U.S. substantially, and has attracted a large number of PIs from outside radiation oncology departments into the field of radiation research. However, continuation of this program is not guarantied and its elimination would have a major negative effect on a field that is ostensibly underfunded.
This study has several limitations. First, the NIH data set is incomplete because some institutions do not list an academic department in their application and those programs were not included in this analysis. However, based on the faculty listed on the web sites of these programs and funding allocated to these PIs in the NIH database, inclusion of these programs would not change the overall picture of the NIH funding landscape in radiation research (Total annual NIH funding for Radiation Oncology Mayo Clinic $721,087, Memorial Sloan Kettering $1,682,565, Harvard University $3,862,981). Second, thematic overlap in radiation physics between Radiation Oncology and Radiology made it hard to register projects to one of the specialties if the home department for Radiation Oncology and Radiology is a center in which both departments are not clearly separated. Third, this study is only a snapshot of NIH funding, which is a moving target and has certain fluctuations during the funding cycles. Fourth, radiation research grants with multiple PIs in which the leading PI does not belong to a Radiology/Radiation Oncology program were not included. Finally, our study did not include other major funding sources like the Department of Defense, NASA, BARDA, DoE, and the NSF. At this point, data from these funding sources is not as easily available as data from the NIH. However, despite the incomplete nature of the available data, our study strongly suggests a dire funding situation for a specialty that treats about 60% of all cancer patients in the United States (5).
Our study indicates an urgent need to separate Radiation Oncology data from Radiology in the NIH database. Adequate reporting, either within the NIH data base or performed by external oversight, should have sufficient granularity and specificity to allow for clarity regarding funds flow and allocation. In addition, this analysis highlights enormous underutilized potential: 1) Physician scientists, are the largest group of academic faculty however, they are underrepresented in the group of NIH-funded PIs in Radiation Oncology. One plausible reason for such a discrepancy might be the allocation of compensation plans which, favor clinical practice over academic accomplishments. This apparent lack of academically active physician scientists raises significant concern regarding translation of basic science results into clinical practice. 2) A large number of programs do not have a critical mass of NIH-funded scientists in their research programs and may not be sustainable in the current and future funding environments. 3) The potential of the many outstanding residents is widely underutilized.
Policies within the specialty of Radiation Oncology, and by the NIH, should address these foundational issues. In the long run, more physician scientists should compete for NIH awards, however they will need to be enabled by new NIH policies promoting clinical translation in radiation oncology. Academic radiation oncology programs should strongly encourage applications for K-type career development awards. However, it must be pointed out that while basic scientists go through years of training that include honing of grant writing skills, medical students and residents in radiation oncology in general lack this experience. Therefore, academic radiation oncology programs should provide appropriate grant writing training and support, as well as mentoring, to allow residents and junior faculty to successfully compete for grant support in a climate of fierce competition.
The overall state of NIH funding in Radiation Oncology raises great concern. Many academic radiation oncology departments have already become “service” departments, where novel research is limited and little, or no translational efforts occur.
A significant number of programs, although currently still funded by the NIH, are at risk of the same fate, unless substantial investment into translational and basic science research occurs within these programs. In order for significant change to take place, funding through federal sources supplemented institutionally and by the private sector, is a necessity. In the future, significant clinical advancement in the field of radiation oncology will likely result from insights gained through basic science research with the potential to be translated to the patient in the clinic in radiation oncology departments with strong clinical translation programs. Radiation oncology must activate the quiescent academic potential of its current and emerging basic and physician scientists or risk the senescence of the field and its relevance to the new cancer treatment strategies of the future.
Summary.
Knowledge of the NIH funding landscape in Radiation Oncology is crucial for academic research programs and for recruitment of faculty. However, this information is not readily available from the NIH because the database does not discriminate between Radiology and Radiation Oncology. This study analyzed NIH funding available to Radiation Oncology Programs at the start of fiscal year 2013.
Acknowledgments
Financial Support: FP was supported by grants from the National Cancer Institute (RO1CA137110, 1R01CA161294) and the Army Medical Research & Material Command’s Breast Cancer Research Program (W81XWH-11-1-0531).
Footnotes
Conflict of Interest: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.(http://projectreporter.nih.gov/reporter.cfm)
- 2.https://www.acgme.org/ads/Public/Reports/ReportRun?CountryId=1&ReportId=1&CurrentYear=2012&SpecialtyId=98&SortId=1
- 3.A National Resident Matching Program, Charting Outcomes in the Match, 2011. National Resident Matching Program; Washington, DC: 2011. [Google Scholar]
- 4.Fuller CD, Choi M, Thomas CR., Jr Bibliometric analysis of radiation oncology departmental scholarly publication productivity at domestic residency training institutions. Journal of the American College of Radiology : JACR. 2009;6:112–118. doi: 10.1016/j.jacr.2008.07.004. [DOI] [PubMed] [Google Scholar]
- 5.https://www.astro.org/News-and-Media/Media-Resources/FAQs/Fast-Facts-About-Radiation-Therapy/Index.aspx