Abstract
Background
Screening mammography rates vary geographically and have recently declined. Inadequate mammography resources in some areas may impair access to this technology. We assessed the relationship between availability of mammography machines and the use of screening.
Methods
The location and number of all mammography machines in the US were identified from US Food and Drug Administration records of certified facilities. Inadequate capacity was defined as <1.2 mammography machines per 10,000 women aged 40 or older, the threshold required to meet the Healthy People 2010 target screening rate. The impact of capacity on utilization was evaluated in two cohorts: female respondents age 40 or older to the 2006 Behavioral Risk Factor Surveillance System survey (BRFSS) and a 5% nationwide sample of female Medicare beneficiaries age 65 or older in 2004–2005.
Results
About 9% of women in the BRFSS cohort and 13% of women in the Medicare cohort lived in counties with <1.2 mammography machines per 10,000 women age 40 or older. In both cohorts, residence in a county with inadequate mammography capacity was associated with lower odds of a recent mammogram (adjusted odds ratio [AOR] in BRFSS: 0.89, 95% CI 0.80 – 0.98, p<0.05; AOR in Medicare: 0.86, 95% CI 0.85 – 0.87, p<0.05), controlling for demographic and health care characteristics.
Conclusion
In counties with few or no mammography machines, limited availability of imaging resources may be a barrier to screening. Efforts to increase the number of machines in low-capacity areas may improve mammography rates and reduce geographic disparities in breast cancer screening.
BACKGROUND
In multiple randomized controlled trials, screening mammography has been shown to reduce breast cancer mortality, particularly among women age 50 to 69.(1, 2) Despite the well publicized benefits of screening mammography and recommendations for population-based screening, (3, 4) about one-third of US women age 40 and older report having no recent mammogram and this proportion varies widely by state.(5) After increasing for 25 years, rates of screening mammography now appear to be declining. From 2000 to 2005, two national surveys found a significant decrease in the percentage of women age 40 and older who reported having a mammogram in the past two years. (6, 7) In addition, about 20% of women with a history of breast cancer do not adhere with guidelines for follow-up mammography.(8–10)
Access to mammography has been a particular concern in the US since the passage of the Mammography Quality Standards Act (MQSA) which established national uniform quality standards for this imaging modality. The law requires certification of mammography facilities by the US Food and Drug Administration (FDA) which enforces the MQSA and can revoke certification from noncompliant facilities.(11) The MQSA has been credited with improvements in mammography quality, but its impact on access is uncertain.(12, 13) Federal reports suggest that overall mammography capacity is sufficient to meet existing needs,(14, 15) but it is not clear whether resources are distributed proportionally to the population. Notably, facility closures in the 1990s may have disproportionately affected areas with substantial minority or rural populations.(16, 17)
Given recent declines and geographic disparities in screening mammography, as well as financial pressures facing many facilities,(18) it is now especially critical to understand how the availability and accessibility of mammography resources affect the use of screening. Our objective was to assess whether the geographic availability of mammography machines influences the use of screening mammography.
METHODS
This study was reviewed and approved by the Institutional Review Board at Memorial Sloan-Kettering Cancer Center.
Mammography capacity
Information on the number, location and characteristics of mammography facilities in 2004 was obtained from the FDA. In accordance with the MQSA, the FDA has maintained administrative records on all certified mammography facilities in the US since 1994. Facilities are inspected annually, and data from inspection reports include the number of mammography machines. All facilities were georeferenced by street address using ArcGIS software (Version 9.2, ESRI, Redlands, California). Mobile mammography facilities were assigned to the county of their mailing address.
For every county in the US (n=3,140), we estimated mammography capacity as the number of mammography machines per 10,000 women age 40 years or older in 2004. Women in this age group constitute the population eligible for annual screening mammography.(4) Mammography capacity in 2004 included only machines at facilities whose FDA certification was effective for the entire calendar year. Age-specific counts of the female population in each county in 2004 were obtained from postcensal population estimates produced by the US Census Bureau.
We hypothesized that women who resided in counties with inadequate mammography capacity would be less likely than other women to have received a recent mammogram. To examine this hypothesis, we defined inadequate capacity as the estimated number of machines needed to reach the Healthy People 2010 goal of a 70% screening rate,(19) a level similar to the current ambient screening rate in the US. We derived this threshold using information from the U.S. Government Accountability Office (GAO), which estimated that an average mammography machine can perform a total of 6,000 mammograms per year, assuming that a single machine can perform 3 mammograms per hour, 8 hours per day, 5 days per week for 50 weeks per year.(14) This implies that a capacity of about 1.7 machines per 10,000 women age 40 or older would be sufficient to screen all eligible women in a county (i.e., 100% screening rate), ignoring the use of resources for diagnostic mammography. Multiplying 1.7 by 70% yielded a threshold of 1.2 machines per 10,000 women age 40 or older required to achieve a 70% screening rate. In sensitivity analysis we examined alternate definitions of inadequate capacity.
Mammography Utilization
We examined mammography utilization in two cohorts: 1) adult female respondents to the 2006 Behavioral Risk Factor Surveillance System (BRFSS) survey, and 2) a 5% random sample of female Medicare beneficiaries. These two data sources have been used extensively to examine cancer screening behaviors, including mammography, and both include geographic identifiers at the county level.
BRFSS
The BRFSS, administered and supported by the Behavioral Surveillance Branch of the Centers for Disease Control and Prevention (CDC), is a state-based, random-digit-dialed telephone survey of the civilian, noninstitutionalized US adult population 18 years of age and older. The BRFSS is conducted annually to collect uniform, state-specific data on preventive health practices and risk behaviors that are linked to injury and disease in the adult population, and BRFSS data are publicly accessible (http://www.cdc.gov/brfss).
In 2006, the core BRFSS module was administered in all 50 states and the District of Columbia. Each respondent’s county of residence was identified, unless there were fewer than 50 respondents in a county. The BRFSS uses a multistage cluster sampling design to obtain a state-stratified nationally representative sample. Within each state, the BRFSS selects a probability sample of households with telephones and interviews one adult per household. In 2006 the number of completed interviews per state varied from fewer than 2,000 to more than 20,000 with a total of 330,075. The cooperation rate – the proportion of respondents interviewed of all eligible units in which a respondent was selected and actually contacted – varied by state from 57% to 89%, and the response rate varied from 35% to 66%.(20)
In the BRFSS cohort recent use of mammography was defined as a report of a mammogram within the past two years, based on responses to the following questions: “A mammogram is an x-ray of each breast to look for breast cancer. Have you ever had a mammogram?” and “How long has it been since your last mammogram?” Of the 165,311 female survey respondents age 40 years or older, 160,465 (97%) answered both of these questions, and 128,802 (80%) of those respondents also had a county identifier. Compared with respondents whose county was identified, those lacking a county identifier (n=31,663) were similar with respect to age, race, marital status, and having health insurance, a regular source of health care and receiving a check-up in the past year, but they reported somewhat lower levels of educational attainment and household income.
Medicare
Medicare enrollment data and claims for a 5% random sample of beneficiaries were obtained from the Center for Medicare and Medicaid’s (CMS’s) Chronic Condition Warehouse (CCW). Medicare is the primary health insurer for nearly all adults age 65 and older. All beneficiaries in the traditional fee-for-service (FFS) program receive inpatient hospital, skilled nursing facility, and home health benefits under Medicare Part A. Ninety-five percent of beneficiaries subscribe to Medicare Part B which covers physician services, outpatient care, and durable medical equipment. The study cohort was restricted to women age 65 and older, enrolled in Medicare by January 1, 2004, who had traditional FFS coverage, including Part B, because claims were not available for beneficiaries enrolled in Medicare managed care plans.
We identified receipt of a mammogram in 2004–2005 based on the presence of a mammography claim in either the Outpatient Standard Analytic File (OutSAF) or the National Claims History (NCH) file. This time interval was similar to the period implicitly covered by the BRFSS mammography endpoint. Screening mammography has been covered by Medicare on a biennial basis since 1991 and annually since 1998, in addition to diagnostic mammography. Although specific billing codes distinguish screening from diagnostic mammography, inferences regarding mammogram indication based on claims are subject to some misclassification. We included codes for both diagnostic and screening mammograms, consistent with prior studies.(21–23) Mammograms preceded by a breast cancer diagnosis were excluded from the primary endpoint. Women with evidence of a breast cancer diagnosis prior to 2004 were excluded from the analysis, based on Medicare claims from 1999 through 2003. County of residence reflected the most recent mailing address, by the end of 2005, in Medicare enrollment records. Of the 892,147 female beneficiaries who met inclusion criteria, 218 (<0.5%) lacked a valid county identifier, leaving 891,929 in the study cohort.
Statistical Analysis
Characteristics of each cohort were summarized, and the frequency of mammography use was estimated. The adjusted impact of inadequate county mammography capacity on the likelihood of having a recent mammogram was estimated using multivariable logistic regression. Covariates included in the BRFSS analysis included age group, race, marital status, educational attainment, annual household income, health insurance status, regular source of health care, and receipt of a check-up in the past two years. These characteristics were self-reported by respondents. In the analysis of Medicare beneficiaries, available covariates included age, race, visit with a primary care physician identified in claims during 2004–2005, and comorbidity based on the Romano modification of the Charlson Comorbidity Index.(24)
In sensitivity analysis we included a proxy for spatial accessibility, identifying counties as urban or rural based on the 2003 Urban Influence Codes (UIC) from the US Department of Agriculture. These designations have been found to reflect regional economic systems and health care utilization patterns.(25) We dichotomized counties as urban (UIC 1–5) or rural (UIC 6–12); comparison with population density estimates suggested that this grouping separated counties that were either densely populated or near metropolitan areas from counties that were sparsely populated and far from metropolitan areas.
All analyses were performed in SAS, version 9.2, using SAS Survey procedures (SAS Institute Inc., Cary, NC). All estimates from the BRFSS cohort were weighted to account for the probability of sample selection and post-stratification adjustment for non-response and non-coverage of households without telephones.
RESULTS
Mammography Capacity
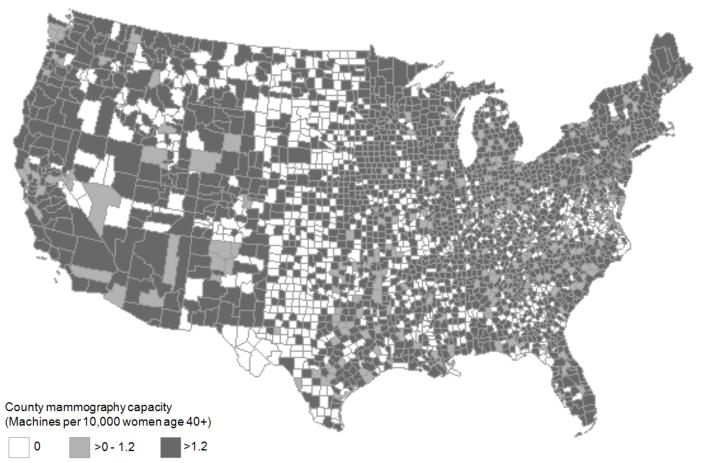
In 2004 there were 8,653 mammography facilities in the US with a total of 13,239 machines. Median county mammography capacity was 1.7 machines per 10,000 women age 40 or older (interquartile range 0 – 2.6 machines per 10,000 women). Inadequate-capacity counties were located throughout the country (Figure 1), although the greatest concentration was in the South, where 41% of 1,423 counties had fewer than 1.2 machines per 10,000 women. Rates of inadequate capacity in other regions were 12% in the Northeast (27 of 217 counties), 33% in the Midwest (347 of 1055 counties) and 35% in the West (158 of 445 counties). Of the 853 counties with no mammography machines and at least one adjacent county, 84% had at least one adjacent neighbor that also had no machines, but nearly all (97%) had at least one adjacent neighbor with mammography capacity greater than zero. Twenty-two counties with no machines were completely surrounded by other zero-capacity counties.
Figure 1. Geographic Distribution of Mammography Capacity in US Countries, 2004.
The number of mammography machines in each county was determined from mammography facility certification records and inspection reports from the US Food and Drug Administration.
Mammography Utilization: BRFSS
Recent use of mammography was reported by 77.4% of women in the BRFSS, including 74.5% of women who lived in counties with inadequate capacity and 77.7% of women in counties with adequate capacity (Table 1). Report of a mammogram in the past two years was more common in women were age 50–79 rather than 40–49 or older than 80; those who were married; had greater educational attainment and annual household income; had health insurance, a regular source of health care or a check-up in the past two years. Black and white women reported similar rates of recent mammography use, which were slightly higher than the rates reported by Hispanic and Asian women.
Table 1.
Characteristics of Cohort and Recent Use of Mammography, BRFSS 2006*
| N | Percent of Cohort | Percent with Mammogram | Adjusted OR | (95% CI) | |
|---|---|---|---|---|---|
| County mammography capacity | |||||
| Inadequate | 14,205 | 8.8 | 74.5 | 0.89 | (0.80 – 0.98) |
| Adequate | 114,597 | 91.2 | 77.7 | Reference | - |
| Age group | |||||
| 40–49 years | 32,783 | 32.1 | 69.8 | Reference | - |
| 50–59 years | 35,688 | 27.9 | 81.5 | 1.94 | (1.79 – 2.11) |
| 60–69 years | 27,480 | 18.1 | 83.5 | 2.15 | (1.97 – 2.35) |
| 70–79 years | 20,763 | 13.9 | 82.9 | 1.88 | (1.69 – 2.09) |
| 80+ years | 12,088 | 8.0 | 70.3 | 0.96 | (0.86 – 1.07) |
| Race | |||||
| White | 105,129 | 74.3 | 77.9 | Reference | - |
| Black | 10,580 | 10.0 | 78.3 | 1.20 | (1.07 – 1.34) |
| Hispanic | 6,001 | 9.8 | 75.5 | 1.51 | (1.28 – 1.79) |
| Asian | 1,959 | 2.3 | 75.2 | 0.80 | (0.60 – 1.07) |
| Other/Unknown | 5,133 | 3.6 | 71.5 | 0.84 | (0.73 – 0.97) |
| Marital status | |||||
| Married | 63,960 | 39.8 | 73.6 | Reference | - |
| Not married | 64,401 | 59.9 | 80.0 | 1.27 | (1.18 – 1.36) |
| Unknown | 441 | 0.3 | 73.0 | 0.86 | (0.58 – 1.27) |
| Educational attainment | |||||
| Less than HS graduate | 12,756 | 10.8 | 68.7 | Reference | - |
| HS graduate | 75,738 | 56.3 | 76.7 | 1.25 | (1.11 – 1.40) |
| College graduate+ | 40,084 | 32.8 | 81.5 | 1.48 | (1.31 – 1.69) |
| Unknown | 224 | 0.1 | 70.7 | 0.94 | (0.53 – 1.66) |
| Annual household income | |||||
| <$25,000 | 35,497 | 23.7 | 69.6 | Reference | - |
| $25,000–49,999 | 31,382 | 22.9 | 77.1 | 1.22 | (1.12 – 1.34) |
| $50,000–74,999 | 16,871 | 13.6 | 80.4 | 1.30 | (1.16 – 1.46) |
| $75,000+ | 24,422 | 24.3 | 82.5 | 1.51 | (1.35 – 1.69) |
| Unknown | 20,630 | 15.5 | 79.2 | 1.32 | (1.19 – 1.46) |
| Health insurance | |||||
| Yes | 118,046 | 90.9 | 79.9 | 1.79 | (1.59 – 2.01) |
| No | 10,593 | 9.0 | 52.5 | Reference | - |
| Unknown | 163 | 0.1 | 62.5 | 1.43 | (0.50 – 4.07) |
| Regular source of health care | |||||
| Yes | 117,821 | 90.7 | 80.4 | 2.15 | (1.91 – 2.42) |
| No | 10,756 | 9.2 | 47.9 | Reference | - |
| Unknown | 225 | 0.2 | 62.6 | 1.09 | (0.62 – 1.92) |
| Check-up in past 2 years | |||||
| Yes | 112,482 | 87.4 | 82.8 | 5.94 | (5.44 – 6.49) |
| No | 14,882 | 11.7 | 38.3 | Reference | - |
| Unknown | 1,438 | 0.9 | 64.9 | 2.89 | (2.23 – 3.74) |
BRFSS: Behavioral Risk Factor Surveillance System Survey
Recent use of mammography was defined by self-report receipt of a mammogram within the past two years.
Percent of Cohort gives the distribution of each characteristic within the cohort. Percent with Mammogram gives the percent of women in each row who reported a recent mammogram.
Adjusted OR: Odds ratio for impact of characteristic on odds of recent mammogram, adjusted for other characteristics in table.
Inadequate county mammography capacity was defined as <1.2 mammography machines per 10,000 women age 40+ in the county of residence.
All estimates, other than actual sample size (N), were weighted to account for the probability of sample selection and for post-stratification adjustment for non-response and non-coverage of households without telephones.
In multivariable analysis women who lived in counties with inadequate capacity had 11% lower odds of having had a mammogram in the prior two years (adjusted odds ratio [AOR] 0.89, 95% CI 0.80 – 0.98, p<0.05), compared with women in counties with adequate capacity, controlling for demographic, socio-economic and health care characteristics. The relationships observed in unadjusted analysis, between these characteristics and recent mammography use, persisted in the multivariable analysis. Having a regular source of health care and having had a check-up in the past year had the greatest influence on the odds of a recent mammogram, with AORs of 2.15 (95% CI 1.91 – 2.42) and 5.94 (95% CI 5.44 – 6.49) respectively.
Mammography Utilization: Medicare
Receipt of a mammogram in 2004–2005 was identified in Medicare claims for 40.2% of women in this cohort, including 38.0% of women in counties with inadequate capacity, compared with 40.5% of women in counties with adequate capacity (Table 2). Mammography use was most likely among Medicare beneficiaries in younger age groups, those with less comorbidity and those with a primary care visit during the study period. Black, Hispanic and Asian Medicare beneficiaries were less likely to have a claim for mammography than their white peers.
Table 2.
Characteristics of Cohort and Use of Mammography, Medicare 2004–2005
| N | Percent of Cohort | Percent With Mammogram | Adjusted OR | (95% CI) | |
|---|---|---|---|---|---|
| County mammography capacity | |||||
| Inadequate | 112,676 | 12.6 | 38.0 | 0.86 | (0.85 – 0.87) |
| Adequate | 779,253 | 87.4 | 40.5 | Reference | - |
| Age group | |||||
| 65–69 years | 164,037 | 18.4 | 56.0 | Reference | - |
| 70–74 years | 201,853 | 22.6 | 52.2 | 0.83 | (0.82 – 0.85) |
| 75–79 years | 197,917 | 22.2 | 44.3 | 0.59 | (0.59 – 0.60) |
| 80–84 years | 164,747 | 18.5 | 31.7 | 0.34 | (0.34 – 0.35) |
| 80+ years | 163,375 | 18.3 | 12.9 | 0.11 | (0.11 – 0.11) |
| Race | |||||
| White | 789,372 | 88.5 | 41.0 | Reference | - |
| Black | 69,629 | 7.8 | 34.8 | 0.74 | (0.73 – 0.75) |
| Hispanic | 11,716 | 1.3 | 32.1 | 0.66 | (0.64 – 0.69) |
| Asian | 10,033 | 1.1 | 31.0 | 0.54 | (0.52 – 0.57) |
| Other/Unknown | 11,539 | 1.3 | 34.3 | 0.67 | (0.65 – 0.70) |
| Charlson comorbidity score | |||||
| 0 | 797,780 | 89.4 | 41.8 | Reference | - |
| 1 | 46,351 | 5.2 | 31.1 | 0.69 | (0.68 – 0.71) |
| ≥2 | 47,798 | 5.4 | 21.2 | 0.39 | (0.38 – 0.40) |
| Primary care visit in past 2 years | |||||
| Yes | 815,393 | 91.4 | 42.5 | 5.05 | (4.94 – 5.16) |
| No | 76,536 | 8.6 | 15.1 | Reference | - |
Percent of Cohort gives the distribution of each characteristic within the cohort. Percent with Mammogram gives the percent of women in each row with a claim for a mammogram during the study period.
Adjusted OR: Odds ratio for impact of characteristic on odds of recent mammogram, adjusted for other characteristics in table.
Inadequate county mammography capacity was defined as <1.2 mammography machines per 10,000 women age 40+ in the county of residence.
Controlling for demographic and health care characteristics, residence in a county with inadequate capacity was associated with 14% lower of odds a mammogram (AOR 0.86, 95% CI 0.85 – 0.87, p<0.05). As observed in unadjusted analysis, non-white race, older age and greater comorbidity were inversely associated with mammography use. The strongest predictor of mammography use was a primary care visit during the study period, with an AOR of 5.05 (95% CI 4.94 – 5.16).
Sensitivity Analysis
In the Medicare cohort, results were not very sensitive to the definition of inadequate capacity. As shown in Figure 2, at all threshold values between 0 and 3.0 machines per 10,000 women, inadequate capacity was significantly associated with lower odds of having a mammogram, controlling for demographic and health care characteristics. In the BRFSS cohort, the relationship between inadequate capacity and mammography use was statistically significant for thresholds less than 1.5 machines per 10,000, but not for most values above 1.5. Regardless of the threshold for defining inadequate capacity, controlling for county urban influence did not alter the estimated impact of inadequate capacity in either cohort.
Figure 2. Adjusted Odds Ratio for Impact of Inadequate Mammography Capacity on Receipt of Recent Mammogram, BRFSS and Medicare.
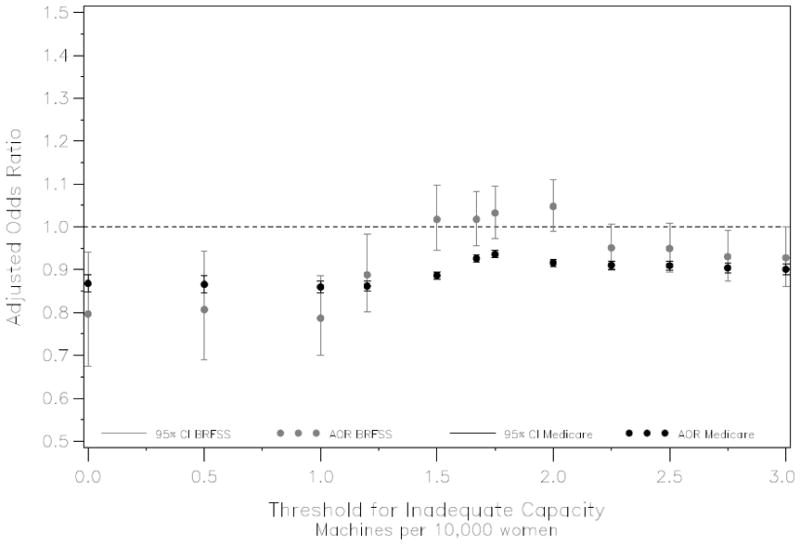
BRFSS: Behavioral Risk Factor Surveillance System Survey
Recent use of mammography defined by self-report receipt of a mammogram within the past two years (BRFSS, 2006) or health insurance claim for mammography in two-year period (Medicare, 2004–2005).
In BRFSS analysis, odds ratios were adjusted for age, race, marital status, educational attainment, household income, health insurance, regular source of health care and check-up in the past 2 years. In Medicare analysis, odds ratios were adjusted for age, race, comorbidity and primary care visit during the two-year study period.
All BRFSS estimates were weighted to account for the probability of sample selection and for post-stratification adjustment for non-response and non-coverage of households without telephones.
DISCUSSION
In the early 1990s, analysts predicted an excess supply of mammography machines in the US.(26) However, the number of mammography facilities decreased in the decade following implementation of the MQSA.(12–15) Our analyses of Medicare beneficiaries and respondents to a large national survey support an inverse relationship between mammography availability and utilization. Despite recent reports that mammography resources are adequate overall,(14) our results suggest that maldistribution of these resources may impair access to breast cancer screening in some areas.
While our results address the relationship between the availability of mammography machines and their utilization, human resources – mammographic technologists, medical physicists and interpreting radiologists – are important components of mammography capacity. A shortage of breast imagers has been reported in both community-based and academic practices.(18, 27) Several factors may be contributing to the reported shortage of qualified breast imagers, including fear of malpractice litigation, declining reimbursement, burdensome volume and education requirements stipulated by the MQSA, and greater interest in more sophisticated imaging modalities.(18, 28, 29) A shortage of mammographic technologists may also be limiting access to breast cancer screening.(30)
Our metric of mammography capacity quantifies the availability of machines, but not their spatial accessibility, both of which may independently influence utilization. For example, women in areas with limited capacity may face longer waiting times for an appointment, and women who live far from the nearest mammography facility may face a substantial travel burden. Resource capacity and proximity have been associated with health care utilization in a variety of other settings, including primary care,(31) prenatal care (32) and cancer treatment.(33, 34) Ongoing research regarding travel burden and appointment wait times should further elucidate the role of these factors in access to screening mammography.
Our estimate of the impact of inadequate capacity on mammography use was similar in the two cohorts evaluated, with AORs of 0.89 in the BRFSS cohort and 0.85 in the Medicare cohort. This similarity is remarkable given the differences between the two data sources and the populations they represent. BRFSS data are self-reported and may therefore be influenced by recall problems and social desirability bias. Recent evidence suggests that self-report surveys are likely to overestimate mammography utilization.(35, 36) Medicare claims, while not subject to these biases, only capture services reimbursed by Medicare. Free or subsidized mammograms will not be identified in claims if providers did not bill Medicare. Claims may therefore underestimate mammography utilization. These differences between the two data sources likely explain the greater estimate of recent mammography use among BRFSS respondents age 70–79, compared with the claims-based estimate among women of the same age in the Medicare analysis. In both cohorts, mammography use was inversely associated with age. This finding is not a surprise, as screening mammography benefits and guidelines are less clear for women age 70 and older than for women 40–69 years of age.(4, 37–39)
While mammography capacity had a similar impact on utilization in the two cohorts, results related to race diverged. In the Medicare cohort black, Hispanic and Asian women were all less likely than white women to receive a mammogram, while black and Hispanic BRSS respondents were more likely than their white peers to report a recent mammogram. Although this may be attributable to true differences between the cohorts, it may also be a function of race-specific variation in the accuracy of each data source for identifying breast cancer screening. Self-report of mammography use may be less sensitive and less specific among black women than white women.(36)
Numerous patient, physician and health insurance characteristics have been shown to facilitate or impede timely screening mammography.(21, 22, 40–47) In both cohorts we examined, the strongest predictors of a recent mammogram were factors related to interaction with the health care system, specifically having a regular source of care and having a check-up or a primary care visit. However, we also found that mammography capacity in a woman’s county of residence was significantly associated with mammogram use, controlling for these factors and for other important characteristics. We were not able to adjust for psycho-social factors or knowledge, attitudes and beliefs about breast cancer screening.
Additional limitations must be noted. We assumed that with respect to non-spatial factors, mammography facilities were equally accessible by all patients. In fact, some facilities may serve only patients participating in specific health insurance plans or physician practices. We defined mammography capacity at the county level, although women may seek health care services outside their county of residence. Also, if mammography capacity is associated with other county-level or even state-level attributes, our analysis would not be able to isolate the role of those factors. Finally, because we excluded women lacking a county identifier in the BRFSS our findings in that cohort likely underrepresent women in the most sparsely populated US counties, where access to health care resources in general is of particular concern.
Among all US counties, the estimated median female population aged 40 years or older was 6,334 in 2007, and only 36% of counties had at least 10,000 women in this age group. Of the 1,164 counties with mammography capacity <1.2 machines per 10,000 in 2007, the median county population of women in this age group was 3,044, the maximum was 574,665, and only 246 counties (21% of those with inadequate capacity) had at least 10,000 adult women potentially eligible for annual screening mammography. It may be unrealistic to expect every low-capacity county to enhance resource capacity alone if it does not have a population large enough to support the service. Rather, more successful strategies to increase mammography capacity might be regional efforts that serve a larger, multi-county population, perhaps with mobile mammography facilities. Areas where multiple adjacent counties have inadequate capacity would be priority targets for such initiatives.
Prior efforts to increase screening mammography have been multi-faceted and have typically focused on patient and physician behavior. Evaluations of interventions directed at patients (such as behavioral and educational programs) and interventions directed at primary care physicians (such as automated mammography reminder notifications) have found varying degrees of effectiveness.(48–50) Our findings suggest a third strategy for improving breast cancer screening rates, namely interventions directed at the local health care infrastructure. Further research on the influence of both technical and human resources will inform the development of specific initiatives, such as subsidies for the purchase of mammography equipment at community health centers or public hospitals in low-capacity areas, increased mammography reimbursement, and incentives for radiologists and technologists to practice in underserved areas. As we have shown here, geographic analysis can identify the communities in greatest need. Targeted enhancement of mammography capacity may boost breast cancer screening rates while optimizing limited health care resources.
Acknowledgments
This work was funded by grants from Susan G. Komen for the Cure (POP107806, PI: Elkin), the American Cancer Society (MRSG-06-127-01-CPHPS, PI: Elkin) and the National Cancer Institute (K07-CA118189, PI: Elkin).
References
- 1.Freedman DA, Petitti DB, Robins JM. On the efficacy of screening for breast cancer. Int J Epidemiol. 2004;33:43–55. doi: 10.1093/ije/dyg275. [DOI] [PubMed] [Google Scholar]
- 2.Kerlikowske K. Efficacy of screening mammography among women aged 40 to 49 years and 50 to 69 years: comparison of relative and absolute benefit. J Natl Cancer Inst Monogr. 1997;22:79–86. doi: 10.1093/jncimono/1997.22.79. [DOI] [PubMed] [Google Scholar]
- 3.Dodd GD. American Cancer Society guidelines from the past to the present. Cancer. 1993;72:1429–1432. doi: 10.1002/1097-0142(19930815)72:4+<1429::aid-cncr2820721403>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 4.U.S. Preventive Services Task Force. Screening for Breast Cancer: Recommendations and Rationale. Rockville, MD: Agency for Healthcare Research and Quality; 2002. [Google Scholar]
- 5.Miller JW, King JB, Ryerson AB, et al. Mammography use from 2000 to 2006: state-level trends with corresponding breast cancer incidence rates. AJR Am J Roentgenol. 2009;192:352–360. doi: 10.2214/ajr.08.1757. [DOI] [PubMed] [Google Scholar]
- 6.Use of mammograms among women aged >/= 40 years--United States, 2000–2005. MMWR Morb Mortal Wkly Rep. 2007;56:49–51. [PubMed] [Google Scholar]
- 7.Breen NAKC, Meissner HI, et al. Reported drop in mammography: is this cause for concern? Cancer. 2007;109:2405–2409. doi: 10.1002/cncr.22723. [DOI] [PubMed] [Google Scholar]
- 8.Geller BM, Kerlikowske K, Carney PA, et al. Mammography surveillance following breast cancer. Breast Cancer Res Treat. 2003;81:107–115. doi: 10.1023/A:1025794629878. [DOI] [PubMed] [Google Scholar]
- 9.Keating NL, Landrum MB, Guadagnoli E, et al. Factors related to underuse of surveillance mammography among breast cancer survivors. J Clin Oncol. 2006;24:85–94. doi: 10.1200/JCO.2005.02.4174. [DOI] [PubMed] [Google Scholar]
- 10.Schapira M, McAuliffe T, Nattinger AB. Underutilization of mammography in older breast cancer survivors. Med Care. 2000;38:281–289. doi: 10.1097/00005650-200003000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Mammography Quality Standards Act (1992) and Reauthorizations (1998, 2004)
- 12.U.S. General Accounting Office. Mammography Services: Impact of Federal Legislation on Quality, Access and Health Outcomes. Washington, DC: U.S. General Accounting Office; 1997. [Google Scholar]
- 13.U.S. General Accounting Office. Mammography Quality Standards Act: X-ray Quality Improved, Access Unaffected, but Impact on Health Outcomes Unknown. Washington, DC: U.S. General Accounting Office; 1998. [Google Scholar]
- 14.U.S. Government Accountability Office. Mammography: Current Nationwide Capacity is Adequate, But Access Problems May Exist in Certain Locations. Washington, DC: U.S. General Accounting Office; 2006. [Google Scholar]
- 15.U.S. Government Accountability Office. Mammography: Capacity Generally Exists to Deliver Services. Washington, DC: U.S. General Accounting Office; 2002. [Google Scholar]
- 16.Fischer R, Houn F, Van De Griek A, et al. The impact of the Mammography Quality Standards Act on the availability of mammography facilities. Prev Med. 1998;27:697–701. doi: 10.1006/pmed.1998.0347. [DOI] [PubMed] [Google Scholar]
- 17.Korn JE, Casey-Paal A, Lazovich D, et al. Impact of the Mammography Quality Standards Act on access in Minnesota. Public Health Rep. 1997;112:142–145. [PMC free article] [PubMed] [Google Scholar]
- 18.Farria DM, Schmidt ME, Monsees BS, et al. Professional and economic factors affecting access to mammography: a crisis today, or tomorrow? Results from a national survey. Cancer. 2005;104:491–498. doi: 10.1002/cncr.21304. [DOI] [PubMed] [Google Scholar]
- 19.U.S. Department of Health and Human Services. Healthy People 2010. Washington, DC: U.S. Government Printing Office; 2000. [Google Scholar]
- 20.Centers for Disease Control and Prevention. BRFSS 2006: Summary Data Quality Report. 2006 Available at: http://www.cdc.gov/brfss/technical_infodata/surveydata/2006.htm.
- 21.Blustein J. Medicare coverage, supplemental insurance, and the use of mammography by older women. New Engl J Med. 1995;332:1138–1143. doi: 10.1056/NEJM199504273321706. [DOI] [PubMed] [Google Scholar]
- 22.Kagay CR, Quale C, Smith-Bindman R. Screening mammography in the American elderly. Am J Prev Med. 2006;31:142–149. doi: 10.1016/j.amepre.2006.03.029. [DOI] [PubMed] [Google Scholar]
- 23.Smith-Bindman R, Quale C, Chu PW, et al. Can Medicare billing claims data be used to assess mammography utilization among women ages 65 and older? Med Care. 2006;44:463–470. doi: 10.1097/01.mlr.0000207436.07513.79. [DOI] [PubMed] [Google Scholar]
- 24.Romano PS, Roos LL, Jollis JG. Adapting a clinical comorbidity index for use with ICD-9-CM administrative data: differing perspectives. J Clin Epidemiol. 1993;46:1075–1079. doi: 10.1016/0895-4356(93)90103-8. [DOI] [PubMed] [Google Scholar]
- 25.Ricketts TC, Johnson-Webb KD, Taylor P. Definitions of Rural: A Handbook for Health Policy Makers and Researchers. Chapel Hill, NC: North Carolina Rural Health Research Program, Cecil G. Sheps Center for Health Services Research, University of North Carolina; 1998. p. 13. [Google Scholar]
- 26.Brown ML, Kessler LG, Rueter FG. Is the supply of mammography machines outstripping need and demand? An economic analysis. Ann Intern Med. 1990;113:547–552. doi: 10.7326/0003-4819-113-7-547. [DOI] [PubMed] [Google Scholar]
- 27.Sunshine JH, Maynard CD. Update on the diagnostic radiology employment market: findings through 2007–2008. J Am Coll Radiol. 2008;5:827–833. doi: 10.1016/j.jacr.2008.02.007. [DOI] [PubMed] [Google Scholar]
- 28.Bassett LW, Monsees BS, Smith RA, et al. Survey of radiology residents: breast imaging training and attitudes. Radiology. 2003;227:862–869. doi: 10.1148/radiol.2273020046. [DOI] [PubMed] [Google Scholar]
- 29.Elmore JG, Taplin SH, Barlow WE, et al. Does litigation influence medical practice? The influence of community radiologists’ medical malpractice perceptions and experience on screening mammography. Radiology. 2005;236:37–46. doi: 10.1148/radiol.2361040512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.D’Orsi C, Tu SP, Nakano C, et al. Current realities of delivering mammography services in the community: do challenges with staffing and scheduling exist? Radiology. 2005;235:391–395. doi: 10.1148/radiol.2352040132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Arcury TA, Gesler WM, Preisser JS, et al. The effects of geography and spatial behavior on health care utilization among the residents of a rural region. Health Serv Res. 2005;40:135–155. doi: 10.1111/j.1475-6773.2005.00346.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McLafferty S, Grady S. Prenatal care need and access: a GIS analysis. J Med Syst. 2004;28:321–333. doi: 10.1023/b:joms.0000032848.76032.28. [DOI] [PubMed] [Google Scholar]
- 33.Polsky D, Armstrong KA, Randall TC, et al. Variation in chemotherapy utilization in ovarian cancer: the relative contribution of geography. Health Serv Res. 2006;41:2201–2218. doi: 10.1111/j.1475-6773.2006.00596.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Punglia RS, Weeks JC, Neville BA, et al. Effect of distance to radiation treatment facility on use of radiation therapy after mastectomy in elderly women. Int J Radiat Oncol Biol Phys. 2006;66:56–63. doi: 10.1016/j.ijrobp.2006.03.059. [DOI] [PubMed] [Google Scholar]
- 35.Holt K, Franks P, Meldrum S, et al. Mammography self-report and mammography claims: racial, ethnic, and socioeconomic discrepancies among elderly women. Med Care. 2006;44:513–518. doi: 10.1097/01.mlr.0000215884.81143.da. [DOI] [PubMed] [Google Scholar]
- 36.Rauscher GH, Johnson TP, Cho YI, et al. Accuracy of self-reported cancer-screening histories: a meta-analysis. Cancer Epidemiol Biomarkers Prev. 2008;17:748–757. doi: 10.1158/1055-9965.EPI-07-2629. [DOI] [PubMed] [Google Scholar]
- 37.Fletcher SW, Black WC, Harris R, et al. Report of the International Workshop on Screening for Breast Cancer. J Natl Cancer Inst. 1993;85:1644–1656. doi: 10.1093/jnci/85.20.1644. [DOI] [PubMed] [Google Scholar]
- 38.Kerlikowske K, Salzmann P, Phillips KA, et al. Continuing screening mammography in women aged 70 to 79 years: impact on life expectancy and cost-effectiveness. J Amer Med Assoc. 1999;282:2156–2163. doi: 10.1001/jama.282.22.2156. [DOI] [PubMed] [Google Scholar]
- 39.Smith-Bindman R, Kerlikowske K, Gebretsadik T, et al. Is screening mammography effective in elderly women? Am J Med. 2000;108:112–119. doi: 10.1016/s0002-9343(99)00406-4. [DOI] [PubMed] [Google Scholar]
- 40.Phillips KA, Kerlikowske K, Baker LC, et al. Factors associated with women’s adherence to mammography screening guidelines. Health Serv Res. 1998;33:29–53. [PMC free article] [PubMed] [Google Scholar]
- 41.Decker SL, Hempstead K. HMO penetration and quality of care: the case of breast cancer. J Health Care Financ. 1999;26:18–32. [PubMed] [Google Scholar]
- 42.Hawley ST, Earp JA, O’Malley M, et al. The role of physician recommendation in women’s mammography use: is it a 2-stage process? Med Care. 2000;38:392–403. doi: 10.1097/00005650-200004000-00006. [DOI] [PubMed] [Google Scholar]
- 43.Finney Rutten LJ, Iannotti RJ. Health beliefs, salience of breast cancer family history, and involvement with breast cancer issues: adherence to annual mammography screening recommendations. Cancer Detect Prev. 2003;27:353–359. doi: 10.1016/s0361-090x(03)00133-8. [DOI] [PubMed] [Google Scholar]
- 44.Schootman M, Jeffe DB, Reschke AH, et al. Disparities related to socioeconomic status and access to medical care remain in the United States among women who never had a mammogram. Cancer Causes Control. 2003;14:419–425. doi: 10.1023/a:1024941626748. [DOI] [PubMed] [Google Scholar]
- 45.Calvocoressi L, Kasl SV, Lee CH, et al. A prospective study of perceived susceptibility to breast cancer and nonadherence to mammography screening guidelines in african american and white women ages 40 to 79 years. Cancer Epidemiol Biomarkers Prev. 2004;13:2096–2105. [PubMed] [Google Scholar]
- 46.Phillips KA, Haas JS, Liang SY, et al. Are gatekeeper requirements associated with cancer screening utilization? Health Serv Res. 2004;39:153–178. doi: 10.1111/j.1475-6773.2004.00220.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rakowski W, Meissner H, Vernon SW, et al. Correlates of repeat and recent mammography for women ages 45 to 75 in the 2002 to 2003 Health Information National Trends Survey (HINTS 2003) Cancer Epidemiol Biomarkers Prev. 2006;15:2093–2101. doi: 10.1158/1055-9965.EPI-06-0301. [DOI] [PubMed] [Google Scholar]
- 48.Bailey TM, Delva J, Gretebeck K, et al. A systematic review of mammography educational interventions for low-income women. Am J Health Promot. 2005;20:96–107. doi: 10.4278/0890-1171-20.2.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mandelblatt JS, Yabroff KR. Effectiveness of interventions designed to increase mammography use: a meta-analysis of provider-targeted strategies. Cancer Epidemiol Biomarkers Prev. 1999;8:759–767. [PubMed] [Google Scholar]
- 50.Yabroff KR, Mandelblatt JS. Interventions targeted toward patients to increase mammography use. Cancer Epidemiol Biomarkers Prev. 1999;8:749–757. [PubMed] [Google Scholar]