Abstract
Objective
Hematopoietic stem cell transplantation (HSCT) is a demanding cancer treatment associated with enduring physical and psychological complications. Survivors' well-being may be further compromised by exposure to chronic stressors common to this population, including difficulties arising from costly medical care, changes in employment status, and health insurance coverage. Thus, we hypothesized that financial, employment, and insurance stressors (collectively referred to as economic survivorship stressors) would be associated with poorer health-related quality of life (HRQOL) among HSCT survivors.
Methods
Survivors (n=181; M=640 days post-transplant) completed measures of study variables through mailed questionnaires and telephone interviews. Hierarchical regression analyses were conducted to test the hypothesized associations between economic survivorship stressors and HRQOL, and to examine whether social and situational factors interact with survivors' stress perceptions to predict HRQOL.
Results
Greater financial and employment stress were associated with poorer functioning across multiple HRQOL domains, even after controlling for the effects of possible confounding sociodemographic and medical variables. Insurance stress was not associated with HRQOL. Some associations were moderated by situational factors including timing of the current financial crisis and portion of the transplant paid for by health insurance.
Conclusions
HSCT survivors can face serious economic challenges during recovery. Results suggest the value of viewing these challenges as chronic stressors capable of reducing survivors' mental and physical well-being. Identifying resources and skills that help survivors cope with these demands is an important goal for clinicians and researchers.
Keywords: psychological stress, finances, quality of life, stem cell transplantation, cancer survivors, oncology
Hematopoietic stem cell transplantation (HSCT) is a demanding treatment for hematologic malignancies. The toxic preparative regimen most patients receive (high-dose chemotherapy, sometimes with total body irradiation) suppresses or destroys their immune function, necessitating protective isolation and causing side effects including fatigue, cognitive difficulties, and sexual dysfunction [1–2]. For many survivors these difficulties are resolved within the first year after transplant; however, they can persist, and survivors continue to face increased risk of all-cause mortality [3–5]. HSCT has also been associated with depression, anxiety, fear of cancer recurrence, and symptoms of post-traumatic stress disorder before, during, and after transplant [4, 6–7].
These physical and psychological effects occur in conjunction with practical difficulties that have been conceptualized as chronic stressors in other populations. Here we focus on three that are interrelated and commonly reported after transplant: persistent financial, employment, and insurance stressors. These stressors (which we refer to collectively as economic survivorship stressors) have the potential to exacerbate negative physical and psychological effects of transplant, thereby reducing survivors' health-related quality of life (HRQOL). HRQOL encompasses the extent to which survivors experience a sense of well-being, have the ability to carry out activities of daily living, and experience disease-related symptoms. It represents a critical aspect of the transplant recovery and survivorship experience, and economic survivorship stressors may adversely affect HRQOL through biological, behavioral, and psychological pathways [8–9]. For instance, financial stress (perceived inadequacy of financial resources) is associated with worse physical and psychological health in community populations [10–12], and has been associated with decreased HRQOL and elevated distress among low-income survivors of breast and gynecologic cancers [13]. Cancer-related financial stress and strain have also been associated with adverse psychological well-being among survivors of breast, prostate, and lung cancer [14]. Furthermore, qualitative work conducted with cancer survivors and their caregivers has demonstrated that financial worries and difficulties have a negative impact on family lifestyle, activities, roles, and relationships [15]. In HSCT, the potential for financial stress is high because of the costliness of the treatment [2], and additional expenses due to treatment-related complications, medications, transportation to and from transplant facilities, and routine medical follow-up.
Employment-related problems are associated with financial stress, in addition to being stressful in their own right. Cancer survivors report difficulties including non-supportive work environments, changes in work schedules and relationships with colleagues, perceived employer discrimination, and reductions in perceived work ability, all of which may be persistent areas of concern with implications for their return to work, financial standing, and overall well-being [16]. Among HSCT survivors, enduring physical effects of transplant can prevent or substantially delay return to work [6]. One study found that approximately 40% of HSCT survivors had not returned to work 1-year post-transplant, and approximately 30% had not returned 2-years post-transplant [17]. Caregivers also lose income due to missed work, and incur substantial out-of-pocket expenses in order to stay at or near the treatment center [18].
Finally, many transplant survivors struggle with health insurance claims, policy caps, and obtaining future coverage. In one study approximately 32% of survivors reported that obtaining insurance was problematic, and 31% reported concerns about changing jobs for fear of losing health insurance coverage [19]. In a study of 10-year survivors of HSCT, 24% reported a history of health insurance denial compared to 0% of age-, sex-, and race-matched controls [5]. In addition to being a source of stress and frustration, insurance problems may increase financial burden among survivors who require ongoing surveillance. The role of insurance stress in cancer survivors' HRQOL has not been explored, although health insurance status has been shown to predict HRQOL in some studies. For instance, lack of insurance coverage has been associated with poorer HRQOL among survivors of prostate cancer [20]. However, insurance status was unrelated to HRQOL in a sample of Hispanic and African-American cancer patients [21].
The present study investigated these economic survivorship stressors and their association with HRQOL among survivors of HSCT. Participants were 181 men and women who had undergone HSCT 9–36 months prior to assessment. First, we examined survivors' post-transplant perceptions of financial, employment, and insurance stressors. Second, we investigated these perceived stressors as predictors of survivors' HRQOL, hypothesizing that greater economic survivorship stress would be associated with poorer HRQOL. Because stress and coping theory posits that people's perceptions of a situation (as opposed to the situation's objective characteristics) are most important in determining health [22], we predicted that associations between economic survivorship stress and HRQOL would remain even after controlling for objective indicators of socioeconomic position including income, education, and employment status. We also examined potential confounding effects of survivors' sociodemographic and medical characteristics on the hypothesized associations.
A final, exploratory aspect of this study was based on the fact that people's social environments and personal resources influence how they appraise and respond to a stressor [22]. Informed by both relative deprivation theory [23–24], which predicts that greater financial disparities are associated with poorer health in part because people experience distress when they perceive their economic standing as worse than others, and social comparison theory [25], which posits that people compare themselves to others when evaluating themselves on a particular dimension, we reasoned that survivors would appraise economic survivorship stressors differently depending on their economic standing relative to others in their social environment. We investigated the effects of the financial crisis that occurred during this study, which led to a sudden, profound shift in the economic well-being of many Americans. We hypothesized that, compared to survivors who completed the study before the crisis, those who completed it after the crisis would appraise each of these stressors as less dire because of the knowledge that many people were experiencing similar problems. Although pinpointing the exact timing of the recession is difficult, experts identify the very public failures in the financial sector in September 2008 as a pivotal turning point [26–27]. We also examined whether the portion of survivors' transplant paid by health insurance, which varies across individuals and affects how much of the treatment costs they bear, would moderate the association between economic survivorship stress and HRQOL. This situational factor may influence how people appraise their financial demands; thus, we predicted that the adverse effects of each economic survivorship stressor on HRQOL would be amplified among those participants whose insurance covered the smallest portions of their transplant expenses.
Methods
Participants were recruited through advertisements and physician referrals from Mount Sinai Medical Center and Hackensack University Medical Center as part of an IRB-approved larger study examining the efficacy of a psychosocial intervention for distressed HSCT survivors. Data for this report were obtained prior to any intervention. Eligible individuals underwent HSCT 9–36 months prior to assessment, were at least age 18 (and older than 16 at the time of HSCT), English-speaking with telephone access, not currently relapsed, and at least moderately distressed according to a screening interview that used standardized measures of generalized and cancer-specific distress.1
Interested individuals (n=272) completed screening telephone interviews to determine their eligibility after completing informed consent procedures. Eligible participants (n=238) were mailed a questionnaire including measures of perceived financial, employment, and insurance stressors, which was to be completed prior to a scheduled telephone interview. During the interview, participants provided sociodemographic, medical, and psychosocial information, including HRQOL. At the time of this report, 199 participants had completed the questionnaire and interview.
Measures
Financial stressors were assessed with two highly correlated (r=.72, p<.001) measures. The first (3 items rated from 1=“not at all” to 5=“a great deal”;[33–34]) assessed how difficult it is for people to live on their income currently, and the extent to which they anticipate facing actual financial hardships or needing to reduce their standard of living over the next two months (in the present study, Cronbach's α=.80). The second measure (6 items rated from 1=“not at all” to 4=“a great deal”;[35–36]) assessed how often in the past month people engaged in behaviors such as borrowing money to pay bills or putting off non-emergency medical treatment because of cost (in the present study, α=.86). A composite financial stress score was computed by summing standardized scores that were linearly transformed to remove negative values. Scores ranged from 0–8.1; higher scores indicate greater perceived financial stress.
Employment stressors were assessed with 12 items developed for this study to measure employment problems likely to be encountered by HSCT survivors. Because no existing measures capture perceptions of employment problems specific to this population, item development was informed by a review of the literature regarding social and practical concerns among HSCT survivors [6], and was guided by the content of feedback the research team received from HSCT survivors participating in a prior study. Items were modeled on classic, well-validated measures of life stressors [e.g., 33, 37]. Items assessed problems including needing to return to work too soon or having an unsupportive employer (see Appendix A for complete measure). If participants were working at the time of diagnosis or transplant (assessed by a separate item), they indicated whether they had experienced each problem since their diagnosis or transplant (0=no, 1=yes) and the extent to which it was upsetting (0=“not at all” to 4=“extremely”). Responses to these two questions were multiplied for each item and the resulting products were summed. Scores ranged from 0–48; higher scores indicate greater perceived employment stress (α=.76). Scores of 0 were imputed for participants not employed at the time of diagnosis or transplant.
Insurance stressors were assessed with 8 items developed for this study to measure insurance-related problems likely to be encountered by HSCT survivors. No existing measures assess perceptions of insurance-related problems specific to this population, yet feedback received by the research team from participants in a prior study identified insurance stressors as an unaddressed problem among HSCT survivors. Therefore, as above, item development was informed by literature on practical problems of HSCT survivorship, comments of prior study participants, and classic measures of life stressors. Items assessed problems including losing health insurance or an insurance company denying payment (see Appendix B for complete measure). For each item, participants indicated whether they had experienced the problem during the course of their illness or transplant (0=no, 1=yes) and the extent to which it was upsetting (0=“not at all” to 4=“extremely”). These responses were multiplied for each item and the resulting products were summed. Scores ranged from 0–32; higher scores indicate greater perceived insurance stress (α=.69).
Health-related quality of life was assessed with the well-validated Functional Assessment of Cancer Therapy-Bone Marrow Transplant (FACT-BMT) scale, Version 4 [30–31]. This measure includes five reliable subscales: physical well-being (α=.85), social/family well-being (α=.76), emotional well-being (α=.75), functional well-being (α=.81), and transplant-specific concerns (α=.65). Higher scores indicate better HRQOL.
Sociodemographic characteristics included age, ethnicity, gender (0=male, 1=female), current employment status (0=unemployed, 1=employed by self or others), years of education, and annual household income (ranging from less than $20,000 to over $110,000).
Medical variables included self-reported HSCT transplant type (0=autologous, 1=allogeneic) and the month and year transplant occurred. Medical comorbidities were assessed with the Self-Administered Comorbidity Questionnaire [38], a self-report measure which correlates with a medical record-based comorbidity instrument, patient health status, and healthcare utilization. Scores range from 0–42; higher scores indicate greater comorbidities.
Timing of the financial crisis was indicated by coding mailed questionnaires completed prior to September 1, 2008 as 0, and those completed on or after September 1, 2008 as 1.
Insurance information included whether participants had health insurance that paid for their transplant (0=no, 1=yes), and the portion of their transplant it paid (ranging from 1=“none” to 4=“all”). For descriptive purposes only, information about participants' type of insurance was also collected.
Statistical Analysis
Data were screened for missing values and violations of necessary analytic assumptions, and descriptive statistics and bivariate correlations were computed. Hierarchical linear regression was used to test whether each type of economic survivorship stress was associated with HRQOL after controlling for potential confounding variables. Thus, models were tested in which each HRQOL subscale (physical, social/family, emotional, functional, and transplant-specific concerns) was regressed separately on sociodemographic characteristics (age, ethnicity, gender, employment status, education, and income; step 1), medical variables (comorbidities, transplant type, and days since transplant; step 2), and economic survivorship stress (financial, employment, and insurance stress; step 3). Because we hypothesized that financial, employment, and insurance stress would be associated with HRQOL independently of indicators of socioeconomic position, all models included employment status, education, and income. Furthermore, because employment and insurance patterns differ by age [39], age was included as a covariate in all models; any other sociodemographic or medical variables were included based on a significant correlation (p≤.05) with the HRQOL outcome for a given model.
We examined the role of potential moderators (timing of the financial crisis and portion of the transplant paid by insurance) in an exploratory manner. For example, to test the interaction between financial stress and timing of the financial crisis, we included significant covariates and other significant types of economic survivorship stress in the initial steps of the model, and then added financial stress and timing of the crisis (i.e., the main effects), followed by an interaction term for financial stress and timing of the crisis. These analyses used mean-centered continuous variables to reduce multicollinearity [40]. Significant interactions were plotted by solving the regression equation including all predictors and covariates [40]. All statistical tests were 2-tailed with α=.05.
Results
After the removal of 18 participants with substantial missing data, data were available for 181 HSCT survivors who completed the questionnaire prior to (M=9.1, SD=10.9 days) the interview. Participant characteristics appear in Table 1; bivariate correlations and descriptive data appear in Table 2.
Table 1.
Participant characteristics (n=181)
| Characteristic | n | % |
|---|---|---|
| Gender (female) | 100 | 55.2 |
| Ethnicitya | ||
| White/non-Hispanic | 158 | 87.3 |
| Black/African American | 5 | 2.8 |
| Spanish/Latino/Hispanic | 5 | 2.8 |
| Caribbean/West Indian | 4 | 2.2 |
| Asian/Pacific Islander | 1 | 0.6 |
| Other | 8 | 4.4 |
| Highest level of education completed | ||
| Less than high school | 1 | 0.6 |
| High school | 16 | 8.8 |
| Partial college/trade school | 38 | 21.0 |
| College degree | 59 | 32.6 |
| Graduate degree | 65 | 35.9 |
| Missing | 2 | 1.1 |
| Employed by self or others | 79 | 43.6 |
| Annual household income | ||
| Less than $20,000 | 21 | 11.6 |
| $20,000–$35,000 | 14 | 7.7 |
| $35,000–$50,000 | 18 | 9.9 |
| $50,000–$65,000 | 12 | 6.6 |
| $65,000–$80,000 | 21 | 11.6 |
| $80,000–$95,000 | 21 | 11.6 |
| $95,000–$110,000 | 13 | 7.2 |
| Over $110,000 | 61 | 33.7 |
| Transplant type | ||
| Allogeneic | 97 | 53.6 |
| Autologous | 84 | 46.4 |
| Had health insurance at time of transplant | 180 | 99.4 |
| Type of health insurance | ||
| Fee-for-service (e.g., Blue Cross/Blue Shield) | 37 | 20.4 |
| Health Maintenance Organization (HMO) or other prepaid plan | 41 | 22.7 |
| PPO or Point of service | 76 | 42.0 |
| Medicaid | 9 | 5.0 |
| Medicare | 7 | 3.9 |
| Other | 7 | 3.9 |
| Missing | 4 | 2.2 |
| Portion of transplant paid by health insuranceb | ||
| None | 1 | 0.6 |
| Less than half | 0 | 0.0 |
| More than half, but not all | 65 | 36.0 |
| All | 107 | 59.1 |
| Missing | 8 | 4.4 |
| Assessment before the financial crisis (September 1, 2008) | 27 | 14.9 |
Due to variable frequencies, for analyses ethnicity was recoded as 0=White/non-Hispanic, 1=non-White.
Due to variable frequencies, for analyses portion of transplant paid by health insurance was recoded as 0=insurance paid for less than all of transplant, 1=insurance paid for all of transplant.
Table 2.
Correlations Among Study Variables (n=181)
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Financial stressa | — | .31*** | .22** | −.39*** | −.23** | −.30*** | −.31*** | −.35*** | −.21** | .16* | .12 | −.19** | −.17* | −.53*** | .10 | .05 | −.06 |
| 2. Employment stressab | — | .29*** | −.36*** | −.19* | −.16* | −.25*** | −.37*** | −.13 | .13 | −.06 | .02 | −.08 | −.17* | −.07 | .16* | −.07 | |
| 3. Insurance stressab | — | −.23b | −.12 | −.09 | −;.23** | −.16* | −.26*** | .19* | −.02 | −.03 | .02 | −.25*** | .02 | .09 | −.05 | ||
| 4. Physical well-being | — | .39* | .55* | .63* | .71* | .04 | .03 | −.05 | .17a | −.04 | .18a | −.46* | −.21b | .05 | |||
| 5. Social/family well-being | — | .37* | .53* | .51* | .07 | −.14 | −.03 | .05 | −.16a | .19b | −.22b | −.08 | .19a | ||||
| 6. Emotional well-being | — | .53* | .59* | .01 | .01 | −.07 | .07 | −.08 | .12 | −.31* | .03 | .16a | |||||
| 7. Functional well-being | — | .65* | −.03 | −.10 | −.01 | .29* | −.12 | .16a | −.43* | −.12 | .05 | ||||||
| 8. Transplant-specific concerns | — | −.02 | −.01 | −.11 | .11 | −.02 | .18a | −.40* | −.14 | .12 | |||||||
| 9. Age | — | −.06 | −.04 | −.17a | .02 | .16a | 37* | −.08 | .12 | ||||||||
| 10. Ethnicity (non-White) | — | .01 | −.10 | −.12 | −.16a | .01 | −.11 | .03 | |||||||||
| 11. Gender (female) | — | −.22b | −.12 | −.22b | .14 | .03 | .08 | ||||||||||
| 12. Employment (employed) | — | .13 | .22b | −.28* | −.01 | .03 | |||||||||||
| 13. Education, years | — | .34* | −.01 | .12 | −.16a | ||||||||||||
| 14. Income | — | −.12 | .08 | .02 | |||||||||||||
| 15. Comorbidities | — | −.06 | .02 | ||||||||||||||
| 16. Transplant type (allogeneic) | — | −.12 | |||||||||||||||
| 17. Days since transplant | — | ||||||||||||||||
|
| |||||||||||||||||
| M | 1.81 | 6.28 | 3.43 | 21.02 | 22.09 | 18.66 | 19.98 | 28.31 | 53.21 | — | — | — | 16.25 | — | 4.13 | — | 640.08 |
| SD | 1.85 | 6.87 | 4.68 | 5.45 | 4.52 | 3.70 | 4.79 | 5.46 | 11.64 | — | — | — | 2.41 | — | 3.30 | — | 263.43 |
| Range | 0–8.1 | 0–38 | 0–20 | 4–28 | 9–28 | 8–24 | 3–28 | 14–39 | 20–75 | — | — | — | 11–24 | — | 0–18 | — | 230–1190 |
Note. Variable categories in parentheses correspond to the highest coding value (e.g., non-White coded as 1 whereas White/non-Hispanic coded as 0). Pearson correlation coefficients are provided for associations between continuous variables; point-biserial correlation coefficients are provided for associations between continuous and dichotomous variables.
Variable centered for interaction analyses; table statistics computed with original variable.
Variable log transformed to correct for nonnormality; table statistics computed with original variable.
=p≤.05;
=p≤.01;
=p≤.001
Perceptions of Economic Survivorship Stressors
On average, participants reported relatively low financial stress (M=1.81, SD=1.85). However, participants' scores spanned the scale's range, demonstrating the variability of their responses. Sources of financial stress most frequently endorsed as occurring moderately or a great deal in the past month included reducing or cancelling vacations or leisure activities (34% of participants), reducing spending on household expenses such as food or clothing (33%), and deciding not to buy something they had planned to purchase (28%). Additionally, 23% of participants felt it was difficult, very difficult, or extremely difficult to live on their income, and 22% at least somewhat anticipated needing to reduce their standard of living to the bare necessities of life.
Although 73% of participants were working at the time of their diagnosis or transplant, only 44% were currently employed. On average, participants reported relatively low employment stress since the time of their diagnosis or transplant (M=8.15, SD=6.88 among those employed at the time of diagnosis or transplant; M=6.28, SD=6.87 among the full sample); however, 87% of those employed at the time of diagnosis or transplant reported some employment stress. Among these participants, the most common problem was a pay cut or loss of income due to their illness (reported by 67% of participants, of whom 46% reported it was very or extremely upsetting). The next most common problems included needing to go on disability (63% of participants) and needing to take a paid leave of absence (55%). These problems were reported as very or extremely upsetting by 29% and 18% of those who experienced these stressors, respectively.
All but one participant (n=180) had health insurance at the time of transplant. Most (59%) reported that insurance paid for all their transplant expenses. On average, insurance stress experienced during the course of their illness or transplant was low (M=3.43, SD=4.68); 41% of participants reported no insurance stress. Among participants who did experience problems, the most common involved spending a lot of time dealing with their health insurance company (reported by 38% of participants, of whom 51% reported it was very or extremely upsetting), someone else spending a lot of time dealing with their insurance company (34% of participants, of whom 33% reported it was very or extremely upsetting), and the insurance company denying a payment (22% of participants, of whom 76% reported it was very or extremely upsetting).
Economic Survivorship Stress and HRQOL
Results of the hierarchical regression analyses indicated that financial stress was most consistently related to HRQOL (Table 3). As predicted, it was inversely associated with physical well-being (p<.001), emotional well-being (p=.001), functional well-being (p=.005), and transplant-related concerns (p=.001). Similarly, employment stress was inversely related to physical well-being (p<.001), functional well-being (p=.01), and transplant-specific concerns (p<.001). Insurance stress did not predict HRQOL. One aspect of HRQOL—social/family well-being—was unrelated to economic survivorship stress.
Table 3.
Hierarchical Regression Analyses Predicting HRQOL from Sociodemographic Characteristics, Medical Variables, and Economic Survivorship Stress (n=181)
| Predictor | Physical well-being |
Social/family well-being |
Emotional well-being |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| R2 change | β | F change | t | R2 change | β | F change | t | R2 change | β | F change | t | |
| Step 1: | .06 | 2.96* | .10 | 4.73*** | .03 | 1.51 | ||||||
| Sociodemographic | ||||||||||||
| Age | .16 | 2.47* | .10 | 1.22 | .06 | .70 | ||||||
| Ethnicity (non-White) | — | — | — | — | — | — | ||||||
| Gender (female) | — | — | — | — | — | — | ||||||
| Employment (employed) | .05 | .79 | −.02 | −.31 | −.04 | −.52 | ||||||
| Education | −.05 | −.80 | −.22 | −2.91** | −.09 | −1.20 | ||||||
| Income | −.07 | −.90 | .17 | 1.92 | −.04 | −.46 | ||||||
| Step 2: | .26 | 34.21*** | .07 | 6.92*** | .11 | 11.34*** | ||||||
| Medical | ||||||||||||
| Comorbidities | −.53 | −8.29*** | −.26 | −3.27*** | −.33 | −4.28*** | ||||||
| Transplant type (allogeneic) | −.16 | −2.78** | — | — | — | — | ||||||
| Days since transplant | — | — | .13 | 1.80 | .12 | 1.77 | ||||||
| Step 3: | .13 | 13.54*** | .03 | 2.20 | .07 | 4.79** | ||||||
| Economic Survivorship Stress | ||||||||||||
| Financial stress | −.28 | −4.05*** | −.12 | −1.43 | −.28 | −3.36*** | ||||||
| Employment stress | −.24 | −3.97*** | −.13 | −1.74 | −.08 | −1.07 | ||||||
| Insurance stress | .01 | .18 | .08 | 1.06 | .03 | .46 | ||||||
| Predictor | Functional well-being |
Transplant-specific concerns |
||||||
|---|---|---|---|---|---|---|---|---|
| R2 change | β | F change | t | R2 change | β | F change | t | |
| Step 1: | .13 | 6.63*** | .05 | 2.13 | ||||
| Sociodemographic | ||||||||
| Age | .09 | 1.22 | .08 | 1.06 | ||||
| Ethnicity (non-White) | — | — | — | — | ||||
| Gender (female) | — | — | — | — | ||||
| Employment (employed) | .20 | 2.94** | .02 | .23 | ||||
| Education | −.16 | −2.47* | −.05 | −.78 | ||||
| Income | −.04 | −.56 | −.03 | −.39 | ||||
| Step 2: | .14 | 33.62*** | .15 | 31.97*** | ||||
| Medical | ||||||||
| Comorbidities | −.42 | −5.95*** | −.45 | −6.43*** | ||||
| Transplant type (allogeneic) | — | — | — | — | ||||
| Days since transplant | — | — | — | — | ||||
| Step 3: | .08 | .16 | 14.44*** | |||||
| Economic Survivorship Stress | ||||||||
| Financial stress | −.21 | −2.83** | −.25 | −3.28*** | ||||
| Employment stress | −.17 | −2.56* | −.32 | −4.85*** | ||||
| Insurance stress | −.08 | −1.12 | .03 | .38 | ||||
Note. Dashes (—) indicate a variable was omitted due to a nonsignificant (p<.05) association with the HRQOL outcome.
p≤.05;
p≤.01;
p≤.001
Moderation Analyses
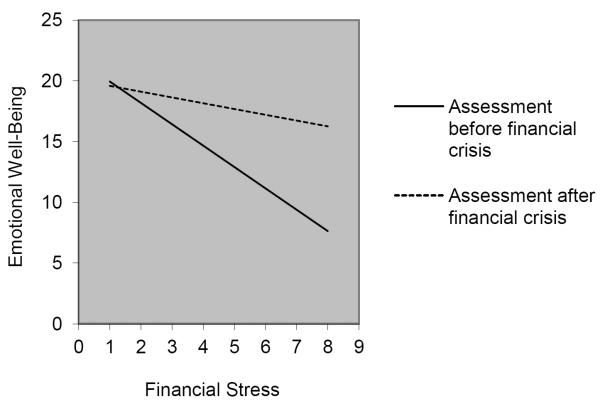
Additional analyses suggested that timing of the financial crisis and portion of transplant paid by insurance did moderate some associations between types of economic survivorship stress and HRQOL; however, when the analyses were corrected for multiple comparisons, these effects exceeded the conservative Bonferroni-corrected α=.01 and thus should be interpreted as marginally significant. Specifically, results suggested that the timing of the financial crisis moderated the association between financial stress and emotional well-being, t(175)=2.41, p=.02, effect size (partial r)=.18. As shown in Figure 1, the inverse association between financial stress and emotional well-being was stronger for participants assessed before the financial crisis than for participants assessed after the crisis. Timing of the financial crisis also moderated the association between employment stress and physical well-being, t(173)=2.40, p=.02, effect size=.18; and between employment stress and functional well-being, t(173)=2.03, p=.04, effect size=.15. These interactions demonstrated a pattern similar to that shown in Figure 1. Thus, the inverse association between employment stress and HRQOL was stronger for participants assessed before the crisis than for participants assessed after.
Figure 1.
Timing of the financial crisis and financial stress interact to predict emotional well-being. Higher emotional well-being scores indicate better HRQOL.
We confirmed that survivors assessed before and after the crisis differed in neither their mean financial (t(179)= −1.15, p=.25) nor employment (t(179)= −1.27, p=.21) stress, thereby highlighting the influence of survivors' psychological rather than objective burden on HRQOL.2 To further explore these interactions, we used the regression equations to predict survivors' HRQOL at the highest levels of stress reported in our sample, and compared these predicted values to published norms for transplant recipients' HRQOL 1-year post-transplant [41].3 At the highest level of financial stress, emotional well-being among survivors assessed after the crisis (predicted M=14.1) was similar to the published norm for this HRQOL subscale (M=16.8, SD=2.5;[41]); however, emotional well-being among survivors assessed before the crisis (predicted M=7.8) was far worse (i.e., more than three SDs below the published norm). Similar patterns emerged upon comparing the published norm for physical well-being (M=22.6, SD=4.8;[41]) to survivors' physical HRQOL at the highest level of employment stress for those assessed after (predicted M=19.9) as opposed to before (predicted M=14.9) the crisis, and upon comparing the published norm for functional well-being (M=19.5, SD=5.0;[41]) to survivors' functional HRQOL for those assessed after (predicted M=19.6) as opposed to before (predicted M=15.9) the crisis.
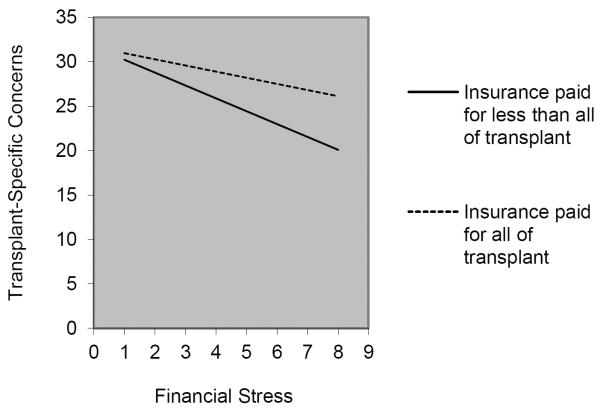
Additionally, results suggested that the portion of the transplant paid by health insurance moderated the association between financial stress and transplant-specific concerns, t(167)=2.25, p=.03, effect size=.17. As shown in Figure 2, this inverse association of financial stress with HRQOL was stronger for participants whose insurance paid less than all of their expenses than for those whose insurance paid all of their expenses. Portion of the transplant paid by insurance did not moderate any other associations between stress and HRQOL. Mean financial stress did not differ among survivors based on portion of transplant paid by insurance, t(171)=.22, p=.83. Additional comparisons indicated that at the highest level of financial stress, the transplant-specific HRQOL of survivors whose insurance paid all their expenses (predicted M=26.1) was similar to the published norm (M=27.0, SD=5.8;[31]).4 Yet, the HRQOL of survivors with residual expenses not covered by insurance (predicted M=20.1) was more than one SD below the published norm.
Figure 2.
Portion of the transplant paid by health insurance and financial stress interact to predict transplant-specific concerns. Higher transplant-specific concerns scores indicate better HRQOL.
Discussion
Many HSCT survivors report having to cope with persistent stress associated with finances, employment, and health insurance. Indeed, compared to other cancer populations, they may be particularly vulnerable to these difficulties because of the expensive and prolonged nature of HSCT treatment and recovery. As hypothesized and consistent with research on chronic stress [8–9], these economic survivorship stressors were associated with survivors' physical and psychological well-being. Specifically, greater perceptions of financial stress and employment stress were associated with poorer physical, functional, and transplant-specific functioning. Greater financial stress was also associated with poorer emotional functioning. These associations could not be explained by survivors' socioeconomic position, background characteristics, or medical factors. Consistent with stress and coping theory [22], and relative deprivation theory [23–24], survivors' perceptions of their economic situation were uniquely associated with their HRQOL. Results suggest that rather than merely being practical problems complicating survivors' lives, financial and employment difficulties need to be viewed as sources of chronic stress with implications for survivors' health long after treatment has ended.
Contrary to our expectations, economic survivorship stress was not associated with social functioning. Financial limitations can strain interpersonal relationships among cancer survivors [15], yet these effects may be mitigated by factors such as social support and coping behaviors [e.g., 43]. It is unknown whether such factors may explain why survivors' economic problems were unrelated to their social well-being. Furthermore, insurance stress was not associated with survivors' HRQOL. Although insurance-related problems may be frustrating without contributing to poor functioning, it is also possible that characteristics of the sample and study measures made detecting such effects unlikely. Virtually all participants had health insurance coverage, and the majority of participants' insurance plans covered all their transplant expenses. This rate of insurance coverage is somewhat higher than that reported in a recent study in which 6% of non-Hispanic White HSCT patients and 24% of Hispanic HSCT patients were uninsured [44]. Also, our measure of insurance stress demonstrated relatively little variability (understandable given the favorable insurance status of most participants) and focused primarily on difficulties encountered during transplantation rather than on current challenges. Thus, we may have failed to capture sources of insurance stress in later stages of recovery. As such, further research is warranted.
Results regarding social and situational moderators of associations between economic survivorship stress and HRQOL further demonstrate the importance of survivors' perceptual experience of stressors, and although these findings are only marginally statistically significant after correcting for multiple comparisons, the same pattern of results emerges across various HRQOL domains and are consistent with existing theory [22–25]. As predicted, the timing of the financial crisis influenced the strength of the association between economic survivorship stress and well-being. Whereas survivors assessed before the crisis experienced steep reductions in HRQOL with increasing stress, survivors assessed after the crisis experienced only minimal reductions. Furthermore, at the highest levels of economic survivorship stress, HRQOL among survivors assessed before the crisis was far poorer than both published norms [41] and that observed among survivors assessed after the crisis.
These results suggest that the association between economic survivorship stress and HRQOL was stronger before the economic recession than after. Although it is seemingly paradoxical that economic survivorship stress is less strongly associated with HRQOL in the context of the financial crisis, these results are consistent with relative deprivation theory [23–24], which predicts that disparities in wealth are associated with poorer health in part because people experience distress upon perceiving their economic standing as worse than others. It could be that survivors assessed prior to the financial crisis perceived greater financial inequalities, which led to negative feelings and self-evaluations. However, survivors assessed after the crisis may have benefited from a perceived reduction in an inequitable distribution of resources. Such possibilities should be explored with future studies.
Situational factors also influenced the association between financial stress and transplant-specific functioning. Among survivors whose health insurance paid for all transplant expenses, increases in financial stress were associated with minimal decreases in transplant-specific functioning. Yet, for survivors with residual expenses not covered by insurance, increasing financial stress was associated with substantial decreases in HRQOL. These results suggest that survivors with insufficient health insurance coverage may be especially vulnerable to the detrimental effects of economic survivorship stress.
Limitations and Future Directions
Because this study was cross-sectional, we cannot make firm conclusions about a causal relationship between economic survivorship stress and health. Associations may be bidirectional or operate in the reverse direction. For example, survivors in worse health with poorer functioning are likely to incur greater expenses. We controlled several important medical variables to address this possibility; these factors did not explain the observed associations. We relied on novel measures of employment and insurance stress to capture experiences common to the study population. Although items were developed based on feedback from HSCT survivors and item wording was modeled after existing measures of life stressors, it is unclear whether the use of unvalidated measures contributed to the observed pattern of results. Furthermore, although the occurrence of the financial crisis during this study provided us with a valuable research opportunity, it should be noted that the dichotomization of the timing of the financial crisis as pre- and post-September 2008 resulted in subsamples of differing sizes which limited our statistical power for analyses involving this variable, and may not have fully captured the complex impact of the economic recession.
The generalizability of these findings is likely limited by the fact that study eligibility required participants to be moderately distressed and willing to participate in a psychosocial intervention; this sample reported low levels of financial, employment, and insurance stress; participants were primarily White/non-Hispanic; many had high incomes (e.g., only 29.2% reported an income below the 2009 US median household income;[45]); and nearly all were insured. Yet, despite this sample's objective economic stability, participants' financial stress scores spanned the full range of the scale and significant associations were consistently observed across HRQOL domains. To further our understanding of the relationship between economic survivorship stress and HRQOL, future studies should include a more diverse group of participants, including those of various racial and ethnic backgrounds, socioeconomic positions, and insurance statuses. For example, by incorporating measures of perceived economic survivorship stressors and HRQOL into prospective cohort study designs that recruit participants at the time of cancer diagnosis, it would be possible to determine how these variables are associated among diverse participants, including those who ultimately fail to proceed to transplant due to financial limitations or those whose disease recurs. Such studies, using longitudinal designs with multiple assessments across the treatment and recovery periods, would enhance our knowledge of this important relationship.
Conclusions
Cancer patients experience multiple challenges during the course of their disease, and for many, these difficulties persist as they navigate life as a survivor. Given both the steady increase over the past 40 years in the number of cancer survivors [46], and recent estimates that over 2 million survivors have forgone one or more needed medical services due to financial concerns [47], economic challenges represent an emerging area of importance. Our findings suggest that persistent financial demands and employment complications may be especially problematic for HSCT survivors' physical and psychological well-being. Yet these stressors are modifiable determinants of health, particularly to the extent that survivors' subjective perceptions contribute to their adverse effects. Traditional oncology treatment strategies focus primarily on physical aspects of patient care [48–49], and are not well-suited to address survivors' subjective experiences and psychosocial needs related to economic stressors. Although some resources exist to help survivors cope with financial, employment, and insurance problems, these services are frequently provided by patient advocacy groups and non-profit organizations [50], and therefore operate outside the formal healthcare system. HSCT survivors would benefit from clinical management by multidisciplnary teams that include psychologists, social workers, patient navigators, or others with expertise to help survivors adjust to the economic challenges engendered by their treatment and recovery. Identifying resources and skills that help survivors cope with these demands is an important goal for clinicians and researchers.
Acknowledgements
This research was supported by funding from the American Cancer Society (PI: Rini; grant #RSGPB-07-285-01-CPPB).
Appendix A Employment Stressors in Hematopoietic Stem Cell Transplantation (HSCT) Questionnaire
Instructions. Listed below are a number of job-related events that some people have said are upsetting to them. If you were working at the time of your diagnosis or transplant, please indicate whether you experienced each event and how upset you were by it.
Were you working at the time of your diagnosis or transplant?
-
__
No (stop here and skip remaining questions)
-
__
Yes (answer remaining questions)
| A. Did this happen to you? |
B. If it did happen, how upsetting was it? |
||||||
|---|---|---|---|---|---|---|---|
| No | Yes | Not at all upsetting |
A little bit upsetting |
Moderately upsetting |
Very upsetting |
Extremely upsetting |
|
| 1. Fired from your job as a result of your illness/transplant |
0 | 1 | 2 | 3 | 4 | ||
| 2. Had to take a paid leave of absence due to your illness/transplant |
0 | 1 | 2 | 3 | 4 | ||
| 3. Had to take an unpaid leave of absence due to your illness/transplant |
0 | 1 | 2 | 3 | 4 | ||
| 4. Had to quit your job or retire as a result of your illness/transplant |
0 | 1 | 2 | 3 | 4 | ||
| 5. Experienced a pay cut or loss of income due to your illness/transplant |
0 | 1 | 2 | 3 | 4 | ||
| 6. You had to go on disability due to your illness/transplant |
0 | 1 | 2 | 3 | 4 | ||
| 7. You were threatened with losing your job due to your illness/transplant |
0 | 1 | 2 | 3 | 4 | ||
| 8. Your partner's work situation was hurt by your illness/transplant |
0 | 1 | 2 | 3 | 4 | ||
| 9. Your employer was unsupportive | 0 | 1 | 2 | 3 | 4 | ||
| 10. Your partner's employer was unsupportive |
0 | 1 | 2 | 3 | 4 | ||
| 11. You had to go back to work too soon after your illness/transplant |
0 | 1 | 2 | 3 | 4 | ||
| 12. You could not go back to work as soon as you wanted after your illness/transplant |
0 | 1 | 2 | 3 | 4 | ||
Note. Responses to Part A are first coded such that “No”=0 and “Yes”=1. Next, for each item, responses to Part A and Part B are multiplied. The resulting products are then summed. Scores range from 0–48 with higher scores indicating greater perceived employment stress.
Appendix B Insurance Stressors in Hematopoietic Stem Cell Transplantation (HSCT) Questionnaire
Instructions. Listed below are a number of events related to health insurance that some people have said are upsetting to them. Please indicate whether you experienced each event and how upset you were by it
| A. Did this happen to you? |
B. If it did happen, how upsetting was it? |
||||||
|---|---|---|---|---|---|---|---|
| No | Yes | Not at all upsetting |
A little bit upsetting |
Moderately upsetting |
Very upsetting |
Extremely upsetting |
|
| 1. You had to have your transplant at a treatment center that was not your first choice because of your health insurance coverage |
0 | 1 | 2 | 3 | 4 | ||
| 2. You had to have your transplant at a treatment center that was far from home because of your health insurance coverage |
0 | 1 | 2 | 3 | 4 | ||
| 3. You lost your health insurance coverage at some point during your illness/transplant |
0 | 1 | 2 | 3 | 4 | ||
| 4. You had to change health insurance carriers because of your illness/transplant |
0 | 1 | 2 | 3 | 4 | ||
| 5. You spent a lot of time dealing with your health insurance company (for instance, to arrange approvals or sort out coverage problems) |
0 | 1 | 2 | 3 | 4 | ||
| 6. Someone else had to spend a lot of time dealing with your health insurance company (for instance, to arrange approvals and sort out coverage problems) |
0 | 1 | 2 | 3 | 4 | ||
| 7. Your health insurance company denied payment at some point during your illness/transplant |
0 | 1 | 2 | 3 | 4 | ||
| 8. Problems with your health insurance company caused some or all of your treatment to be delayed |
0 | 1 | 2 | 3 | 4 | ||
Note. Responses to Part A are first coded such that “No”=0 and “Yes”=1. Next, for each item, responses to Part A and Part B are multiplied. The resulting products are then summed. Scores range from 0–32, with higher scores indicating greater perceived insurance stress.
Footnotes
The authors have no financial interests to disclose.
Eligible participants demonstrated at least moderate distress on one or more of the following measures: Impact of Event Scale [28], Brief Symptom Inventory-Global Severity Index [29], Functional Assessment of Cancer Therapy-Bone Marrow Transplant scale [30–31], or Life Engagement Test [32]. Exact cut-offs are available from the last author.
These two groups also did not differ on any sociodemographic, medical, or other study variables (all ps≥.08), suggesting that group differences were not due to methodological factors (e.g., bias due to joining the trial earlier compared to later).
Published norms only exist for the FACT-BMT Version 3. To allow comparisons across Versions 3 and 4, adjustments were made to participants' scores on the emotional subscale [30]. No adjustments were required for the physical and functional subscales due to item similarly across versions.
Because published norms for survivors 1-year post-transplant were computed in a manner inconsistent with current scoring recommendations [42], this comparison used appropriately-computed published norms for survivors 100-days post-transplant.
References
- 1.Appelbaum FR. The use of bone marrow acid peripheral blood stem cell transplantation in the treatment of cancer. CA Cancer J Clin. 1996;46:142–164. doi: 10.3322/canjclin.46.3.142. DOI: 10.3322/canjclin.46.3.142. [DOI] [PubMed] [Google Scholar]
- 2.Copelan EA. Hematopoietic stem-cell transplantation. N Engl J Med. 2006;354:1813–1826. doi: 10.1056/NEJMra052638. DOI: 10.1056/NEJMra052638. [DOI] [PubMed] [Google Scholar]
- 3.Andrykowski MA, Bishop MM, Hahn EA, Cella DF, Beaumont JL, Brady MJ, et al. Long-term health-related quality of life, growth, and spiritual well-being after hematopoietic stem-cell transplantation. J Clin Oncol. 2005;23:599–608. doi: 10.1200/JCO.2005.03.189. DOI: 10.1200/jco.2005.03.189. [DOI] [PubMed] [Google Scholar]
- 4.Syrjala KL, Langer SL, Abrams JR, Storer B, Sanders JE, Flowers MED, et al. Recovery and long-term function after hematopoietic cell transplantation for leukemia or lymphoma. JAMA. 2004;291:2335–2343. doi: 10.1001/jama.291.19.2335. DOI: 10.1001/jama.291.19.2335. [DOI] [PubMed] [Google Scholar]
- 5.Syrjala KL, Langer SL, Abrams JR, Storer BE, Martin PJ. Late effects of hematopoietic cell transplantation among 10-year adult survivors compared with case-matched controls. J Clin Oncol. 2005;23:6596–6606. doi: 10.1200/JCO.2005.12.674. DOI: 10.1200/jco.2005.12.674. [DOI] [PubMed] [Google Scholar]
- 6.Mosher CE, Redd WH, Rini CM, Burkhalter JE, DuHamel KN. Physical, psychological, and social sequelae following hematopoietic stem cell transplantation: A review of the literature. Psycho-Oncol. 2009;18:113–127. doi: 10.1002/pon.1399. DOI: 10.1002/pon.1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Prieto JM, Atala J, Blanch J, Carreras E, Rovira M, Cirera E, et al. Patient-rated emotional and physical functioning among hematologic cancer patients during hospitalization for stem-cell transplatation. Bone Marrow Transplant. 2005;35:307–314. doi: 10.1038/sj.bmt.1704788. DOI: 10.1038/sj.bmt.1704788. [DOI] [PubMed] [Google Scholar]
- 8.Andersen BL, Kiecolt-Glaser JK, Glaser R. A biobehavioral model of cancer stress and disease course. Am Psychol. 1994;49:389–404. doi: 10.1037//0003-066x.49.5.389. DOI: 10.1037//0003-066X.49.5.389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McEwen BS, Gianaros PJ. Central role of the brain in stress and adaptation: Links to socioeconomic status, health, and disease. Ann N Y Acad Sci. 2010;1186:190–222. doi: 10.1111/j.1749-6632.2009.05331.x. DOI: 10.1111/j.1749-6632.2009.05331.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kahn JR, Pearlin LI. Financial strain over the life course and health among older adults. J Health Soc Behav. 2006;47:17–31. doi: 10.1177/002214650604700102. DOI: 10.1177/002214650604700102. [DOI] [PubMed] [Google Scholar]
- 11.McGonagle KA, Kessler RC. Chronic stress, acute stress, and depressive symptoms. Am J Community Psychol. 1990;18:681–706. doi: 10.1007/BF00931237. DOI: 10.1007/BF00931237. [DOI] [PubMed] [Google Scholar]
- 12.Rosengren A, Hawken S, Ôunpuu S, Sliwa K, Zubaid M, Almahmeed WA, et al. Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the INTERHEART study): Case-control study. Lancet. 2004;364:953–962. doi: 10.1016/S0140-6736(04)17019-0. DOI: 10.1016/S0140-6736(04)17019-0. [DOI] [PubMed] [Google Scholar]
- 13.Ell K, Xie B, Wells A, Nedjat-Haiem F, Lee P-J, Vourlekis B. Economic stress among low-income women with cancer. Cancer. 2008;112:616–625. doi: 10.1002/cncr.23203. DOI: 10.1002/cncr.23203. [DOI] [PubMed] [Google Scholar]
- 14.Sharp L, Carsin A-E, Timmons A. Associations between cancer-related financial stress and strain and psychological well-being among individuals living with cancer. Psycho-Oncol. 2012 doi: 10.1002/pon.3055. DOI: 10.1002/pon.3055. [DOI] [PubMed] [Google Scholar]
- 15.Amir Z, Wilson K, Hennings J, Young A. The meaning of cancer: Implications for family finances and consequent impact on lifestyle, activities, roles and relationships. Psycho-Oncol. 2011 doi: 10.1002/pon.2021. DOI: 10.1002/pon.2021. [DOI] [PubMed] [Google Scholar]
- 16.Mehnert A. Employment and work-related issues in cancer survivors. Crit Rev Oncol Hematol. 2011;77:109–130. doi: 10.1016/j.critrevonc.2010.01.004. DOI: 10.1016/j.critrevonc.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 17.Lee SJ, Fairclough D, Parsons SK, Soiffer RJ, Fisher DC, Schlossman RL, et al. Recovery after stem-cell transplantation for hematologic diseases. J Clin Oncol. 2001;19:242–252. doi: 10.1200/JCO.2001.19.1.242. [DOI] [PubMed] [Google Scholar]
- 18.Meehan KR, Fitzmaurice T, Root L, Kimtis E, Patchett L, Hill J. The financial requirements and time commitments of caregivers for autologous stem cell transplant recipients. J Support Oncol. 2006;4:187–190. [PubMed] [Google Scholar]
- 19.Baker F, Denniston M, Zabora JR, Marcellus D. Cancer problems in living and quality of life after bone marrow transplantation. J Clin Psychol Med Settings. 2003;10:27–34. doi: 10.1007/BF01991682. DOI: 10.1023/A:1022801713046. [DOI] [PubMed] [Google Scholar]
- 20.Penson DF, Stoddard ML, Pasta DJ, Lubeck DP, Flanders SC, Litwin MS. The association between socioeconomic status, health insurance coverage, and quality of life in men with prostate cancer. J Clin Epidemiol. 2001;54:350–358. doi: 10.1016/s0895-4356(00)00312-7. DOI: 10.1016/S0895-4356(00)00312-7. [DOI] [PubMed] [Google Scholar]
- 21.Wan GJ, Counte MA, Cella DF, Hernandez L, McGuire DB, Deasay S, et al. The impact of socio-cultural and clinical factors on health-related quality of life reports among Hispanic and African-American cancer patients. J Outcome Meas. 1999;3:200–215. [PubMed] [Google Scholar]
- 22.Lazarus RS, Folkman S. Stress, appraisal, and coping. Springer; New York: 1984. [Google Scholar]
- 23.Wilkinson RG. Socioeconomic determinants of health: Health inequalities: Relative or absolute material standards? Br Med J. 1997;314:591–595. doi: 10.1136/bmj.314.7080.591. DOI: 10.1136/bmj.314.7080.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wilkinson RG, Pickett KE. Income inequality and population health: A review and explanation of the evidence. Soc Sci Med. 2006;62:1768–1784. doi: 10.1016/j.socscimed.2005.08.036. DOI: 10.1016/j.socscimed.2005.08.036. [DOI] [PubMed] [Google Scholar]
- 25.Festinger L. A theory of social comparison processes. Hum Relat. 1954;7:117–140. DOI: doi: 10.1177/001872675400700202. [Google Scholar]
- 26.Bartram SM, Bodnar GM. No place to hide: The global crisis in equity markets in 2008/2009. J Int Money Finan. 2009;28:1246–1292. DOI: 10.1016/j.jimonfin.2009.08.005. [Google Scholar]
- 27.Ivashina V, Scharfstein D. Bank lending during the financial crisis of 2008. J Financ Econ. 2010;97:319–338. DOI: 10.1016/j.jfineco.2009.12.001. [Google Scholar]
- 28.Horowitz MJ, Wilner N, Alvarez W. Impact of Event Scale: A measure of subjective stress. Psychosom Med. 1979;41:209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- 29.Derogatis LR, Melisaratos N. The Brief Symptom Inventory: An introductory report. Psychol Med. 1983;13:595–605. DOI: 10.1017/S0033291700048017. [PubMed] [Google Scholar]
- 30.Cella DF. Functional Assessment of Chronic Illness Therapy (FACIT) Measurement System Manual Version 4. Evanston Northwestern Healthcare and Northwestern University, Center on Outcomes, Research, and Education (CORE); Evanston, IL: 1997. [Google Scholar]
- 31.McQuellon RP, Russell GB, Cella DF, Craven BL, Brady M, Bonomi A, et al. Quality of life measurement in bone marrow transplantation: Development of the functional assessment of cancer therapy-bone marrow transplant (FACT-BMT) scale. Bone Marrow Transplant. 1997;19:357–368. doi: 10.1038/sj.bmt.1700672. DOI: 10.1038/sj.bmt.1700672. [DOI] [PubMed] [Google Scholar]
- 32.Scheier MF, Wrosch C, Baum A, Cohen S, Martire LM, Matthews KA, et al. The Life Engagement Test: Assessing purpose in life. J Behav Med. 2006;29:291–298. doi: 10.1007/s10865-005-9044-1. DOI: 10.1007/s10865-005-9044-1. [DOI] [PubMed] [Google Scholar]
- 33.Vinokur AD, Caplan RD. Attitudes and social support: Determinants of job-seeking behavior and well-being among the unemployed. J Appl Soc Psychol. 1987;17:1007–1024. DOI: 10.1111/j.1559-1816.1987.tb02345.x. [Google Scholar]
- 34.Vinokur AD, Price RH, Caplan RD. Hard times and hurtful partners: How financial strain affects depression and relationship satisfaction of unemployed persons and their spouses. J Pers Soc Psychol. 1996;71:166–179. doi: 10.1037//0022-3514.71.1.166. DOI: 10.1037//0022-3514.71.1.166. [DOI] [PubMed] [Google Scholar]
- 35.Pearlin LI, Menaghan EG, Morton AL, Mullan JT. The stress process. J Health Soc Behav. 1981;22:337–356. DOI: 10.2307/2136676. [PubMed] [Google Scholar]
- 36.Vinokur AD. [Accessed February 15, 2008];Measures of economic deprivation/pressure: Economic hardship. from: http://sitemaker.umich.edu/avinokur/measures.
- 37.Sarason IG, Johnson JH, Siegel JM. Assessing the impact of life changes: Development of the Life Experiences Survey. J Consult Clin Psychol. 1978;46:932–946. doi: 10.1037//0022-006x.46.5.932. DOI: 10.1037/0022-006X.46.5.932. [DOI] [PubMed] [Google Scholar]
- 38.Sangha O, Stucki G, Liang MH, Fossel AH, Katz JN. The Self-Administered Comorbidity Questionnaire: A new method to assess comorbidity for clinical and health services research. Arthritis Rheum. 2003;49:156–163. doi: 10.1002/art.10993. DOI: 10.1002/art.10993. [DOI] [PubMed] [Google Scholar]
- 39.National Institute on Aging . Growing older in America: The Health & Retirement Study. National Institutes of Health, U.S. Department of Health and Human Services; Bethesda: 2007. [Google Scholar]
- 40.Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Sage; Thousand Oaks, CA: 1991. [Google Scholar]
- 41.McQuellon RP, Russell GB, Rambo TD, Craven BL, Radford J, Perry JJ, et al. Quality of life and psychological distress of bone marrow transplant recipients: The `time trajectory' to recovery over the first year. Bone Marrow Transplant. 1998;21:477–486. doi: 10.1038/sj.bmt.1701115. DOI: 10.1038/sj.bmt.1701115. [DOI] [PubMed] [Google Scholar]
- 42.FACIT.org [Accessed October 18, 2011];FACT-BMT Scoring and Interpretation Materials. from: http://www.facit.org/FACITOrg/Questionnaires.
- 43.Conger RD, Rueter MA, Elder GH. Couple resilience to economic pressure. J Pers Soc Psychol. 1999;76:54–71. doi: 10.1037//0022-3514.76.1.54. DOI: 10.1037//0022-3514.76.1.54. [DOI] [PubMed] [Google Scholar]
- 44.Armenian SH, Sun CL, Teh JB, Arora M, Baker KS, Francisco L, et al. Ethnic differences in chronic health conditions after hematopoietic cell transplantation: A report from the Bone Marrow Transplant Survivor Study. Cancer. 2010;116:4152–4159. doi: 10.1002/cncr.25157. DOI: 10.1002/cncr.25157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.DeNavas-Walt C, Proctor BD, Smith JC. Income, Poverty, and Health Insurance Coverage in the United States: 2009. US Census Bureau, Current Population Reports, P60-238, U.S. Government Printing Office; Washington, DC: 2010. [Google Scholar]
- 46.Centers for Disease Control and Prevention Cancer survivors -- United States, 2007. MMWR. 2011;60:269–272. [Google Scholar]
- 47.Weaver KE, Rowland JH, Bellizzi KM, Aziz NM. Forgoing medical care because of cost. Cancer. 2010;116:3493–3504. doi: 10.1002/cncr.25209. DOI: 10.1002/cncr.25209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Detmar SB, Aaronson NK, Wever LDV, Muller M, Schornagel JH. How are you feeling? Who wants to know? Patients' and oncologists' preferences for discussing health-related quality-of-life issues. J Clin Oncol. 2000;18:3295–3301. doi: 10.1200/JCO.2000.18.18.3295. [DOI] [PubMed] [Google Scholar]
- 49.Jacobsen PB, Shibata D, Siegel EM, Lee J-H, Fulp WJ, Alemany C, et al. Evaluating the quality of psychosocial care in outpatient medical oncology settings using performance indicators. Psycho-Oncol. 2010 doi: 10.1002/pon.1849. DOI: 10.1002/pon.1849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Landro L. Another cancer battle: Costs. The Wall Street Journal. 2010 [Google Scholar]