Abstract
OBJECTIVE
The objective of our study was to assess the experiences and preferences of radiology residents with respect to breast imaging.
MATERIALS AND METHODS
We surveyed radiology residents at 26 programs in New York and New Jersey. Survey topics included plans for subspecialty training, beliefs, and attitudes toward breast imaging and breast cancer screening and the likelihood of interpreting mammography in the future.
RESULTS
Three hundred forty-four residents completed the survey (response rate, 62%). The length of time spent training in breast imaging varied from no dedicated time (37%) to 1–8 weeks (40%) to more than 9 weeks (23%). Most respondents (97%) agreed that mammography is important to women’s health. More than 85% of residents believed that mammography should be interpreted by breast imaging specialists. Respondents shared negative views about mammography, agreeing with statements that the field was associated with a high risk of malpractice (99%), stress (94%), and low reimbursement (68%). Respondents endorsed several positive attributes of mammography, including job availability (97%), flexible work schedules (94%), and few calls or emergencies (93%). Most radiology residents (93%) said that they were likely to pursue subspecialty training, and 7% expressed interest in breast imaging fellowships.
CONCLUSION
Radiology residents’ negative and positive views about mammography seem to be independent of time spent training in mammography and of future plans to pursue fellowship training in breast imaging. Systematic assessment of the plans and preferences of radiology residents can facilitate the development of strategies to attract trainees to careers in breast imaging.
Keywords: breast cancer screening, breast imaging, education, mammography, screening mammography, workforce
Mammography is a central component of breast cancer screening, diagnosis, staging, and surveillance and is credited with improving mortality from breast cancer in the United States [1, 2]. Screening mammography has been shown to reduce mortality from breast cancer by 20–35% in women 50–69 years old and approximately 20% in women 40–49 years old [3, 4]. Current guidelines from the American Cancer Society recommend annual screening for women 40 years old and older [5]. Estimates suggest that an additional 1.2 million women become eligible for screening mammography each year in the United States [6].
The rate of screening mammography steadily increased for more than a decade and, in 2000, achieved the Healthy People 2010 goal of 70% of women reporting a screening mammogram within the preceding 2 years [7]. However, two recent national surveys report that this trend might be changing. The National Health Interview Survey (NHIS) found a decrease from 70% in 2000 to 66% in 2005 of women 40 years old and older who reported a recent mammogram, and the Behavioral Risk Factor Surveillance System (BRFSS) found a drop from 76.4% to 74.6% in the same time period [8]. Both changes, although small, represented statistically significant declines in the use of screening mammography.
The Institute of Medicine and the Society of Breast Imaging have independently reported that a shortage of radiologists qualified to interpret mammography threatens access to this life-saving screening technique [9, 10]. Although leaders in the field are looking to graduating residents and breast imaging fellows to help address this manpower shortage, prior surveys of radiology residents have found a lack of interest in pursuing fellowships or employment in this subspecialty [11, 12]. Our recent survey of breast, women’s, and breast and body fellowship programs nationwide suggested a possible resurgence of interest in breast imaging [13]. The objective of the current study was to assess the experiences and preferences of radiology residents with respect to breast imaging and future work plans.
Materials and Methods
Study Participants
Between November 2007 and March 2008 we invited all radiology residency programs in the states of New York and New Jersey to participate in our study. The programs were identified using the American Medical Association’s online listing of residency programs, the Fellowship and Residency Electronic Interactive Database (FREIDA). Directors or chief residents from 26 of the 35 residency programs, including 22 of the 27 programs in New York and four of the eight programs in New Jersey, agreed to allow their residents to participate in the study. The self-administered, paper-based survey was completed by residents present during a scheduled visit at 21 of the programs. Residents in the remaining five programs returned completed surveys by mail or email. Residents at all levels of radiology training were included from postgraduate year (PGY) 2 through PGY 5. The participating programs included a total of 553 (83%) of the 669 radiology residents training in the academic year 2007–2008 in the two states.
A cover letter accompanying the survey explained the purpose of the study. Participants were assured confidentiality of their individual responses and no personal identifying information was collected. Completion of the survey was considered consent to participate. The institutional review board at Memorial Sloan-Kettering Cancer Center reviewed the survey and cover letter before distribution.
Survey Instrument
The survey instrument addressed three domains: experiences during radiology residency, future career plans, and opinions regarding mammography. Items regarding residency experiences included current year of training, program size, breast imaging techniques available, and amount of time spent training in each breast imaging technique. In addition, residents were asked if they had identified a mentor and, if so, in which subspecialty of radiology. Residents were also asked whether they felt prepared to read mammograms independently.
Items regarding future work plans included questions about the likelihood of pursuing fellowship training after residency, future subspecialization, desire to work part-time, plans for working in academia, and interest in interpreting mammograms in the future.
Attitudes and opinions regarding mammography were assessed by asking residents their level of agreement with a series of statements, using a 6-point Likert scale ranging from “strongly agree” to “strongly disagree,” requiring residents to have a weighted opinion in either direction. Using the same response scale, residents were asked to rank their attitudes regarding the role of mammography in women’s health and the role of breast imaging specialists in interpreting mammography. For the purposes of data analysis and reporting, the Likert scale was collapsed into three categories: agree, disagree, and no response. We also collected basic demographic information about respondents including age, sex, marital status, location of medical school, and preferred location of future practice.
Statistical Analysis
We used descriptive statistics to characterize the survey sample and their responses. Chi-square tests were used to evaluate associations between resident characteristics and their survey responses, including future work plans and opinions and attitudes toward mammography. All analyses were performed using SAS software (version 9.1, SAS Institute).
Results
Resident and Program Characteristics
A total of 35 radiology residency programs were identified in New York and New Jersey. The 26 programs that participated in the study varied in size from eight to 40 residents, with an average of 20 residents. The programs that did not participate were somewhat smaller than those that did. Of the five residency programs at institutions that also offered fellowship-level training in women’s imaging, breast and body imaging, or breast imaging, all participated in the resident survey.
The 26 participating programs had a total of 553 residents, of whom 344 completed the survey (response rate, 62%). The respondents were distributed equally across years of training: 95 (28%) PGY 2, 79 (23%) PGY 3, 83 (24%) PGY 4, and 87 (25%) PGY 5. Approximately two thirds of participating residents were male (Table 1). Of the 344 residents surveyed, 137 (39.8%) had identified a mentor at the time of the survey.
TABLE 1.
Resident Characteristics
| Resident Characteristics | No. (%) of Residents (n =344) |
|---|---|
| Year of radiology residency | |
| First (PGY 2) | 95 (27.6) |
| Second (PGY 3) | 79 (23.0) |
| Third (PGY 4) | 83 (24.1) |
| Fourth (PGY 5) | 87 (25.3) |
| Time spent in breast imaging | |
| None yet | 127 (36.9) |
| 1–4 wk | 83 (24.1) |
| 5–8 wk | 55 (16.0) |
| 9–12 wk | 51 (14.8) |
| > 12 wk | 28 (8.1) |
| Age (y) | |
| 25–29 | 147 (42.7) |
| 30–34 | 174 (50.6) |
| 35–39 | 19 (5.5) |
| ≥ 40 | 2 (0.6) |
| No response | 2 (0.6) |
| Sex | |
| Male | 223 (64.8) |
| Female | 121 (35.2) |
| Plans to pursue a fellowship | |
| Very likely or somewhat likely | 320 (93.0) |
| Unlikely | 12 (3.5) |
| Somewhat unlikely or not at all likely | 12 (3.5) |
| Selected subspecialty | |
| Neuroradiology | 56 (16.3) |
| Musculoskeletal | 36 (10.5) |
| Interventional radiology | 36 (10.5) |
| Body | 31 (9.0) |
| Other | 31 (9.0) |
| Breast/breast-body/women’s | 24 (7.0) |
| Undecided/no answer | 130 (37.8) |
Note—PGY = postgraduate year.
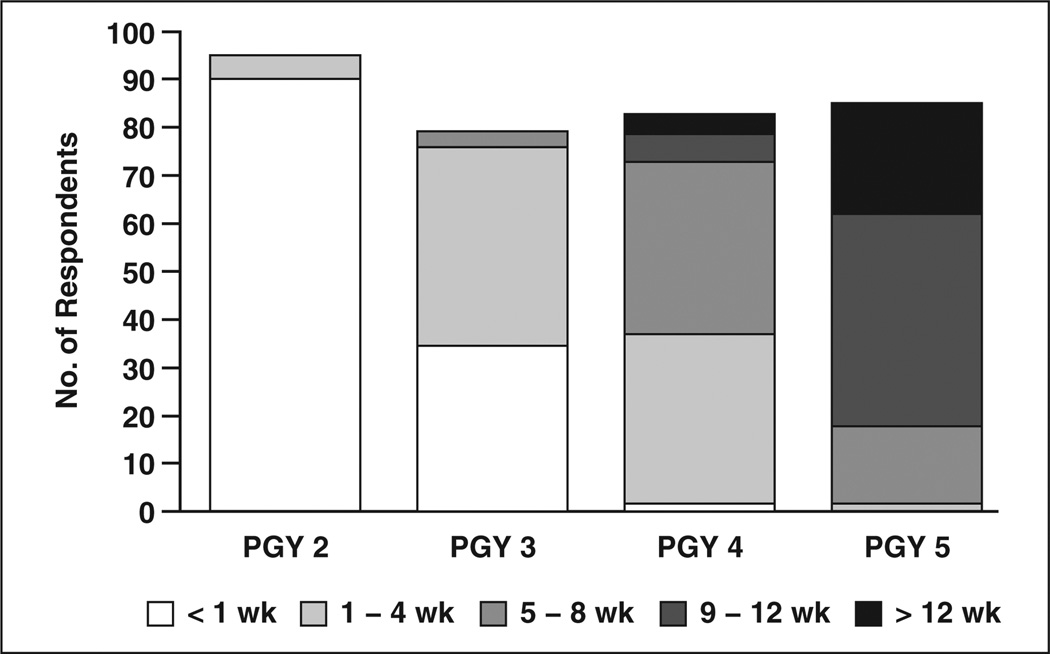
According to the survey respondents, all programs offered training in mammography, breast ultrasound, and breast MRI. Residents reported spending various amounts of dedicated time in breast imaging at the time of the survey (Fig. 1). At the time of the survey, 95% of PGY 2 residents and 35% of PGY 3 residents had spent no time in breast imaging. Of the 87 PGY 5 residents who participated in the survey, 36 (41%) felt prepared to read mammography independently. Of the 28 residents who had completed the 12 weeks of mammography training required by the Mammography Quality Standards Act, half felt prepared to interpret mammograms on their own.
Fig. 1.
Bar graph shows amount of time respondents to survey had spent in breast imaging at the time of the study. PGY = postgraduate year.
Future Work Plans
Nearly all residents surveyed (93%) said they were likely to pursue fellowship training after residency, and more than half identified a subspecialty field of interest (Table 1). Of the 214 residents who identified a preferred subspecialty, 147 (69%) were male and 67 (31%) were female. Male residents make up the majority of residents choosing fellowship in interventional radiology (92%), neuroradiology (84%), musculoskeletal imaging (69%), and body imaging (68%). This gender difference is greater than would be expected due to representation in residency alone (p < 0.0001). Of the 24 residents who identified breast imaging, women’s imaging, or breast and body imaging as their preferred fellowship, 23 (96%) were female. In this survey, female residents were 42 times more likely to choose a breast imaging fellowship than male residents.
Among all residents, one third were likely, one third were unlikely, and one third said they were uncertain about reading mammography as part of their future practice. With respect to practice setting, 104 residents (30%) said that they were somewhat likely or very likely to remain in an academic environment. Of the 24 residents who reported interest in breast imaging as a subspecialty, none said that they were very likely to remain in academics, five (21%) were somewhat likely, seven (29%) were unlikely, and 12 (50%) were uncertain. Eight residents had identified a mentor in breast imaging, and all of these residents planned to pursue a fellowship in breast imaging. When asked to identify a preferred region of the United States for practice after completion of training, the most frequently selected regions were the mid-Atlantic region, which includes New York and New Jersey, followed by the West and then New England (Table 2). Those interested in fellowships in breast imaging most commonly indicated a preference for the mid-Atlantic region.
TABLE 2.
Where Residents Plan to Work in the Future
| U.S. Census Region | No. of Respondents | |
|---|---|---|
| All Residents Surveyed | Residents Interested in Breast Imaging, Women’s Imaging, or Breast and Body Imaging Fellowships |
|
| New England | 105 | 5 |
| Mid-Atlantic | 193 | 16 |
| East North Central | 18 | 0 |
| West North Central | 3 | 0 |
| South Atlantic | 58 | 2 |
| East South Central | 5 | 1 |
| West South Central | 21 | 3 |
| Mountain | 23 | 3 |
| West | 107 | 3 |
| Territory | 1 | 0 |
Note—Respondents were asked to select all preferred regions
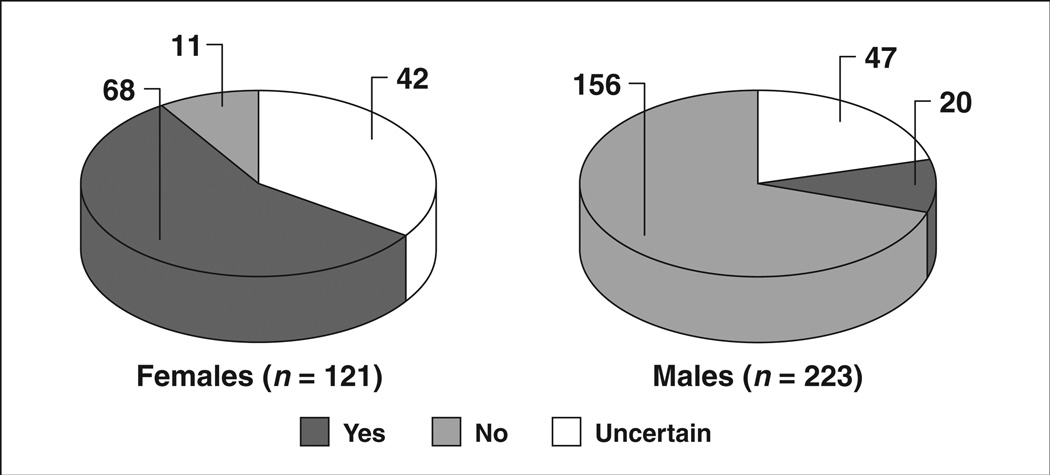
Of the full sample, 88 residents (26%) said they planned to work part-time at some point in the next 10 years. Responses to this question varied by gender, with more than half of the female residents planning to work part-time at some point (Fig. 2). Of the 24 residents expressing interest in breast imaging, 14 planned to work part-time at some point, eight were uncertain and two did not plan to work part-time at any point in the future. Or, alternatively, 16% of residents planning on working part-time chose breast imaging as their fellowship choice compared with 9% of residents who are uncertain about working part-time and only 1% of residents who have no plan to work part-time in the future.
Fig. 2.
Pie chart shows plans to work part-time by gender at time of study.
Residents in PGY 4 of training were more likely to choose breast imaging as a subspecialty (14%) than residents in the other 3 years of training: PGY 3 (6%), PGY 5 (6%), and PGY 2 (2%). Residents who had spent any amount of time in breast imaging training were more likely to choose a subspecialty in breast imaging (9%) than residents who had no experience in breast imaging (4%).
Opinions and Attitudes Toward Mammography
Independent of future work plans or time spent in breast imaging during residency, residents shared many attitudes and preferences regarding mammography. Overwhelmingly, residents thought that mammography is an important element of women’s health, with 97.4% expressing agreement with this statement (p < 0.0001) (Table 3). A majority of residents (69.5%) believed that mammography should be interpreted by radiologists specializing in breast imaging (p < 0.0001). They agreed almost unanimously (96.8%) that interpreting mammography has a high risk of malpractice (p < 0.0001). There was also a high level of agreement regarding stress caused by reading mammograms, as well as low reimbursement for mammography interpretation and a lack of interest in the field. There was a high level of agreement regarding positive lifestyle elements of a career in breast imaging. Residents believed that there was good job availability in the field of mammography, a potentially flexible work schedule, and few calls or emergencies (p < 0.0001).
TABLE 3.
Opinions and Attitudes by Future Work Plans
| No. (%) of Respondents | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| All Residents Surveyed (n = 344) | Residents Likely to Read Mammography in the Future (n = 110) |
Residents Interested in Breast Imaging, Women’s Imaging, or Breast and Body Imaging Fellowship (n = 24) |
|||||||
| Statement | Agree | Disagree | Did Not Respond |
Agree | Disagree | Did Not Respond |
Agree | Disagree | Did Not Respond |
| Mammography is an interesting field. | 94 (27.3) | 250 (72.7) | 0 (0.0) | 54 (49.1) | 56 (50.9) | 0 (0.0) | 21 (87.5) | 3 (12.5) | 0 (0.0) |
| There are many jobs available in mammography. | 313 (91.0) | 18 (5.2) | 13 (3.8) | 100 (90.9) | 8 (7.3) | 2 (1.8) | 22 (91.7) | 2 (8.3) | 0 (0.0) |
| Mammography is an attractive subspecialty because there are few calls or emergencies. | 279 (81.1) | 61 (17.7) | 4 (1.2) | 100 (90.9) | 10 (9.1) | 0 (0.0) | 23 (95.8) | 1 (4.2) | 0 (0.0) |
| Emergence of new technology (e.g., MRI, CT) makes breast imaging more interesting. | 302 (87.8) | 7 (2.0) | 35 (10.2) | 105 (95.5) | 5 (4.5) | 0 (0.0) | 24 (100.0) | 0 (0.0) | 0 (0.0) |
| Mammography is a very important element of women’s health. | 335 (97.34) | 5 (1.5) | 1 (0.3) | 107 (97.3) | 3 (2.7) | 0 (0.0) | 24 (100.0) | 0 (0.0) | 0 (0.0) |
| Mammography is an attractive subspecialty because it offers a flexible work schedule. | 289 (84.0) | 49 (14.2) | 6 (1.7) | 98 (89.1) | 11 (10.0) | 1 (0.9) | 23 (95.8) | 1 (4.2) | 0 (0.0) |
| Mammography is a screening modality that should be offered to all women age 40 and older. | 333 (96.8) | 7 (2.0) | 4 (1.2) | 106 (96.4) | 3 (2.7) | 1 (0.9) | 24 (100.0) | 0 (0.0) | 0 (0.0) |
| Mammography is a female-dominated subspecialty of radiology. | 258 (75.0) | 80 (23.3) | 6 (1.7) | 81 (73.6) | 28 (25.5) | 1 (0.9) | 22 (91.7) | 2 (8.3) | 0 (0.0) |
| Mammography should be interpreted only by radiologists who have completed a breast or women’s imaging fellowship. | 239 (69.5) | 101 (29.4) | 4 (1.2) | 76 (69.1) | 33 (30.0) | 1 (0.9) | 20 (83.3) | 4 (16.7) | 0 (0.0) |
| Reading mammograms is stressful. | 261 (75.9) | 74 (21.5) | 9 (2.6) | 76 (69.1) | 30 (27.3) | 4 (3.6) | 13 (54.2) | 10 (41.7) | 1 (4.2) |
| The reimbursement rate for reading mammography is too low. | 245 (71.2) | 71 (20.6) | 28 (8.1) | 79 (71.8) | 22 (20.0) | 9 (8.2) | 20 (83.3) | 3 (12.5) | 1 (4.2) |
| The risk of malpractice in mammography is high. | 333 (96.8) | 4 (1.2) | 7 (2.0) | 102 (92.7) | 2 (1.8) | 6 (5.5) | 24 (100.0) | 0 (0.0) | 0 (0.0) |
The opinions of residents who planned to pursue a fellowship in breast imaging were consistent with the attitudes and opinions expressed by all respondents with a few exceptions. First, there was a trend for greater agreement with positive lifestyle factors associated with reading mammography, including a flexible work schedule, low call burden, and interest generated by emerging technology. Although 88% of residents planning to pursue fellowship training in breast imaging agreed that mammography is an interesting field, only 17% of residents who did not plan to interpret mammography as part of their future practice shared that view. Also, whereas 54% of the residents interested in a breast imaging fellowship agreed that reading mammograms is stressful, 73% of residents who planned to read mammograms but did not plan to pursue a fellowship in the field shared that view.
Discussion
For reasons including concern about malpractice litigation, job-related stress, and low reimbursement, the number of radiologists choosing to interpret mammography is declining [10]. In our survey of more than 300 radiology residents in two large states, we found that residents at all levels of training shared these views regarding mammography. Surprisingly, residents who hoped to pursue subspecialty training in breast imaging held these views as well; for them, the lifestyle benefits and importance of mammography to women’s health may have outweighed the perceived negative aspects of a career in breast imaging.
Our survey captured the experiences and preferences of radiology residents at all levels of training. The high level of agreement we observed in opinions and attitudes regarding mammography is consistent with prior surveys of third- and fourth-year radiology residents [11, 12]. Although beliefs and attitudes toward breast imaging among our survey respondents did not vary with length of exposure to the field, interest in a breast imaging fellowship was more likely among residents who had spent more time training in breast imaging as part of their general radiology residency program. One of the potential avenues to increase interest in careers in breast imaging, then, may involve offering rotations in breast imaging earlier in training. Our findings suggest that most residents do not get exposure to breast imaging until their second year of radiology training, if not later.
The need to recruit mammography specialists to academic practice is especially critical because these radiologists will train subsequent generations of specialists. They are also the individuals most likely to attract young residents to the field through clinical exposure, research opportunities, and mentorship [14]. More than half of the residents in our survey had not yet identified a mentor in any subspecialty of radiology. One third of residents interested in breast imaging fellowship had a mentor in breast imaging at the time of the survey, suggesting that faculty commitment to mentoring may nurture further interest in the field among residents. Incentives targeted to academic settings, such as part-time opportunities, flexible schedules, or improved workload, might also enhance this vital segment of the mammography workforce [15].
Over the past decade, mammography has been identified as the subspecialty of radiology with the highest growth rate of job vacancies [16, 17]. Nearly 30% of radiology practices surveyed in 2002, in both academic and community settings, reported at least one opening for a mammographer, and 10% reported more than one opening [9]. In a separate survey of community-based radiology practices, 44% of mammography facilities reported a shortage of radiologists relative to their mammographic volume [18].
Alleviating the mammography workforce shortage will require efforts on several fronts. In addition to stimulating interest among radiology residents, concerns about malpractice and reimbursement must be addressed. Currently, misinterpretation of mammography with a missed diagnosis of breast cancer is the most common medical malpractice complaint and second most expensive type of malpractice suit in the United States [19]. Even though the perceived risk of a malpractice claim is higher than the actual risk, it remains a deterrent to radiologists who might otherwise read mammograms [20]. In a survey conducted by the American College of Radiology (ACR), 14% of radiologists reported that they had stopped performing certain studies, particularly mammography, because of concerns about malpractice [21]. However, there was no increased concern about the medicolegal climate among mammographers compared with radiologists in other subspecialties [21].
Another factor influencing the mammography workforce is financial pressure from historically low reimbursement rates and the rising cost of malpractice insurance [22]. Reimbursement for mammography varies by indication, either screening or diagnostic. The ACR defines screening mammography as a radiologic examination performed to detect unsuspected breast cancer in asymptomatic women, whereas a diagnostic mammogram is a problem-solving breast evaluation indicated to follow up an abnormality or physical examination finding. Diagnostic mammography involves more focused imaging with more views and thus requires more time for evaluation than screening mammography. An analysis of seven university-based programs found that, on average, institutions incur losses by providing mammography services. Whereas screening mammography can be profitable, diagnostic mammography and breast ultrasound studies are generally not profitable [22]. Increasing reimbursement rates and achieving malpractice reform may help attract trainees to a career in breast imaging and improve the financial viability of practices.
Consistent with prior studies of both trainees and practicing radiologists, most residents in our survey stated that reading mammography was stressful [10, 11]. Although we did not include open-ended questions to identify specific sources of stress, it is possible that concerns over malpractice and reimbursement are contributing factors. We also did not ask residents about stress associated with other imaging techniques for the purpose of comparison. Further research is needed to better elucidate the causes and potential remedies for this negative emotion associated with interpreting mammography.
Responses to our survey highlighted the interest in breast imaging among female radiology residents. This reflects the current workforce, where women are more concentrated in breast imaging than men [23]. Women make up a growing percentage of the radiology workforce in the United States, 18% in 2003 versus 13% in 1990 [23], and there is a concerted effort to ensure that female medical students continue to consider careers in radiology by emphasizing the positive lifestyle associated with the field including predictable and controllable working hours [15, 24].
We found substantial agreement among all residents regarding the positive lifestyle aspects of a career in breast imaging, which typically involves few calls and emergencies. As such, mammography might be an ideal field for radiologists interested in working part-time. Although only a quarter of all residents we surveyed thought they might work part-time in the future, 56% of all female residents and 58% of those who hoped to pursue a subspecialty in breast imaging (all but one of whom were female) planned to work part-time at some point in the next 10 years. Thus, emphasizing the lifestyle benefits of a career in breast imaging, including the predictable and potentially flexible schedule, might draw more radiology residents to this subspecialty.
Our survey confirms prior findings that most radiology residents are interested in pursuing some type of subspecialization [25]. Fellowship-level training in mammography is provided through breast imaging, breast and body imaging, and women’s imaging fellowships that, traditionally, have not had great success in filling positions on a national scale [26]. However, the number of breast imaging fellowship programs and individual fellowship positions offered nationwide is growing [13]. Furthermore, compared with prior surveys of radiology residents, we found a greater proportion of residents interested in pursuing breast imaging fellowships [11, 12]. The increased interest among radiology residents suggests a favorable trend for the breast imaging workforce, but may not suffice to alleviate current and predicted manpower shortages in mammography.
The residents we surveyed generally agreed that mammography should be interpreted by radiologists with specialty training in this area. The trend of breast imaging specialists interpreting mammography will likely grow as the radiology workforce continues to subspecialize [27]. As a result, fewer radiologists will be reading a greater share of mammograms each year, potentially resulting in the improved accuracy associated with higher volume [28]. However, a greater burden is placed on ensuring adequate manpower in the field, further highlighting the need to recruit trainees to the field of breast imaging [29].
Several limitations of our study must be noted. Our sample was limited to radiology residents at participating programs in New York and New Jersey, and it is not clear whether their experiences, opinions, and future work plans generalize to trainees at programs that declined to participate or to programs in other states. Also, all items were self-reported by residents; we could not verify specific aspects of their training, such as components of the curriculum or number of weeks spent in breast imaging. We did not collect information regarding the faculty dedicated to breast imaging at each program, which might influence residents’ experiences during training. Finally, our study offers a cross-sectional view at a single point in time. Longitudinal studies may provide additional insights regarding the concordance between residents’ plans and their eventual choices, as well as trends over time in the experiences and attitudes of radiology residents regarding mammography.
The demand for screening mammography will continue to grow with an aging population in this country. Any assessment of manpower needs in breast imaging should include radiology residents because they are an important element of the future workforce. National surveys may further elicit specific aspects of breast imaging that may be particularly powerful in attracting both trainees and educators to this field, thereby ensuring continued access to mammography for women in the United States.
References
- 1.Shapiro S, Venet W, Strax P, Venet L, Roeser R. Ten- to fourteen-year effect of screening on breast cancer mortality. J Natl Cancer Inst. 1982;69:349–355. [PubMed] [Google Scholar]
- 2.Tabár L, Fragerberg CJ, Gad A, et al. Reduction in mortality from breast cancer after mass screening with mammography: randomised trial from the Breast Cancer Screening Working Group of the Swedish National Board of Health and Welfare. Lancet. 1985;1:829–832. doi: 10.1016/s0140-6736(85)92204-4. [DOI] [PubMed] [Google Scholar]
- 3.Fletcher SW, Elmore JG. Clinical practice: mammographic screening for breast cancer. N Engl J Med. 2003;348:1672–1680. doi: 10.1056/NEJMcp021804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Elmore JG, Armstrong K, Lehman CD, Fletcher SW. Screening for breast cancer. JAMA. 2005;293:1245–1256. doi: 10.1001/jama.293.10.1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Summaries for patients: screening for breast cancer—recommendations from the U.S. Preventive Services Task Force. Ann Intern Med. 2002;137(5 Part 1):I47. doi: 10.7326/0003-4819-137-5_part_1-200209030-00004. [No authors listed] [DOI] [PubMed] [Google Scholar]
- 6.Meyer J. Age: Census 2000 brief. Washington, DC: U.S. Census Bureau; 2001. C2KBR/01-12. [Google Scholar]
- 7.Swan J, Breen N, Coates RJ, Rimer BK, Lee NC. Progress in cancer screening practices in the United States: results from the 2000 National Health Interview Survey. Cancer. 2003;97:1528–1540. doi: 10.1002/cncr.11208. [DOI] [PubMed] [Google Scholar]
- 8.Breen N, Cronin AK, Meissner HI, et al. Reported drop in mammography: is this cause for concern? Cancer. 2007;109:2405–2409. doi: 10.1002/cncr.22723. [DOI] [PubMed] [Google Scholar]
- 9.Farria DM, Schmidt ME, Monsees BS, et al. Professional and economic factors affecting access to mammography: a crisis today, or tomorrow? Results from a national survey. Cancer. 2005;104:491–498. doi: 10.1002/cncr.21304. [DOI] [PubMed] [Google Scholar]
- 10.Joy JE, Penhoet EE, Petitti DB, editors. Strategies for improving breast cancer detection and diagnosis. Washington, DC: National Academies Press; 2000. Committee on New Approaches to Early Detection and Diagnosis of Breast Cancer; Institute of Medicine and National Research Council of the National Academies. [Google Scholar]
- 11.Bassett LW, Monsees BS, Smith RA, et al. Survey of radiology residents: breast imaging training and attitudes. Radiology. 2003;227:862–869. doi: 10.1148/radiol.2273020046. [DOI] [PubMed] [Google Scholar]
- 12.Hardy SM, Kornguth PJ, Baum JK. Massachusetts radiology resident attitudes toward mammography. J Am Coll Radiol. 2005;2:432–435. doi: 10.1016/j.jacr.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 13.Baxi SS, Liberman L, Lee C, Elkin EB. Breast imaging fellowships in the United States: who, what, and where? AJR. 2009;192:403–407. doi: 10.2214/AJR.08.1571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mainiero MB. Mentoring radiology residents: why, who, when, and how. J Am Coll Radiol. 2007;4:547–550. doi: 10.1016/j.jacr.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 15.Beyond bias and barriers: fulfilling the potential of women in academic science and engineering. Washington, DC: National Academies Press; 2007. Committee on Maximizing the Potential of Women in Academic Science and Engineering, National Academy of Sciences, National Academy of Sciences, Institute of Medicine. 2006. [PubMed] [Google Scholar]
- 16.Sunshine JH, Maynard CD. Update on the diagnostic radiology employment market: findings through 2006–2007. J Am Coll Radiol. 2007;4:686–690. doi: 10.1016/j.jacr.2007.06.015. [DOI] [PubMed] [Google Scholar]
- 17.Sunshine JH, Maynard CD. Update on the diagnostic radiology employment market: findings through 2007–2008. J Am Coll Radiol. 2008;5:827–833. doi: 10.1016/j.jacr.2008.02.007. [DOI] [PubMed] [Google Scholar]
- 18.D’Orsi C, Tu SP, Nakano C, et al. Current realities of delivering mammography services in the community: do challenges with staffing and scheduling exist? Radiology. 2005;235:391–395. doi: 10.1148/radiol.2352040132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Physician Insurers Association of America. Physician Insurers Association of America (PIAA) study: 2002 study. Rockville, MD: Physician Insurers Association of America, Spring; 2002. [Google Scholar]
- 20.Elmore JG, Taplin SH, Barlow WE, et al. Does litigation influence medical practice? The influence of community radiologists’ medical malpractice perceptions and experience on screening mammography. Radiology. 2005;236:37–46. doi: 10.1148/radiol.2361040512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cypel YS, Sunshine JH, Ellenbogen PH. The current medical liability insurance crisis: detailed findings from two ACR surveys in 2003 and 2004. J Am Coll Radiol. 2005;2:595–601. doi: 10.1016/j.jacr.2005.01.012. [DOI] [PubMed] [Google Scholar]
- 22.Enzmann DR, Anglada PM, Haviley C, Venta LA. Providing professional mammography services: financial analysis. Radiology. 2001;219:467–473. doi: 10.1148/radiology.219.2.r01ma18467. [DOI] [PubMed] [Google Scholar]
- 23.Lewis RS, Bhargavan M, Sunshine JH. Women radiologists in the United States: results from the American College of Radiology’s 2003 survey. Radiology. 2007;242:802–810. doi: 10.1148/radiol.2423060282. [DOI] [PubMed] [Google Scholar]
- 24.Fielding JR, Major MN, Mullan BF, et al. Choosing a specialty in medicine: female medical students and radiology. AJR. 2007;188:897–900. doi: 10.2214/AJR.06.0539. [DOI] [PubMed] [Google Scholar]
- 25.Shetty SK, Venkatesan AM, Foster KM, Galdino GM, Lawrimore TM, Davila JA. The radiology class of 2005: postresidency plans. J Am Coll Radiol. 2005;2:852–858. doi: 10.1016/j.jacr.2005.03.011. [DOI] [PubMed] [Google Scholar]
- 26.Bassett LW, Lubisich JP, Bresch JP, Jessop NW, Hendrick RE. Quality assurance in mammography: status of residency education. AJR. 1993;160:271–274. doi: 10.2214/ajr.160.2.8424332. [DOI] [PubMed] [Google Scholar]
- 27.Lewis RS, Sunshine JH, Bhargavan M. A portrait of breast imaging specialists and of the interpretation of mammography in the United States. AJR. 2006;187:1167. doi: 10.2214/AJR.05.1858. [web]:W456–W468. [DOI] [PubMed] [Google Scholar]
- 28.Esserman L, Cowley H, Eberle C, et al. Improving the accuracy of mammography: volume and outcome relationships. J Natl Cancer Inst. 2002;94:369–375. doi: 10.1093/jnci/94.5.369. [DOI] [PubMed] [Google Scholar]
- 29.Smith-Bindman R, Miglioretti DL, Rosenberg R, et al. the National Institutes of Health Breast Cancer Surveillance Consortium. Physician workload in mammography. AJR. 2008;190:526–532. doi: 10.2214/AJR.07.2500. [DOI] [PubMed] [Google Scholar]