Abstract
Objective:
This study describes developmental trajectories of depressive symptoms in adolescents and examines the association between trajectory group and mental health outcomes in young adulthood.
Methods:
Depressive symptoms were self-reported every three months from grade seven through grade 11 by 1293 adolescents in the Nicotine Dependence in Teens (NDIT) study and followed in young adulthood (average age 20.4, SD=0.7, n=865). Semi-parametric growth modeling was used to identify sex-specific trajectories of depressive symptoms.
Results:
Three distinct trajectory groups were identified: 50% of boys and 29% of girls exhibited low, decreasing levels of depressive symptoms; 14% of boys and 28% of girls exhibited high and increasing levels; and 36% of boys and 43% of girls exhibited moderate levels with linear increase. Trajectory group was a statistically significant independent predictor of depression, stress, and self-rated mental health in young adulthood in boys and girls. Boys, but not girls, in the high trajectory group had a statistically significant increase in the likelihood of seeking psychiatric care.
Conclusions:
Substantial heterogeneity in changes in depressive symptoms over time was found. Because early depressive symptoms predict mental health problems in young adulthood, monitoring adolescents for depressive symptoms may help identify those most at risk and in need of intervention.
Keywords: depressive symptoms, adolescents, latent growth modeling, mental health, development
Résumé
Objectif:
Cette étude décrit les trajectoires développementales des symptômes dépressifs chez les adolescents et examine l’association entre le groupe des trajectoires et les résultats de santé mentale au début de l’âge adulte.
Méthodes:
Les symptômes dépressifs ont été auto-déclarés tous les trois mois, de la 7e à la 11e année, par 1293 adolescents de l’étude prospective NICO, et ont fait l’objet d’un suivi au début de l’âge adulte (âge moyen 20,4, ET=0,7, n=865). Une modélisation semi-paramétrique de la croissance a été utilisée pour identifier les trajectoires sexospécifiques des symptômes dépressifs.
Résultats:
Trois groupes de trajectoires distincts ont été discernés: 50% des garçons et 29% des filles présentaient des niveaux faibles, décroissants de symptômes dépressifs; 14% des garçons et 28% des filles présentaient des niveaux élevés et croissants; et 36% des garçons et 43% des filles présentaient des niveaux modérés avec accroissement linéaire. Le groupe de trajectoires était un prédicteur indépendant statistiquement significatif de dépression, de stress, et de santé mentale autoévaluée chez les jeunes adultes, filles et garçons. Les garçons, mais pas les filles, du groupe de trajectoires élevées avaient une hausse statistiquement significative de la probabilité de recourir à des soins psychiatriques.
Conclusions:
Une hétérogénéité substantielle des changements des symptômes dépressifs avec le temps a été observée. Parce que les symptômes dépressifs précoces prédisent des problèmes de santé mentale au début de l’âge adulte, surveiller les symptômes dépressifs des adolescents peut contribuer à identifier ceux qui sont les plus à risque et qui ont besoin d’une intervention.
Keywords: symptômes dépressifs, adolescents, modélisation de croissance latente, santé mentale, développement
Introduction
By 2020, depression disorders are expected to be second only to heart disease in terms of the global burden of disease in higher income countries (Lopez & Disease Control Priorities Project, 2006). Population-based studies have reported prevalence rates of major depression (MDD) ranging between 0.4% and 2.5% in children and between 0.4% and 9% in adolescents (Domènech-Llaberia et al., 2009; Essau, Conradt, & Petermann, 2000; Johnston & Reynolds, 1994; Lewinsohn, Clarke, Seeley, & Rohde, 1994; Merikangas et al., 2010; Costello, Foley, & Angold, 2006; Williams, O’Connor, Eder, & Whitlock, 2009) and that more than 50% of depressed adolescents will continue to experience MDD into adulthood (Lewinsohn, Rohde, Klein, & Seeley, 1999). An even higher percentage (18%) of adolescents experience sub-threshold depression (i.e., temporary affective state or cluster of symptoms that fail to meet the diagnostic criteria; Saluja et al., 2004). The longitudinal pattern of depressive symptoms over time (i.e., trajectory) in adolescence could signal risks for the development of mental illness in young adulthood. In Canada, the prevalence of depression is thought to increase considerably during adolescence (Afifi, Enns, Cox, & Martens, 2005). Analyses of the Canadian Community Health Survey found that the past 12-month prevalence of depression among adolescents was 6.5% (Afifi et al., 2005). Other factors such as immigrant background and socio-economic status have also been shown to alter the development of depression through adolescence (Nguyen, Rawana, & Flora, 2011; Wickrama, Noh, & Elder, 2009).
Major depressive disorder (MDD) occurs at approximately the same rate in girls and boys during childhood, but the girl:boy ratio increases during adolescence to approximately 2:1, which mirrors the ratio reported in adults (Essau, et al., 2000; Fleming & Offord, 1990; Kessler et al., 1994; Lewinsohn, et al., 1994). Higher levels of depressive symptoms in girls emerge by age 14 (Hankin, 2009; Wade, Cairney, & Pevalin, 2002), with the greatest increase in sex difference occurring between the ages of 15 and 18 years (Essau, et al., 2000; Hankin et al., 1998).
While a number of studies (Garber, Keiley, & Martin, 2002; Ge, Natsuaki, & Conger, 2006) use a mean trajectory approach to identify a single pattern of depressive symptoms over time, there is increasing evidence that trajectories during adolescence may be heterogeneous (Nandi, Beard, & Galea, 2009; Rodriguez, Moss, & Audrain-McGovern, 2005; Côté, et al., 2009; Brendgen, Wanner, Morin, & Vitaro, 2005; Repetto, Zimmerman, & Caldwell, 2004; Stoolmiller, Kim, & Capaldi, 2005; Dekker et al., 2007). Increased understanding of the specific trajectories and heterogeneity for boys and girls may help identify subpopulations that should be targeted to reduce the prevalence of depression. Dekker et al. (2007) examined latent depression trajectories by sex but relied on the use of parent reports of child depressive symptoms (Côté et al., 2009; Dekker, et al., 2007), which may underreport internalizing problems in their children (Briggs-Gowan, Carter, & Schwab-Stone, 1996; Garber & Cole, 2010) compared to self-report in adolescence.
The first objective of this study was to identify sex-specific developmental trajectories of depressive symptoms during adolescence in a Canadian population-based sample of adolescents. Secondly, we sought to examine how these depressive symptom trajectories were associated with mental health outcomes in young adulthood, including mental health indicators (self-reported major depression, stress, self-rated mental health), and mental health diagnoses and treatment (seeking psychiatric care, mood disorder diagnosis, anxiety disorder diagnosis, and antidepressant use), after controlling for other predictors of future mental health (immigrant status, socio-economic status), and baseline depressive symptoms. We hypothesized that adolescents in a trajectory characterized by high levels of depressive symptoms would have poorer mental health in early adulthood.
Methods
Population and Design
The Nicotine Dependence in Teens (NDIT) Study is an ongoing cohort study that began in 1999 and is designed to investigate the natural course of early cigarette use and the development of nicotine dependence in novice smokers. The cohort includes 1293 students (52% girls) initially aged 12–13 years recruited from all grade seven classes in a convenience sample of ten secondary schools in Montreal, Canada. Schools were selected to include a mix of French and English, urban, suburban, and rural, and schools located in high and low socioeconomic neighbourhoods. More detailed descriptions of the sample can be found elsewhere (O’Loughlin, Karp, Koulis, Paradis, & Difranza, 2009).
All students from every grade seven class in the study schools were invited to participate. Signed informed parent/ guardian consent and student assent was obtained from all participants. Over half of eligible students (56.2%) participated in the baseline data collection in the fall of 1999. This relatively low response was due, in part, to a labour dispute that resulted in teachers from several schools refusing to collect consent forms.
Participants completed a 45-minute questionnaire administered to groups of classes either in the classroom or in the school cafeteria. Participants were surveyed every three months on average during the ten-month school year for five years, resulting in 20 survey-cycles. Most data collection took place during the months of October, January, March, and May. Alternative data collection dates were scheduled for participants who were not available on the originally scheduled date. Approximately 94% of participants eligible for follow-up in each survey-cycle completed questionnaires.
Additional data were collected from participants when they were aged 18–24 years in 2007/2008 in survey cycle 21, approximately two years after survey cycle 20, using mailed self-report questionnaires. Data on socio-demographic characteristics, depression, anxiety, stress, smoking, and use of psychoactive substances were collected for 865 NDIT participants. Data collection for this study was approved by the ethics research committees of the Direction de santé publique de Montréal-Centre and the Centre de Recherche du Centre Hospitalier de l’Université de Montréal.
Description of Study Variables
Depressive symptoms
Depressive symptoms during adolescence were measured in a validated 6-item depressive symptom scale (Escobedo, Kirch, & Anda, 1996; Kandel & Davies, 1986) that assessed how often in the past three months participants: (1) felt too tired to do things; (2) had trouble going to sleep or staying asleep; (3) felt unhappy, sad, or depressed; (4) felt hopeless about the future; (5) felt nervous or tense; and, (6) worried too much about things. Response choices ranged from never to often on a 4-point scale, where higher scores represent higher levels of depressive symptoms. The depressive symptom score was calculated as the mean value of the six items. Cronbach’s alpha reliability coefficient was 0.89 at baseline.
Major Depression
Depression symptom severity at young adulthood (survey cycle 21) was measured with the self-report Major Depression Inventory (MDI) (Bech et al., 1997). Participants were asked how much time in the past two weeks they had: (1) felt low in spirits or sad; (2) lost interest in, or could no longer enjoy their daily activities; (3) felt a lack of energy and strength; (4) felt less confident; (5) had a bad conscience or feelings of guilt; (6) felt life wasn’t worth living; (7) had difficulty concentrating; (8) felt very restless; (9) felt subdued or slowed down; (10) had trouble sleeping at night or waking up too early; (11) suffered from reduced appetite; and, (12) suffered from increased appetite. Response choices, on a 6-point scale, ranged from no time = 0 to all the time = 5. A score of four or more for questions 1 and 2, and a score of three or more for the other questions indicates having met the diagnostic demarcation for the presence of a depression symptom. The measure was used as a continuous score by summing the responses. Ten of the 12 items were retained as only the highest score from questions 8 or 9, and the highest score from questions 11 or 12 are included in the composite score. Range of possible scores is from 0 to 50 with higher scores indicating more severe symptoms. While the MDI could be used to report a classification of clinically significant depression, only 1% (n=14) people met this cut-off.
Other Mental Health Indicators
Additional indicators of mental health were assessed (stress, self-rated mental health, self-reported mood and/ or anxiety disorder diagnosed by a mental health professional, having sought psychiatric care, and taking antidepressant medication). Stress was measured by asking participants, “Thinking about the amount of stress in your life, would you say that most days are: (1) not at all stressful; (2) not very stressful; (3) a bit stressful; (4) quite stressful; and, (5) extremely stressful.” Individuals answering 4 or 5 were categorized as experiencing stress. Self-rated mental health was measured by asking participants, “In general, how would you rate your mental health? (1) excellent, (2) very good, (3) good, (4) average, (5) poor.” Individuals answering 5 were categorized as having poor reported mental health. Diagnosed major depression and anxiety disorder by a professional was assessed by asking participants “Has a health professional ever diagnosed you with a mood disorder?” and “Has a health professional ever diagnosed you with an anxiety disorder?” (yes/no). Seeking psychiatric care was assessed by asking participants “In the past year, have any of the following happened to you: sought psychological or psychiatric care?” (yes/no). To assess use of anti-depressants, participants were asked “In the past month, did you take any of the following medications, either prescription or over-the-counter: antidepressants (Prozac, Paxil, Effexor)?” (yes/no).
Potential confounders
Immigration status was measured through a question that asked respondents for country of birth. As a substantial number of countries were reported, responses were categorized into those born in Canada compared to those born elsewhere. Socio-economic status was assessed through self-reported highest level of mother’s education (high school or less versus more than high school).
Statistical Analysis
Demographic characteristics (age, percent born in Canada, mother’s education) and mean depressive symptoms scores were measured at baseline. Differences between mean depressive symptom scores at baseline were tested using a t-test. Semiparametric group-based latent class growth modeling was used to identify depressive symptom trajectory groups separately for boys and girls based on the first 20 survey cycles. The SAS procedure ‘Proc Traj’ was used to conduct the latent class analysis (Jones, Nagin, & Roeder, 2001). The censored normal distribution was applied since the depressive symptom scores were negatively skewed. All available values from each participant were used, resulting in a total of 19,337 observations. Age was centered at 12 years to provide intercepts that correspond to mean depressive symptom scores near study entry at age 12 years (average age = 12.8, SD=0.6)).
Modeling began with a one-group unconditional linear growth model against which models with additional groups were tested. Model selection was guided by pursuit of maximal parsimony, interpretability, and goodness-of-fit of the model. Statistical criteria for model selection included the Bayesian Information Criterion (BIC), the sample size adjusted BIC and the Likelihood Ratio Test (for K-1 vs K groups). Models with lower BIC were favored (Nagin, 1999; Raftery, 1995). Consistent with other literature (Nagin, 1999; Raftery, 1995), we set the minimum group prevalence at 10% due to the poor replicability of trajectories of small groups. Each group was tested with up to a quadratic growth term using a t-test (at 0.05 alpha level) and BIC (Brendgen, et al., 2005; Hipp & Bauer, 2006). Participants were assigned to the group for which they had the highest estimated posterior probability. Trajectory groups are robust to classification errors when mean estimated posterior probabilities exceed 0.7 (Roeder, Lynch, & Nagin, 1999).
Differences in the percentage of boys and girls between trajectories groups were assessed using tests of difference of proportions. The associations between trajectory group and dichotomous mental health indicators in young adulthood (n=865) were examined first bivariately using chi square tests. Then the independent association of the trajectory with young adult outcomes was assessed using logistic or linear regression (for the continuous MDI scale score) controlling for age at cycle 21, mother’s education, and having been born in Canada, and baseline depressive symptoms. Finally, males and females were combined into one dataset. A series of regressions were performed including the interactions of sex and trajectory group to assess if the effect of trajectory group differed by sex. Covariates from the previous regressions above were also included. The significance of the interaction terms was assessed by performing a test of the overall interaction on two degrees of freedom.
Results
Mean depressive symptoms scores were statistically significantly different between boys (Mean=2.0, SD=0.6)) and girls (Mean=2.2, SD=0.6) at study entry. Of the baseline sample, 52% were girls and average age at baseline was 12.8 (SD=0.6). Nine percent of the sample was born outside of Canada, and 54% had mothers with education beyond high school.
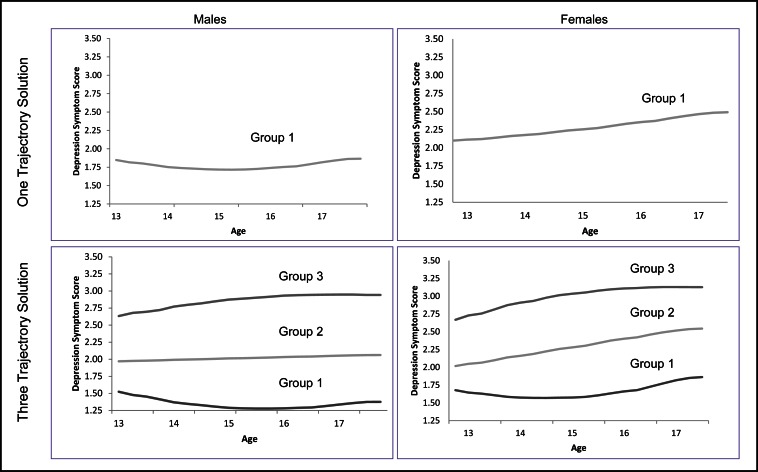
Three trajectory groups were identified in both boys and girls, estimated in separate models: high, moderate and low (See Table 1). The models for boys and girls were similar in shape but the percentage of the population within each trajectory differed. In the final models, the high trajectory groups for both boys and girls demonstrated increasing depressive symptom scores over adolescence that slowed over time (Table 2) with significant linear and quadratic parameters. The low trajectory groups declined over time, with the rate of decline increasing during later adolescence, as indicated by the linear and quadratic parameter. The moderate trajectory groups had a linear increase in depressive symptom scores over time, but there was no significant acceleration or deceleration over time. Figure 1 shows the final three trajectories, as well as the mean trajectory, for boys and girls, respectively. The four-trajectory solution was rejected since it included two moderate groups with one group smaller than the minimum 10% criteria specified.
Table 1.
Quantitative model selection criteria for depression symptom trajectory models
| Model (# of groups) | Delta df | Bayes Information Criterion | Sample size adjusted Bayes Information Criterion | Likelihood | Minimum group size |
|---|---|---|---|---|---|
| Boys | |||||
| 1 | - | −10882.67 | −10878.62 | −10868.86 | 100 |
| 2 | 2 | −9002.78 | −8994.62 | −8975.09 | 45 |
| 3 | 2 | −6371.91 | −6360.27 | −6331.32 | 15 |
| 3 | 2 | −6303.30 | −6285.20 | −6240.17 | 14 |
| Girls | |||||
| 1 | - | −9821.16 | −9817.13 | −9807.47 | 100 |
| 2 | 2 | −7756.39 | −7748.33 | −7729.01 | 32 |
| 3 | 2 | −7659.93 | −7648.25 | −7618.96 | 27 |
| 3 | 2 | −7606.04 | −7591.77 | −7555.98 | 28 |
Table 2.
Parameter estimates of final trajectory models in boys (n=622) and girls (n=671)
| Classes | Group membership (%) | Constant | p | Linear | p | Quadratic | p |
|---|---|---|---|---|---|---|---|
| Boys | |||||||
| Low | 50 | 1.67 | <0.01 | −0.24 | <0.01 | 0.04 | <0.01 |
| Moderate | 36 | 1.95 | <0.01 | 0.02 | <0.01 | -- | -- |
| High | 14 | 2.49 | <0.01 | 0.20 | <0.01 | −0.02 | <0.01 |
| Girls | |||||||
| Low | 29 | 1.78 | <0.01 | −0.19 | <0.01 | 0.04 | <0.01 |
| Moderate | 43 | 1.93 | <0.01 | 0.12 | <0.01 | -- | -- |
| High | 28 | 2.48 | <0.01 | 0.27 | <0.01 | −0.05 | <0.01 |
Figure 1.
One and Three depressive symptom trajectories among boys (n=622) and girls (n=671) during adolescence in the Nicotine Dependence in Teens Study, Montreal, Quebec. Group 1, 2, and 3 correspond to low, moderate and high trajectory groups, respectively.
While the three trajectories were similar in boys and girls, the distribution of the participants in the high, moderate, and low trajectories differed by sex (Table 2). Half of the boys, but only 29% of the girls, were classified in the low trajectory group (p<0.01). Only 14% of boys, but 28% of girls, were in the high trajectory group (p<0.01). Finally, 36% of boys compared to 43% of girls were in the moderate group (p=0.03).
A total of 865 participants reported complete data for the mental outcomes in young adulthood. Age at follow up was 20.5 years (SD=0.7) for boys and 20.3 (SD=0.7) for girls. Participants who were male, those born outside Canada, and those with lower maternal education were significantly more likely to be lost to follow-up; however, loss to follow-up was not significantly different between depression symptom trajectory groups (data not shown). MDI scores were higher among females (10.8, SD=8.5) than among males (7.4, SD=6.0) (p<0.001). Fifty-five percent of boys and 66% of girls in high trajectory group reported at least one symptom of major depression at cycle 21 compared to 20% of boys and 29% of girls in the low trajectory group. Table 3 presents the sample descriptions of the other mental health outcomes assessed at survey cycle 21. All mental health outcomes differed by significantly by sex in young adulthood.
Table 3.
Description of mental health outcomes at cycle 21 by sex and depressive symptom trajectory group in the Nicotine Dependence in Teens study, Montreal, Quebec (n=865)
| Girls (n=470)
|
Boys (n=395)
|
|||||||
|---|---|---|---|---|---|---|---|---|
| High n=134 | Moderate n=208 | Low n=127 | Total | High n=46 | Moderate n=205 | Low n=125 | Total | |
| Stress (days are)** | ||||||||
| No | 25% | 37% | 54% | 38%++ | 41% | 59% | 64% | 59%+ |
| Yes | 75% | 63% | 46% | 62% | 59% | 41% | 36% | 41% |
| Rate your mental health** | ||||||||
| Excellent | 73% | 90% | 90% | 85%++ | 83% | 91% | 96% | 92%+ |
| Poor | 27% | 10% | 10% | 15% | 17% | 9% | 4% | 8% |
| Diagnosed mood disorder** | ||||||||
| No | 86% | 95% | 95% | 92%++ | 91% | 95% | 99% | 96%+ |
| Yes | 14% | 5% | 5% | 8% | 9% | 5% | 2% | 4% |
| Diagnosed anxiety disorder** | ||||||||
| No | 83% | 95% | 92% | 91%++ | 94% | 97% | 97% | 97% |
| Yes | 17% | 5% | 8% | 9% | 7% | 3% | 3% | 3% |
| Sought psychiatric care* | ||||||||
| No | 85% | 89% | 91% | 88% | 74% | 95% | 94% | 92%++ |
| Yes | 15% | 11% | 9% | 12% | 26% | 5% | 6% | 8% |
| Take antidepressants* | ||||||||
| No | 93% | 98% | 99% | 97%++ | 96% | 99% | 100% | 99%+ |
| Yes | 7% | 2% | 1% | 3% | 4% | 1% | 0% | 1% |
Test for differences between sex
p<0.01,
p<0.05
Test for differences among trajectory groups
p<0.01,
p<0.05
In boys, trajectory group membership was significantly associated with all mental health outcomes in young adulthood, except for reported diagnosed Anxiety Disorder (p=0.40) (Table 3). After adjusting for baseline depressive symptom score, age at follow-up, mother’s education, and country of birth, those in the high and moderate trajectory groups were both more likely to report higher MDI scores than the low trajectory group (Table 4). Those in the high trajectory group also were more likely to report stress, poor mental health, and having sought psychiatric care. However, after controlling for other predictors, group membership was not associated with diagnoses of anxiety or mood disorders. The likelihood of past month use of antidepressants according to group membership could not be estimated among boys because all users of antidepressants were in the high trajectory group. Baseline depressive symptoms in grade seven were not independent predictors of young adult outcomes except for having sought psychiatric care where there were lower odds of seeking care for increased symptoms at baseline after controlling for trajectory group. This suggests that participants with high reports of symptoms that are inconsistent with the trajectory were less likely to report having sought care.
Table 4.
Associations between developmental trajectories of depressive symptoms to outcomes at young adulthood among girls and boys in separate logistic or linear regressions. Nicotine Dependence in Teens study, Montreal, Quebec
| Linear regression
|
Logistic regressions
|
||||||
|---|---|---|---|---|---|---|---|
| Major Depression Inventory scorea | Stress (days are) | Rate your mental health (ref: excellent) | Mood disorder diagnosed (ref: no) | Anxiety disorder diagnosed (ref: no) | Sought psychiatric care (ref: no) | Take antidepressants last month (ref: no)b | |
| Girls trajectory group, n=470
|
|||||||
| High vs. low | 7.35 (5.29 – 9.40)* |
4.09 (2.21 – 7.57)* |
3.17 (1.40 – 7.19)* |
2.23 (0.74 – 6.73) |
1.83 (0.73 – 4.59) |
2.08 (0.81 – 5.31) |
4.27 (0.46 – 39.87) |
| Moderate vs. low | 2.45 (0.75 – 4.15)* |
2.15 (1.33 – 3.48)* |
1.06 (0.48 – 2.34) |
0.98 (0.34 – 2.82) |
0.57 (0.23 – 1.43) |
1.49 (0.64 – 3.43) |
1.7 (0.18 – 16.02) |
| Age at follow up | 0.37 (−0.60 – 1.35) |
1.12 (0.84 – 1.50) |
1.14 (0.78 – 1.68) |
1 (0.61 – 1.62) |
1.04 (0.66 – 1.62) |
1.02 (0.68 – 1.55) |
1.03 (0.50 – 2.15) |
| Mother’s education | −0.66 (−2.18 – 0.87) |
0.75 (0.48 – 1.16) |
0.67 (0.36 – 1.24) |
0.78 (0.32 – 1.89) |
0.95 (0.44 – 2.03) |
0.85 (0.43 – 1.71) |
1.09 (0.29 – 4.07) |
| Born in Canada | 0.03 (−2.65 – 2.72) |
0.92 (0.42 – 2.01) |
1.21 (0.43 – 3.39) |
0.84 (0.19 – 3.79) |
0.63 (0.14 – 2.81) |
2.66 (1.06 – 6.64)** |
1.13 (0.13 – 9.70) |
| Baseline Depressive Symptom Score | −0.15 (−1.45 – 1.14) |
0.79 (0.54 – 1.15) |
1.41 (0.86 – 2.31) |
1.31 (0.69 – 2.52) |
1.27 (0.70 – 2.31) |
1.18 (0.68 – 2.05) |
2.48 (0.95 – 6.49) |
| Boys trajectory group, n=395
|
|||||||
| High vs. low | 7.47 (5.44 – 9.49)* |
2.6 (1.16 – 5.82)** |
4.87 (1.32 – 17.98)** |
4.44 (0.67 – 29.59) |
1.54 (0.22 – 10.84) |
14.21 (3.92 – 51.46)* |
— — |
| Moderate vs. low | 2.67 (1.46 – 3.87)* |
1.19 (0.74 – 1.93) |
2.31 (0.89 – 5.98) |
2.7 (0.64 – 11.31) |
0.77 (0.19 – 3.22) |
1.03 (0.37 – 2.92) |
— — |
| Age at follow up | −0.07 (−0.84 – 0.70) |
1.42 (1.04 – 1.94)** |
1.08 (0.63 – 1.85) |
1.57 (0.78 – 3.14) |
1.73 (0.85 – 3.53) |
1.22 (0.71 – 2.08) |
— — |
| Mother’s education | −0.74 (−1.99 – 0.51) |
1.04 (0.64 – 1.71) |
1.12 (0.45 – 2.81) |
1.14 (0.31 – 4.15) |
1.18 (0.27 – 5.19) |
1.09 (0.39 – 3.05) |
— — |
| Born in Canada | 1.83 (−0.11 – 3.77) |
0.98 (0.45 – 2.12) |
0.84 (0.19 – 3.78) |
0.85 (0.11 – 6.86) |
2.16 (0.44 – 10.54) |
2.33 (0.71 – 7.62) |
— — |
| Baseline Depressive Symptom Score | 0.18 (−0.89 – 1.25) |
0.87 (0.57 – 1.33) |
1.03 (0.49 – 2.18) |
1.33 (0.48 – 3.70) |
1.62 (0.55 – 4.73) |
0.36 (0.16 – 0.83)** |
— — |
| Interaction of sex by group c
|
|||||||
| chi square (2 df) | 0.04 | 2.73 | 1.55 | 1.7 | 0.76 | 6.4 | 180.18 |
| p-value | 0.959 | 0.255 | 0.461 | 0.428 | 0.683 | 0.04 | <0.001 |
Linear Regression. Confidence Intervals that do not cross 0 suggest statistical significance. All other regressions are logistic in which odds ratios are presented where confidence intervals that do not cross 1 suggest statistical significance.
Outcome among males predicted exactly leading to model failure
Separate analysis including combining both genders in one dataset and including an interaction between sex and group. Test of significance of the two interaction terms is reported. 95% confidence intervals in parentheses.
significant at 5%;
significant at 1%
For girls, group membership prior to adjustment was statistically significantly associated with all mental health outcomes in young adulthood, with the exception of seeking psychiatric care (p=0.274) (Table 3). After adjusting for baseline depression and other potential confounders, those in either high or moderate trajectory groups were found to be significantly more likely to have higher MDI scores and report that most days were stressful (Table 4). Those in the high trajectory group had over three times the odds of reporting poor self-rated health, after controlling for other predictors of outcomes at young adulthood. Baseline depressive symptoms in grade seven were not independent predictors of young adult outcomes, suggesting that the trajectories provided information beyond the magnitude of reported symptoms at baseline.
Combined models were run for each outcome with both boys and girls, including an interaction term to assess whether the effect of the trajectory group differed by sex (Table 4). Trajectory groups predicted differently for boys and girls for having sought psychiatric care and taking antidepressants.
Discussion
This paper identified three distinct trajectory groups of depressive symptoms during adolescence for both boys and girls. Further, depressive symptoms trajectory groups were associated with some mental health outcomes in young adulthood, even after controlling for baseline depressive symptoms, immigrant status, and socio-economic status. Despite large differences in prevalence of mental health outcomes during young adulthood between males and females, the trajectories of depressive symptoms, while defined independently, were similar in shape and magnitude, and predicted outcomes similarly for most outcomes. The exceptions were help-seeking behaviour, and reported taking of antidepressants.
The identification of three trajectory patterns suggests that a single average trajectory, as reported in previous research, may be a simplistic representation of the course of depressive symptoms during adolescence (Garber & Cole 2010; Garber, et al., 2002; Kim & Cicchetti, 2006). Both Garber et al. (2002) and Ge et al. (2006) found U-shaped developmental patterns of depressive symptoms, with an increase in depressive symptoms beginning at age 14 years. In contrast, our analysis suggests that a U-shaped pattern may be an artifact of masked heterogeneity. Many adolescents in this study (50% of boys and 29% of girls) experienced declining depressive symptoms from age 12 to 17. This decline would not have been detectable in a single trajectory approach as evidenced in Figure 1. Several reports (Brendgen, et al., 2005; Dekker, et al., 2007; Stoolmiller, et al., 2005) suggest the presence of four or more trajectory groups, yet consistent with the current findings Rodriguez and colleagues (Rodriguez et al., 2005) and Côté and colleagues (Côté, et al., 2009) also identified three trajectories.
As expected, mean depressive symptoms for boys and girls differed; however, the trajectories for boys and girls were similar throughout adolescence. Specifically, the same number of trajectory groups was identified for each sex, and the intercepts, slopes, and acceleration rates for each of the groups were of comparable direction and magnitude. Moderate groups demonstrated linear increases while high and low groups had decreasing and increasing rates of changes, respectively. Nonetheless, there were relatively more girls than boys in the high and moderate depressive symptom trajectory groups. The differences in mean depressive symptoms between boys and girls do not appear to be due to different trajectories during adolescence. The mean sex difference appears to be driven by more girls in the higher depressive symptom trajectory group, rather than differences in the shape of the trajectory. Other research (Brunet et al., In Review) has reported that depressive symptom measures are invariant by sex.
Depressive symptoms between boys and girls have consistently been shown to be similar in childhood (Hankin, Gibb, Abela, & Flory, 2010; Nolen-Hoeksema & Girgus, 1994; Piccinelli & Wilkinson, 2000), yet the differences in distribution between trajectory groups suggest a developmental divergence in depression symptoms prior to the beginning of the study at age 12 (grade seven). These findings contrast those of Hankin and colleagues (1998) who found substantial differences in depression symptoms in boys and girls between age 15 and 18 years. Dekker et al. (2007) also described trajectories for girls with dramatic increases prior to age 11 and trajectories for boys that declined by age 13. This study, congruent with Dekker et al. (2007), suggests that the shift in prevalence in girls and boys with respect to depressive symptoms likely occurs before adolescence.
Previous research has reported declining trajectories among boys (Dekker, et al., 2007; Stoolmiller, et al., 2005) but not girls. A number of potential mechanisms suggested by Dekker and colleagues (2007) for a decline in depressive symptoms such as distance in time from negative life events, increasing experience in dealing with problems on their own and increased independence from parents over adolescence are common to both boys and girls. Furthermore, with increased age and independence, many adolescents may develop resilience and positive coping skills that may be protective of developing depressive symptoms. Irrespective of start levels of depressive symptomatology, both boys and girls should benefit from learning positive coping behaviours.
Understanding depressive trajectories is important for a number of reasons. Of more clinical concern, the trajectory groups identified in the current study were associated with numerous mental health outcomes in young adulthood. There were marked differences between the low, moderate, and high trajectory groups in severity and number of major depression symptoms. While the association itself is unsurprising, the independent effect (on depressive symptoms in adulthood, stress, and self-rated mental health, as well as help-seeking in boys) after controlling for baseline magnitude of symptoms and other predictors of mental health suggests the trajectory groups are robustly indicative of future events. Furthermore, the lack of independent effect of baseline depressive symptoms suggests that changes through adolescence are more important than a measure of magnitude alone. The exception – the independent, and inverse, association baseline depressive symptoms and help-seeking for boys – shows that a single elevated report of depressive symptoms over and above the effect of trajectory was less likely to lead to boys seeking care, suggesting that it is more likely that the single elevated value is spurious. Apart from mental health outcomes, trajectory groups may also be associated with other poor physical and social outcomes (Dekker, et al., 2007), and early identification of those at risk could lead to effective intervention. Specifically, special attention should be paid to adolescents with consistently high symptoms and increasing symptoms of depression. Future research on factors that have the potential to influence depressed mood and alter the trajectories we observed are warranted and would contribute to the development of intervention and prevention programs that are tailored to different subgroups of adolescents. While identifying and treating depressed adolescents may have the potential to reduce or eliminate the burden of the disorder, at a population level, trajectories of depressive symptoms, or how depressive symptoms change during adolescence, are more important than the initial magnitude of reported symptoms. It is possible that clinicians do not expect declines or decreasing rates of change among girls through adolescence that has previously been found among boys.
For girls, trajectory groups were associated with all the mental health outcomes prior to adjustment except seeking psychiatric care. This null finding may reflect girls being more likely to seek treatment for depressive symptoms at lower levels of symptoms or, conversely, regarding elevated depressive symptoms as normal (Addis & Mahalik, 2003; Boldero & Fallon, 1995; Kessler et al., 1996). While the prevalence of mental health outcomes among males is lower, the pattern of treatment seeking and use of medication is more consistent with that expected from their trajectory group membership.
Limitations
In addition to sample size and number of outcomes, other limitations of this study include that the depressive symptom score is self-reported and not a measure of major depression. Nonetheless, the depression symptom score is a commonly used and well validated measure suitable for community and population based studies (Kandel & Davies, 1982). The results may not be generalizable to clinical populations since more severe cases (as may be seen in clinical populations) may exhibit different trajectories than those observed in the general population; however, the results should apply more broadly than those found in clinical samples. Further, while attrition may have led to bias, as 67% of the original sample was retained at cycle 21, there was no differential loss to follow-up by trajectory group. Finally, trajectories during adolescence may reflect ‘practice effects’ as participants repeat the same scale many times, which could be problematic if some adolescents were more susceptible to practice effects. Compared to previous research in general population settings, there are a high number of repeated surveys with a short duration between surveys.
Conclusions
Compared to examining mean scores, the trajectory approach indicates that there are distinct trajectory groups, and that not all adolescents experience increases in depressive symptoms over time. In fact, a large percentage of both boys and girls in the moderate and low groups experienced decreases in depressive symptoms during adolescence. While many more girls than boys experienced elevated depressive symptoms during adolescence, monitoring all adolescents for continued elevated depressive symptoms may help identify those most at risk for poor mental health outcomes in young adulthood. The changes observed of depressive symptoms during adolescence and the predictive effect of trajectories are consistent between boys and girls. Early identification and the development of interventions for those at higher risk could mitigate the impact of poor mental health on a clinical and societal level and should be implemented appropriately by sex. This study demonstrates that subclinical levels and changes in depressive symptoms can have important mental health implications.
Acknowledgements / Conflicts of Interest
The Nicotine Dependence in Teens Study is funded by the Canadian Cancer Society, which had no role in the study design; the collection, analysis, and interpretation of data; the writing of the report; or the decision to submit the manuscript for publication.
References
- Addis ME, Mahalik JR. Men, masculinity, and the contexts of help seeking. American Psychologist. 2003;58(1):5–14. doi: 10.1037/0003-066x.58.1.5. [DOI] [PubMed] [Google Scholar]
- Afifi TO, Enns MW, Cox BJ, Martens PJ. Investigating health correlates of adolescent depression in Canada. Canadian Journal of Public Health. 2005;96(6):427–431. doi: 10.1007/BF03405182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bech P, Stage KB, Nair NP, Larsen JK, Kragh-Sorensen P, Gjerris A. The Major Depression Rating Scale (MDS). Inter-rater reliability and validity across different settings in randomized moclobemide trials Danish University Antidepressant Group. Journal of Affective Disorders. 1997;42(1):39–48. doi: 10.1016/s0165-0327(96)00094-8. [DOI] [PubMed] [Google Scholar]
- Boldero J, Fallon B. Adolescent Help-Seeking: What do they get help for and from whom? Journal of Adolescence. 1995;18(2):193–209. [Google Scholar]
- Brendgen M, Wanner B, Morin AJ, Vitaro F. Relations with parents and with peers, temperament, and trajectories of depressed mood during early adolescence. Journal of Abnormal Child Psychology. 2005;33(5):579–594. doi: 10.1007/s10802-005-6739-2. [DOI] [PubMed] [Google Scholar]
- Briggs-Gowan MJ, Carter AS, Schwab-Stone M. Discrepancies among mother, child, and teacher reports: Examining the contributions of maternal depression and anxiety. Journal of Abnormal Child Psychology. 1996;24(6):749–765. doi: 10.1007/BF01664738. [DOI] [PubMed] [Google Scholar]
- Brunet J, Sabiston C, Low N, Chaiton M, Barnett T, Contreras G, et al. Measurement invariance of the depressive symptoms scale during adolescence. (In Review) [DOI] [PMC free article] [PubMed]
- Costello EJ, Foley DL, Angold A. Ten-year research update review: The epidemiology of child and adolescent psychiatric disorders: II. Developmental epidemiology. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:8–25. doi: 10.1097/01.chi.0000184929.41423.c0. [DOI] [PubMed] [Google Scholar]
- Côté SM, Boivin M, Liu X, Nagin DS, Zoccolillo M, Tremblay RE. Depression and anxiety symptoms: Onset, developmental course and risk factors during early childhood. Journal of Child Psychology and Psychiatry. 2009;50(10):1201–1208. doi: 10.1111/j.1469-7610.2009.02099.x. [DOI] [PubMed] [Google Scholar]
- Dekker MC, Ferdinand RF, van Lang ND, Bongers IL, van der Ende J, Verhulst FC. Developmental trajectories of depressive symptoms from early childhood to late adolescence: Gender differences and adult outcome. Journal of Child Psychology and Psychiatry. 2007;48(7):657–666. doi: 10.1111/j.1469-7610.2007.01742.x. [DOI] [PubMed] [Google Scholar]
- Domènech-Llaberia E, Viñas F, Pla E, Jané MC, Mitjavila M, Corbella T, et al. Prevalence of major depression in preschool children. European Child and Adolescent Psychiatry. 2009;18(10):597–604. doi: 10.1007/s00787-009-0019-6. [DOI] [PubMed] [Google Scholar]
- Escobedo LG, Kirch DG, Anda RF. Depression and smoking initiation among US Latinos. Addiction. 1996;91(1):113–119. [PubMed] [Google Scholar]
- Essau CA, Conradt J, Petermann F. Frequency, comorbidity, and psychosocial impairment of depressive disorders in adolescents. Journal of Adolescent Research. 2000;15(4):470–481. [Google Scholar]
- Fleming JE, Offord DR. Epidemiology of childhood depressive disorders: A critical review. Journal of the American Academy of Child and Adolescent Psychiatry. 1990;29(4):571–580. doi: 10.1097/00004583-199007000-00010. [DOI] [PubMed] [Google Scholar]
- Garber J, Cole DA. Intergenerational transmission of depression: A launch and grow model of change across adolescence. Development and Psychopathology. 2010;22(4):819–830. doi: 10.1017/S0954579410000489. [DOI] [PubMed] [Google Scholar]
- Garber J, Keiley MK, Martin C. Developmental trajectories of adolescents’ depressive symptoms: Predictors of change. Journal of Consulting and Clinical Psychology. 2002;70(1):79–95. doi: 10.1037//0022-006x.70.1.79. [DOI] [PubMed] [Google Scholar]
- Ge X, Natsuaki MN, Conger RD. Trajectories of depressive symptoms and stressful life events among male and female adolescents in divorced and nondivorced families. Devevelopment and Psychopathology. 2006;18(1):253–273. doi: 10.1017/S0954579406060147. [DOI] [PubMed] [Google Scholar]
- Hankin BL. Development of sex differences in depressive and co-occurring anxious symptoms during adolescence: Descriptive trajectories and potential explanations in a multiwave prospective study. Journal of Clinical Child and Adolescent Psychology. 2009;38(4):460–472. doi: 10.1080/15374410902976288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL, Abramson LY, Moffitt TE, Silva PA, McGee R, Angell KE. Development of depression from preadolescence to young adulthood: Emerging gender differences in a 10-year longitudinal study. Journal of Abnormal Psychology. 1998;107(1):128–140. doi: 10.1037//0021-843x.107.1.128. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Gibb BE, Abela JR, Flory K. Selective attention to affective stimuli and clinical depression among youths: Role of anxiety and specificity of emotion. Journal of Abnormal Psychology. 2010;119(3):491–501. doi: 10.1037/a0019609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hipp JR, Bauer DJ. Local solutions in the estimation of growth mixture models. Psychological Methods. 2006;11(1):36–53. doi: 10.1037/1082-989X.11.1.36. [DOI] [PubMed] [Google Scholar]
- Johnston HF, Reynolds WM. Handbook of depression in children and adolescents. New York, NY: Plenum Press; 1994. [Google Scholar]
- Jones BL, Nagin DS, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociological Methods and Research. 2001;29(3):374–393. [Google Scholar]
- Kandel DB, Davies M. Epidemiology of depressive mood in adolescents: An empirical study. Archives of General Psychiatry. 1982;39(10):1205–1212. doi: 10.1001/archpsyc.1982.04290100065011. [DOI] [PubMed] [Google Scholar]
- Kandel DB, Davies M. Adult sequelae of adolescent depressive symptoms. Archives of General Psychiatry. 1986;43(3):255–262. doi: 10.1001/archpsyc.1986.01800030073007. [DOI] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Nelson CB, Hughes M, Swartz M, Blazer DG. Sex and depression in the National Comorbidity Survey. II: Cohort effects. Journal of Affective Disorders. 1994;30(1):15–26. doi: 10.1016/0165-0327(94)90147-3. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Nelson CB, McGonagle KA, Edlund MJ, Frank RG, Leaf PJ. The epidemiology of co-occurring addictive and mental disorders: Implications for prevention and service utilization. American Journal of Orthopsychiatry. 1996;66(1):17–31. doi: 10.1037/h0080151. [DOI] [PubMed] [Google Scholar]
- Kim J, Cicchetti D. Longitudinal trajectories of self-system processes and depressive symptoms among maltreated and nonmaltreated children. Child Development. 2006;77(3):624–639. doi: 10.1111/j.1467-8624.2006.00894.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewinsohn PM, Clarke GN, Seeley JR, Rohde P. Major depression in community adolescents: Age at onset, episode duration, and time to recurrence. Journal of the American Academy of Child and Adolescent Psychiatry. 1994;33(6):809–818. doi: 10.1097/00004583-199407000-00006. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Klein DN, Seeley JR. Natural course of adolescent major depressive disorder: I. Continuity into young adulthood. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38(1):56–63. doi: 10.1097/00004583-199901000-00020. [DOI] [PubMed] [Google Scholar]
- Lopez AD, Disease Control Priorities Project . Global burden of disease and risk factors. New York, NY: Oxford University Press; 2006. [Google Scholar]
- Merikangas KR, He J-P, Brody D, Fisher PW, Bourdon K, Koretz DS. Prevalence and treatment of mental disorders among US children in the 2001–2004 NHANES. Pediatrics. 2010;125(1):75–81. doi: 10.1542/peds.2008-2598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagin DS. Analyzing developmental trajectories: A semiparametric, group-based approach. Psychological Methods. 1999;4(2):139–157. doi: 10.1037/1082-989x.6.1.18. [DOI] [PubMed] [Google Scholar]
- Nandi A, Beard JR, Galea S. Epidemiologic heterogeneity of common mood and anxiety disorders over the lifecourse in the general population: A systematic review. BMC Psychiatry. 2009;9:31. doi: 10.1186/1471-244X-9-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen H, Rawana JS, Flora DB. Risk and protective predictors of depression trajectories among adolescents from immigrant backgrounds. Journal of Youth and Adolescence. 2011;40(11):1544–1558. doi: 10.1007/s10964-011-9636-8. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Girgus JS. The emergence of gender differences in depression during adolescence. Psychoogical Bulletin. 1994;115(3):424–443. doi: 10.1037/0033-2909.115.3.424. [DOI] [PubMed] [Google Scholar]
- O’Loughlin J, Karp I, Koulis T, Paradis G, Difranza J. Determinants of first puff and daily cigarette smoking in adolescents. American Journal of Epidemiology. 2009;170(5):585–597. doi: 10.1093/aje/kwp179. [DOI] [PubMed] [Google Scholar]
- Piccinelli M, Wilkinson G. Gender differences in depression. Critical review. British Journal of Psychiatry. 2000;177:486–492. doi: 10.1192/bjp.177.6.486. [DOI] [PubMed] [Google Scholar]
- Raftery A. Bayesian model selection in social research. Sociological Methodology. 1995;25:111–163. [Google Scholar]
- Repetto PB, Zimmerman MA, Caldwell CH. A longitudinal study of the relationship between depressive symptoms and alcohol use in a sample of inner-city black youth. Journal of Studies on Alcohol. 2004;65(2):169–178. doi: 10.15288/jsa.2004.65.169. [DOI] [PubMed] [Google Scholar]
- Rodriguez D, Moss HB, Audrain-McGovern J. Developmental heterogeneity in adolescent depressive symptoms: Associations with smoking behavior. Psychosomatic Medicine. 2005;67(2):200–210. doi: 10.1097/01.psy.0000156929.83810.01. [DOI] [PubMed] [Google Scholar]
- Roeder K, Lynch K, Nagin DS. Modeling uncertainty in latent class membership: A case study in criminology. Journal of the American Statistical Association. 1999;94:766–776. [Google Scholar]
- Saluja G, Iachan R, Scheidt PC, Overpeck MD, Sun W, Giedd JN. Prevalence of and risk factors for depressive symptoms among young adolescents. Archives of Pediatrics & Adolescent Medicine. 2004;158:760–765. doi: 10.1001/archpedi.158.8.760. [DOI] [PubMed] [Google Scholar]
- Stoolmiller M, Kim HK, Capaldi DM. The course of depressive symptoms in men from early adolescence to young adulthood: Identifying latent trajectories and early predictors. Journal of Abnormal Psychology. 2005;114(3):331–345. doi: 10.1037/0021-843X.114.3.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wade TJ, Cairney J, Pevalin DJ. Emergence of gender differences in depression during adolescence: National panel results from three countries. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41(2):190–198. doi: 10.1097/00004583-200202000-00013. [DOI] [PubMed] [Google Scholar]
- Wickrama KAS, Noh S, Elder G. An investigation of family SES-based inequalities in depressive symptoms from early adolescence to emerging adulthood. Advances in Life Course Research. 2009;14(4):147–161. doi: 10.1016/j.alcr.2010.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams SB, O’Connor EA, Eder M, Whitlock EP. Screening for child and adolescent depression in primary care settings: A systematic evidence review for the US Preventive Services Task Force. Pediatrics. 2009;123(4):e716–735. doi: 10.1542/peds.2008-2415. [DOI] [PubMed] [Google Scholar]