Abstract
Adult and childhood obesity and related adverse outcomes are most common among racial/ethnic minorities and socio-economically disadvantaged populations in the United States. Research approaches to obesity developed in mainstream populations and deploying new information technologies may exacerbate existing disparities in obesity. Current obesity management and prevention research priorities will not maximally impact this critical problem unless investigators explicitly focus on discovering innovative strategies for preventing and managing obesity in the disadvantaged populations that are most affected. On the basis of our research experience, four key research approaches are needed: (1) elucidating the underlying social forces that lead to disparities; (2) directly involving community members in the development of research questions and research methods; (3) developing flexible strategies that allow tailoring to multiple disadvantaged populations; and (4) building culturally and socio-economically tailored strategies specifically for populations most affected by obesity. Our experience with a community-based longitudinal cohort study and two health-center-based clinical trials illustrate these principles as a contrast to traditional research priorities that can inadvertently worsen existing social inequities. If obesity research does not directly address healthcare and health-outcome disparities, it will contribute to their perpetuation.
Keywords: community-based participatory research, tailored strategies, flexible strategies, disparities
Introduction
The societal value of medical research is diminished if discoveries aimed at widespread clinical conditions are not equally accessible to the entire population. Especially for publicly funded research, there is an ethical obligation and a human rights responsibility to emphasize research that benefits the most affected subpopulations. Unfortunately, the bulk of research on obesity prevention and management is developed, tested and implemented in such a way that it does not specifically address the already underserved subpopulations that deserve the greatest attention. Disadvantaged social groups, including racial/ethnic minorities (we use the term racial/ethnic minorities to refer to the social construction of subgroups that may share a combination of similar country/region of origin, social, cultural and economic factors) and people with low income and/or low educational attainment, experience the greatest burden of obesity in the United States.1 Unless research specifically addresses the underlying factors that account for existing health disparities and social inequalities in these populations, research activities can easily contribute to the maintenance and exacerbation of disparities and the perpetuation of broader social injustice.
As obesity researchers, we often take for granted that all strategies aimed at obesity prevention and management are equally valuable from a societal perspective. We assume that discoveries have an incremental value that will lead to the amelioration of a widespread epidemic of a potent risk factor for chronic disease, including its adverse impact on mortality, morbidity and quality of life. However, this is not always the case. When strategies are developed for and tested in middle-class, predominantly White populations, these strategies help only a subset of the population. In fact, they target a subset that has less need for these strategies compared with minority and lower socio-economic status populations that experience a greater burden of obesity and obesity-related adverse outcomes. Similarly, researchers often assume that if strategies are proven efficacious in middle-class White populations, they can be readily tailored and adapted to fit other subpopulations effectively. However, failure to directly address the factors that lead to obesity in disadvantaged populations will make prevention and management in these populations challenging and short-lived. Thus, from both a methodological and practical perspective, to have the greatest impact on the prevalence of obesity, more investigators should explicitly focus their research on discovering novel and innovative strategies for preventing and managing obesity in the populations most affected. Researchers who continue to focus on mainstream populations can recruit more diverse populations and develop more flexible interventions that can reach beyond the mainstream.
The goal of this paper is to highlight several approaches that have the potential to minimize these shortcomings in the current obesity prevention and management research agenda. These approaches include the following: (1) policy-oriented research that seeks to uncover intervention opportunities in socially disadvantaged groups; (2) community-based participatory frameworks that include members of underserved populations and work to overcome the historical and continuing barriers that limit minority participation in research; (3) flexible interventions that can serve multiple segments of the population; and (4) tailored interventions that specifically address the barriers faced by specific underserved populations. These strategies must be pursued both by investigators who conduct research and policy makers who set research priorities.
Unequal distribution of research discoveries
Current patterns of obesity research and statements of research priorities are not aligned with the unequal distribution of obesity and its clinical consequences. If anything, current research patterns and priorities will yield a continued unequal distribution of research findings that benefit the White, middle-class populations, thus perpetuating and further contributing to widening of health disparities.
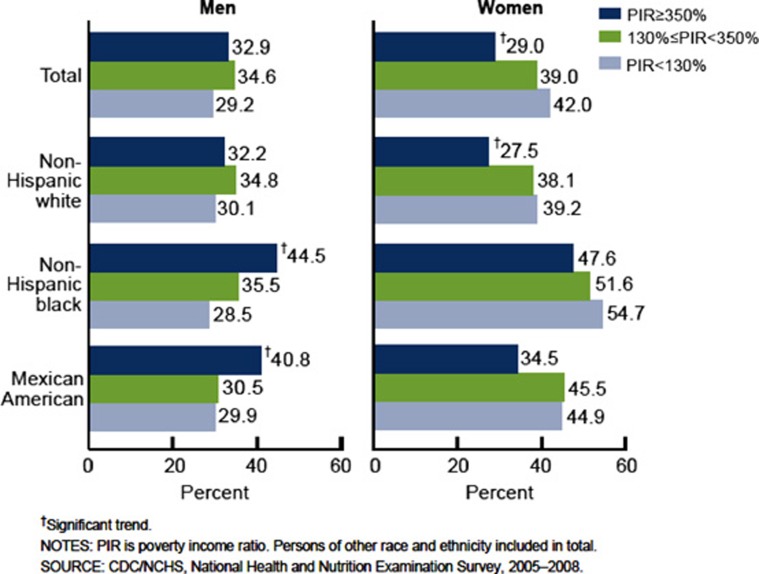
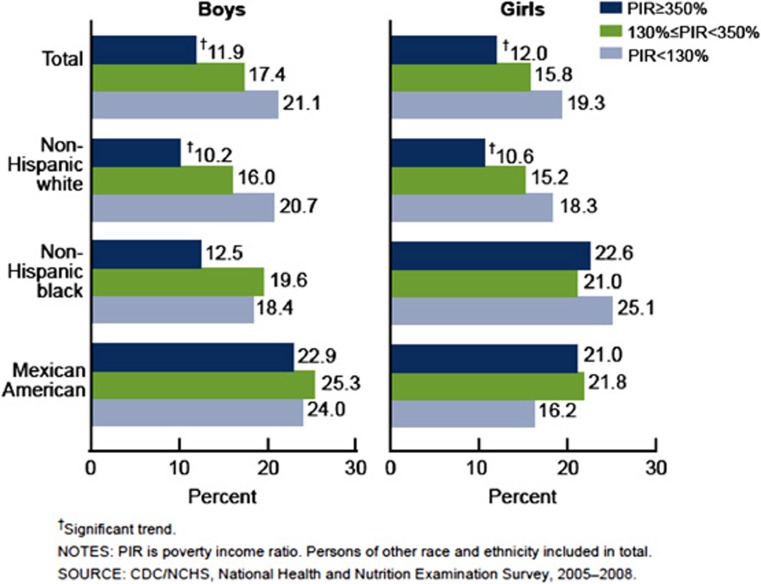
Obesity and its clinical consequences, such as diabetes, are more prevalent among minority and lower socio-economic status populations in general. Among adults, age-adjusted prevalence of obesity (body mass index (BMI)>30) is lower in non-Hispanic Whites (32.4%) compared with African Americans (44.1%) and Mexican Americans (40.4%), based on the 2008 National Health and Nutrition Survey (NHANES) data.2 Mexican American adults had the greatest increases in obesity prevalence between 1999 and 2000 (39.7%), and 2007 and 2008 (45.1%). Disparities for diabetes are even larger than those for obesity in the 2008 NHANES sample: 7.1% of non-Hispanic Whites, 12.6% of non-Hispanic Blacks and 13.3% of Mexican Americans had diagnosed diabetes.3 Obesity is also more prevalent among racial/ethnic minority children based on the most recent NHANES data that show 15.3% of non-Hispanic White children classified as obese (BMI>95th%), compared with 20.9% of Hispanic children and 20.0% of non-Hispanic Black children.4 However, there are complex associations of race/ethnicity and socio-economic status with obesity among adults and children by gender. Using NHANES data, education and income appear to be inversely associated with the prevalence of obesity across race/ethnicity categories among adult women, whereas the associations of income and education vary by race/ethnicity for men (see Figure 1).5 In addition, obesity prevalence among children increased as income decreased overall; however, the pattern varied by gender and race/ethnicity as well (see Figure 2).6 These complex relationships between gender, socio-economic status and race/ethnicity argue against a one-size-fits-all approach to obesity prevention and management. Rather, research and established research priorities should allow for and reflect the multifaceted patterns of obesity among disadvantaged adults and children.
Figure 1.
Prevalence of obesity among adults aged 20 years and over, by poverty income ratio, sex, and race and ethnicity: United States, 2005–2008. Adapted from ref. 6.
Figure 2.
Prevalence of obesity among children and adolescents aged 2–19 years, by poverty income ratio, sex, and race and ethnicity: United States, 2005–2008. Adapted from ref. 6.
The studies funded to investigate obesity do not equitably reflect the distribution of obesity and diabetes. The presumption is that strategies developed for the mainstream population will be readily applicable and acceptable to disadvantaged populations. Certain types of research are particularly likely to benefit middle-class populations, whereas neglecting disadvantaged populations. Innovative information technology strategies may be less applicable to disadvantaged populations given the continued, although perhaps lessening, ‘digital divide' in this country. Biomedical research aimed at the development of pharmacological agents may be unlikely to readily trickle down to populations in which access to healthcare is problematic. Similarly, behavioral strategies seeking lifestyle solutions may not readily encompass low-income populations who face disproportionate environmental barriers to healthy eating and physical activity.7 In addition, failure to recognize the social forces of poverty, marginalization and discrimination will make it unlikely that current research will be able to adequately address current disparities.
As they should, federal priorities for obesity research (Strategic Plan for NIH Obesity Research, 2011) continue to promote innovation in obesity research with a focus on understanding biological mechanisms, developing successful interventions, understanding the causes of obesity and harnessing technology. As in earlier research priorities,8 the 2011 National Institutes of Health priorities acknowledge that research directed at disadvantaged populations is needed. This is incorporated into the priority of ‘evaluating promising strategies for obesity prevention and treatment in real-world settings and diverse populations.' Nevertheless, pursuit of the selected priorities is likely to exacerbate existing obesity-related disparities.
Research strategies needed to address disparities in obesity
Fully addressing disparities in obesity and related outcomes for adults and children will require new strategies that may require shifting research away from current priorities. On the basis of our own experience and that of other researchers in health disparities, we believe that the following approaches are required:
Policy-oriented research that elucidates the underlying social forces, which lead to disparities. It is particularly important to identify those causes of health disparities that can be addressed through social and political change.
The use of strategies that directly involve members of these communities in the development of research questions and research methods. Community-based participatory research (CBPR) is particularly critical in addressing the underlying needs of disadvantaged communities.
Research that builds flexible strategies allowing the ability to tailor for different languages, levels of technology access and health literacy. There is a need for obesity prevention and treatment strategies that work across a range of populations and that can be readily tailored for even greater effectiveness.
Research that specifically develops culturally and socio-economically tailored strategies for disadvantaged populations that are subject to the greatest burdens.
Within each of these categories, research should be maximally policy-relevant, and information should be collected and analyzed to inform cost effectiveness. We will illustrate these approaches to obesity research with examples from our own experience. In particular, we review our work on the CHAMACOS (Center for the Health Assessment of Mothers and Children of Salinas) observational study to suggest the value of research that elucidates underlying social factors and the inclusion of community participation in developing research priorities. We also review two clinical trials to illustrate strategies aimed at building interventional flexibility to reach multiple communities (Heart-to-Heart) and development of a focused intervention in a specific disadvantaged population (Vivamos Activos).
Research that elucidates the underlying social forces that lead to disparities
To effectively design, implement, and test prevention and management interventions that address the disproportionately higher prevalence of obesity among disadvantaged subpopulations, we need research that systematically seeks to understand the modifiable factors that influence obesity in these communities. Although disadvantaged populations are often simplified to racial/ethnic minority groups, research to inform interventions aimed at decreasing disparities should give careful consideration to social and psychosocial disadvantage as well. In practice, this means adequately measuring and studying factors, such as social class, discrimination, segregation and acculturation, in conjunction with race/ethnicity. Levels of analysis may include individual, as most traditionally performed, as well as family, home, neighborhood, school and workplace. Such an approach is described by Dr Paula Braveman in her 2009 article, ‘A health disparities perspective on obesity research'.9 Dr Braveman argues that explicitly studying these social and psychosocial factors, as opposed to controlling for them, will lead to a sound base of evidence for future interventions and policy.9 Such research has the greatest potential to inform policy-relevant and cost-effective interventions.
CHAMACOS: understanding obesity disparities with a community-based participatory framework
The CHAMACOS study is a longitudinal birth cohort study centered in the Salinas Valley, CA, USA, which was designed to examine exposure to environmental contaminants and their impact on children's health, growth and development. Using a CBPR framework, this study is a partnership between UC Berkeley and Clinica de Salud del Valle de Salinas with numerous additional academic and community-based collaborators. CBPR is a collaborative orientation to research that equitably involves all partners throughout the research process.10
With detailed measurements of children's growth, as well as extensive information on their in utero, familial, physical and social environments, the CHAMACOS cohort is ideally suited to better understand the determinants of obesity among low-income children of Mexican descent, a population disproportionately affected by obesity. In addition, the community-based participatory orientation embedded in the study provides ample opportunity for community input into the investigation of determinants, as well as the infrastructure in place to build and test community-based interventions based on these findings.
In 1999–2000, 601 pregnant women living in the agricultural Salinas Valley were enrolled. Mothers and their children have been periodically followed up from birth to 11 years of age, with plans for follow-up until 12 years of age. Mothers in the CHAMACOS sample were primarily born in Mexico (85%), belonged to the low-income (62%) stratum of the society, had less than a high-school education (81%) and either worked in agriculture (42%) or had household members who worked in farms at the time of enrollment (82%).11 By 2 years of age, 30% of the children in the CHAMACOS sample were classified as overweight or obese,12 which is higher than national samples for non-Hispanic White children and Mexican American children as well.4 Warner et al.12 found that 2-year-old children in the CHAMACOS cohort, who drank one or more sodas per day had a 3.4 (95% confidence interval 1.4, 8.1) greater odds of being obese compared with children who consumed no soda. Over half of the mothers in the CHAMACOS cohort (56%) reported that their children consumed at least some soda in the prior week.
To better understand the impacts of migration on childhood obesity in this immigrant population, we recruited a similar sample of mothers and children from the communities of origin in Mexico to compare with their US resident counterparts. The number of children classified as obese or overweight (greater than the 85th percentile compared with 2000 CDC growth charts) was significantly higher in California compared with Mexico (53 vs 15%).13 Household food insecurity was higher among families in Mexico than among Mexican immigrants in California (75 vs 39% P<0.01).14 However, the dietary consequences of food insecurity differed by country of residence. In California, children from households classified as food insecure tended to consume more energy, fat, and sweets and snacks compared with children in food-secure households. In Mexico, children from food-insecure households tended to consume less energy, carbohydrates, fruit, dairy and meat than children from food-secure households. Mexican immigrant parents may come to the United States with past experiences of food insecurity similar to what we observed in the Mexico sample. Mexican immigrant parents in the United States may overcompensate for previous experiences of food insecurity in Mexico by providing their children with packaged, energy-dense foods that are readily available and inexpensive in the United States, but not accessible in Mexico. This research provides an example of how social factors such as food insecurity and country of residence impact obesity-related outcomes. In addition, this research was designed to inform nutritional policy targeting low-income children of Mexican descent in both the United States and Mexico. Forthcoming and future research using the CHAMACOS sample will seek to understand prenatal and early-life biological and psychosocial factors associated with later obesity, as well as the complex interplay of environmental and genetic factors.
Heart-to-Heart: building in flexibility to reach multiple communities
San Mateo County
Stanford Heart-to-Heart was a clinical trial evaluating the effectiveness of nurse and dietitian case management for cardiovascular disease (CVD) risk-factor control in a multiethnic low-income population. The goal was to develop a flexible intervention that functioned well across a diversity of low-income subpopulations. In 2003–2005, we recruited 419 low-income patients receiving care at one of four San Mateo County-run satellite health centers.15, 16 Eligible participants had one or more inadequately controlled CVD risk factors. Only 15% were White, non-Latinos, with the remaining population being Latino (63%), Asian/Pacific Islander (12%) and African American (10%). Obesity (mean BMI 35) and diabetes (63%) were prominent among participants. Participants were randomized into case management (n=212) or usual primary care, followed by delayed case management intervention (n=207). The primary outcome of Framingham risk score (estimated 10-year risk of CVD risk) was assessed after a mean duration of 16 months.
Case management consisted of one-on-one visits to nurses and dietitians, which focused on the following: (1) behavioral change around diet, physical activity, weight management and medication adherence; (2) care coordination for primary care, specialty care and mental health services; and (3) optimizing medication therapy for diabetes and other CVD factors. These strategies were delivered in Spanish and English. The intervention approach focused on providing culturally appropriate information and behavioral change strategies to each of the study's six main subpopulations: Latino, African American, Samoan/Tongan, Chinese, Filipino and White, non-Latinos.
Mean Framingham risk scores decreased with case management (from 17.6% at baseline to 16.7% at follow-up), whereas it increased with usual care (17.1% at baseline to 17.3% at follow-up), with a net change in risk of 1.1% attributable to the intervention or to 200 individuals receiving the intervention to prevent 1 event per year. The main driver of these differences was lowering systolic blood pressure. The intervention's impact was similar across ethnic subgroups. On the basis of these results, and as initially planned, the intervention was successfully transitioned into an ongoing County-run risk-factor management program that has the potential to be easily replicated in other low-income communities. Despite high levels of participant and physician satisfaction, the intervention's focus on medical management did not fully address the participants' interest in weight loss.17 In addition, participants could have used extra help implementing case-manager advice, particularly navigating family, community and cultural barriers to behavior change.
Vivamos Activos: reducing disparities by focusing attention on a disadvantaged population
Vivamos Activos is an ongoing clinical trial testing two strategies for facilitating weight loss in obese, low-income Latinos compared with usual care.18 In this County health-center-based study, a case-management approach delivered by a health educator is being tested with and without the community health worker support. A goal of the program is to seek strategies that can reduce disparities by focusing attention on a population in which the burden of obesity and its clinical consequences is high.
In 2009–2010, 207 obese, low-income, Latino primary care patients (76% < high-school education) with one or more inadequately controlled CVD risk factors were randomized into three arms: case management alone (n=84), case management plus community health worker home visits (n=82) and usual primary care (n=41). As shown in Table 1, the randomized population is 77% female with a mean age of 47.1 years; 55% of participants have eighth-grade education or less. Participants have a mean BMI of 35.6 with high rates of diabetes (43%) and elevated triglyceride levels (mean 164 mg dl−1). The primary outcome is reduction in BMI at 24 months of follow-up. The case-management weight-loss approach was derived from the Diabetes Prevention Program.19 The approach includes both group sessions (15 meetings) and one-on-one counseling sessions (6 visits). These group and one-on-one sessions focus on improving practical knowledge and skills, facilitating behavior change, building peer support, raising awareness about environmental influences and in-class physical activity. The home visits (6 visits) were designed to help participants navigate their home and neighborhood environments to make healthy choices around eating and physical activity.
Table 1. Demographic and clinical profile of Vivamos Activos participants by gender.
| Categorical variables |
Total (N=207) |
Female (N=159) |
Male (N=48) |
P-value (male vs female) | |||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | ||
| Age categories (years) | |||||||
| 20–29 | 12 | (5.8) | 8 | (5.0) | 4 | (8.3) | 0.96 |
| 30–39 | 44 | (21.3) | 33 | (20.8) | 11 | (22.9) | — |
| 40–49 | 69 | (33.3) | 54 | (34.0) | 15 | (31.3) | — |
| 50–59 | 52 | (25.1) | 40 | (25.2) | 12 | (25.0) | — |
| 60–69 | 25 | (12.1) | 20 | (12.6) | 5 | (10.4) | — |
| 70–79 | 5 | (2.4) | 4 | (2.5) | 1 | (2.1) | — |
| Diabetes mellitus Type 2 | 89 | (43.0) | 71 | (44.7) | 18 | (37.5) | 0.38 |
| Education | |||||||
| Eight grade or less | 113 | (54.6) | 93 | (58.5) | 20 | (41.7) | 0.02 |
| Some high school | 40 | (19.3) | 29 | (18.2) | 11 | (22.9) | — |
| High school or GED certificate | 24 | (11.6) | 18 | (11.3) | 6 | (12.5) | — |
| Technical school or any college | 30 | (14.5) | 19 | (12.0) | 11 | (22.9) | — |
| Employment status | |||||||
| Employed for wages | 90 | (43.5) | 61 | (38.4) | 29 | (60.4) | <0.01 |
| Self-employed | 6 | (2.9) | 4 | (2.5) | 2 | (4.2) | — |
| Out of work | 21 | (10.2) | 10 | (6.3) | 11 | (22.9) | — |
| Homemaker | 74 | (35.7) | 74 | (46.5) | 0 | (0.0) | — |
| Retired | 10 | (4.8) | 8 | (5.0) | 2 | (4.2) | — |
| Unable to work | 6 | (2.9) | 2 | (1.3) | 4 | (8.3) | — |
| Annual personal income | |||||||
| Less than $10 000 | 58 | (28.0) | 47 | (29.6) | 11 | (22.9) | 0.06 |
| $10 000 to less than $15,000 | 42 | (20.3) | 32 | (20.1) | 10 | (20.8) | — |
| $15 000 to less than $20 000 | 50 | (24.2) | 42 | (26.4) | 8 | (16.7) | — |
| $20 000 to less than $25 000 | 22 | (10.6) | 17 | (10.7) | 5 | (10.4) | — |
| $25 000 to less than $35 000 | 26 | (12.6) | 15 | (9.4) | 11 | (22.9) | — |
| $35 000 to less than $75 000 | 8 | (3.9) | 5 | (3.1) | 3 | (3.1) | — |
| Do not know | 1 | (0.5) | 1 | (0.6) | 0 | (0.0) | — |
| Country of birth | |||||||
| Mexico | 159 | (76.8) | 126 | (79.2) | 33 | (68.8) | 0.13 |
| Other (mostly Central America) | 48 | (23.2) | 33 | (20.8) | 15 | (31.3) | — |
| Continuous Variables | Mean | s.d. | Mean | s.d. | Mean | s.d. | P-value |
| (male vs female) | |||||||
| BMI (kg m−2) | 35.6 | 5.3 | 36.0 | 5.2 | 34.3 | 5.4 | 0.05 |
| Systolic blood pressure (mm Hg) | 115.2 | 13.0 | 114.1 | 13.0 | 118.6 | 12.8 | 0.04 |
| LDL-cholesterol (mg dl−1) | 104.9 | 34.9 | 103.1 | 31.7 | 110.8 | 43.6 | 0.26 |
| HDL-cholesterol (mg dl−1) | 45.6 | 10.8 | 46.7 | 11.4 | 41.7 | 7.6 | < 0.01 |
| Triglycerides (mg dl−1) | 164.3 | 99.5 | 166.4 | 108.9 | 157.5 | 58.9 | 0.47 |
| Total cholesterol (mg dl−1) | 181.6 | 42.0 | 181.2 | 40.0 | 183.0 | 48.5 | 0.79 |
| Fasting plasma glucose (mg dl−1) | 113.4 | 33.3 | 112.7 | 31.8 | 115.8 | 38.1 | 0.57 |
| Glycated hemoglobin (%) | 6.5 | 1.4 | 6.5 | 1.4 | 6.4 | 1.4 | 0.71 |
| C-reactive protein (mg dl−1) | 0.7 | 0.5 | 0.7 | 0.5 | 0.6 | 0.5 | 0.40 |
| Age (years) | 47.1 | 11.1 | 47.5 | 11.1 | 45.7 | 11.5 | 0.32 |
| Years lived in neighborhood | 11.2 | 8.2 | 11.2 | 8.0 | 11.3 | 9.1 | 0.94 |
Abbreviations: BMI, body mass index; LDL, low-density lipoprotein; HDL, high-density lipoprotein.
Linguistic and cultural tailoring of intervention components that had been successfully used in other programs was carried out in partnership with a community-based organization. Additional input was obtained from community members, service providers working in the community (e.g., local senior center, food bank) and the health center into which the intervention was integrated. The 2-year intervention consists of an initial intensive phase (6 months), a continued weight-loss phase (6 months) and a maintenance phase (12 months). The group of patients initially randomized to usual care will receive the case-management intervention after a 2-year delay. No outcome information is currently available, as the intervention will conclude in September 2012. In addition to assessment of weight loss, the planned analysis will consider the impact on CVD risk factors and the cost-effectiveness of the two interventions. Following the clinical trial, the program will transition to an ongoing County program, provided that evidence of effectiveness and cost-effectiveness is obtained. The intervention was also designed to enable replication in similar low-income Latino communities across California and the US.
Practical research strategies in disadvantaged populations
These research strategies and studies we have reviewed illustrate key strategies that are needed to address health disparities in obesity and obesity-related diseases using a community-based approach. They also suggest several practical mechanisms for incorporating a CBPR orientation to research on the prevention and management of obesity in disadvantaged populations. First, it is vital to confront the valid suspicions and concerns that disadvantaged communities have about research that is based on historical betrayal by past researchers and current patterns of marginalization by academic medical centers. This can be done through extensive community work before research begins and by setting up community advisory boards as was done in the CHAMACOS study. Although not described in detail in the above examples, we found it critical to equitably partner with and include community-based and governmental organizations in all phases of the research process. In addition, wherever possible, obesity researchers should endeavor to improve existing healthcare settings rather than set up alternative systems of delivering interventions that will no longer be available once research funding ends, as was done in Heart-to-Heart and Vivamos Activos. In the case of randomized controlled trials, equity suggests that research participants be compensated with appropriate incentives, although it is perhaps ideal for reimbursement to be provided only for the research aspects of programs rather than for the interventions themselves. Similarly, where statistically appropriate, the size of control groups should be minimized in keeping with the principle that research should benefit the maximum fraction of the population. As in the Heart-to-Heart and Vivamos Activos clinical trials, ‘delayed intervention' should be used as model for control groups, so that all research participants receive eventual benefits. Finally, steps should be taken to maximize the likelihood of sustainability from the beginning. Research studies can serve to inform both science and the operational planning of organizations that can nurture and sustain research interventions into ongoing service programs. Using a community-based orientation, some strategies of which we describe above, will often lead to insights that are not otherwise available. Combined with rigorous research on the underlying causes of social and racial/ethnic disparities in obesity, a CBPR approach will maximize the participation of disadvantaged communities and increase the value of research for the involved communities.
Challenges of community-based obesity research
Although it is imperative that obesity researchers focus on neglected populations in greatest need, it is important to acknowledge the challenges of community-based research in low-income communities. Compared with other research settings, community-based research may have multiple logistical obstacles to success. Very often, organizations serving disadvantaged populations have fewer resources, lack the infrastructure available in other settings and may be organizationally unstable owing to funding concerns or ongoing turf wars. The process of including community members and community organizations adds extra time and complexity to research development. In addition, for historical and contemporary reasons, populations may be legitimately skeptical about the value of research and wary of experimentation. This is particularly true regarding suspicion around the need to have a control group in clinical trials. In addition, community organizations often have priorities that reduce their commitment to scientific rigor. For example, the priorities to serve as many population members as possible may reduce their commitment to having a control group or their support for the collection of in-depth survey questionnaire information from participants. These acknowledged challenges should be weighed alongside the benefits.
The benefits of a community-based approach
A community-based approach is one of the only mechanisms available to meet the needs of low-income, minority populations that are at risk of being neglected by mainstream research on obesity prevention and management. This approach not only helps develop strategies that are accessible to disadvantaged populations, but may also identify and intervene on upstream social problems that help contribute to risk of obesity in the first place. By focusing on populations most at risk for obesity and its clinical complications, research is targeted to the populations at greatest need. This approach also allows health to be conceptualized from a community's perspective (rather than an academic perspective). Interventions developed by and for communities allow research to reach real-world populations, and not the optimized middle-class, White, research clinic population. Although working with governmental and community-based organizations can increase the organizational complexity of research, oftentimes these are grateful organizations whose survival can depend on the value that a rigorous outcomes-based perspective can contribute. Community-based research in disadvantaged populations can help reduce health disparities by developing strategies that are effective in the communities that are most affected by obesity. An additional benefit of this approach is that strategies that are proven effective in disadvantaged communities are likely to be applicable across multiple populations, because they are designed for the most challenging settings in which resources are scarce and environmental influences of obesity are prevalent.
Conclusions
In the context of population-based obesity research, where known disparities exist, if our work is not directly addressing disparities, it contributes to their perpetuation. Not only do we inadvertently reinforce existing social inequities, but we also have the potential to make them worse. We also have an obligation to address the upstream social forces that lead to disparities in the first place.
Acknowledgments
This report was supported by a research grant (LGR, RSS R01 HL 089448) and a mid-career mentoring award (RSS, K24 HL086703), both from the National Heart, Lung, and Blood Institute. Publication of this supplement was partially supported by Nutrilite Health Institute with an unrestricted educational contribution to Stanford Prevention Research Center.
RS Stafford received consulting fees from Mylan Pharmaceuticals as an expert witness. LG Rosas declares no conflict of interest.
References
- Wang Y, Beydoun MA. The obesity epidemic in the United States—gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev 2007; 29: 6–28. [DOI] [PubMed] [Google Scholar]
- Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA 2012; 303: 235–241. [DOI] [PubMed] [Google Scholar]
- Center for Disease Control and Prevention.. National Diabetes Fact Sheet: National Estimates and General Information on Diabetes and Prediabetes in the United States. U.S. Department of Health and Human Services, Center for Disease Control and Prevention: Atlanta, GA, 2011. [Google Scholar]
- Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA 2012; 303: 242–249. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Lamb MM, Carroll MD, Flegal KM. Obesity and Socioeconomic Status in Adults: United States, 2005–2008. NCHS Data Brief, Number 50. National Center for Health Statistics: Hyattsville, MD, 2010. [PubMed] [Google Scholar]
- Ogden CL, Lamb MM, Carroll MD, Flegal KM. Obesity and Socioeconomic Status in Children and Adolescents: United States, 2005–2008. NCHS Data Brief, Number 51. National Center for Health Statistics: Hyattsville, MD, 2010. [PubMed] [Google Scholar]
- Lovasi GS, Hutson MA, Guerra M, Neckerman KM. Built environments and obesity in disadvantaged populations. Epidemiol Rev 2009; 31: 7–20. [DOI] [PubMed] [Google Scholar]
- Spiegel AM, Alving BM. Executive summary of the Strategic Plan for National Institutes of Health Obesity Research. Am J Clin Nutr 2005; 82: 211S–214S. [DOI] [PubMed] [Google Scholar]
- Braveman P. A health disparities perspective on obesity research. Prev Chronic Dis 2009; 6: A91. [PMC free article] [PubMed] [Google Scholar]
- Minkler M. Linking science and policy through community-based participatory research to study and address health disparities. Am J Public Health 2010; 100 (Suppl 1): S81–S87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eskenazi B, Marks AR, Bradman A, Harley K, Barr DB, Johnson C et al. Organophosphate pesticide exposure and neurodevelopment in young Mexican-American children. Environ Health Perspect 2007; 115: 792–798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner ML, Harley K, Bradman A, Vargas G, Eskenazi B. Soda consumption and overweight status of 2-year-old mexican-american children in california. Obesity (Silver Spring) 2006; 14: 1966–1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosas LG, Guendelman S, Harley K, Fernald LC, Neufeld L, Mejia F et al. Factors associated with overweight and obesity among children of Mexican descent: results of a binational study. J Immigr Minor Health 2011; 13: 169–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosas LG, Harley K, Fernald LC, Guendelman S, Mejia F, Neufeld LM et al. Dietary associations of household food insecurity among children of Mexican descent: results of a binational study. J Am Diet Assoc 2009; 109: 2001–2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma J, Lee KV, Berra K, Stafford RS. Implementation of case management to reduce cardiovascular disease risk in the Stanford and San Mateo Heart to Heart randomized controlled trial: study protocol and baseline characteristics. Implement Sci 2006; 1: 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma J, Berra K, Haskell WL, Klieman L, Hyde S, Smith MW et al. Case management to reduce risk of cardiovascular disease in a county health care system. Arch Intern Med 2009; 169: 1988–1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berra K, Ma J, Klieman L, Hyde S, Monti V, Guardado A et al. Implementing cardiac risk-factor case management: lessons learned in a county health system. Crit Pathw Cardiol 2007; 6: 173–179. [DOI] [PubMed] [Google Scholar]
- Drieling RL, Ma J, Stafford RS. Evaluating clinic and community-based lifestyle interventions for obesity reduction in a low-income Latino neighborhood: Vivamos Activos Fair Oaks Program. BMC Public Health 2011; 11: 98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knowler WC, Barrett-Connor E, Fowler SE, Barrett-Connor E, Fowler SE, Hamman RF et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002; 346: 393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]