Myocardial infarction (MI) is characterized by an extended subclinical phase leading to the sudden onset of life-threatening acute events (Figure). Acute MI is often preceded by specific triggers, which may include common activities such as alcohol consumption, heavy meals, physical exertion, and stressful events. Most research on MI triggers has emphasized the increased risks to the individual. The population burden of MI triggers has not received as much attention.
Figure.
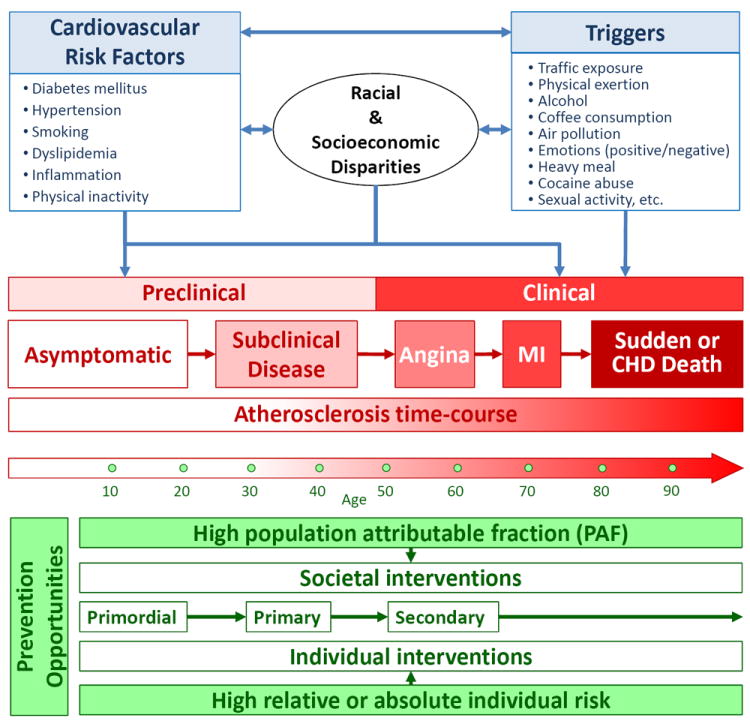
Conceptual model linking atherosclerosis time course, cardiovascular risk factors and triggers with acute cardiovascular events. The figure shows the roles of racial and socioeconomic disparities and the opportunities for prevention at the individual and societal level.
Abbreviations: MI, myocardial infarction; CHD, coronary heart disease
In the Lancet, a meta-regression analysis of 36 studies on 13 MI triggers now addresses this gap.1 Instead of just focusing on the risk to the individual, Nawrot and collaborators use the relative risks (i.e., Odds Ratios [ORs]) and frequencies of each trigger to compute population attributable fractions (PAFs). PAFs estimate the proportion of cases that could be avoided if a risk factor were removed.2 PAFs depend not just on the risk factor strength at the individual level, but also on its frequency in the community. A very strong, but uncommon risk factor will be very detrimental for the few individuals who are exposed to it, but nonetheless account for a relatively small number of cases in the community.
The authors skillfully show how the concepts of individual versus population risks apply to MI triggers. At the individual level, cocaine use was by far the strongest trigger (OR=23.7). However, because of the low reported frequency in the community,3 only 0.9% of MI cases were estimated to be triggered by cocaine.
Conversely, a novel insight provided by Nawrot and collaborators was the population burden of air pollution. Particulate matter <10 μm in aerodynamic diameter (PM10) is the air pollutant most consistently associated with MI onset.4 If the levels of PM10 in a hypothetical city were to be decreased by 30 μg/m3, 4.8% of MIs might be avoided or delayed. Despite the low relative risk (OR=1.05) associated with PM10, the population benefit would be considerable because the entire community of this hypothetical city would be advantaged by the air pollution reduction. The 30 μg/m3 PM10 decrease corresponds to a change that would bridge the gap in a number of European cities toward the 20 μg/m3 annual mean limit recommended by the World Health Organization.5 However, this decrease is larger than that needed or even achievable in most cities in the U.S. and several in Europe. For instance, in 20006 the large majority of US cities had PM10 annual concentrations <30 μg/m3 and many had levels <20 μg/m3. The PAF of 1.57% computed for a 10 μg/m3 PM10 decrease is still far from negligible and may be a more appropriate estimate of MI triggering burden in those communities exposed to low to moderate air pollution levels. Yet, the two mitigation scenarios examined by Nawrot et al. are too moderate for most Asian metropolitan areas, where PM10 levels are considerably higher than in the U.S. and Europe.7
The current MI trigger research has several limitations highlighted by Nawrot et al. Of the 13 triggers identified, only six were evaluated in multiple studies. The single-study results include the triggers with highest strength (cocaine, heavy meals), and most of those with the largest PAFs (traffic, alcohol, coffee). Hence, the studies will need to be replicated as these high risk/burden estimates may just represent the “winner’s curse”.8 In addition, several MI triggers have been loosely defined. Traffic exposure, for instance, might be considered a composite trigger resulting from air pollution, driving-related stress, and noise.
One major area of research that has been understudied is how triggers contribute to health care disparities by interacting with each other and with cardiovascular risk factors (Figure). For instance, the models assume a prevalence of 100% for air pollution, but it is established that air pollution is inordinately concentrated in lower socioeconomic neighborhoods.9 Similarly, triggers may be most relevant to individuals with higher levels of cardiovascular risk factors, which also are clustered disproportionately in racial minorities and individuals with lower socioeconomic status.10
Despite limitations, Nawrot and collaborators have provided us with an exemplary piece of epidemiological work that furthers our understanding of MI triggers. Their work stands as a warning against overlooking the public health relevance of ubiquitous risk factors with moderate or weak strength that have high frequency in the community.
References
- 1.Nawrot TS, Perez L, Kunzli N, Munters E, Nemery B. Public health importance of triggers of myocardial infarction. Lancet. doi: 10.1016/S0140-6736(10)62296-9. in press. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Metrics: Population Attributable Fraction (PAF) [21/12/2010];Quantifying the contribution of risk factors to the Burden of Disease. 2010 Available from: http://www.who.int/healthinfo/global_burden_disease/metrics_paf/en/index.html.
- 3.Mittleman MA, Mintzer D, Maclure M, Tofler GH, Sherwood JB, Muller JE. Triggering of myocardial infarction by cocaine. Circulation. 1999;99(21):2737–41. doi: 10.1161/01.cir.99.21.2737. [DOI] [PubMed] [Google Scholar]
- 4.Brook RD, Rajagopalan S, Pope CA, 3rd, Brook JR, Bhatnagar A, Diez-Roux AV, et al. Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation. 2010;121(21):2331–78. doi: 10.1161/CIR.0b013e3181dbece1. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. Global update 2005: Summary of risk assessment. Geneva: World Health Organization; 2006. WHO Air quality guidelines for particulate matter, ozone, nitrogen dioxide and sulfur dioxide. [Google Scholar]
- 6.Hart JE, Yanosky JD, Puett RC, Ryan L, Dockery DW, Smith TJ, et al. Spatial modeling of PM10 and NO2 in the continental United States, 1985-2000. Environ Health Perspect. 2009;117(11):1690–6. doi: 10.1289/ehp.0900840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.United Nations Environment Programme. GEO4 Environment for Development- State and trend of the Environment: 1987–2007: Air Pollution Nairobi, Kenia. 2007 [Google Scholar]
- 8.Kraft P. Curses--winner’s and otherwise--in genetic epidemiology. Epidemiology. 2008;19(5):649–51. doi: 10.1097/EDE.0b013e318181b865. discussion 57-8. [DOI] [PubMed] [Google Scholar]
- 9.O’Neill MS, Jerrett M, Kawachi I, Levy JI, Cohen AJ, Gouveia N, et al. Health, wealth, and air pollution: advancing theory and methods. Environ Health Perspect. 2003;111(16):1861–70. doi: 10.1289/ehp.6334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De Simone G, et al. Executive summary: heart disease and stroke statistics--2010 update: a report from the American Heart Association. Circulation. 2010;121(7):948–54. doi: 10.1161/CIRCULATIONAHA.109.192666. [DOI] [PubMed] [Google Scholar]


