Abstract
Arthritogenic alphaviruses are human pathogens maintained in nature through alternating replication in vertebrates and mosquitoes. Using chimeric viruses, we previously reported that replacement of the PE2 coding region of the T48 strain of Ross River virus (RRV-T48) with that from the attenuated DC5692 strain, which differ by 7 amino acids, resulted in an attenuated disease phenotype in a mouse model of RRV-induced rheumatic disease. Here, we demonstrate that introduction of one of these amino acid differences, a tyrosine (Y)-to-histidine (H) change at position 18 of the E2 glycoprotein (E2 Y18H), into the RRV-T48 genetic background was sufficient to generate a virus that caused dramatically less severe musculoskeletal disease in mice. The attenuated phenotype of RRV-T48 E2 Y18H was associated with reduced viral loads in musculoskeletal tissues, reduced viremia, and less efficient virus spread. Consistent with these findings, RRV-T48 E2 Y18H replicated less well in mammalian cells in vitro due to significantly reduced PFU released per infected cell. In contrast, RRV-T48 E2 Y18H replicated more efficiently than RRV-T48 in C6/36 mosquito cells. Competition studies confirmed that RRV-T48 E2 Y18H had a fitness advantage in mosquito cells and a fitness disadvantage in mammalian cells. Interestingly, all sequenced Ross River viruses encode either a tyrosine or a histidine at E2 position 18, and this holds true for other alphaviruses in the Semliki Forest antigenic complex. Taken together, these findings suggest that a tyrosine-to-histidine switch at E2 position 18 functions as a regulator of RRV fitness in vertebrate and invertebrate cells.
INTRODUCTION
Arthritogenic alphaviruses (genus Alphavirus, family Togaviridae), including Ross River virus (RRV), chikungunya virus (CHIKV), o'nyong-nyong virus, and Mayaro virus, are a group of mosquito-transmitted viruses with positive-sense, single-stranded RNA genomes that cause musculoskeletal inflammatory diseases in humans (1). In addition to causing endemic disease in Australia, Africa, Asia, and South America, these viruses are capable of causing explosive epidemics. Previous outbreaks include a 1959-1962 epidemic of o'nyong-nyong fever in Africa involving at least 2 million cases (2) and a 1979-1980 epidemic of RRV disease in Australia and islands in the South Pacific, which involved more than 60,000 cases (3). Since 2004, CHIKV has caused a series of epidemics in the Indian Ocean region, resulting in millions of cases of severe, debilitating, and often persistent arthralgia (4). Furthermore, autochthonous transmission resulting in the first CHIKV disease outbreaks in Europe and the Pacific region occurred in Italy in 2009 (5), in France in 2010 (6), and in New Caledonia in 2011 (7). These examples illustrate the ability of these viruses to reemerge and to spread to new geographical regions.
Clinical manifestations which follow infection with an arthritogenic alphavirus develop after an incubation period of between 2 and 12 days. Human disease is most commonly characterized by fever, maculopapular rash, intense pain in the peripheral joints, myalgia, and difficulty ambulating (3, 8). A multitude of studies have indicated that musculoskeletal pain persists for months to years in a subset of patients infected with RRV or CHIKV; however, the underlying cause of these persistent symptoms remains unclear (1, 9). No specific therapies or licensed vaccines are currently available. Treatment is limited to supportive care with analgesics and anti-inflammatory drugs (1, 9).
To study the pathogenesis of arthritogenic alphaviruses, we utilize a previously described mouse model of RRV-induced disease based on subcutaneous inoculation of the T48 strain of RRV (RRV-T48) into the footpad of 3- to 4-week-old C57BL/6 mice (10–12). Studies using this model have shown that following a high-titer serum viremia, bone/joint-associated tissues and skeletal muscle tissue are the primary sites of RRV replication (11). Viral replication in these tissues leads to severe inflammation with significant tissue damage and associated deficits in grip strength and altered gait. Human disease associated with infection by an arthritogenic alphavirus shows a similar progression, with (i) high-titer serum viremia (13, 14), (ii) detection of virus RNA and/or antigen in musculoskeletal tissues (15, 16), (iii) the presence of mononuclear inflammatory infiltrates in musculoskeletal tissues (13, 15, 17, 18), and (iv) difficulty ambulating and performing routine tasks. These similarities suggest that an understanding of host and viral factors which contribute to disease in this mouse model will increase our understanding of the pathogenesis of these viruses and may aid in the development of therapies and vaccines to treat or prevent human disease.
Previously, we reported that replacement of the PE2 coding region of RRV-T48 with that from the attenuated DC5692 strain resulted in an attenuated disease phenotype in mice (19). Here, we find that a single tyrosine (Y)-to-histidine (H) change at position 18 of the RRV-T48 E2 glycoprotein (E2 Y18H) was sufficient to generate a virus that caused dramatically less severe musculoskeletal disease in the mouse model. The attenuated phenotype of RRV-T48 E2 Y18H was associated with reduced viral loads in tissues and less efficient virus spread. Consistent with these data, RRV-T48 E2 Y18H replicated less well in murine and human cells in vitro. In contrast, the RRV-T48 E2 Y18H mutant virus replicated more efficiently than RRV-T48 in C6/36 mosquito cells. Competition studies confirmed that RRV-T48 E2 Y18H had a fitness advantage in mosquito cells and a fitness disadvantage in mammalian cells. In mammalian cells, RRV-T48 E2 Y18H produced significantly fewer PFU per infected cell, suggesting that this mutation confers a late-stage replication defect. Interestingly, all sequenced Ross River viruses encode either a Y or H at E2 position 18, and this holds true for other alphaviruses in the Semliki Forest (SF) antigenic complex. These findings suggest that a tyrosine-to-histidine switch at E2 position 18 functions as a critical regulator of RRV fitness in invertebrate and vertebrate cells.
MATERIALS AND METHODS
Viruses.
The T48 strain of RRV was isolated from Aedes vigilax mosquitoes in Queensland, Australia. Prior to cDNA cloning, the virus was passaged 10 times in suckling mouse brain, followed by two passages on Vero cells (20, 21). RRV strain DC5692 was isolated in 1995 from Aedes camptorhynchus mosquitoes in the Peel region of Western Australia (22). The virus was passaged 1 time in C6/36 cells, 1 time in Vero cells, and 1 time in BHK-21 cells prior to cDNA cloning (19). Virus stocks were generated from full-length wild-type and mutant virus cDNAs as previously described (19). Briefly, plasmids encoding virus cDNAs were linearized by digestion with SacI (NEB). 5′-capped full-length RNA transcripts were generated in vitro by using SP6-specific mMessage mMachine transcription kits (Ambion). Full-length transcripts were electroporated into BHK-21 cells (ATCC CCL-10) by using a Gene Pulser electroporator (Bio-Rad). Culture supernatants were harvested at 24 h after electroporation, centrifuged for 20 min at 3,000 rpm, aliquoted, and stored at −80°C. Stocks were titrated by plaque assays on BHK-21 cells. For purified virus stocks, virus particles were banded on a 60% to 20% discontinuous sucrose gradient by centrifugation at 24,000 rpm in a Beckman SW-24 rotor. Banded virus was collected and centrifuged through 20% sucrose at 24,000 rpm in a Beckman SW-24 rotor. Virus pellets were then resuspended, aliquoted, and stored at −80°C.
Site-directed mutagenesis.
Single-amino-acid substitutions (E3 R59G, E2 Y18H, E2 I67M, E2 H94R, E2 R251K, E2 H256Q, and E2 E302V) were generated by site-directed mutagenesis of plasmid pRR64, which encodes the RRV-T48 genome, by using the QuikChange II XL site-directed mutagenesis kit (Agilent). The mutagenized XbaI-RsrII fragment was subcloned back into pRR64. Clones for each mutant were verified by sequencing. To verify that the mutations were present in virus stocks, virion RNA was isolated, reverse transcribed, and cloned into pCR2-TOPO, and a portion of the E2 coding region was sequenced. For competition studies, a synonymous mutation was introduced into the RRV-T48 genome in plasmid pRR64, which eliminated the endogenous RsrII restriction site at position 9573. The XbaI (position 6340)/XmaI (position 10693) fragment from this mutagenized plasmid was sequenced, digested, and ligated into the same sites in pRR64 and pRR64 E2 Y18H to generate plasmids pRR64ΔRsrII and pRR64 E2 Y18H ΔRsrII.
Cells.
BHK-21 cells (ATCC CCL-10) were grown in α-minimal essential medium (Gibco) supplemented with 10% bovine calf serum (HyClone), 10% tryptose phosphate broth, penicillin and streptomycin, and 0.29 mg/ml l-glutamine. C2C12 murine muscle cells (ATCC CRL-1772) were grown in high-glucose Dulbecco's modified Eagle medium (Gibco) supplemented with 10% fetal bovine serum (Lonza), penicillin and streptomycin, 0.29 mg/ml l-glutamine, and 110 mg/liter sodium pyruvate. Normal primary human synovial fibroblasts were obtained commercially (Asterand) and grown in DMEM-F12 medium (Gibco) supplemented with 10% fetal bovine serum (Lonza), penicillin and streptomycin, and 0.29 mg/ml l-glutamine. Aedes albopictus clone C6/36 mosquito cells (ATCC CRL-1660) were grown in minimum essential medium with Earle's salts (Gibco) supplemented with 5% fetal bovine serum (Lonza), nonessential amino acids (Gibco), penicillin and streptomycin, and 0.29 mg/ml l-glutamine.
Western blots.
Culture supernatants or 105, 104, and 103 PFU of sucrose gradient-purified RRV-T48 or RRV-T48 E2 Y18H were lysed in 2× Laemmli buffer and boiled for 5 min. Lysates were separated by SDS-PAGE, and proteins were transferred onto polyvinylidene fluoride membranes (Bio-Rad). Membranes were blocked in 5% milk dissolved in phosphate-buffered saline (PBS)–0.1% Tween (PBS-T), and blocked membranes were probed with RRV immune ascitic fluid (ATCC VR-1246AF) at a 1:1,000 dilution in 5% milk dissolved in PBS-T. Secondary donkey anti-mouse horseradish peroxidase (HRP)-conjugated antibody (GE Healthcare) was used for detection at a 1:2,500 dilution in 5% milk dissolved in PBS-T. Membrane images were obtained by using a Chemi-Doc XRS+ system (Bio-Rad), and band intensities were quantified by using ImageLab software (Bio-Rad).
In vitro virus replication.
Triplicate wells were inoculated with virus at a multiplicity of infection (MOI) of 0.01 or 5. Viruses were adsorbed onto cells for 1 h at 30°C or 37°C. Wells were then washed three times with 1 ml of room temperature PBS. One milliliter of growth medium was then added to each well, and cells were incubated at 37°C or 30°C. For cumulative growth analysis, 100-μl samples of culture supernatants were removed at various times postinfection, and an equal volume of fresh growth medium was added to maintain a constant volume within each well. Samples were stored at −80°C for analysis by plaque assays on BHK-21 cells.
Competition assays.
C6/36 or C2C12 cells were plated into 24-well dishes. Growth medium was removed, and triplicate wells were inoculated at an MOI of 0.01 (C6/36) or 1 (C2C12) with a 1:1, 1:10, or 10:1 ratio of either RRV-T48 to RRV-T48 E2 Y18H-ΔRsrII or RRV-T48-ΔRsrII to RRV-T48 E2 Y18H. Viruses were adsorbed onto cells for 1 h. Wells were then washed three times with 1 ml of room temperature PBS. One milliliter of growth medium was then added to each well. Culture supernatants were collected at 24 h postinoculation (hpi) and stored at −80°C for analysis. Virus titers in the supernatants were quantified by plaque assays and used to infect additional C6/36 cells or C2C12 cells at an MOI of 0.01 or 1, respectively. Total RNA was extracted from supernatants by using a PureLink RNA minikit (Life Technologies), and cDNA was generated by using Superscript III reverse transcriptase (Life Technologies). RRV genomic DNA was amplified via PCR using primers designed to flank the endogenous RsrII restriction site (forward primer, E2 9194-5′-CACTACCAGTACTGACAAGACC-3′; reverse primer, 6K 9869-5′-CCACAGATATGCCATAGTCTCAGC-3′). PCRs were purified by using a PCR cleanup kit (Qiagen) and digested with RsrII (NEB). Digested PCR products were run on a 1.8% agarose gel, stained with ethidium bromide (Sigma), and imaged by using a Chemi-Doc XRS+ system (Bio-Rad). Relative band intensities were quantified by using ImageLab 4.0 software (Bio-Rad).
Protein expression kinetics assay.
C6/36 or C2C12 cells were plated into 24-well dishes and inoculated at an MOI of 5 with either RRV-T48 or RRV-T48 E2 Y18H. At 6, 9, 12, 18, and 24 hpi, cell lysates were collected via harvesting of cell culture supernatants, followed by one wash in room temperature PBS. After removal of PBS wash fluid, 100 μl ice-cold radioimmunoprecipitation assay (RIPA) buffer with protease inhibitors (Roche) was added to wells. Wells were then scraped, and lysates were stored at −80°C until analysis. SDS-PAGE and Western blotting were performed as described above.
Assay of PFU per cell.
C2C12 or C6/36 cells were plated into 48-well dishes and allowed to adhere for 6 or 12 h, respectively. Growth medium was removed, and cells were infected at an MOI of 5 with either RRV-T48-double-promoter green fluorescent protein (dpGFP) or RRV-T48 E2 Y18H-dpGFP. Viruses were adsorbed onto cells for 1 h. Wells were washed 5 times with 200 μl room temperature PBS. Following removal of the terminal wash fluid, 300 μl of normal growth medium was added to each well. At 18 hpi, culture supernatants were collected for titer determination on BHK-21 cells, and cells were collected via scraping (C6/36) or trypsin digestion (C2C12) and analyzed for percent GFP-positive cells by using a FACScalibur instrument (Becton Dickenson) and FlowJo analysis software (Tree Star). The total number of infected cells was calculated, and titer data were used to determine the PFU released per infected cell.
Fusion-infection assay.
Fusion of viruses with the plasma membrane was assayed by using a variation of a well-established protocol utilized to investigate fusion of Sindbis virus and Semliki Forest virus (23–25). C2C12 cells were plated into 12-well dishes and allowed to adhere for 18 h. Cells were washed twice with ice-cold RMed (RPMI without sodium bicarbonate plus 2% bovine serum albumin [BSA] and 10 mM HEPES). RRV-T48-dpGFP and RRV-T48 Y18H-dpGFP were diluted in ice-cold RMed at an MOI of 5 and allowed to adsorb onto cells for 90 min on ice. Cells were then treated with buffered ice-cold pH media (pH < 6.0, RMed plus 20 mM sodium succinate; pH ∼6.0, RMed plus 10 mM sodium succinate and 10 mM MES [morpholineethanesulfonic acid]; pH >6.0, RMed plus 20 mM MES), shifted to 37°C for 1 min, and returned to ice. Buffered fusion medium was removed and replaced with normal growth medium containing 20 mM NH4Cl to prevent secondary infection, and cells were returned to 37°C. At 18 hpi, cells were collected, fixed overnight in 1% paraformaldehyde (PFA), and then analyzed for percent GFP-positive cells by using a FACScalibur instrument (Becton Dickson) and FlowJo analysis software (Tree Star).
Analysis of E2 surface expression.
C2C12 cells were plated into 12-well dishes and mock inoculated or inoculated at an MOI of 5 with either RRV-T48 or RRV-T48 E2 Y18H. At 6 and18 hpi, cells were collected and incubated for 1 h on ice with D7 anti-RRV E2 mouse monoclonal antibody (26), a kind gift from John Aaskov (Queensland University of Technology) and Michael Rossmann (Purdue University). Bound D7 was visualized by incubating cells with phycoerythrin (PE)-conjugated goat anti-mouse secondary antibody for 1 h. After staining, cells were fixed overnight with 1% PFA and analyzed for E2 surface expression by using a FACScalibur instrument (Becton Dickson) and FlowJo analysis software (Tree Star).
Plaque assays.
BHK-21 cells or C2C12 cells were seeded into 6-well dishes. Growth medium was removed, and cell monolayers were inoculated with serial 10-fold dilutions of virus-containing samples. Samples were adsorbed for 1 h at 37°C, followed by an overlay with 0.5% immunodiffusion agarose (MP Biomedicals) in medium for 38 to 40 h. Plaques were visualized by neutral red staining (Sigma). Plaque sizes were measured by using a 10× Scale Lupe (Peak), and plaque numbers were enumerated to determine the number of BHK-21 or C2C12 PFU per ml of culture supernatant and mouse serum or BHK PFU per gram of tissue. Plaque assays performed on BHK-21 cells and C2C12 cells resulted in the detection of similar titers of infectious RRV-T48 and RRV-T48 E2Y18H.
Mouse experiments.
C57BL/6J mice were obtained from The Jackson Laboratory (Bar Harbor, ME) and bred in-house. Animal husbandry and experiments were performed in accordance with all University of Colorado School of Medicine Institutional Animal Care and Use Committee guidelines. Although RRV is classified as a biosafety level 2 pathogen, due to its exotic nature, all mouse studies were performed in a biosafety level 3 laboratory. Three- to four-week-old mice were used for all studies. Mice were inoculated in the left rear footpad with 103 or 105 PFU of virus in diluent (PBS–1% bovine calf serum) in a 10-μl volume. Mock-infected animals received diluent alone. Mice were monitored for disease signs and weighed at 24-h intervals. Disease scores were determined by assessing grip strength, hind limb weakness, and altered gait, as previously described, by using the following scoring system: 1, very mild deficit in hind paw gripping ability of injected foot only; 2, very mild deficit in bilateral hind paw gripping ability; 3, bilateral loss of gripping ability, mild bilateral hind limb paresis, and altered gait not readily observable; 4, bilateral loss of gripping ability, moderate bilateral hind limb paresis, observable altered gait, and difficulty righting self; 5, bilateral loss of gripping ability, severe bilateral hind limb paresis, altered gait, and inability to right self; and 6, moribund (19, 27). To determine virus titers in tissues, mice were euthanized by thoracotomy, blood was collected, and mice were perfused by intracardial injection of 1× PBS. The right and left ankles and right and left quadriceps muscles were removed by dissection and weighed. Tissues were homogenized in 1× PBS supplemented with 1% bovine calf serum, Ca2+, and Mg2+ with a MagNA Lyzer (Roche) and stored at −80°C. The amounts of virus present in tissue homogenates were quantified by plaque assays on BHK-21 cells.
Quantification of viral RNA.
RRV RNA in mouse tissues, culture supernatants, or gradient-purified virus stocks was quantified as previously described (27). For cell culture supernatants and gradient-purified virus stocks, 5 μl of medium or stock virus was mixed with 500 ng of a sequence-tagged (in lowercase type) RRV-specific reverse transcription (RT) primer (4415-5′-ggcagtatcgtgaattcgatgcAACACTCCCGTCGACAACAGA-3′). The reaction mixtures were incubated at 94°C for 5 min and at 70°C for 5 min prior to the RT reaction (28). A tag-sequence-specific reverse primer (5′-GGCAGTATCGTGAATTCGATGC-3′) was used with a RRV sequence-specific forward primer (RRV 4346-5′-CCGTGGCGGGTATTATCAAT-3′) and an internal TaqMan probe (RRV 4375-5′-ATTAAGAGTGTAGCCATCC-3′) during quantitative PCR (qPCR) to enhance specificity. To create a standard curve, 10-fold dilutions from 108 to 100 copies of RRV genomic RNA, synthesized in vitro, were spiked into RNA from BHK-21 cells, and reverse transcription and qPCR were performed in an identical manner. Absolute quantification was performed by using a Light Cycler 480 instrument (Roche).
Histological analysis.
At the times indicated, mice were sacrificed by exsanguination and perfused by intracardial injection of 4% paraformaldehyde (pH 7.3). Tissues were embedded in paraffin, and 5-μm sections were prepared. To assess histopathological changes such as tissue inflammation and damage, sections were stained with hematoxylin and eosin (H&E) and evaluated by light microscopy.
Statistical analysis.
Data were analyzed with Prism 5 software (GraphPad Software). Disease scores, percent weight gain, mouse tissue titers, and in vitro growth curve data were evaluated for statistically significant differences by two-way analysis of variance (ANOVA) followed by Bonferroni's posttest. The PFU/cell experiments were evaluated by using a two-tailed t test with Welch's correction. C6/36 cell competition assays were evaluated by using one-way ANOVA followed by Tukey's multiple-comparison test, while C2C12 cell competition assays were evaluated by using two-tailed t tests. A P value of <0.05 was considered statistically significant. All differences not specifically indicated to be significant were not significant (P > 0.05).
RESULTS
A single mutation in RRV E2, Y18H, results in severe attenuation in the mouse model.
In previous studies, substitution of the PE2 coding region of the mouse-virulent T48 strain of RRV with that from the attenuated DC5692 strain generated a RRV that was severely attenuated in a mouse model of alphavirus-induced musculoskeletal inflammatory disease (19). Furthermore, replacement of the PE2 coding region of the attenuated DC5692 strain with that from the virulent T48 strain, along with a substitution of the nsP1 coding region, was sufficient to restore full virulence to the DC5692 strain in the mouse model (19). These findings indicated that the PE2 coding region encodes critical virulence determinants of RRV-T48-induced rheumatic disease. Sequence comparison between the PE2 regions of the DC5692 and T48 strains showed that there were nucleotide differences in this region which resulted in seven amino acid changes (E3, R59G; E2, Y18H, I67M, H94R, R251K, H255Q, and E302V) (19). To investigate the role of specific amino acid changes in attenuation, we introduced each DC5692 coding change individually into the infectious clone of RRV-T48 and tested the ability of virus derived from these clones to cause disease in the mouse model. Inoculation of a cohort of mice (n = 3 mice per group) with 103 BHK PFU of each virus revealed that RRV E3 R59G, E2 I67M, E2 H94R, E2 R251K, E2 H256Q, or E2 E302V caused disease signs similar to those caused by the virulent RRV-T48 (P > 0.05) (Fig. 1A and B). In contrast, mice inoculated with E2 Y18H developed significantly milder disease signs (P < 0.001) (Fig. 1A and B), similar to our previously reported findings with a chimeric virus encoding the complete DC5692 PE2 coding region in the T48 strain genetic background (19). Consistent with these data, the severity of inflammatory tissue pathology in quadriceps muscle tissue was similar for RRV-T48, E3 R59G, E2 I67M, E2 H94R, E2 R251K, E2, H256Q, and E2 E302V, whereas it was markedly less severe in sections derived from mice inoculated with E2 Y18H (Fig. 1C). To confirm these results, additional mice were inoculated with RRV-T48 (n = 10) or RRV-T48 E2 Y18H (n = 11) and monitored for disease development. As shown in Fig. 1D and E, mice inoculated with E2 Y18H had significantly less severe disease signs. In addition, mice inoculated with 105 BHK PFU of RRV-T48 E2 Y18H still exhibited mild disease signs (Fig. 1D and E). Taken together, these findings indicate that a single-amino-acid change from the T48 strain-encoded tyrosine to the DC5692 strain-encoded histidine at position 18 in the RRV-T48 E2 glycoprotein results in dramatic attenuation of the virus in this mouse model of inflammatory musculoskeletal disease.
Fig 1.
RRV E2 Y18H is an attenuating mutation in a mouse model. Three- to four-week old C57BL/6J mice were inoculated with PBS or 103 PFU of RRV-T48, E3 R59G, E2 Y18H, E2 I67M, E2 H94R, E2 R251K, E2 H256Q, or E2 E302V in the left rear footpad (n = 3 per group). (A and B) At 24-h intervals, mice were assessed for weight gain (A) and scored for the development of disease signs, including loss of gripping ability, hind limb weakness, and altered gait (B). Each data point represents the arithmetic mean ± standard deviation. Data were evaluated for statistically significant differences by two-way ANOVA followed by Bonferroni's test. ***, P < 0.001. (C) At 10 dpi, mice were sacrificed and perfused with 4% paraformaldehyde. Five-micrometer-thick paraffin-embedded sections generated from the quadriceps muscle were stained with H&E. Images are representative of 3 mice per group. (D and E) Cumulative percent weight gain and disease scores for PBS-inoculated mice (n = 3) and mice inoculated with 103 PFU RRV-T48 (n = 10), 103 PFU RRV-T48 E2 Y18H (n = 14), or 105 PFU E2 Y18H (n = 3). Data are combined from 3 to 4 independent experiments. Each data point represents the arithmetic mean ± standard deviation. Data were evaluated for statistically significant differences by two-way ANOVA followed by Bonferroni's test. **, P < 0.01; ***, P < 0.001.
We next analyzed available sequence data to determine the amino acid residues present at E2 position 18 of various Ross River virus isolates (Table 1). Interestingly, all sequenced Ross River viruses encode either a Y or H at E2 position 18, suggesting a critical role for these two amino acids at this position during the RRV replication cycle. Based on serological cross-reactivity, viruses in the Alphavirus genus are classified into seven antigenic complexes (29). All E2 sequences from members of the Semliki Forest (SF) antigenic complex, which includes RRV, CHIKV, Mayaro virus, o'nyong-nyong virus, and others, possess either a Y or H at E2 position 18 (Table 1), further supporting an important role for these two amino acids at E2 position 18 in this group of medically important alphaviruses.
Table 1.
Amino acid residue at position 18 (or equivalent) of the alphavirus E2 glycoprotein
| Antigenic complex | Virus | Strain | Source(s) | Location(s) | Yr of isolation | E2 position 18 residue | GenBank accession no. |
|---|---|---|---|---|---|---|---|
| Semliki Forest | Ross River virus | 2975 | Grallina cyanoleuca (bird) | Australia (northeast) | 1965 | Y | ACV67004.1 |
| Ross River virus | 2982 | Microeca fascinans (bird) | Australia (northeast) | 1965 | Y | ACV66994.1 | |
| Ross River virus | 3078 | Poephila personata (bird) | Australia (northeast) | 1965 | Y | ACV66996.1 | |
| Ross River virus | 8961 | Macropus agilis (wallaby) | Australia (northeast) | 1965 | H | ACV66998.1 | |
| Ross River virus | 9057 | Macropus agilis (wallaby) | Australia (northeast) | 1968 | H | ACV67000.1 | |
| Ross River virus | DC5692 | Aedes camptorhynchus | Australia (western) | 1995 | H | ADJ78349.1 | |
| Ross River virus | NB5092 | Aedes vigilax | New South Wales, Australia | 1969 | X | NP_740684.1 | |
| Ross River virus | PW11 | Homo sapiens | Australia (Northwest) | 2009 | H | AEC49766.1 | |
| Ross River virus | PW14 | Homo sapiens | Australia (Northwest) | 2009 | H | AEC49788.1 | |
| Ross River virus | PW7 | Homo sapiens | Australia (Southwest) | 2010 | H | AEC49747.1 | |
| Ross River virus | QML1 | Homo sapiens | Australia (northeast) | 2004 | H | GQ433354 | |
| Ross River virus | SN39 | Homo sapiens | Australia (East Coast) | 2009 | H | AEC49809.1 | |
| Ross River virus | SN85 | Homo sapiens | Australia (Eastern) | 2009 | H | AEC49829.1 | |
| Ross River virus | T48 | Aedes vigilax | Australia (Northern) | 1959 | Y | DQ226993 | |
| Chikungunya virus | 06-027 | Homo sapiens (CS fluid) | Unknown (PMID 16700631) | 2005–2006 | H | CAJ90488.1 | |
| Chikungunya virus | 653496 | Homo sapiens | India (Nagpur) | 2003? | H | AAR84279.1 | |
| Chikungunya virus | Angola M2022 | Unknown | Angola | 1962 | H | ADG95956.1 | |
| Chikungunya virus | ArD 93229 | Aedes dalzieli | Senegal | 1993 | H | ADG95948.1 | |
| Chikungunya virus | DakAr B 16878 | Anopheles (Ceilia) funestus | Central Africa (Bououi) | 1984 | H | ADG95881.1 | |
| Chikungunya virus | DRDE-07 | Homo sapiens | India (Kerala) | 2007 | H | ACA81773.1 | |
| Chikungunya virus | Gibbs 63-263 | Homo sapiens | India | 1963 | H | ADG95936.1 | |
| Chikungunya virus | IND-06-MH2 | Unknown (PMID 17554030) | India (Maharashtra) | 2006 | H | ABN04192.1 | |
| Chikungunya virus | LR2006-OPY1 | Homo sapiens | Reunion Island | 2006 | H | ABD95938.1 | |
| Chikungunya virus | PM2951 | Aedes aegypti | Senegal | 1966 | H | ADG95883.1 | |
| Chikungunya virus | Ross low-passage | Homo sapiens | Tanzania | 1953 | H | ADG95932.1 | |
| Chikungunya virus | RSU1 | Homo sapiens | Indonesia | 1985 | H | ADG95906.1 | |
| Chikungunya virus | S27 | Homo sapiens | Tanzania | 1953 | H | AAO33341.1 | |
| Chikungunya virus | SL-CK1 | Homo sapiens | Sri Lanka | 2007 | H | ADG95913.1 | |
| Chikungunya virus | SL10571 | Homo sapiens | Sri Lanka (Japanese patient) | 2006 | H | BAH97933.1 | |
| Chikungunya virus | SL15649 | Homo sapiens | Sri Lanka | 2006 | H | ACZ72971.1 | |
| Chikungunya virus | TH35 | Homo sapiens | Thailand | 1958 | H | ADG95930.1 | |
| O'nyong-nyong virus | Gulu | Homo sapiens and Anopheles | Uganda | 1959 | H | P22056.1 | |
| O'nyong-nyong virus | SG650 | Homo sapiens | Uganda | 1996 | H | AAC97205.1 | |
| Igbo Ora | IBH10964 | Homo sapiens | Nigeria | 1966 | H | AAC97207.1 | |
| Mayaro virus | TRVL 4675 | Homo sapiens | Trinidad and Tobago | 1954 | Y | AAO33335.1 | |
| Mayaro virus | MAYLC | Homo sapiens (laboratory technician) | French Guiana | 1998 | Y | AAY45742.1 | |
| Getah virus | HB0234 | Culex tritaeniorhynchus Giles | China | 2002 | Y | ABV68937.1 | |
| Getah virus | LEIV 16275 Mag | Aedes sp. | Russia | 2000 | Y | ABR23661.1 | |
| Getah virus | LEIV 17741 | Culex sp. | Mongolia | 2000 | Y | ABR23663.1 | |
| Getah virus | Swine | Porcine | South Korea | 2004 | Y | AAU85260.1 | |
| Getah virus | YN0540 | Armigeres subalbatus | China | 2005 | Y | ABV68939.1 | |
| Sagiyama virus | Original | Adult female mosquitoes | Japan | 1956 | Y | AAO33337.1 | |
| Bebaru virus | Original | Culex sp. | Malaysia | 1956 | Y | AEJ36225.1 | |
| Una virus | Original | Psorophora ferox | Brazil | 1959 | Y | AEJ36237.1 | |
| Semliki Forest virus | A7 | Mosquitoes | Uganda | 1942? | Y | CAD90834.1 | |
| Semliki Forest virus | A774 (A7 strain) | Mosquitoes | Uganda | 1942? | Y | CAA55002.1 | |
| Semliki Forest virus | L10 | Aedes abnormalis | Uganda | 1952 | Y | AAM64227.1 | |
| Semliki Forest virus | Vietnam | Culex tritaeniorhynchus | Vietnam | 1971 | Y | ACB12688.1 | |
| Barmah Forest | Barmah Forest virus | BH2193 | Culex annulirostris | Australia | 1974 | W | NP_054024.1 |
| Western equine encephalitis | Western equine encephalitis virus | 71V1658 | Equine brain | USA | 1971 | F | ACT75286.1 |
| Western equine encephalitis virus | 85-452NM | Culex tarsalis | USA | 1985 | F | ACT75290.1 | |
| Western equine encephalitis virus | Imperial | Culex tarsalis | USA | 2005 | F | ACT75278.1 | |
| Western equine encephalitis virus | McMillan | Homo sapiens | Canada | 1941 | F | ACN87273.1 | |
| Western equine encephalitis virus | Montana-64 | Equine brain | USA | 1967 | F | ACT75282.1 | |
| Highlands J virus | 585-01 | Buteo jamaicensis (hawk) | USA | 2001 | H | ACO59902.1 | |
| Highlands J virus | 744-01 | Strix varia (barred owl) | Georgia | 2001 | H | ACZ34298.1 | |
| Highlands J virus | B-230 | Cyanocitta cristata | Florida | 1960 | H | ACT32135.1 | |
| Fort Morgan virus | CM4-146 | Oeciacus vicarius | Colorado | 1973 | R | ACT68009.1 | |
| Sindbis virus | 631310 | Culex sp. | India | 1963 | T | ACU25461.1 | |
| Sindbis virus | 95M116 | Aedes cinereus | Sweden | 1995 | T | ACU25469.1 | |
| Sindbis virus | B322/23/24 | Motacilla alba | India | 1953 | T | ACU25463.1 | |
| Sindbis virus | Girdwood | Culex univittatus | Egypt | ∼1955 | T | AAA86134.1 | |
| Sindbis virus | hrsp | Unknown | Unknown | Unknown | T | NP_740675.1 | |
| Sindbis virus | MRE-16 | Culex tritaeniorhynchus | Malaysia | 1966–1969 | T | AAC59319.1 | |
| Sindbis virus | SA80-294 | Culex univittatus | Saudi Arabia | 1980 | T | ACU25467.1 | |
| Sindbis virus | SAAR86 | Culex sp. | South Africa | 1954 | T | Unknown | |
| Sindbis virus | SW6562 | Culex annulirostris | Australia | 1990 | T | AAM10630.1 | |
| Sindbis virus | XJ-160 | Anopheles sp. | China | 1990 | T | AAC83379.1 | |
| Ockelbo virus | Edsybn 82-5 | Culiseta sp. | Sweden | 1982 | T | AAA96973.1 | |
| Eastern Equine Encephalitis | Eastern equine encephalitis virus | FL93-1637 | Culex erraticus | Florida | 1993 | D | ADB08661.1 |
| Eastern equine encephalitis virus | MA06 | Phoca vitulina (seal) | Massachusetts | 2006 | D | ACY66806.1 | |
| Eastern equine encephalitis virus | ME77132 | Mosquito | Massachusetts | 1977 | D | AAC53758.1 | |
| Eastern equine encephalitis virus | NJ/60 | Culiseta melanura | New Jersey | 1959 | D | ABQ63086.1 | |
| Eastern equine encephalitis virus | Williams | Equine brain | Connecticut | 1990 | D | AAC53760.1 | |
| Venezuelan equine encephalitis | Venezuelan equine encephalitis virus | 243937 | Horse | Venezuela | 1992 | R | AAC71998.2 |
| Venezuelan equine encephalitis virus | Fe-37c | Culex sp. | Florida | 1963 | R | P36330.1 | |
| Venezuelan equine encephalitis virus | MX01-22 | Syrian hamster | Mexico | 2001 | R | AAW30006.1 | |
| Venezuelan equine encephalitis virus | SH3 | Homo sapiens | Venezuela | 1993 | R | AAC71999.2 | |
| Venezuelan equine encephalitis virus | Trinidad donkey | Donkey | Trinidad and Tobago | 1943 | R | AAC19322.1 | |
| Venezuelan equine encephalitis virus | ZPC738 | Hamster | Venezuela | 1997 | R | AAD27803.1 | |
| Middelburg | Middelburg virus | 857 | Dead horse spleen | Zimbabwe | 1993 | Y | ABP73666.1 |
| Ndumu | Ndumu virus | Original isolate | Aedes sp. | South Africa | 1959 | Y | AEJ36231.1 |
E2 Y18H diminishes RRV replication and spread in mice.
To investigate the extent to which the reduced disease severity observed in mice inoculated with RRV-T48 E2 Y18H was associated with effects on viral replication and spread, mice were inoculated in the left rear footpad with 103 BHK PFU of RRV-T48 or RRV-T48 E2 Y18H, and the amounts of infectious virus present in tissues at 1, 3, 5, and 7 days postinoculation (dpi) were quantified by plaque assays. At 1 dpi, the titer of RRV-T48 E2 Y18H was significantly lower in the left ankle (14.6-fold decrease; P < 0.001) (Fig. 2A), a site near the site of inoculation. The titers of RRV-T48 E2 Y18H in the left ankle remained significantly lower at 3, 5, and 7 dpi (P < 0.001). More dramatic differences in virus titers were detected in tissues distal to the site of inoculation. At 1 dpi, the titer of RRV-T48 E2 Y18H was significantly lower in the right ankle (29.5-fold decrease; P < 0.001) (Fig. 2B), the left quadriceps (77.4-fold decrease; P < 0.001) (Fig. 2C), and the right quadriceps (115-fold decrease; P < 0.001) (Fig. 2D) than the titers of RRV-T48. Again, viral loads of RRV-T48 E2 Y18H in these tissues remained significantly lower at 3, 5, and 7 dpi (Fig. 2B to D). Consistent with these findings, infection with RRV-T48 E2 Y18H produced significantly lower serum viremia at 1 dpi (59.6-fold decrease; P < 0.001) and became undetectable in the serum more rapidly than RRV-T48 (Fig. 2E). To confirm these data, we utilized quantitative RT-PCR (qRT-PCR) to quantify RRV-T48 and RRV-T48 E2 Y18H RNA levels in ankle tissues and found that RRV-T48 E2 Y18H-inoculated mice had reduced RRV RNA levels in both the left and right ankles at 1 and 3 dpi (data not shown). These data indicate that the E2 Y18H mutation severely reduced RRV-T48 replication and spread in the mouse model, thus providing a likely explanation for the reduced disease severity.
Fig 2.
The E2 Y18H mutation reduces RRV tissue titers and spread. Three- to four-week old C57BL/6J mice were inoculated with 103 PFU of RRV-T48 or E2 Y18H mutant virus by injection in the left rear footpad. At 1, 3, 5, and 7 dpi, mice (n = 4 to 7) were sacrificed, blood was collected via cardiac puncture, and mice were perfused via intracardial injection with 1× PBS. Tissues were dissected, weighed, and homogenized, and the amounts of infectious virus present were quantified via plaque assays. Dashed lines indicate the limit of detection. Data were evaluated for statistically significant differences by two-way ANOVA followed by Bonferroni's test. *, P < 0.05; **, P < 0.01; ***, P < 0.001.
E2 Y18H affects RRV replication in a cell-type-dependent manner.
We next investigated the extent to which the E2 Y18H mutant virus exhibited differences in replication in cell culture. To mimic a site of infection in vivo, virus growth analyses were performed in C2C12 murine muscle cells. At an MOI of 0.01, we detected significantly reduced titers of RRV-T48 E2 Y18H in culture supernatants by 12 h postinoculation (hpi) (P < 0.05) (Fig. 3A). At 18 and 24 hpi, titers of RRV-T48 E2 Y18H were reduced 17.8-fold (P < 0.05) and 80-fold (P < 0.001), respectively, compared to titers of RRV-T48. At an MOI of 5 (Fig. 3B), we also detected significantly reduced titers of RRV-T48 E2 Y18H in culture supernatants at 18 and 24 hpi, although the differences were less dramatic than those detected when C2C12 cells were inoculated at an MOI of 0.01 (15-fold [P < 0.001] and 11.3-fold [P < 0.001] at 18 and 24 hpi, respectively). Similar differences in virus yields were detected in murine L929 fibroblasts and RAW 264.7 macrophages (data not shown). To investigate whether the E2 Y18H mutation also affected replication in human cells, virus growth analyses were performed with primary human synovial fibroblasts. Similar to the murine cells, at an MOI of 0.01, we detected significantly reduced titers of RRV-T48 E2 Y18H in culture supernatants at 18 and 24 hpi (82-fold decrease [P < 0.05] and 36-fold decrease [P < 0.001], respectively) (Fig. 3C). At an MOI of 5, the titers of RRV-T48 E2 Y18H in culture supernatants of primary human synovial cells were reduced approximately 3-fold at 18 and 24 hpi; however, these differences were not statistically significant (Fig. 3D). In contrast to these findings, when Aedes albopictus C6/36 cells were inoculated at an MOI of 0.01 (Fig. 3E), we detected significantly higher titers of RRV-T48 E2 Y18H in culture supernatants at 12 and 18 hpi (13-fold [P < 0.01] and 7.7-fold [P < 0.001] increases, respectively). When C6/36 cells were inoculated at an MOI of 5 (Fig. 3F), no significant differences in virus titers were detected. Because of the temperature difference between the C2C12 and C6/36 cell growth analyses, we next investigated replication in C2C12 cells at 30°C to determine if RRV-T48 E2 Y18H conferred a temperature-sensitive phenotype. At an MOI of 0.01, we observed that RRV-T48 E2 Y18H replicated to significantly lower titers than RRV-T48 at both 37°C and 30°C (Fig. 3G). Further characterization studies of RRV-T48 E2 Y18H indicated that the mutation did not affect virion stability at 37°C (data not shown). Taken together, these data suggest that a tyrosine at RRV-T48 E2 position 18 provides a replication advantage in murine muscle cells, whereas a histidine at RRV-T48 position 18 provides a replication advantage in C6/36 mosquito cells.
Fig 3.
The E2 Y18H mutation affects RRV replication in a cell-type-dependent manner. (A to F) C2C12 murine muscle cells (A and B), primary human synovial fibroblasts (C and D), or C6/36 mosquito cells (E and F) were inoculated with RRV-T48 or RRV-T48 E2 Y18H at an MOI of 0.01 (A, C, and E) or 5 (B, D, and F). At 0 hpi (input) and 1, 6, 12, 18, and 24 hpi, the amounts of infectious virus present in culture supernatants were quantified by plaque assays. Each data point represents the arithmetic mean ± standard deviation. Data were evaluated for statistically significant differences by two-way ANOVA followed by Bonferroni's test. *, P < 0.05; **, P < 0.01; ***, P < 0.001. (G) C2C12 murine muscle cells were inoculated with RRV-T48 or RRV-T48 E2 Y18H at an MOI of 0.01 and incubated at 37°C or 30°C. At 0 hpi (input) and 1, 12, and 24 hpi, the amounts of infectious virus present in culture supernatants were quantified by plaque assays. Each data point represents the arithmetic mean ± standard deviation. Data were evaluated for statistically significant differences by two-way ANOVA followed by Bonferroni's test. *, P < 0.05; **, P < 0.01; ***, P < 0.001.
The amino acid at RRV E2 position 18 is a determinant of virus fitness in cells.
To confirm that a Y or H at RRV E2 position 18 enhances RRV fitness in mammalian and mosquito cells, respectively, we utilized a competition assay (30, 31). A synonymous mutation (9569-5′-gccggtCcgcc-3′ → 9569-5′-gccggtAcgcc-3′) was introduced into the RRV-T48 and RRV-T48 E2 Y18H genomes, which ablated the endogenous RsrII restriction site (ΔRsrII). C6/36 cells were inoculated with a 1:1, 1:10, or 10:1 ratio of either RRV-T48 to E2 Y18HΔRsrII or RRV-T48ΔRsrII to E2 Y18H at an MOI of 0.01, and virus derived from these infections was serially passaged for a total of 5 to 10 passages. RNA was isolated from culture supernatants, the region containing the RsrII restriction site was amplified, and the relative abundance of each competitor was quantified by measuring the intensity of RsrII-digested DNA fragments, as described in Materials and Methods. As shown in Fig. 4A and B, after 5 passages, we detected increased amounts of RRV-T48 E2 Y18H in supernatants derived from C6/36 cell cultures which had been inoculated at a 1:1 ratio. Importantly, similar results were obtained in parallel competitions when either RRV-T48 (Fig. 4A) or RRV-T48 Y18H (Fig. 4B) carried the RsrII marker. Consistent with these results, RRV-T48 Y18H remained the predominant genotype detected in culture supernatants from cells that were inoculated with a 1:10 ratio of RRV-T48 to RRV-T48 Y18H (Fig. 4C and D). After 5 passages, we detected a shift in favor of RRV-T48 E2 Y18H when cells were inoculated with a 10:1 ratio of RRV-T48 to RRV-T48 Y18H (Fig. 4E and F). To further verify this, the samples with a 10:1 ratio were passaged an additional 5 times. By passage 10, RRV-T48 E2 Y18H was significantly more abundant than RRV-T48 (P < 0.001) (Fig. 4E and F). Taken together, these data suggest that a histidine at E2 position 18 of RRV provides a fitness advantage in mosquito cells. In stark contrast, similar competition experiments demonstrated that a tyrosine at RRV E2 position 18 provided a strong fitness advantage in C2C12 murine muscle cells by three passages (Fig. 4G and H).
Fig 4.
The amino acid at RRV position 18 toggles RRV fitness in disparate host cells. (A to F) C6/36 cells were inoculated at an MOI of 0.01 with a 1:1 ratio (A and B), a 1:10 ratio (C and D), or a 10:1 ratio (E and F) of either T48 to E2 Y18HΔRsrII (A, C, and E) or T48ΔRsrII to E2 Y18H (B, D, and F). At 24 hpi, culture supernatants were collected, and titers were determined on BHK-21 cells. New C6/36 cells were then inoculated at an MOI of 0.01. This process was repeated a total of 5 to 10 times. At the passages shown, total RNA was isolated from culture supernatants, and a portion of the E2 gene was amplified by RT-PCR. PCR amplicons were digested with RsrII, and band intensities of undigested and digested products were quantified to determine the relative ratios of each virus genome. Data were evaluated for statistically significant differences by two-way ANOVA followed by Bonferroni's test. **, P < 0.01; ***, P < 0.001. (G and H) C2C12 cells were infected at an MOI of 1 with a 1:1, 1:10, or 10:1 ratio of T48 to E2 Y18HΔRsrII (G) or T48ΔRsrII to E2 Y18H (H). At 24 hpi, culture supernatants were collected, and titers were determined on BHK-21 cells. New C2C12 cells were then inoculated at an MOI of 1. This process was repeated a total of three times, and the relative amounts of each genotype present in culture supernatants were quantified as described above. Data were analyzed for statistically significant differences by a two-tailed t test.
A tyrosine-to-histidine mutation at RRV E2 position 18 causes a late-stage replication defect in mammalian cells but not mosquito cells.
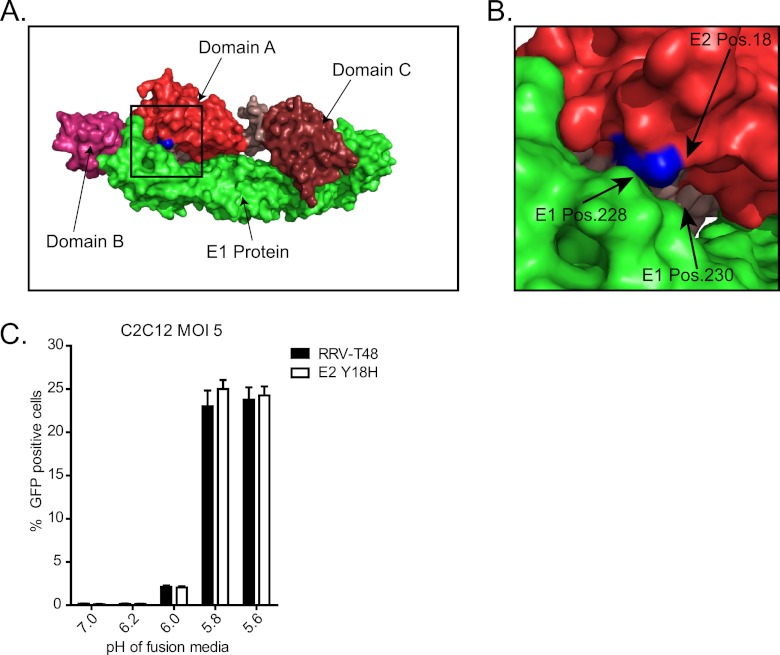
The E2 glycoprotein has a variety of functions during the alphavirus replication cycle, including receptor binding, dissociation from E1 to promote the membrane fusion reaction, spike assembly, and virion budding (32). Based on the atomic structures of the E2 glycoproteins of Sindbis virus and CHIKV, E2 position 18 is localized on the underside of E2, near the fusion loop of the E1 protein, in what Voss et al. previously termed the “N-flap” region of domain A, which is composed of E2 amino acid residues 16 to 30 (Fig. 5A and B) (33, 34). In the CHIKV structure, a histidine at E2 position 18 is predicted to interact with E1 residues 228 to 230 (Fig. 5B) and residues 142 to 146 in arch 1 of the E2 molecule present in the neighboring dimer. Due to the proximity of E2 position 18 to the fusion loop of E1 and the unique pKa properties of histidine (35), we tested whether the E2 Y18H mutation affected the pH of RRV entry. Utilizing a previously described fusion assay (23–25), we found no differences in the pH of entry between RRV-T48 and the E2 Y18H mutant virus in C2C12 cells (Fig. 5C), suggesting that this mutation regulates some other aspect of the replication cycle. To investigate if the E2 Y18H mutation affects RRV gene expression, C2C12 or C6/36 cells were infected with RRV-T48 or RRV-T48 E2 Y18H (MOI = 5), and capsid protein levels at various times postinoculation were analyzed by Western blotting (Fig. 6A and B). Despite significant differences in virus yields from C2C12 cells, but not C6/36 cells, infected at this MOI (Fig. 3B and F), quantification of capsid protein expression in C2C12 and C6/36 cells showed no significant differences between RRV-T48 and RRV-T48 E2 Y18H at any time point (Fig. 6A and B). Additionally, we utilized flow cytometry to quantify expression of E2 on the surface of infected C2C12 cells. As shown in Fig. 6C and D, the amounts of E2 protein expressed on the surface of C2C12 cells infected with RRV-T48 and RRV-T48 E2 Y18H were similar at both 6 and 18 hpi. Taken together, these results suggest that the E2 Y18H mutation does not affect steps of the RRV replication cycle such as binding, entry, fusion, and structural protein expression. To investigate whether the E2 Y18H mutation affected a late stage of the RRV replication cycle, we inoculated C2C12 or C6/36 mosquito cells with recombinant viruses that express GFP (RRV-T48-dpGFP or RRV-T48 E2 Y18H-dpGFP) and quantified the PFU released per GFP-positive cell. When C2C12 cells were infected with RRV-T48-dpGFP or RRV-T48 E2 Y18H-dpGFP, we detected a significant (P < 0.0001) but <2-fold difference in the percentage of GFP-positive cells (Fig. 7A), despite a 41-fold difference in PFU (P < 0.0001) in culture supernatants (Fig. 7C). Based on these data, we calculated that E2 Y18H virus-infected C2C12 cells released approximately 40 PFU/cell, while RRV-T48-infected C2C12 cells released approximately 1,000 PFU/cell (Fig. 7E), a 24-fold difference (P < 0.0001). In C6/36 cells, no significant differences in the percentage of GFP-positive cells were detected by flow cytometry (Fig. 7B) or fluorescence microscopy (data not shown). The PFU present in culture supernatants (P = 0.0044) (Fig. 7D) and the PFU released per infected cell (P = 0.0004) (Fig. 7F) were significantly higher for RRV-T48 E2 Y18H than for RRV-T48; however, the magnitude of these effects was quite small. Taken together, our analyses of RRV gene expression and virus production suggest that the E2 Y18H mutation affects a late stage of the RRV replication cycle in mammalian cells.
Fig 5.
The E2 Y18H mutation does not affect the pH of RRV entry. (A) Surface view of the alphavirus E1 (green) and E2 heterodimer showing the location and structural orientation of E2 domain A (red), E2 domain B (magenta), E2 domain C (maroon), E2 arches (tan), and E2 position 18 (blue). The E1-E2 heterodimer was modeled based on data reported under Protein Data Bank accession number 3N42 and was displayed by using PyMol (http://www.pymol.org/). (B) Expanded view of E2 position 18 (blue) and potential interacting residues in E1 (green). (C) RRV-T48 and RRV-T48 E2 Y18H were adsorbed onto C2C12 cells on ice at an MOI of 5. Following adsorption, cells were treated with fusion medium at the indicated pH for 1 min and then incubated in the presence of 20 mM NH4Cl. At 18 h postfusion, the percentage of GFP-positive cells was quantified by flow cytometry. No statistically significant differences were detected.
Fig 6.
The E2 Y18H mutation does not affect the kinetics or magnitude of RRV structural gene expression. C2C12 murine muscle cells or C6/36 mosquito cells were inoculated at an MOI of 5. (A) At 6, 9, 12, 18, and 24 hpi, capsid protein expression was analyzed by Western blotting. (B) Relative capsid band intensities (n = 3) were quantified by using ImageLab 4.0 software. No statistically significant differences were detected. (C and D) C2C12 cells were inoculated at an MOI of 5. At 6 and 18 hpi, cells were harvested and stained for E2 surface expression with an anti-E2 monoclonal antibody followed by a PE-conjugated secondary antibody. (C) Representative histogram displaying the anti-E2-specific fluorescence intensity of mock-, RRV-T48-, and RRV-T48 E2 Y18H-infected cells at 18 hpi. (D) The mean fluorescence intensity (MFI) of E2 staining at 6 and 18 hpi was determined by flow cytometry (n = 3). Each bar represents the arithmetic mean ± standard deviation. No significant differences were detected.
Fig 7.
The E2 Y18H mutation impacts a late stage of the RRV replication cycle. C2C12 murine muscle cells or C6/36 mosquito cells were inoculated with GFP-expressing RRV-T48 or RRV-T48 E2 Y18H at an MOI of 5. (A and B) At 18 hpi, the percentage of GFP-positive cells was quantified by flow cytometry. Each data point represents an independent culture of cells. Data were analyzed for statistically significant differences by two-tailed t tests with Welch's correction. (C and D) At 18 hpi, the amounts of infectious virus present in culture supernatants were quantified by plaque assays. Each data point represents an independent culture of cells. Data were analyzed for statistically significant differences by two-tailed t tests with Welch's correction. (E and F) The PFU released per infected cell were calculated based on the total number of PFU present in culture supernatants and the percent GFP-positive cells. Each data point represents an independent culture of cells. Data were analyzed for statistically significant differences by two-tailed Student's t test with Welch's correction.
To determine the extent to which the differences in production of infectious virus from C2C12 cells were associated with differences in the total number of particles produced, we used qRT-PCR to quantify the number of RRV RNA copies present in clarified cell culture supernatants (28). C2C12 cells infected with either RRV-T48 or the E2 Y18H mutant virus produced similar numbers of copies of RRV genomes/ml of culture supernatant (Fig. 8A), despite the significantly reduced PFU/ml detected in the supernatants of cells infected with the E2 Y18H mutant virus (P < 0.0001) (Fig. 8B). Previous Western blot and qRT-PCR analyses of sucrose gradient-purified virus stocks of RRV-T48 and RRV-T48 E2 Y18H grown in BHK-21 cells indicated that the E2 Y18H mutation had an approximately 2-fold effect on particle-to-PFU ratios (data not shown). To investigate whether the E2 Y18H mutation conferred cell-type-dependent effects on the particle-to-PFU ratio, RRV-T48 and RRV-T48 E2 Y18H were grown in BHK-21 cells or C2C12 cells, and the amounts of RRV genomes and infectious virus present in culture supernatants were quantified by qRT-PCR and plaque assays, respectively (Fig. 8C and D). In addition, a portion of the culture supernatants was utilized for sucrose gradient purification of viruses, which were then subjected to similar analyses (Fig. 8F and G). As shown in Fig. 8C, the amount of infectious RRV-T48 E2 Y18H compared to infectious RRV-T48 in cell culture supernatants was reduced in both cells lines, although the magnitude of the difference was larger in C2C12 cells (72-fold) than in BHK-21 cells (6.7-fold). In contrast, the amounts of RRV-T48 and E2 Y18H RNA present in cell culture supernatants were not significantly different in cell culture supernatants of infected BHK-21 cells or C2C12 cells (Fig. 8D). Based on these data, the genome-to-PFU ratio of the E2 Y18H mutant virus derived from C2C12 cells was increased 82-fold compared to that of C2C12-derived RRV-T48 (Fig. 8E). In contrast, the difference in the genome-to-PFU ratios of RRV-T48 and the E2 Y18H mutant virus grown in BHK-21 cells was smaller in magnitude (6.1-fold) (Fig. 8E). Similar results were detected with sucrose gradient-purified virus (Fig. 8F and G), although the magnitude of the differences in genome-to-PFU ratios between RRV-T48 and the E2 Y18H mutant virus were reduced in both BHK-21 cells and C2C12 cells (2.4-fold and 15-fold, respectively). Taken together, these results indicate that the E2 Y18H mutation has cell-type-dependent effects on production of infectious virus from cells, suggesting that this mutation affects the assembly of fully infectious virions.
Fig 8.
The E2 Y18H mutation reduces the infectivity of RRV in a cell-type-dependent manner. C2C12 murine muscle cells were inoculated with GFP-expressing RRV-T48 or RRV-T48 E2 Y18H at an MOI of 5. (A and B) RRV RNA copies (A) and PFU present in clarified C2C12 culture supernatants (B) were quantified by qRT-PCR and plaque assays, respectively. Each data point represents an individual cell culture. Data were analyzed for statistically significant differences by two-tailed t tests with Welch's correction. (C to H) RRV-T48 and RRV-T48 E2 Y18H were grown in C2C12 cells and BHK-21 cells. Clarified cell culture supernatants were analyzed directly (C to E), or virions were purified through a 60% to 20% discontinuous sucrose gradient prior to analysis (F to H). PFU (C and F) and RRV RNA copies (D and G) were quantified by plaque assays and qRT-PCR, respectively. The genome-to-PFU ratios were calculated based on the number of genomes/ml and the number of PFU/ml present in culture supernatants of gradient-purified virus stocks (E and H).
DISCUSSION
Few studies have identified viral virulence determinants that contribute to alphavirus-induced rheumatic disease. Using chimeric viruses, we previously reported that replacement of the PE2 coding region of the T48 strain of RRV with that from the attenuated DC5692 strain resulted in an attenuated disease phenotype in a mouse model of alphavirus-induced musculoskeletal inflammatory disease (19). In gain-of-virulence studies, we found that replacement of both the nsP1 and the PE2 coding regions of the DC5692 strain with those from the virulent T48 strain was required for a gain of virulence (19). In this study, we identified a single-amino-acid substitution, E2 Y18H, which functioned as the major attenuating mutation within the PE2 coding region. Furthermore, we showed that attenuation in the mouse model due to the E2 Y18H mutation was associated with reduced RRV-T48 loads in tissues and reduced RRV-T48 spread, suggesting that the mutation affected the RRV-T48 replication cycle. Consistent with these data, RRV-T48 E2 Y18H replicated less efficiently than RRV-T48 in a variety of murine and human cells. Mechanistically, we found that the E2 Y18H mutation did not affect RRV entry and gene expression. Rather, yields of infectious virus per RRV-infected cell were significantly reduced, suggesting that the amino acid at position 18 regulates a late stage of the RRV replication cycle. In contrast to the effects of this mutation in mammalian systems, RRV-T48 E2 Y18H replicated more efficiently in C6/36 mosquito cells. Competition studies in both mammalian and mosquito cells confirmed that a tyrosine at RRV E2 position 18 is advantageous in mammalian cells, whereas a histidine at RRV E2 position 18 is advantageous in mosquito cells. Thus, our studies suggest that the amino acid at RRV E2 position 18 toggles the fitness of RRV in disparate hosts.
Identification of RRV E2 Y18H as a major attenuating mutation.
To identify attenuating mutations encoded in the PE2 region, we introduced each of the attenuated RRV DC5692 strain PE2 amino acid coding changes, 7 in total, individually into the genetic backbone of the virulent RRV-T48 strain. This panel of viruses was then tested in our mouse model of RRV-induced musculoskeletal inflammatory disease, a model that recapitulates many aspects of human disease caused by arthritogenic alphaviruses (1, 11, 19). These studies revealed that a single-amino-acid change, E2 Y18H, was sufficient to recapitulate the attenuated phenotype of a chimeric virus that encoded the entire DC5692 PE2 coding region in the genetic backbone of the T48 strain (19). In comparison to RRV-T48, the E2 Y18H mutant was attenuated by all measurements of disease severity: body weight changes, musculoskeletal disease signs such as altered gait and diminished grip strength, and histopathological changes in skeletal muscle tissues (Fig. 1). While E2 Y18H was identified as the major attenuating mutation, other mutations in this region (such as E2 R251K and E2 H256Q) altered body weight changes compared to RRV-T48, suggesting that these mutations may also make minor contributions to virulence. To investigate the mechanisms of attenuation, we measured the amounts of infectious virus present in tissues near and distal to the site of inoculation at time points throughout the acute stage. These experiments demonstrated that the attenuated disease phenotype of RRV-T48 E2 Y18H was associated with significantly reduced viral loads in tissues and less efficient spread of the virus to tissues distal to the site of inoculation (Fig. 2), suggesting that the E2 Y18H mutation altered a critical aspect of the RRV replication cycle.
Recently, the structures of the Sindbis virus and CHIKV E2 proteins were solved (33, 34), allowing for the accurate placement of RRV E2 position 18 within the context of the alphavirus E1-E2 heterodimer (Fig. 5). Based on the published structures, E2 position 18 is localized on the underside of E2, near the fusion loop of the E1 protein, in what Voss et al. previously termed the N-flap domain, which is composed of E2 amino acid residues 16 to 30 (34). While a variety of studies have identified virulence determinants within the E2 glycoprotein of various alphaviruses, many of these determinants are located near the distal-most “petal” region of E2 in domain B or the outer surface of domain A, which have been implicated in host cell receptor binding, antibody neutralization, and the acquisition of mutations that increase E2 and virus binding to glycosaminoglycans (36–45). For example, an amino acid substitution in the E2 protein of CHIKV, G82R, was identified as a major attenuation determinant of the 181/clone 25 vaccine strain (36). CHIKV E2 position 82 is located on the outer surface of E2 domain A, and a glycine-to-arginine mutation at this position has been postulated to increase interactions with glycosaminoglycans, which was identified as a possible attenuating mechanism for the CHIKV 181/clone 25 strain (46). Based on the localization of position 18 within the E2 glycoprotein, it is unlikely that a tyrosine-to-histidine mutation at this position alters the interaction of RRV with cell surface glycosaminoglycans. This conclusion is supported by our own experiments that failed to detect enhanced susceptibility of RRV-T48 E2 Y18H plaque formation to preincubation with heparin (our unpublished results). Furthermore, a single-amino-acid change on the exposed petal region of RRV E2, N218R, was shown previously to confer heparan sulfate binding to RRV (47, 48). In addition to the R82G mutation, E2 T12I was also identified as a major attenuating mutation of the CHIKV 181/clone 25 vaccine strain. Interestingly, an identical mutation in Semliki Forest virus reduced the pH required to trigger E1 fusion activity by regulating the dissociation of the E1-E2 dimer (49). Although this position is near E2 position 18, the crystal structure of the CHIKV E2 glycoprotein suggests that position 12 and position 18 are in distinct domains, and as discussed below, we did not observe any effect of the RRV E2 Y18H mutation on the pH of RRV entry. Thus, to our knowledge, this study is the first to identify an important alphavirus virulence determinant in the N-flap domain of the E2 glycoprotein.
A tyrosine at position 18 is advantageous in mammalian cells, whereas a histidine at position 18 is advantageous in mosquito cells.
Our studies in mice indicated that a histidine at E2 position 18 diminished RRV replication in tissues. To investigate if the RRV-T48 E2 Y18H mutation affected RRV replication in cultured cells, we performed virus growth analyses in a variety of murine cell lines and primary human synovial cells. These experiments showed that the E2 Y18H mutant virus replicated to significantly lower titers than RRV-T48 (Fig. 3). Furthermore, these studies indicated that the effects of the E2 Y18H mutation on replication capacity were not limited to murine tissues and cells. As an arbovirus, RRV is maintained in nature by alternating cycles of replication in vertebrates and mosquitoes. Strikingly, RRV-T48 E2 Y18H replicated more efficiently than RRV-T48 in C6/36 mosquito cells, suggesting that a histidine at E2 position 18 enhances RRV fitness in mosquito cells. In both mammalian and mosquito cells, our results indicated that the effects of the E2 Y18H mutation on yields of infectious virus were MOI dependent, suggesting that the E2 Y18H mutation has subtle effects in a single replication cycle that are amplified after several cycles of replication. In addition, our experiments showed that the E2 Y18H mutant virus replicated less efficiently than RRV-T48 in C2C12 cells regardless of temperature, suggesting that the advantage of the E2 Y18H mutant virus in C6/36 cells was not due to the lower incubation temperature. In competition experiments in C2C12 cells, we detected a rapid shift in favor of the virus containing a tyrosine at E2 position 18 (Fig. 4). In contrast, competition experiments in C6/36 cells demonstrated that a histidine at E2 position 18 is advantageous for the virus, even when starting at 10-fold-lower levels. Taken together, these experiments suggest that the amino acid at RRV E2 position 18 toggles the fitness of RRV in mammalian and mosquito cells. Important future studies will investigate the extent to which a histidine at E2 position 18 provides a fitness advantage in mosquitoes.
The Alphavirus genus is composed of a diverse group of viruses. Based on serological cross-reactivity, viruses in the Alphavirus genus are classified into seven antigenic complexes, and these classifications are largely supported by recent phylogenetic analyses based on complete genomic sequences (29). We analyzed available sequence data to determine the amino acid residues present at E2 position 18 of alphaviruses from each of the antigenic complexes (Table 1). Interestingly, all E2 sequences from members of the Semliki Forest (SF) antigenic complex, which includes Ross River virus, possess either a tyrosine or histidine at position 18, suggesting a critical role for these two amino acids at this position during the virus replication cycle. Perhaps more interesting is the passage history of the various isolates, where we observed that viruses which possess a tyrosine at E2 position 18 tended to have a more extensive passage history in mammalian cells, while viruses which possess a histidine at position 18 tended to have a more insect-heavy passage history. However, this does not appear to hold true for CHIKV, which invariably encoded a histidine at E2 position 18. Further studies will be required to determine if the host passage history affects the amino acid residue at E2 position 18.
A histidine at E2 position 18 affects a late stage of the RRV replication cycle in mammalian cells.
During the alphavirus replication cycle, the E2 glycoprotein has a variety of functions during both virus entry and exit (32). Our analyses of virus growth indicated that the E2 Y18H mutation caused a significant replication defect in mammalian cells (Fig. 3). This defect was not associated with effects on the pH of RRV entry (Fig. 5), RRV gene expression kinetics (Fig. 6), or the expression of E2 on the cell surface (Fig. 6). Instead, we found that the number of PFU released per RRV-T48 E2 Y18H-infected C2C12 cell was significantly reduced in comparison to RRV-T48-infected C2C12 cells (Fig. 7). In contrast, the same analyses in mosquito cells yielded the opposite results, with RRV-T48 E2 Y18H-infected cells yielding slightly more PFU per cell, further supporting that the E2 Y18H mutation has cell-type-dependent effects and suggesting that the E2 Y18H mutation affects a late stage of the RRV replication cycle. Interestingly, quantification of RRV RNA in clarified cell culture supernatants, as an indicator of virion particle production (28), revealed that the E2 Y18H mutation did not affect particle release into the culture supernatants (Fig. 8A and B). Instead, our analyses indicated that the E2 Y18H mutation reduced the infectivity of RRV particles in a cell-type-dependent manner (Fig. 8C to H). In the crystal structure of the CHIKV E2 glycoprotein, Voss et al. identified that E2 position 18 is involved in E2-E1 contacts within E1-E2 heterodimers that form the trimeric spikes (Fig. 5) as well as E2-E2 intraspike contacts across E1-E2 heterodimers (34). These data, together with our findings, suggest that the amino acid at E2 position 18 may alter lateral interactions that are known to be critical for assembly of the trimeric spikes (50). Interestingly, Li et al. previously described results similar to our findings, where an alanine (A)-to-valine (V) mutation at position 251 of the Sindbis virus E2 glycoprotein, which arose during repeated passages of the virus in clone C7-10 Aedes albopictus mosquito cells, resulted in a virus which was defective for production of infectious virus from avian but not mosquito cells (51). However, in contrast to our findings, the Sindbis virus A251V mutation seemed to prevent the release of extracellular virions in a cell-type-dependent manner (51). More recently, Snyder et al. reported that mutation of conserved cysteines at positions 19 and 22 within the N-flap domain of the RRV-T48 E2 glycoprotein resulted in assembly defects and altered particle morphology (28), supporting the idea that the N-flap domain of E2 functions during the late stages of the RRV replication cycle, likely in assembly of infectious particles. Further experiments will be required to determine the precise processes regulated by the nature of the amino acid at position 18 and how those processes differ in vertebrate and invertebrate hosts.
ACKNOWLEDGMENTS
This research was supported by NIH NIAID research grant K22 AI079163 awarded to T.E.M. H.J.J. was supported by NIH NIAID training grant T32 AI052066. M.M.-R. was a participant in the Graduate Experiences for Multicultural Students (GEMS) research internship program at the University of Colorado Anschutz Medical Campus supported by NIH NHBLI grant R25 HL103286.
Footnotes
Published ahead of print 20 March 2013
REFERENCES
- 1. Suhrbier A, Jaffar-Bandjee MC, Gasque P. 2012. Arthritogenic alphaviruses—an overview. Nat. Rev. Rheumatol. 8:420–429 [DOI] [PubMed] [Google Scholar]
- 2. Williams MC, Woodall JP. 1961. O'nyong-nyong fever: an epidemic virus disease in East Africa. II. Isolation and some properties of the virus. Trans. R. Soc. Trop. Med. Hyg. 55:135–141 [DOI] [PubMed] [Google Scholar]
- 3. Harley D, Sleigh A, Ritchie S. 2001. Ross River virus transmission, infection, and disease: a cross-disciplinary review. Clin. Microbiol. Rev. 14:909–932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Weaver SC, Reisen WK. 2010. Present and future arboviral threats. Antiviral Res. 85:328–345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rezza G, Nicoletti L, Angelini R, Romi R, Finarelli AC, Panning M, Cordioli P, Fortuna C, Boros S, Magurano F, Silvi G, Angelini P, Dottori M, Ciufolini MG, Majori GC, Cassone A. 2007. Infection with chikungunya virus in Italy: an outbreak in a temperate region. Lancet 370:1840–1846 [DOI] [PubMed] [Google Scholar]
- 6. Grandadam M, Caro V, Plumet S, Thiberge JM, Souares Y, Failloux AB, Tolou HJ, Budelot M, Cosserat D, Leparc-Goffart I, Despres P. 2011. Chikungunya virus, southeastern France. Emerg. Infect. Dis. 17:910–913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. ProMed-mail 25 May 2011. Chikungunya: New Caledonia. ProMED-mail. Archive no. 20110525.1595 Accessed 3 August 2011 http://www.promedmail.org
- 8. Powers AM, Logue CH. 2007. Changing patterns of chikungunya virus: re-emergence of a zoonotic arbovirus. J. Gen. Virol. 88:2363–2377 [DOI] [PubMed] [Google Scholar]
- 9. Dupuis-Maguiraga L, Noret M, Brun S, Le Grand R, Gras G, Roques P. 2012. Chikungunya disease: infection-associated markers from the acute to the chronic phase of arbovirus-induced arthralgia. PLoS Negl. Trop. Dis. 6:e1446 doi:10.1371/journal.pntd.0001446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Morrison TE, Fraser RJ, Smith PN, Mahalingam S, Heise MT. 2007. Complement contributes to inflammatory tissue destruction in a mouse model of Ross River virus-induced disease. J. Virol. 81:5132–5143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Morrison TE, Whitmore AC, Shabman RS, Lidbury BA, Mahalingam S, Heise MT. 2006. Characterization of Ross River virus tropism and virus-induced inflammation in a mouse model of viral arthritis and myositis. J. Virol. 80:737–749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gunn BM, Morrison TE, Whitmore AC, Blevins LK, Hueston L, Fraser RJ, Herrero LJ, Ramirez R, Smith PN, Mahalingam S, Heise MT. 2012. Mannose binding lectin is required for alphavirus-induced arthritis/myositis. PLoS Pathog. 8:e1002586 doi:10.1371/journal.ppat.1002586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hoarau JJ, Jaffar Bandjee MC, Krejbich Trotot P, Das T, Li-Pat-Yuen G, Dassa B, Denizot M, Guichard E, Ribera A, Henni T, Tallet F, Moiton MP, Gauzere BA, Bruniquet S, Jaffar Bandjee Z, Morbidelli P, Martigny G, Jolivet M, Gay F, Grandadam M, Tolou H, Vieillard V, Debre P, Autran B, Gasque P. 2010. Persistent chronic inflammation and infection by Chikungunya arthritogenic alphavirus in spite of a robust host immune response. J. Immunol. 184:5914–5927 [DOI] [PubMed] [Google Scholar]
- 14. Parola P, de Lamballerie X, Jourdan J, Rovery C, Vaillant V, Minodier P, Brouqui P, Flahault A, Raoult D, Charrel RN. 2006. Novel chikungunya virus variant in travelers returning from Indian Ocean islands. Emerg. Infect. Dis. 12:1493–1499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Fraser JR, Cunningham AL, Clarris BJ, Aaskov JG, Leach R. 1981. Cytology of synovial effusions in epidemic polyarthritis. Aust. N. Z. J. Med. 11:168–173 [DOI] [PubMed] [Google Scholar]
- 16. Soden M, Vasudevan H, Roberts B, Coelen R, Hamlin G, Vasudevan S, La Brooy J. 2000. Detection of viral ribonucleic acid and histologic analysis of inflamed synovium in Ross River virus infection. Arthritis Rheum. 43:365–369 [DOI] [PubMed] [Google Scholar]
- 17. Hazelton RA, Hughes C, Aaskov JG. 1985. The inflammatory response in the synovium of a patient with Ross River arbovirus infection. Aust. N. Z. J. Med. 15:336–339 [DOI] [PubMed] [Google Scholar]
- 18. Ozden S, Huerre M, Riviere JP, Coffey LL, Afonso PV, Mouly V, de Monredon J, Roger JC, El Amrani M, Yvin JL, Jaffar MC, Frenkiel MP, Sourisseau M, Schwartz O, Butler-Browne G, Despres P, Gessain A, Ceccaldi PE. 2007. Human muscle satellite cells as targets of Chikungunya virus infection. PLoS One 2:e527 doi:10.1371/journal.pone.0000527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jupille HJ, Oko L, Stoermer KA, Heise MT, Mahalingam S, Gunn BM, Morrison TE. 2011. Mutations in nsP1 and PE2 are critical determinants of Ross River virus-induced musculoskeletal inflammatory disease in a mouse model. Virology 410:216–227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kuhn RJ, Niesters HG, Hong Z, Strauss JH. 1991. Infectious RNA transcripts from Ross River virus cDNA clones and the construction and characterization of defined chimeras with Sindbis virus. Virology 182:430–441 [DOI] [PubMed] [Google Scholar]
- 21. Dalgarno L, Rice CM, Strauss JH. 1983. Ross River virus 26 s RNA: complete nucleotide sequence and deduced sequence of the encoded structural proteins. Virology 129:170–187 [DOI] [PubMed] [Google Scholar]
- 22. Lindsay M, Oliveira N, Jasinska E, Johansen C, Harrington S, Wright AE, Smith D. 1996. An outbreak of Ross River virus disease in Southwestern Australia. Emerg. Infect. Dis. 2:117–120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Liao M, Kielian M. 2005. Domain III from class II fusion proteins functions as a dominant-negative inhibitor of virus membrane fusion. J. Cell Biol. 171:111–120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Qin ZL, Zheng Y, Kielian M. 2009. Role of conserved histidine residues in the low-pH dependence of the Semliki Forest virus fusion protein. J. Virol. 83:4670–4677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Liu CY, Kielian M. 2009. E1 mutants identify a critical region in the trimer interface of the Semliki forest virus fusion protein. J. Virol. 83:11298–11306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Aaskov J, Fokine A, Liu W. 2012. Ross River virus evolution: implications for vaccine development. Future Virol. 7:173–178 [Google Scholar]
- 27. Stoermer KA, Burrack A, Oko L, Montgomery SA, Borst LB, Gill RG, Morrison TE. 2012. Genetic ablation of arginase 1 in macrophages and neutrophils enhances clearance of an arthritogenic alphavirus. J. Immunol. 189:4047–4059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Snyder AJ, Sokoloski KJ, Mukhopadhyay S. 2012. Mutating conserved cysteines in the alphavirus e2 glycoprotein causes virus-specific assembly defects. J. Virol. 86:3100–3111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Forrester NL, Palacios G, Tesh RB, Savji N, Guzman H, Sherman M, Weaver SC, Lipkin WI. 2012. Genome-scale phylogeny of the alphavirus genus suggests a marine origin. J. Virol. 86:2729–2738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Tsetsarkin KA, Chen R, Leal G, Forrester N, Higgs S, Huang J, Weaver SC. 2011. Chikungunya virus emergence is constrained in Asia by lineage-specific adaptive landscapes. Proc. Natl. Acad. Sci. U. S. A. 108:7872–7877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Coffey LL, Vignuzzi M. 2011. Host alternation of chikungunya virus increases fitness while restricting population diversity and adaptability to novel selective pressures. J. Virol. 85:1025–1035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Jose J, Snyder JE, Kuhn RJ. 2009. A structural and functional perspective of alphavirus replication and assembly. Future Microbiol. 4:837–856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Li L, Jose J, Xiang Y, Kuhn RJ, Rossmann MG. 2010. Structural changes of envelope proteins during alphavirus fusion. Nature 468:705–708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Voss JE, Vaney MC, Duquerroy S, Vonrhein C, Girard-Blanc C, Crublet E, Thompson A, Bricogne G, Rey FA. 2010. Glycoprotein organization of Chikungunya virus particles revealed by X-ray crystallography. Nature 468:709–712 [DOI] [PubMed] [Google Scholar]
- 35. Thurlkill RL, Grimsley GR, Scholtz JM, Pace CN. 2006. pK values of the ionizable groups of proteins. Protein Sci. 15:1214–1218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Gorchakov R, Wang E, Leal G, Forrester NL, Plante K, Rossi SL, Partidos CD, Adams AP, Seymour RL, Weger J, Borland EM, Sherman MB, Powers AM, Osorio JE, Weaver SC. 2012. Attenuation of Chikungunya virus vaccine strain 181/clone 25 is determined by two amino acid substitutions in the E2 envelope glycoprotein. J. Virol. 86:6084–6096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Davis NL, Powell N, Greenwald GF, Willis LV, Johnson BJ, Smith JF, Johnston RE. 1991. Attenuating mutations in the E2 glycoprotein gene of Venezuelan equine encephalitis virus: construction of single and multiple mutants in a full-length cDNA clone. Virology 183:20–31 [DOI] [PubMed] [Google Scholar]
- 38. Klimstra WB, Ryman KD, Johnston RE. 1998. Adaptation of Sindbis virus to BHK cells selects for use of heparan sulfate as an attachment receptor. J. Virol. 72:7357–7366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Bernard KA, Klimstra WB, Johnston RE. 2000. Mutations in the E2 glycoprotein of Venezuelan equine encephalitis virus confer heparan sulfate interaction, low morbidity, and rapid clearance from blood of mice. Virology 276:93–103 [DOI] [PubMed] [Google Scholar]
- 40. Glasgow GM, Killen HM, Liljestrom P, Sheahan BJ, Atkins GJ. 1994. A single amino acid change in the E2 spike protein of a virulent strain of Semliki Forest virus attenuates pathogenicity. J. Gen. Virol. 75(Part 3):663–668 [DOI] [PubMed] [Google Scholar]
- 41. Glasgow GM, Sheahan BJ, Atkins GJ, Wahlberg JM, Salminen A, Liljestrom P. 1991. Two mutations in the envelope glycoprotein E2 of Semliki Forest virus affecting the maturation and entry patterns of the virus alter pathogenicity for mice. Virology 185:741–748 [DOI] [PubMed] [Google Scholar]
- 42. Santagati MG, Maatta JA, Itaranta PV, Salmi AA, Hinkkanen AE. 1995. The Semliki Forest virus E2 gene as a virulence determinant. J. Gen. Virol. 76(Part 1):47–52 [DOI] [PubMed] [Google Scholar]
- 43. Tucker PC, Griffin DE. 1991. Mechanism of altered Sindbis virus neurovirulence associated with a single-amino-acid change in the E2 glycoprotein. J. Virol. 65:1551–1557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Lee P, Knight R, Smit JM, Wilschut J, Griffin DE. 2002. A single mutation in the E2 glycoprotein important for neurovirulence influences binding of Sindbis virus to neuroblastoma cells. J. Virol. 76:6302–6310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Lustig S, Jackson AC, Hahn CS, Griffin DE, Strauss EG, Strauss JH. 1988. Molecular basis of Sindbis virus neurovirulence in mice. J. Virol. 62:2329–2336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Gardner CL, Burke CW, Higgs ST, Klimstra WB, Ryman KD. 2012. Interferon-alpha/beta deficiency greatly exacerbates arthritogenic disease in mice infected with wild-type chikungunya virus but not with the cell culture-adapted live-attenuated 181/25 vaccine candidate. Virology 425:103–112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Zhang W, Heil M, Kuhn RJ, Baker TS. 2005. Heparin binding sites on Ross River virus revealed by electron cryo-microscopy. Virology 332:511–518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Heil ML, Albee A, Strauss JH, Kuhn RJ. 2001. An amino acid substitution in the coding region of the E2 glycoprotein adapts Ross River virus to utilize heparan sulfate as an attachment moiety. J. Virol. 75:6303–6309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Glomb-Reinmund S, Kielian M. 1998. fus-1, a pH shift mutant of Semliki Forest virus, acts by altering spike subunit interactions via a mutation in the E2 subunit. J. Virol. 72:4281–4287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Ekstrom M, Liljestrom P, Garoff H. 1994. Membrane protein lateral interactions control Semliki Forest virus budding. EMBO J. 13:1058–1064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Li ML, Liao HJ, Simon LD, Stollar V. 1999. An amino acid change in the exodomain of the E2 protein of Sindbis virus, which impairs the release of virus from chicken cells but not from mosquito cells. Virology 264:187–194 [DOI] [PubMed] [Google Scholar]