Abstract
Background
Children tend to be sedentary during the after-school hours, and this has deleterious effects on their health. The objective of the present study was to determine the effects of a 3-year after-school physical activity (PA) program, without restriction of dietary energy intake, on percent body fat (%BF), cardiorespiratory fitness (CRF), and cardiometabolic markers in children.
Methods
A cluster randomization design was employed. A total of 574 3rd grade children from 18 elementary schools in the southeastern United States participated. The intervention consisted of 80 minutes of age-appropriate moderate-to-vigorous PA each school day. The main outcomes of interest were %BF measured by dual-energy X-ray absorptiometry; CRF measured by heart rate in response to a submaximal step test; nonfasting total and high-density lipoprotein cholesterol (HDL-C); and resting blood pressure (BP).
Results
Intent-to-treat analyses showed significant treatment by time interactions for %BF (p=0.009) and CRF (p=0.0003). The change pattern of the means suggested that %BF and CRF in intervention children improved relative to control children during the school months, rebounding to the levels of control children over the summers following years 1 and 2. Year-by-year analyses of what occurred during the months when the program was offered revealed dose–response relations for %BF and CRF, such that the clearest beneficial effects were seen for those youth who attended at least 60% of the after-school sessions. No significant intervention effects were seen for cholesterol or BP.
Conclusions
An after-school PA program was effective in reducing adiposity and improving CRF, especially in the children who attended the sessions at least 3 days/week. However, the favorable effects on %BF and CRF were lost over the summer. Thus, it is critical to incorporate strategies that attract and retain the children to receive an adequate dose of PA year-round.
Trial Registration
Clinicaltrials.gov number, NCT00061841.
Introduction
A dramatic increase in childhood obesity has been observed in the United States1 and other developed countries over the last three decades.2 This increase can be partially attributed to an obesogenic environment during nonschool hours,3–5 including a lack of access to safe and supervised physical activity (PA) programs,5,6 popularity of video games,7 and preoccupation with electronic communication (e.g., text messaging, social media).8 The 2008 Physical Activity Guidelines for Americans recommend that school-aged children should engage in 60 minutes or more of PA daily, including muscle- and bone-strengthening activities, and vigorous PA at least 3 days/week.9 At present time, less than half of American children achieve the recommended amount of PA through school physical education (PE) and unstructured play throughout the day.10 Clearly, dramatic policy and environmental changes are required to increase children's participation in PA.11 Although many efforts are ongoing to increase PA during school hours,12 less has been done to test the effectiveness of programs delivered during after-school hours at schools and community recreation facilities.13 In addition to academic and social benefits,14,15 organized, structured after-school programs provide a unique opportunity to engage children in a large amount of moderate-to-vigorous PA (MVPA). These programs have access to trained school staff and well-maintained facilities while avoiding competition with academic pursuits.13,16
This paper reports the results of the Medical College of Georgia (MCG) FitKid Program (FitKid), a voluntary, no-fee, after-school obesity prevention program.17 The primary hypothesis was that FitKid would have a favorable effect on percent body fat (%BF) and cardiorespiratory fitness (CRF) in young children.
Methods
Study Design
This study was a cluster-randomized study with measurements at 1, 9, 13, 21, 25, and 33 months in a school district (66% African-American and 65% qualified for reduced price or free school lunches) with 36 elementary schools in the southeastern United States. To qualify, schools had to agree to be randomized and have PA facilities (e.g., a gym or multiuse room) available during after-school hours. Eighteen eligible schools agreed to participate in the study and were pair-matched by urban and nonurban (i.e., suburban/rural) locale and randomized. Participant recruitment took place from late spring in 2nd grade students to early fall in 3rd grade students in 2003. Additional recruitment occurred at the beginning of years 2 and 3 in schools with low enrollment. The study was approved by the MCG Human Assurance Committee.
Study Measures
The primary outcomes were %BF and CRF. %BF was assessed by dual-energy X-ray absorptiometry (DXA; Hologic QDR-4500W, Waltham, MA).18,19 CRF was assessed by heart rate (HR) at the completion of the YMCA submaximal bench-stepping test,20 which was chosen over the PACER21 due to its sensitivity to CRF-related changes in heart rate and ease of implementation in a mobile laboratory. We also measured height, weight, waist circumference (WC), nonfasting total cholesterol (TC), and high-density lipoprotein cholesterol (HDL-C), and resting blood pressure (BP) as secondary outcomes. Each year, participants also reported their participation in organized and unorganized PA programs (youth sport leagues, school organized sport teams, and individual sports) and sedentary activities during after-school hours as well as during summer breaks.
Physiologic data were collected by the research staff, who were not blind to the intervention condition, in a 38-foot mobile testing laboratory during early hours on school ground. Additional details of the study sample, design, and measurements have been previously provided elsewhere.17,22,23
Intervention Program
Built on our previous research with obese and nonobese youth,24–26 the FitKid after-school program reconstructed the block of time immediately after school when children are likely to engage in sedentary behaviors. The program was offered daily following the completion of regular school activities, under the supervision of two FitKid Instructors, during regular school days. Children were encouraged to attend at least 3 days/week to provide flexibility for them to attend other after-school activities. There was no minimum attendance requirement because it was a voluntary program. To make the program appealing to parents and school officials, FitKid also included a free snack (USDA after-school snack program),27 academic assistance (homework and study skills), and transportation to home by school bus. FitKid was designed in collaboration with school officials and teachers that allowed the utilization of school personnel, resources, and facilities, and thus increased its potential for translation and sustainability. Finally, we formed an advisory board consisting of parents, teachers, school principals, district officials, and community representatives who provided feedback and recommendations on the implementation of study protocol. The board met annually prior to the beginning of the school year.
The 120-minute structured after-school program began with 40 minutes for snacks and teacher-assisted homework and academic enrichment activities in a classroom. All participants were required to bring their homework assignment list with them, and this usually required 30–40 minutes to complete with FitKid instructors providing assistance to the students as needed. On Fridays, a day in which no homework was assigned, a lesson was provided with a health-related focus. The next 80 minutes consisted of 20-minute skill-based PA that incorporated skill instructions, 40-minute vigorous PA that used developmentally appropriate activities with a monthly theme, and 20-minute stretching/resistance training and cool down. The actual time for each segment varied depending on time used for activity transition. Children were not given the option to sit out during the PA time as a condition of attendance. The intensity goal for the 40-minute vigorous PA portion was to reach a HR of ≥150 beats/minute (bpm). To monitor the level of intensity, 50% of the children wore HR monitors each day.
The FitKid PA program was designed to teach sport skills and improve aerobic and musculosketical fitness following a mastery-oriented youth sport activity program philosophy that focuses on confidence building, enjoyment, team play, and learning skills and deemphasizes competition and winning. Monthly themes (e.g., fitness, dance, soccer, etc.) with session plans were developed annually based on the changes of developmental needs. FitKid Instructors followed the monthly themes and adapted the session plans based on the participants of their school. However, the time allocation of the after-school program components was strictly reinforced and monitored by research staff with scheduled and unannounced site visits.
FitKid Instructors consisted of PE teachers, classroom teachers, and paraprofessionals. All FitKid instructors participated in a 2-day workshop at the beginning of the study to learn the FitKid after-school intervention program and teaching strategies. They were required to attend two 1-day training sessions every year (at beginning of school years 2 and 3 and winter breaks). These workshops were used to: (1) Provide program updates, (2) introduce monthly activity themes and activity lesson plans, and (3) develop instructional skills and strategies. At the end of the year, a reception was held to show appreciation to the FitKid Instructors. This was also used as an opportunity to get feedback from the instructors on issues related to FitKid program delivery. On the basis of the feedback and process evaluation results, strategies were developed to improve implementation in the following year. With few exceptions, all FitKid instructors attended all training sessions and annual receptions. A senior PA specialist provided ongoing supervision of FitKid instructors and coordinated logistical issues with school officials. Other members of the research team had very limited contact with FitKid participants and instructors. Additional details of program rationale and design have been provided elsewhere.15
Statistical Analysis
Primary analyses were performed following the intent-to-treat (ITT) principle, in which the intervention status (control vs. intervention) was determined by the school of enrollment at baseline in year 1. Children were excluded from the analysis if they had crossover school migrations (i.e., intervention to control or control to intervention). Three percent of data points were excluded from analysis due to crossover school migrations.
General linear models are typically used in ITT analysis of obesity prevention trials with two measurement points (baseline and posttest).28,29 The FitKid intervention was implemented over 3 school years with six measurement points and encountered a complicated set of confounding factors, such as participant attrition and migration, annual fluctuation of program attendance, effects of program suspension during summer, differences in growth and maturation, changes of school environments, and secular trends of society. To reduce potential confounds and examine the effect of program exposure, we used a three-step analysis plan combining a 3-year longitudinal and three single-year analyses, instead of relying entirely on an ITT analysis. In step 1, we used a mixed-model analysis of variance for repeated measures using SAS PROC MIXED to determine if the intervention influenced the pattern of means over the six measurement points. Inclusion in this analysis required a valid measure of %BF at baseline in year 1. The statistic of interest was the significance of the treatment by time intervention. In step 2, we examined the intervention effect of a single year to see if the intervention altered %BF and CRF during the school months when the after-school program was in session, as well as when the program was not offered during summer break. At step 3, we investigated how the levels of participation in FitKid [attendance rate of ≥2 days/week (40%) and ≥3 days/week (60%)] affected the outcomes. Children recruited in years 2 and 3 were included in steps 2 and 3 analyses.
In all analyses, a priori contrasts were constructed to test equality of mean differences from baseline (month 1) with a follow-up measurement time. We also included as fixed effects covariates, including ethnicity, gender, age, a proxy of socioeconomic status (SES; paid vs. free/reduced price lunch), and residence (urban vs. nonurban). Only significant covariates were retained in the models. A random term representing school was included in the models to account for the nesting effect due to randomization by school. Adjusted means (least-square means) and 95% confidence intervals (95% CI) were calculated. Statistical significance was set at alpha ≤0.05 (two-tailed test). SAS, version 9.2 was used for all analyses.
Results
Study Participant Enrollment and Retention
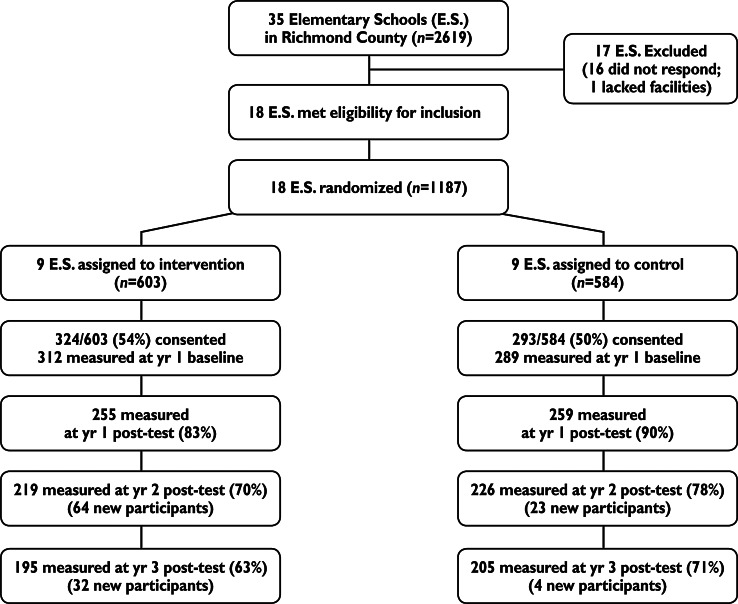
Figure 1 shows the flow of the participants at each measurement point, including those recruited in years 2 and 3. Parental consent and child assent were obtained from 614 children at baseline in year 1 of the study, representing a participation rate of 52% of all eligible children, of which 601 were tested and a valid measure of %BF was obtained from 574 participants. Participant retention rate (calculated for those with year 1 baseline data) was 86%, 74%, and 67% at the end of years 1, 2, and 3, respectively. The sample provided adequate statistical power (over 80%) to test the primary study hypothesis (0.5 unit of standard deviation).17 It was difficult to assess the reasons for missing data at each follow-up time point (i.e., lost to follow-up or discontinued intervention) in this study because children were allowed to rejoin the program at any time after absence from the study. Frequent change of schools within same school year (20–25%) also made the tracking difficult. Children were tested as long as they attended a study school. Children were allowed to continue their participation in the FitKid program if they moved from an intervention school to another intervention school. As an incentive, participants received up to $50/year for participating in data collection, whereas each school received $2000 annually in its general fund account. All schools remained in the study for the entire study period.
Figure 1.
Flow diagram of study participants.
Experimental Control Checks and Program Implementation
Table 1 displays the characteristics of study participants and sample size included in longitudinal ITT and annual analyses. There were no significant differences in demographic characteristics between control and intervention groups except percent of minority children in years 2 and 3. Previously, we have reported that there were no differences in study outcome and demographic variables between intervention and control schools at baseline in year 1, except children in intervention schools had higher TC than children in control schools.30 We observed no consistent patterns to distinguish the self-reported lifestyle related behaviors during after-school hours and PA and sedentary activities during summer break between control and intervention children (data not shown).
Table 1.
Characteristics of Study Participants Included in Longitudinal Intent-to-Treat and Annual Analyses at Baseline
| |
|
Annual analysis |
|||||
|---|---|---|---|---|---|---|---|
| |
Longitudinal intent-to-treat analysis |
Control |
Intervention |
||||
| Year 1 baseline | Year 1 | Year 2 | Year 3 | Year 1 | Year 2 | Year 3 | |
| Sample size (n)a | 576 | 284 | 251 | 219 | 292 | 276 | 262 |
| White (%)b | 32 | 35 | 34 | 36 | 28 | 25 | 26 |
| Males (%) | 47 | 48 | 46 | 44 | 47 | 48 | 48 |
| Age (yr; mean/SD) | 8.7/0.5 | 8.7/0.5 | 9.7/0.5 | 10.7/0.5 | 8.7/0.6 | 9.8/0.6 | 10.8/0.6 |
| Qualified for school lunch program (%) | 64 | 62 | 67 | 64 | 66 | 72 | 69 |
The number of children in each school ranged from 11 to 45, 7 to 48, and 5 to 45 at the beginning of years 1, 2, and 3, respectively.
African-American participants were grouped with other small minority group participants in all analysis.
SD, Standard deviation.
Table 2 shows attendance rates in the after-school program, which decreased across years with lower attendance in spring terms. There were no significant gender, race, or residence differences in attendance rates. The average HR (medians/ranges) from each intervention school during the vigorous PA portion consistently exceeded 150 bpm, which has been linked to significant improvements in body composition and cardiometabolic risk measures (see Table 2).24 Finally, the incident rate of adverse events are displayed in Table 2. The rates were lower than those previously reported.31
Table 2.
Attendance Rates, Medians, and Ranges of Levels of Activity Intensity, and Rates of Adverse Events in FitKid After-School Program
| |
Year 1 |
Year 2 |
Year 3 |
|||
|---|---|---|---|---|---|---|
| Fall | Spring | Fall | Spring | Fall | Spring | |
| Attendance rate (%) | 55 | 43 | 50 | 38 | 41 | 35 |
| Nonrural | 49 | 37 | 49 | 39 | 46 | 36 |
| Rural | 62 | 49 | 52 | 37 | 38 | 33 |
| White | 55 | 38 | 41 | 29 | 30 | 24 |
| Black | 54 | 43 | 50 | 38 | 45 | 39 |
| Male | 55 | 44 | 51 | 39 | 38 | 33 |
| Female | 56 | 43 | 50 | 37 | 44 | 36 |
| Participants with ≥40% attendance (%) | 67 | 52 | 61 | 46 | 51 | 44 |
| Participants with ≥60% attendance (%) | 48 | 40 | 44 | 29 | 34 | 30 |
| Average heart rates (bpm) during 80-min physical activity sessiona | 155 (146, 158) | 152 (145, 156) | 153 (147, 161) | 151 (145, 157) | 148 (144, 153) | |
| Average heart rates (bpm) during 20-min skills segment | 148 (135, 152) | 141 (134, 157) | 147 (134, 159) | 141 (129, 151) | 141 (130, 144) | |
| Average heart rates (bpm) during 40-min aerobic segment | 158 (153, 163) | 157 (150, 161) | 156 (153, 165) | 155 (148, 166) | 154 (149, 161) | |
| Incident rate of adverse events | 0.03 (20 mild; 3 moderate; 1 severe) | 0.02 (4 mild; 6 moderate; 2 severe) | 0.01 (5 mild; 2 severe) | |||
Activity intensity data not available for each school term in year 1.
bpm, beats per minute.
Previously, we have reported the cost to deliver the FitKid after-school program ($558 per student) in year 1 of the study.32 Staffing (63%) and transportation (23%) were the most expensive items. The cost was estimated to be lower in years 2 and 3 due to reduced cost in equipment and fewer program participants. The per-person cost was similar to those previously reported in after-school programs.33
Influence on the Outcome Measures
Table 3 shows the means and standard deviations over six measurement points and results of step 1 analyses on the primary and secondary outcome measures as well as the intraclass correlations. The reliability of the measurements were strongest for %BF and anthropometric measures (≥0.90), moderate for CRF (≥0.58), and low for the cardiometabolic biomarkers.
Table 3.
Means (Standard Deviations) and Intraclass Correlations of Study Outcome Measures and Model Statistics Comparing the Trends Between Control (C) and Intervention Schools (I) over Six Measurement Time Points
| Year 1 baseline (month 1) | Year 1 posttest (month 9) | Year 2 baseline (month 13) | Year 2 posttest (month 20) | Year 3 baseline (month 24) | Year 3 posttest (month 33) | ICC | F/pvalue for treatment – time interaction term | ||
|---|---|---|---|---|---|---|---|---|---|
| Percent body fat | C | 26.66 (9.69) | 26.96 (9.70) | 27.56 (9.48) | 27.73 (9.42) | 29.05 (9.74) | 27.44 (9.40) | 0.94 | F=3.10 |
| (%)a | I | 26.00 (9.07) | 25.53 (9.27) | 26.89 (9.59) | 26.32 (10.04) | 28.15 (10.37) | 27.23 (9.84) | p=0.009 | |
| Contrast estimate (SE) | −0.33 (0.21) | 0.03 (0.28) | −0.44 (0.19) | 0.26 (0.38) | 0.54 (0.43) | ||||
| p value | 0.11 | 0.91 | 0.19 | 0.49 | 0.21 | ||||
| Cardiorespiratory | C | 162.17 (17.46) | 160.52 (15.72) | 161.83 (17.04) | 159.25 (18.44) | 162.2 (19.21) | 160.55 (17.84) | 0.58 | F=4.74 |
| fitness (bpm)b,c | I | 159.25 (17.84) | 154.06 (20.31) | 161.45 (18.33) | 156.98 (20.53) | 162.81 (21.61) | 158.26 (19.20) | p<0.001 | |
| Contrast estimate (SE) | −2.87 (1.39) | 2.87 (1.53) | 1.39 (1.58) | 4.32 (1.65) | 0.70 (1.65) | ||||
| p value | 0.039 | 0.062 | 0.38 | 0.009 | 0.67 | ||||
| Weight (kg)a,e | C | 34.30 (10.28) | 37.14 (11.38) | 39.18 (11.58) | 42.24 (12.87) | 44.81 (13.88) | 47.83 (14.88) | 0.95 | F=1.92 |
| I | 34.74 (11.39) | 37.06 (12.35) | 40.21 (13.53) | 43.22 (14.92) | 46.03 (16.20) | 49.77 (17.02) | p=0.09 | ||
| Contrast estimate (SE) | –0.24 (0.20) | 0.23 (0.30) | 0.29 (0.40) | 0.83 (0.50) | 1.01 (0.59) | ||||
| p value | 0.24 | 0.45 | 0.47 | 0.095 | 0.087 | ||||
| Height (cm)d,e | C | 133.03 (6.72) | 136.57 (7.01) | 138.96 (7.17) | 143.03 (7.58) | 145.65 (7.68) | 149.53 (8.02) | 0.96 | F=0.94 |
| I | 133.55 (7.81) | 137.26 (8.27) | 140.41 (8.58) | 144.39 (8.66) | 146.77 (8.72) | 151.20 (8.85) | p=0.45 | ||
| Contrast estimate (SE) | 0.09 (0.11) | 0.16 (0.17) | 0.22 (0.22) | 0.04 (0.27) | 0.18 (0.32) | ||||
| p value | 0.40 | 0.33 | 0.31 | 0.88 | 0.58 | ||||
| BMI z-scoree | C | 0.78 (1.07) | 0.78 (1.10) | 0.74 (1.09) | 0.76 (1.10) | 0.76 (1.13) | 0.70 (1.13) | 0.96 | F=1.78 |
| I | 0.76 (1.10) | 0.67 (1.11) | 0.69 (1.21) | 0.67 (1.19) | 0.71 (1.25) | 0.72 (1.17) | p=0.12 | ||
| Contrast estimate (SE) | −0.04 (0.02) | –0.03 (0.03) | –0.03 (0.04) | 0.02 (0.04) | 0.05 (0.05) | ||||
| p value | 0.075 | 0.30 | 0.39 | 0.62 | 0.28 | ||||
| Waist circumference | C | 62.37 (10.36) | 63.98 (10.86) | 65.32 (10.81) | 67.37 (12.92) | 67.72 (11.86) | 67.51 (11.64) | 0.90 | F=2.52 |
| (cm)e | I | 62.67 (10.86) | 63.62 (11.11) | 65.85 (12.24) | 67.31 (12.96) | 68.74 (14.18) | 68.90 (13.27) | p=0.03 | |
| Contrast estimate (SE) | −0.26 (0.42) | 0.17 (0.50) | −0.53 (0.53) | 0.89 (0.50) | 1.05 (0.58) | ||||
| p value | 0.54 | 0.73 | 0.32 | 0.073 | 0.072 | ||||
| TC/HDL ratioc | C | 2.89 (0.71) | 3.28 (0.90) | 3.64 (1.27) | 3.68 (1.23) | 3.59 (1.16) | 3.44 (1.07) | 0.49 | F=0.45 |
| I | 3.04 (0.93) | 3.30 (1.16) | 3.65 (1.22) | 3.69 (1.20) | 3.69 (1.35) | 3.61 (1.53) | p=0.82 | ||
| Contrast estimate (SE) | −l0.06 (0.11) | −0.05 (0.12) | −0.10 (0.12) | 0.05 (0.12) | 0.03 (0.12) | ||||
| p value | 0.55 | 0.66 | 0.41 | 0.68 | 0.80 | ||||
| Systolic blood | C | 110.30 (9.02) | 107.79 (9.36) | 108.97 (9.96) | 108.98 (8.16) | 108.31 (8.94) | 110.98 (8.62) | 0.55 | F=1.47 |
| pressure (mmHg)b,d | I | 110.60 (9.55) | 106.60 (10.17) | 109.93 (9.26) | 109.28 (9.63) | 109.29 (8.89) | 111.48 (9.49) | p=0.20 | |
| Contrast estimate (SE) | −1.17 (0.75) | 1.10 (0.84) | −0.12 (0.87) | −0.06 (0.87) | −0.25 (0.92) | ||||
| p value | 0.12 | 0.19 | 0.89 | 0.94 | 0.79 | ||||
| Diastolic blood | C | 66.14 (4.97) | 64.69 (5.59) | 65.42 (5.76) | 65.57 (5.11) | 64.78 (4.95) | 66.04 (4.78) | 0.42 | F=0.75 |
| pressure (mmHg)d | I | 65.89 (5.21) | 63.84 (6.35) | 65.15 (6.11) | 65.10 (5.33) | 65.08 (5.08) | 66.06 (5.58) | p=0.59 | |
| Contrast estimate (SE) | −0.52 (0.50) | 0.17 (0.55) | −0.36 (0.56) | 0.44 (0.57) | 0.04 (0.55) | ||||
| p value | 0.29 | 0.77 | 0.52 | 0.44 | 0.94 |
Model adjusted for sex, race, age, economic disadvantage status, and their interactions with intervention status. Only significant effects are included in the model. A priori contrasts were used to compare the changes from year 1 pretest (month 0) at each time point.
Male<female; bMale>female; cWhite>non-white; dWhite<non-white; eIncreases with age.
SE, Standard error; bpm, beats per minute;TC, total cholesterol; HDL-C, high-density lipoprotein cholesterol.
Significant treatment by time interactions was seen for %BF, CRF, and WC, suggesting that the intervention significantly affected these measures over the six measurement points. Further examination of the patterns of means of %BF, CRF, and WC showed that the children in the intervention group improved during the months when school was in session and rebounded to levels similar to those of the control group following the summer months. The interaction terms for biomarkers, weight, and BMI were nonsignificant (data not shown).
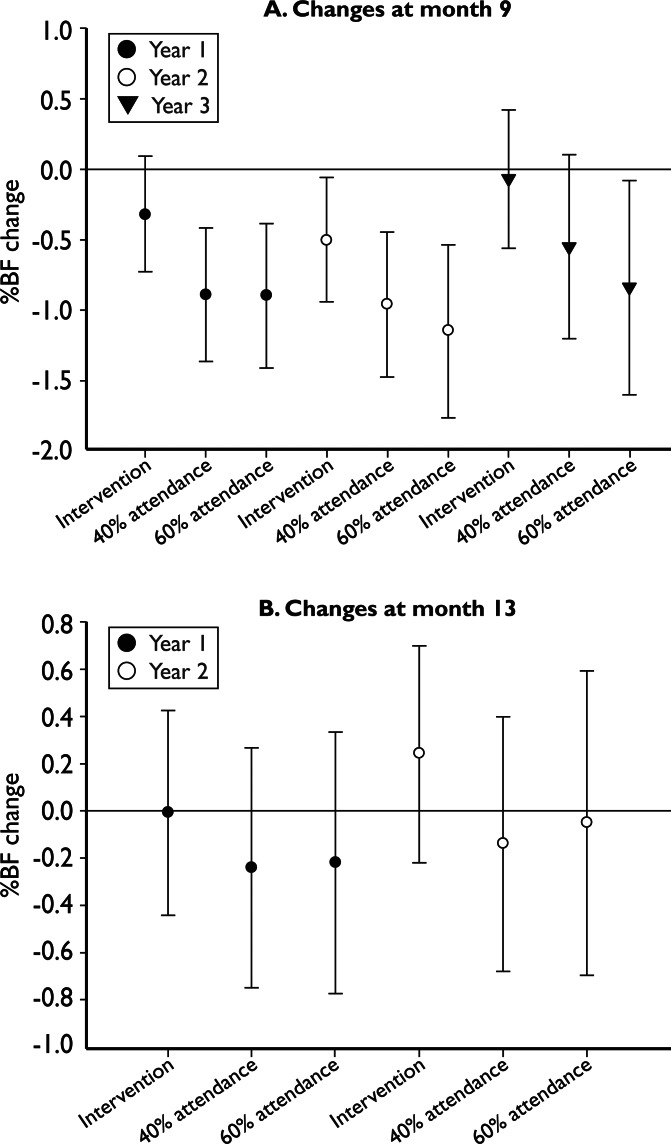
The annual analysis in step 2 showed that intervention children had a smaller gain in %BF, which reached significance only at the end of year 2 (see Fig. 2). In step 3 of the analyses, the increase of %BF was significantly smaller at the end of the school year (month 1 vs. month 9) in intervention children who attended 40% and 60% of FitKid sessions in all 3 years, with the exception of the 40% attendance group in year 3. The difference dissipated after the summer months (month 1 vs. month 13).
Figure 2.
Adjusted changes and 95% confidence intervals of percent body fat (%BF) of all children in intervention schools (Intervention), children with ≥40% attendance (40% attendance), and children with ≥60% attendance (60% attendance), in comparison with children in control schools at month 9 (a) and month 13 (b).
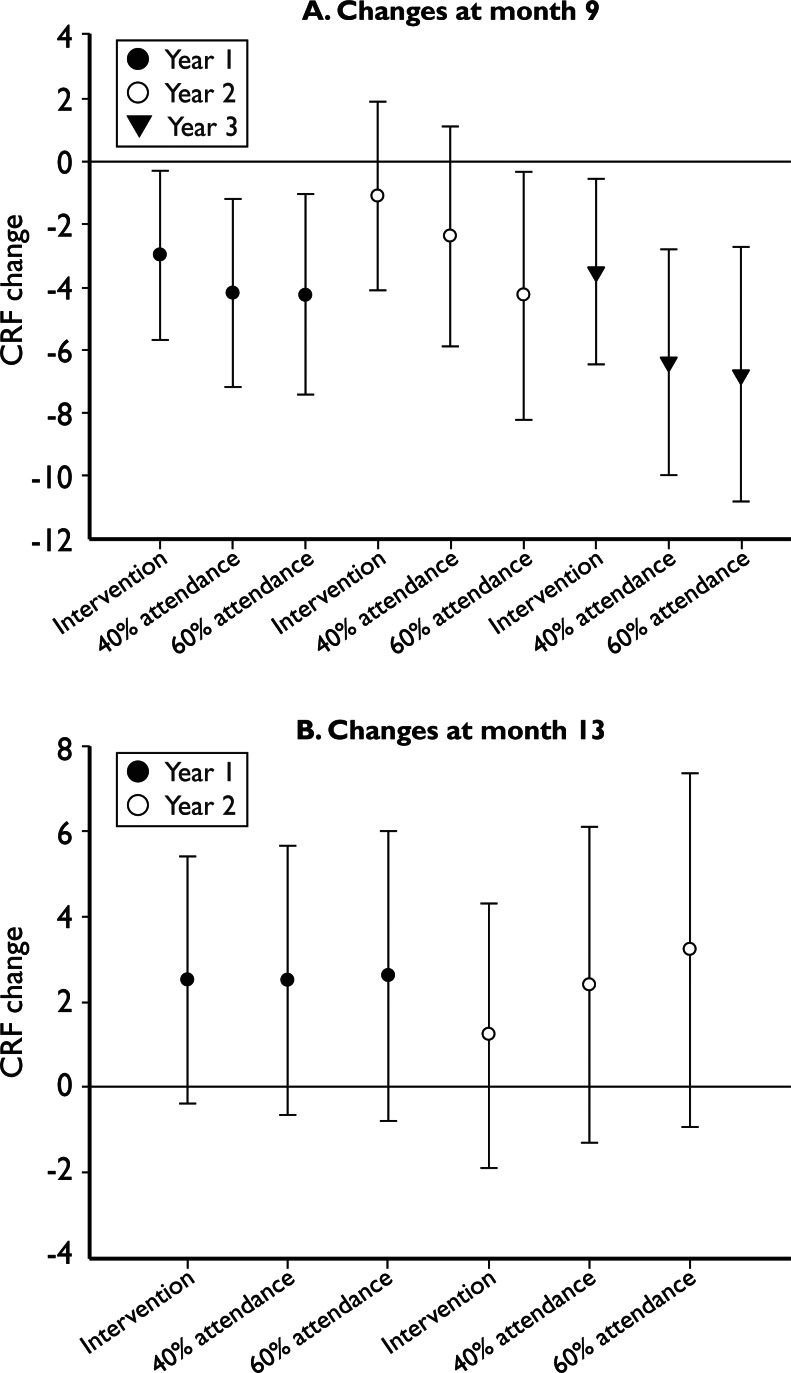
The analysis for CRF revealed similar patterns to those of %BF; compared to the control group, children in the intervention group had significant improvements in CRF during school years 1 and 3, and a decrease over the summers in step 2 analyses (see Fig. 3). The patterns were repeated in step 3 analysis; the magnitudes of improvement in CRF were greater in those with higher attendance. Results for WC were similar to %BF and CRF and not shown here.
Figure 3.
Adjusted changes and 95% confidence intervals of cardiorespiratory fitness (CRF; beats per minute) of all children in intervention schools (Intervention), children with ≥40% attendance (40% attendance), and children with ≥60% attendance (60% attendance), in comparison with children in control schools at month 9 (a) and month 13 (b).
Discussion
To our knowledge, this is the first longitudinal, randomized study with a direct measure of adiposity over six measurement points that examined the effectiveness of an after-school obesity prevention program in a large sample of elementary school children.13 Another strength of the study is that the fidelity of the study design and intervention implementation was assessed with process evaluation data, which are often not reported. Following a three-step analysis strategy, the data provided support for the primary study hypothesis that body fatness and CRF of elementary school children can be favorably influenced by a program that emphasizes vigorous PA, without any attempt to restrict energy intake, over a 3-year period. However, the FitKid impact was lost during the summer months when the program was not offered. When a criterion of exposure to the intervention was applied, children who attended at least 40% of the intervention sessions showed especially clear benefits.
The step 1 analysis revealed a general trend over 3 years that favored the intervention children. However, in the third year, favorable changes were smaller in the intervention group and favorable changes occurred unexpectedly in the control group. There is no clear explanation for this finding. We speculate that the reduced program impact can be partly attributed to lower FitKid program attendance in the third year. Children of this age start developing nonsport interests and hobbies, which inevitably will take them away from PA-oriented programs. Societal secular trends may have led to changes in PA and diet in control schools.1 A similar reduction in obesity in control participants was reported in the recently completed HEALTHY study.28,34 Finally, children in our study started entering puberty during year 3 of the study. Maturation exerts powerful, but varied, influences on body composition and CRF, depending on gender and race/ethnic group,35–37 and might have masked the intervention effect.38 We planned, but did not collect, self-rated physical maturation data from the children. We were advised by our community advisory board and some school principals that having the youth rate their maturation level by viewing drawings that depicted pubic hair and breast development would cause some schools to drop out of the project.
It is important to note that we observed favorable but nonsignificant effects on BMI in the intervention group. Because MVPA can increase fat-free mass and bone mass, using BMI to assess the effect of a PA intervention on body fatness may produce misleading results. There were no significant intervention effects on the cardiometabolic biomarkers (e.g., lipids, BP) and anthropometric measures. This is consistent with findings from other lifestyle intervention studies in nonobese school-aged children.28,39,40 It appears that PA has a clear effect on biomarkers in obese youth who start with unfavorable biomarker values, but does not show clear effects on nonobese youth.28,39,40 A higher dose of PA and/or dietary intervention may be needed to induce favorable changes in cardiometabolic biomarkers.39
The results of the annual analyses (step 2 analyses) showed significant intervention effects in %BF (only in year 2) and CRF (in years 1 and 3) over the 9-month intervention periods. The program impacts became more apparent and consistent with increased attendance in the step 3 analysis. A 40% attendance is equivalent to adding at least 160 minutes/week of MVPA or 80 minutes/week of vigorous PA to the amount of PA (30 minutes/day) that might be obtained from PE and/or recess activities offered at school (daily PE was offered at the participating schools). As a result, children in the FitKid intervention schools had the opportunity to accumulate enough PA to meet the minimum PA recommendation (≥60 minutes/day). At 60% attendance, FitKid could add 240 minutes/week of MVPA or 120 minutes/week of vigorous PA. We and others have previously reported similar findings with respect to the dose of PA that produced favorable changes in body composition and fitness in children, without dietary intervention.25,26,41–43 In the past few years, a large number of laws and policies addressing obesity and PA have been introduced and enacted.11 However, most of them have called for 30 minutes of MVPA a day, which by itself may not generate the amount of PA sufficient to influence body composition in children.9
Questions may be raised concerning the sustainability and generalizability of the FitKid program. It is important to note that we designed the FitKid project as a research study to determine whether such an after-school program could have favorable effects on fatness and fitness. Our results suggest that a program that provides a sufficient dose of MVPA, without restriction of energy intake, can enhance body composition and fitness. This study is not able to cast light on the biologic mechanisms underlying this effect. One possibility is that the PA increased total energy expenditure, thereby reducing total body energy content; however, the absence of a significant effect on BMI suggests that an explanation focusing on body composition, rather than body weight, might be more appropriate. Another possibility is that the mechanical stimulation of the vigorous PA stimulated immature stem cells to preferentially differentiate into lean tissue, rather than fat tissue.44
It should be noted that this study did not collect data to assess factors influencing children's participation in the FitKid program. It is possible that the intensive nature of the physical activities may have been unappealing to a substantial proportion of the youth as compared to other activities they might have selected for the after-school hours. These are important questions that need to be addressed to help in the design of future public health interventions. The next step is to incorporate our results, along with those of other investigators, into health promotion programs that will be optimally effective in enhancing the body composition and fitness of our youth.
After-school PA programs can be implemented with staff training using resources that currently are in existence in most communities, while these facilities and equipment in schools are generally underutilized during after-school hours, weekends, holidays, and school breaks.13 According to information compiled by After-school Alliance,45 an overwhelming majority of parents expressed difficulties in accessing quality after-school programs in their communities. Successful after-school programs require consistent supervised structure, well-qualified and well-trained staff, and involvement of community partners, and they must be responsive to needs and interests of both participating children and parents.5,46 However offering such programs to all school-aged children, especially in low-resource communities, requires funding, training, and expertise that may be unavailable and difficult to obtain. Despite these challenges, states such as North Carolina have recently recommended that all after-school programs spend a minimum of 20% of the program time engaged in MVPA, with physical activity programs dedicating 80% of program time to MVPA.43
The rebound effect due to program discontinuity during the summer breaks, which has been shown by others,47 is noteworthy. This implies that gains achieved in the 9 months of a school year can be lost during the 3 months of summer. Based on self-report, children in both the intervention and control schools stayed inactive during the summer. According to information gathered from our formative study,30 we speculate that it was most likely the result of lack of access to safe, supervised, and low-cost PA programs in their neighborhoods during summertime.48 The availability and accessibility to safe and supervised PA are paramount to promote and facilitate year-round, regular participation to meet the PA recommendations in this age group.5 Policy makers must find ways to fund and implement such programs for young children, especially in low-income communities.
Several weaknesses limit the internal and external validity of this study. First, we were unable to assess the reasons of discontinuation in FitKid because children were allowed to rejoin the program freely. It was likely that only the most PA-oriented children regularly attended the program over the years and benefited from it. Second, to overcome the transportation barrier, we used school buses to send children home after the program; this was costly and logistically challenging to the school officials, and may be difficult to implement in community programs.32 Third, the step 3 analyses relied on levels of attendance that were not randomly assigned and therefore were not experimentally controlled dose–effect analyses. Nonetheless, the results are consistent with those found in other voluntary after-school programs.26,42,49 Finally, the FitKid intervention focused primarily on increasing PA with little attention to nutrition. We did offer snacks through the USDA snack program that might have had a modest and unmeasured effect on diet. There is some evidence that interventions combining PA and dietary modifications are most effective in reducing obesity in children.50,51
If you build it, will they come? The average attendance in FitKid decreased from 47% in year 1 (2.3 days/week) to 35% (1.5 days/week) in year 3. Although data are limited, typical voluntary, paid or subsidized after-school programs have shown enrollments of approximately 50% and attendance rates ranging from 1.9 to 2.4 days/week when offered daily in low SES elementary schools in the United States.33,52 Reviews of successful non-PA afterschool programs showed that significant impacts on the study outcome measures (e.g., academic performance, delinquency, and self-concepts) have been observed with attendance rates of 2–3 days/week.33,46 The declining trend in FitKid attendance was consistent with the general age-related decline in participation of sport and PA in youth.53
Conclusions
We conclude that the FitKid after-school program represents a promising approach to meet the recommended amount of MVPA for prevention of childhood obesity. The FitKid study was a translation study designed to examine what would happen to body composition and fitness if such a program were offered in an after-school setting. We found that youth who participated at least 2 days/week, without any dietary intervention, obtained a beneficial result during the period of exposure. On the other hand, beneficial results were lost during the summer breaks. Although it is not expected that the FitKid program can be adopted in whole by any community or school system, the findings from our study can be informative for researchers and health promotion specialists in formulating their future projects or interventions. For example, research is needed to improve our understanding of how to attract and retain participants in such programs and how to offer such programs through holidays and school breaks in all communities. It can also be fruitful to replicate the FitKid program in other sustainable after-school settings in the community.
Notes
Please contact the first author for a copy of the FitKid Intervention Manual and Testing Manual, which provide information on program administration, intervention activities, staff training, and process evaluation.
Acknowledgments
We want to express our appreciation to Dr. Paule Barbeau, Dr. John Hanes, Ms. Janet Thornburg, and Ms. Elizabeth Stewart for their assistance in program implementation, coordination of data collection, data management, and the FitKid schools, teachers, and participants for their participation. We also want to thank Dr. Tom Baranowski, Dr. Ken Resnicow, and Dr. Alice Yan for their consultation and guidance in the design, implementation, and data analysis of this study. This study was funded by the National Institutes of Health National Institute of Diabetes and Digestive and Kidney Diseases (DK063391).
Dr. Yin was responsible for the conception and design of the study, drafting of the manuscript, and obtaining funding for the project. Dr. Yin had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Dr. Moore was responsible for acquisition of data, drafting of the manuscript, and administrative support. Mrs. Johnson was responsible for analysis and interpretation of data, drafting of the manuscript, and technical support. Mrs. Vernon was responsible for acquisition of data, critical revision of the manuscript for important intellectual content, and administrative support. Dr. Gutin was responsible for the conception and design of the study, drafting of the manuscript, and obtaining funding for the project.
Author Disclosure Statement
No financial disclosures are reported by the authors of this paper. None of the authors has a known conflict of interest, financial or otherwise that would affect the analysis or interpretation of the data presented within this manuscript. This study was funded by the National Institutes of Health (DK063391).
References
- 1.Ogden CL. Carroll MD. Curtin LR, et al. Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA. 2010;303:242–249. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 2.de Wilde JA. van Dommelen P. Middelkoop BJC, et al. Trends in overweight and obesity prevalence in Dutch, Turkish, Moroccan and Surinamese South Asian children in the Netherlands. Arch Dis Child. 2009;94:795–800. doi: 10.1136/adc.2009.163709. [DOI] [PubMed] [Google Scholar]
- 3.Temple JL. Giacomelli AM. Kent KM, et al. Television watching increases motivated responding for food and energy intake in children. Am J Clin Nutr. 2007;85:355–361. doi: 10.1093/ajcn/85.2.355. [DOI] [PubMed] [Google Scholar]
- 4.Blass E. Anderson D. Kirkorian H, et al. On the road to obesity: Television viewing increases intake of high-density foods. Physiol Behav. 2006;88:597–604. doi: 10.1016/j.physbeh.2006.05.035. [DOI] [PubMed] [Google Scholar]
- 5.Moore JB. Schneider L. Lazorick S, et al. Rationale and development of the Move More North Carolina: Recommended standards for after-school physical activity. J Public Health Manag Pract. 2010;16:359–366. doi: 10.1097/PHH.0b013e3181ca2634. [DOI] [PubMed] [Google Scholar]
- 6.Molnar BE. Gortmaker SL. Bull FC, et al. Unsafe to play? Neighborhood disorder and lack of safety predict reduced physical activity among urban children and adolescents. Am J Health Promot. 2004;18:378–386. doi: 10.4278/0890-1171-18.5.378. [DOI] [PubMed] [Google Scholar]
- 7.Vandewater E. Shim M. Caplovitz A. Linking obesity and activity level with children's television and video game use. J Adolesc. 2004;27:71–85. doi: 10.1016/j.adolescence.2003.10.003. [DOI] [PubMed] [Google Scholar]
- 8.Vandelanotte C. Sugiyama T. Gardiner P, et al. Associations of leisure-time internet and computer use with overweight and obesity, physical activity and sedentary behaviors: Cross-sectional study. J Med Internet Res. 2009;11:e28. doi: 10.2196/jmir.1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Physical Activity Guidelines Advisory Committee. Department of Health and Human Services; Washington, DC: 2008. Physical Activity Guidelines Advisory Committee Report. [Google Scholar]
- 10.Troiano R. Berrigan D. Dodd K, et al. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40:181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 11.Beighle A. Beets MW. Erwin HE, et al. Physical activity promotion in afterschool programs. Afterschool Matters. 2010;11:24–35. [Google Scholar]
- 12.Beighle A. Morgan C. Le Masurier G, et al. Children's physical activity during recess and outside of school. J Sch Health. 2006;76:516–520. doi: 10.1111/j.1746-1561.2006.00151.x. [DOI] [PubMed] [Google Scholar]
- 13.Beets M. Beighle A. Erwin H, et al. After-school program impact on physical activity and fitness: A meta-analysis. Am J Prev Med. 2009;36:527–537. doi: 10.1016/j.amepre.2009.01.033. [DOI] [PubMed] [Google Scholar]
- 14.Scully D. Kremer J. Meade MM, et al. Physical exercise and psychological well being: A critical review. Br J Sports Med. 1998;32:111–120. doi: 10.1136/bjsm.32.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Scott-Little C. Hamann MS. Jurs SG. Evaluations of after-school programs: A meta-evaluation of methodologies and narrative synthesis of findings. Am J Eval. 2002;23:387–419. [Google Scholar]
- 16.Huberty J. Balluff M. O'Dell M, et al. From good ideas to actions: A model-driven community collaborative to prevent childhood obesity. Prev Med. 2010;50(Suppl 1):S36–S43. doi: 10.1016/j.ypmed.2009.08.013. [DOI] [PubMed] [Google Scholar]
- 17.Yin Z. Hanes J., Jr. Moore JB, et al. An after-school physical activity program for obesity prevention in children: The Medical College of Georgia FitKid Project. Eval Health Prof. 2005;28:67–89. doi: 10.1177/0163278704273079. [DOI] [PubMed] [Google Scholar]
- 18.Gutin B. Litaker M. Islam S, et al. Body-composition measurement in 9–11-y-old children by dual-energy X-ray absorptiometry, skinfold-thickness measurements, and bioimpedance analysis. Am J Clin Nutr. 1996;63:287–292. doi: 10.1093/ajcn/63.3.287. [DOI] [PubMed] [Google Scholar]
- 19.Litaker M. Barbeau P. Humphries M, et al. Comparison of Hologic QDR-1000/W and 4500W DXA scanners in 13- to 18-year olds. Obes Res. 2003;11:1545–1552. doi: 10.1038/oby.2003.206. [DOI] [PubMed] [Google Scholar]
- 20.Golding LA. YMCA Fitness Testing and Assessment Manual. 4th. Human Kinetics; Champaign, IL: 2000. [Google Scholar]
- 21.FITNESSGRAM Test Administration Manual. In: Meredith M, editor; Welk G, editor. Human Kinetics; Champaign, IL: 2004. [Google Scholar]
- 22.Yin Z. Davis CL. Moore JB, et al. Physical activity buffers the effects of chronic stress on adiposity in youth. Ann Behav Med. 2005;29:29–36. doi: 10.1207/s15324796abm2901_5. [DOI] [PubMed] [Google Scholar]
- 23.Yin Z. Gutin B. Johnson MH, et al. An environmental approach to obesity prevention in children: MCG FitKid Project year 1 results. Obes Res. 2005;13:2153–2161. doi: 10.1038/oby.2005.267. [DOI] [PubMed] [Google Scholar]
- 24.Gutin B. Barbeau P. Yin Z. Exercise interventions for prevention of obesity and related disorders in youths. Quest. 2004;56:120–141. [Google Scholar]
- 25.Howe CA. Harris RA. Gutin B. A 10-month physical activity intervention improves body composition in young black boys. J Obes. 2011:2011. doi: 10.1155/2011/358581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Barbeau P. Johnson MH. Howe CA, et al. Ten months of exercise improves general and visceral adiposity, bone, and fitness in black girls. Obesity. 2007;15:2077–2085. doi: 10.1038/oby.2007.247. [DOI] [PubMed] [Google Scholar]
- 27.United States Department of Agriculture (USDA) Afterschool Snack Program. 2004. www.fns.usda.gov/cnd/Afterschool/default.htm/ [Dec 17;2011 ]. www.fns.usda.gov/cnd/Afterschool/default.htm/
- 28.HEALTHY Study Group. Foster GD. Linder B. Baranowski T, et al. A school-based intervention for diabetes risk reduction. N Engl J Med. 2010;29:443–453. doi: 10.1056/NEJMoa1001933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stevens J. Murray DM. Catellier DJ, et al. Design of the Trial of Activity in Adolescent Girls (TAAG) Contemp Clin Trials. 2005;26:223–233. doi: 10.1016/j.cct.2004.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yin Z. Moore JB. Johnson MH, et al. The Medical College of Georgia FitKid Project: The relations between program attendance and changes in outcomes in year 1. Int J Obes Relat Metab Disord. 2005;29:S40–S45. doi: 10.1038/sj.ijo.0803061. [DOI] [PubMed] [Google Scholar]
- 31.Backx FJG. Erich WBM. Kemper ABA, et al. Sports injuries in school-aged children. Am J Sports Med. 1989;17:234–240. doi: 10.1177/036354658901700214. [DOI] [PubMed] [Google Scholar]
- 32.Wang LY. Gutin B. Barbeau P, et al. Cost-effectiveness of a school-based obesity prevention program. J Sch Health. 2008;78:619–624. doi: 10.1111/j.1746-1561.2008.00357.x. [DOI] [PubMed] [Google Scholar]
- 33.Kane TJ. William T. Grant Foundation; New York: 2004. The Impact of After-School Programs: Interpreting the Results of Four Recent Evaluations. [Google Scholar]
- 34.Kaufman F. Hirst K. Buse J, et al. Effect of secular trends on a primary prevention trial: The HEALTHY Study experience. Childhood Obes. 2011;7:291–297. [Google Scholar]
- 35.Phillips SM. Bandini LG. Compton DV, et al. A longitudinal comparison of body composition by total body water and bioelectrical impedance in adolescent girls. J Nutr. 2003;133:1419–1425. doi: 10.1093/jn/133.5.1419. [DOI] [PubMed] [Google Scholar]
- 36.Freedman DS. Serdula MK. Srinivasan SR, et al. Relation of circumferences and skinfold thicknesses to lipid and insulin concentrations in children and adolescents: The Bogalusa Heart Study. Am J Clin Nutr. 1999;69:308–317. doi: 10.1093/ajcn/69.2.308. [DOI] [PubMed] [Google Scholar]
- 37.Vizmanos B. Marti-Henneberg C. Puberty begins with a characteristic subcutaneous body fat mass in each sex. Eur J Clin Nutr. 2000;54:203–208. doi: 10.1038/sj.ejcn.1600920. [DOI] [PubMed] [Google Scholar]
- 38.Frisancho AR. University of Michigan Press; Ann Arbor, MI: 1990. Anthropometric Standards for the Assessment of Growth and Nutritional Status. [Google Scholar]
- 39.Gutin B. Owens S. The influence of physical activity on cardiometabolic biomarkers in youths: A review. Pediatr Exerc Sci. 2011;23:169–185. doi: 10.1123/pes.23.2.169. [DOI] [PubMed] [Google Scholar]
- 40.Vizcaino V. Aguilar F. Martinez M, et al. Association of adiposity measures with blood lipids and blood pressure in children aged 8–11 years. Acta Paediatr. 2007;96:1338–1342. doi: 10.1111/j.1651-2227.2007.00441.x. [DOI] [PubMed] [Google Scholar]
- 41.Gutin B. Diet vs exercise for the prevention of pediatric obesity: The role of exercise. Int J Obes Relat Metab Disord. 2011;35:29–32. doi: 10.1038/ijo.2010.140. [DOI] [PubMed] [Google Scholar]
- 42.Gutin B. Barbeau P. Owens S, et al. Effects of exercise intensity on cardiovascular fitness, total body composition, and visceral adiposity of obese adolescents. Am J Clin Nutr. 2002;75:818–826. doi: 10.1093/ajcn/75.5.818. [DOI] [PubMed] [Google Scholar]
- 43.Move More After-School Collaborative. North Carolina Division of Public Health; Raleigh, North Carolina: 2009. Move More North Carolina: Recommended Standards for After-School Physical Activity. [Google Scholar]
- 44.Gutin B. The role of nutrient partitioning and stem cell differentiation in pediatric obesity: A new theory. Int J Pediatr Obes. 2011;6(Suppl 1):7–12. doi: 10.3109/17477166.2011.590201. [DOI] [PubMed] [Google Scholar]
- 45.Earle A. Afterschool Alliance; Washington, DC: 2009. Roadmap to Afterschool for All. [Google Scholar]
- 46.Fashola OS. Building Effective Afterschool Programs. Corwin Press, Inc.; Thousand Oaks, CA: 2002. [Google Scholar]
- 47.Carrel AL. Clark RR. Peterson SE, et al. Improvement of fitness, body composition, and insulin sensitivity in overweight children in a school-based exercise program: A randomized, controlled study. Arch Pediatr Adolesc Med. 2005;159:963–968. doi: 10.1001/archpedi.159.10.963. [DOI] [PubMed] [Google Scholar]
- 48.Evenson KR. Scott MM. Cohen DA, et al. Girls' perception of neighborhood factors on physical activity, sedentary behavior, and BMI. Obesity. 2007;15:430–445. doi: 10.1038/oby.2007.502. [DOI] [PubMed] [Google Scholar]
- 49.Story M. Sherwood NE. Himes JH, et al. An after-school obesity prevention program for African-American girls: the Minnesota GEMS pilot study. Ethn Dis. 2003;13:S54–S64. [PubMed] [Google Scholar]
- 50.Taylor RW. McAuley KA. Barbezat W, et al. APPLE Project: 2-y findings of a community-based obesity prevention program in primary school age children. Am J Clin Nutr. 2007;86:735–742. doi: 10.1093/ajcn/86.3.735. [DOI] [PubMed] [Google Scholar]
- 51.Nemet D. Barkan S. Epstein Y, et al. Short- and long-term beneficial effects of a combined dietary-behavioral-physical activity intervention for the treatment of childhood obesity. Pediatrics. 2005;115:e443–e449. doi: 10.1542/peds.2004-2172. [DOI] [PubMed] [Google Scholar]
- 52.Mahoney JL, editor; Larson RW, editor; Eccles JS, editor. Organized Activities As Contexts of Development Extracurricular Activities, After School and Community Programs. Lawrence Erlbaum Associates; Mahwah, NJ: 2005. [Google Scholar]
- 53.Allison K. Adlaf E. Dwyer J, et al. The decline in physical activity among adolescent students: a cross-national comparison. Can J Public Health. 2007;98:97–100. doi: 10.1007/BF03404317. [DOI] [PMC free article] [PubMed] [Google Scholar]