Abstract
Program approaches for addressing acute malnutrition and those for addressing chronic malnutrition have grown in different directions. Their specialization has led to productive advances in the efficacy of specific interventions but has also created divergences in implementation. Greater convergence and integration between the 2 sets of approaches would help programs respond to the diversity of conditions faced in the field and enable a more comprehensive continuum of care from prevention to treatment. After reviewing the causes of the differences in approach, this paper examines programmatic and scientific challenges to greater convergence and suggests steps to promote effective integration of acute and chronic malnutrition services. Steps include strengthening community linkages between program platforms, assessing the degree and type of integration needed in various situations, identifying cost efficiencies, and developing joint tools where possible.
Introduction
The different manifestations of malnutrition (chronic vs. acute) have led to academic and programmatic specialization. Good program models exist to address each of these conditions, but few programs are designed to cover both chronic and acute malnutrition. Yet the nutrition situation in the field is characterized by considerable overlap of chronic and acute malnutrition within regions, communities, and households. To comprehensively address malnutrition, programs thus need to blend available knowledge and combine multiple approaches. An important area for nutrition delivery science is how to design and implement programs that bridge this diversity.
The first purpose of this paper is to substantiate the claim that acute and chronic malnutrition often coexist in the same locations.6 A second purpose is to describe the tools, approaches, and actors engaged in the different responses, stressing the sources of differences and challenges to convergence. A 3rd purpose is to suggest where potential for linkages exists and identify areas where research on the delivery of nutrition actions can extend field programs’ ability to offer more integrated services.
Coexistence of acute and chronic malnutrition
Wasting and stunting generally coexist within populations. This has been known for some time (1, 2, 3). A quick data extraction using MEASURE DHS’s StatCompiler and classifying countries by their prevalence of each condition expressed in tercile (low, medium, and high) confirms this (Table 1). The different nutrition situations described by the various cells in Table 1 each require a specialized response based on the types and prevalence of malnutrition found in each country. The type and severity of malnutrition also vary within countries, and the responses at subnational levels depend on the specific nutrition situation and other factors such as health system capacity, food availability, enabling environment, and resource availability.
Table 1.
| Stunting <−2HAZ (tercile) | Wasting (<−2 WHZ) (tercile) |
||
| Low | Mid | High | |
| Low | Armenia, Bolivia, Colombia, Dominican Rep, El Salvador, Jordan, Moldova, Swaziland | Azerbaijan, Ghana | Maldives |
| Mid | Honduras | Congo (Brazza), Egypt, Kenya, Namibia, Sierra Leone, Uganda, Zimbabwe | Bangladesh, Guinea, Haiti, Mali |
| High | Guatemala, Zambia | Benin, Cambodia | DRC, Ethiopia, India, Nepal, Nicaragua, Niger, Nigeria |
HAZ, H/A Z-score; WHZ, W/H Z-score.
This table was created with MEASURE DHS StatCompiler, available at http://www.measuredhs.com/data/STATcompiler.cfm. All countries with the data available to classify the country were used. This resulted in the inclusion of the following surveys: Bangladesh 2007, Benin 2006, Bolivia 2008, Burkina Faso 2003, Burundi 1987, Cambodia 2005, Cameroon 2004, Chad 2004, Congo 2005, Cote d‘Ivoire 1998–1999, DRC 2007, Ecuador 2004, Eritrea 2002, Ethiopia 2005, Gabon 2000, Ghana 2008, Guatemala 2008, Guinea 2005, Haiti 2005–2006, Honduras 2005–2006, India 2005–2006, Kenya 2008–2009, Lesotho 2004, Malawi 2004, Mali 2006, Mauritania 2000–2001, Morocco 2003–2004, Mozambique 2003, Namibia 2006–2007, Nepal 2006, Nigeria 2008, Peru 2000, Sierra Leone 2008, Swaziland 2006–2007, Tanzania 2004–2005, Uganda 2006, Yemen 1997, Zambia 2007, Zimbabwe 2005–2006.
Sources and types of divergence between program approaches
To understand the reasons for current divergences between program approaches, we examine the causes and consequences of each condition and consider how the distinct manifestations of malnutrition have led to program approaches that differ in their primary aims, the actors involved, the detection of the problem and targeting of interventions, the products and treatments used as responses, and the intervention models associated with each condition.
Causes and consequences of acute and chronic malnutrition
The causes of each condition help to explain the current specialization; acute malnutrition often results from an immediate problem, a crisis induced by illness (4–6) or deprivation due to seasonal shortages, sudden catastrophes, or other such reasons. Chronic malnutrition by contrast is more closely associated with latent poverty, chronic food insecurity, poor feeding practices, and protracted health problems (7).
The consequences of each condition are also quite different. Acute malnutrition is accompanied by a high risk of mortality; 14.6% of all child deaths are attributed to acute malnutrition (8) and unless provided with appropriate treatment, the fatality rate among children who are severely malnourished is 8 times that of normal children (9, 10).
Chronic malnutrition is also a key underlying factor of child mortality but is less likely to be the direct cause of death. However, chronic malnutrition in early childhood has long-lasting consequences on a wide array of other outcomes such as educability, future work capacity, income-earning ability, and susceptibility to chronic diseases, all of which have profound effects on individual and social development (11).
The differing causes and consequences of acute compared to chronic malnutrition have in turn led to specialized practice in terms of the actors involved; the screening methods applied; the foods, supplements, and other services provided; and the program models implemented.
Key actors and approaches.
The primary aim of programs dealing with acute malnutrition is to avert child mortality, an aim that requires swift action to treat an immediate condition. This link between acute malnutrition and mortality has placed the design of solutions largely within the medical profession and implementation within humanitarian organizations (and more recently within development organizations and government health systems) staffed by medically trained personnel. Acute malnutrition is seen much like a disease and emphasis has been placed on developing effective treatment products and protocols, which have been formalized in internationally defined guidance (12, 13). This proximity with the medical profession has facilitated the establishment of acute malnutrition services within MOH7 at various levels from policy making, to national guidelines, to pre-/in-service training, to delivery of services at clinical and community sites, to referral systems that link health centers and community health posts to hospitals.
By contrast, programs concerned with chronic malnutrition primarily focus on changing long-standing determinants of the condition to prevent the problem from happening in the first place. Programs aimed at addressing chronic malnutrition generally include multi-sectoral actions aimed at promoting the adoption of practices to improve the quality of local diets, improving child feeding practices, and reducing exposure to illnesses (14, 15).
The more protracted nature of chronic malnutrition has led to 2 primary program approaches that complement each other: vertical programs (e.g., food fortification programs, or micronutrient supplementation programs, at times carried out in the context of national immunization days), and horizontal programs (often community-based programs attempting to address the complex set of factors that cause stunting). MOH are the dominant players for vertical programs; NGO often play leading roles in horizontal programs, with active linkages to ministries at the regional or local levels, e.g. through support to CHW in integrated management of childhood illnesses programs, community mobilization for participants in national immunization days, or SBCC to create demand for services.
A primary difference in approach between acute and chronic malnutrition is that there is little evidence of effective approaches to treat or reverse chronic malnutrition once children are stunted, so in contrast to the swift medicalized treatment used to treat acute cases, the reduction of chronic malnutrition needs to focus mainly on prevention. This contrast in emphasis between treatment (for acute malnutrition programs) and prevention (for chronic malnutrition programs) is a key distinction, from which many other differences stem.
Screening and admission indicators.
W/H has long been the indicator of choice for the detection of acute malnutrition, but collection of data for this indicator in developing country settings has posed practical challenges due to the equipment and skills required for measurement. Increasingly, programs are using MUAC to screen and assess children for acute malnutrition. In addition to being much easier to collect and interpret and therefore ideally suited for CHW, there is evidence that MUAC is also a better predictor of mortality than W/H (16). These factors explain why MUAC is fast becoming the indicator of choice for CMAM beneficiary screening and admission.
The key indicator for chronic malnutrition is H/A. Again, both components of the indicator (height and age) are difficult to measure reliably and, in practice, W/A is used in many community-based programs to assess growth and detect problems at the individual level. Although the correlation between W/A and H/A is usually high, they measure different outcomes, and whether or not W/A is a good screening method for stunting has not, to our knowledge, been tested. In addition, weight and age are also prone to significant measurement errors under field conditions. Therefore, in contrast to the use of MUAC for acute malnutrition, chronic malnutrition lacks a viable, field-friendly alternative, which means that assessing stunting in the field remains prone to error and misclassification.
Specialized food products.
Traditionally, the products used in the treatment of acute malnutrition were confined to therapeutic milks such as F75 and F100, administered through in-patient services such as TFC (12). The advent of RUTF in the 2000s expanded the range of treatment options considerably. RUTF contain very little water and require no cooking. They are less susceptible to bacterial contamination and have an extended shelf life under ambient conditions, which allows them to be safely stored at home (13). These features have in turn allowed for the development of out-patient care services for children who present with SAM but no medical complications. Combining RUTF with antibiotic prophylaxis and antihelminth treatment, a new kind of program emerged that dramatically expanded coverage by decentralizing some services to the community level, enabling many children to be treated at home, and increasing recuperation rates among children with SAM (17–19). By all accounts, the RUTF revolution has been a great public health success.
Efforts to address chronic malnutrition promoted the development of a different class of products meant to complement local diets and prevent malnutrition by providing nutrients that would otherwise be lacking in children’s diets. FBF such as CSB and wheat-soy blends (21) and point-of-use fortificants such as micronutrient powders (e.g., Sprinkles) (22, 23) were shown to be effective in addressing some micronutrient deficiencies (e.g., iron) and in preventing chronic malnutrition (24) when combined with strong SBCC and preventive health services (25, 26). The success of RUTF in the fight against acute malnutrition also led to the development of different formulations of specialized lipid-based products meant to supplement usual diets, including products designed to prevent chronic malnutrition in infants and young children. These products, together with RUTF, are known by the generic name of LNS (27). More recent developments have included CSB++, a product developed by the World Food Programme that is more nutrient dense, includes milk powder, has fewer antinutrients, and has stricter microbiological standards than CSB. Aimed at overcoming the problems noted with FBF (i.e., too many antinutrients, especially phytates, which impede the absorption of iron and zinc; suboptimal micronutrient content; high bulk and viscosity) (21), the World Food Programme developed CSB++ especially for the prevention of chronic malnutrition among infants and young children and for the treatment of MAM among children (28).
Intervention models.
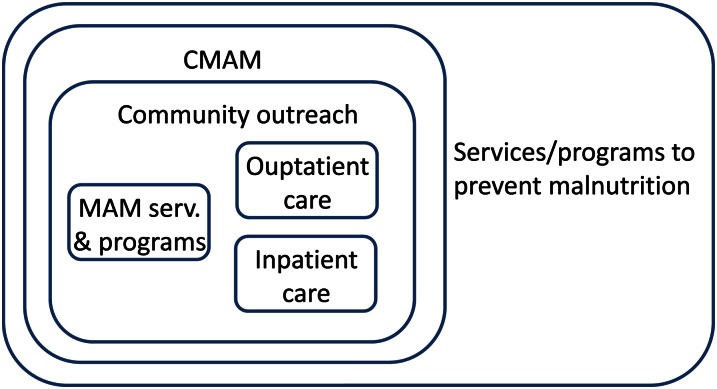
As mentioned earlier, the advent of RUTF allowed for the emergence of new intervention models that took advantage of decentralization of management of acute malnutrition to vastly expand program outreach and coverage. The initial model was community therapeutic care, which focused on emergency settings (29), and subsequently evolved into CMAM, which incorporates the treatment of acute malnutrition in development settings and in routine health services. CMAM is now accepted as a global standard (13, 30). The main components of CMAM include (Fig. 1): 1) outpatient care for children 6–59 mo with SAM but without medical complications; 2) inpatient care for children 6–59 mo with SAM and medical complications and for children < 6 mo with acute malnutrition; 3) the management of MAM among children 6–59 mo; and 4) community outreach, screening, and active case-finding for early detection and referral of SAM/MAM cases.
Figure 1.
CMAM model. Adapted with permission from FANTA-2 project (25). CMAM, community-based management of acute malnutrition.
The effectiveness of CMAM relies on an enabling policy environment; adequately trained personnel; an effective supply chain management system for RUTF and associated medications; adequate infrastructure for screening, inpatient care, and outpatient care; effective community outreach and active case finding; follow-up and referral systems; and active community participation. Increasingly, MOH in several countries are managing and implementing CMAM services, often with technical and financial inputs from specialized international organizations (e.g., multilaterals such as UNICEF and NGO such as Valid International) that play key roles in building staff competencies and logistics capacities.
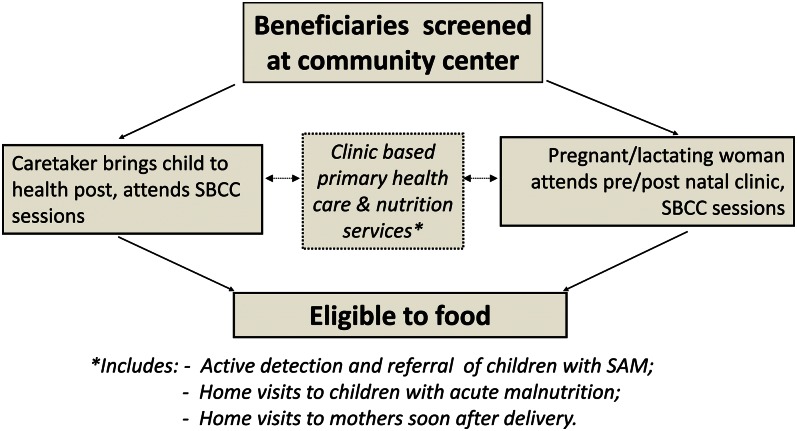
By contrast, the control of chronic malnutrition in children focuses on maternal nutrition during pregnancy and lactation and on protecting the health and nutrition of the young child and mother during the first 2 y of life, the 1000-d window of opportunity for preventing malnutrition (31). Community-based approaches such as AIN-C (32) and PM2A (30) have been developed using the well-established UNICEF model (33) for child nutrition with key action points covering health, diet, and care. Figure 2 illustrates the process by which beneficiaries are screened and supported throughout the 1000-d period in a food-assisted program such as PM2A (15) to prevent chronic malnutrition.
Figure 2.
Example of a food-assisted intervention to address chronic malnutrition. Adapted with permission from FANTA-2 project (15).
This model emphasizes addressing the underlying determinants of nutrition, including income, education, food security, women’s empowerment, and availability/access to water, sanitation, and health services. The compound nature of chronic malnutrition calls for embedding prevention into more comprehensive multi-sectoral approaches to reduce poverty and food insecurity by designing gender-sensitive social protection programs, engaging with the agricultural sector to improve the availability of nutrient-rich foods, using SBCC and counseling to improve child feeding practices, and strengthening health services and the promotion of water and sanitation interventions to reduce exposure to illnesses.
Table 2 summarizes the sources of divergence between acute malnutrition and chronic malnutrition programs that were listed in the sections above.
Table 2.
Programmatic divergences between acute and chronic malnutrition1
| Programs |
|||||
| Type of malnutrition (causes; consequences) | Response approach | Actors | Products | Delivery models | Admission indicators |
| Acute (caused by crises; associated with high risk of mortality) | Medicalized treatment | MOH, humanitarian organizations, medical staff | RUTF, therapeutic milks | CMAM, CTC, TFC | W/H, MUAC |
| Chronic (caused by multi-faceted factors; leads to long-term physical and cognitive impairment, reduced economic performance, and increased risk of chronic diseases) | Preventive, multi-sectoral programs | NGO, MOH, CHW, | Complementary foods, FBF, LNS, and other home fortificants, | Community-based programs, social protection | H/A, W/A |
CHW, community health worker; CMAM, community-based management of acute malnutrition; CTC, community therapeutic care; FBF, fortified blended food; H/A, height for age; LNS, lipid-based nutrient supplement; MOH, ministries of health; MUAC, mid-upper arm circumference; NGO, nongovernmental organization; RUTF, ready-to-use therapeutic food; TFC, therapeutic feeding center; W/A, weight for age; W/H, weight for height.
Considerations and challenges for integration
We now turn to the challenges programs face in improving implementation and integration, and identify programmatic and scientific issues influencing integration capacity.
Programmatic issues: constraints and opportunities
Challenges to integration due to differing mandates.
Although the medical model used by programs addressing SAM is remarkably effective in saving lives, it does not focus on preventing SAM from occurring in the first place and has limited ability to prevent children from relapsing after they exit the program (34, 35). This is not surprising, because these programs are generally not mandated to control the causes of SAM and understandably so, because causes include social, economic, or political factors as well as natural or weather-related disasters.8 By contrast and as mentioned earlier, addressing the socio-economic factors underlying malnutrition is an area of focus for prevention programs, and treating existing malnutrition is not. In theory, CMAM and prevention programs could collaborate to complement treatment services with socio-economic and other prevention interventions. However, several factors hinder such collaboration. First, there are often different organizations implementing the 2 sets of programs. Strategic and technical divides between organizations, combined with the often pressing need to focus on achieving the specific mandated results, seem to discourage the exchange of information. Evidence from observing the 2 types of programs working in the same geographic areas without communicating suggests that such collaboration across organizations and programs is not a natural inclination (personal communication, Mary Ann Anderson, FANTA-2 Project). Competition for a limited pool of resources for nutrition programs may also inhibit collaboration and information sharing. Second, the ability of preventive programs to address acute malnutrition may be weakened from the start by guidance and mandates from funding sources. For instance, whereas multi-sectoral development interventions like USAID’s food-assisted PM2A programs incorporate identification of SAM cases, their response to acute malnutrition is restricted to the screening and referral of cases to the appropriate clinical facilities, which may be distant or nonexistent in some PM2A program areas. Thus, although on the one hand donor policies that confine resources to a particular type of intervention may enhance efficiency of these interventions, on the other hand they can hamper potential convergence of expertise and interventions, limiting the services provided to beneficiaries.
Matching the extent of integration to the situation.
It is important to recognize that the integration of services may take many forms and that different forms are appropriate in different contexts, including situations where it may be desirable not to integrate at all. The various types of integration can be organized in a spectrum from simple awareness of other programs and light coordination around coverage and policies to establishing formal linkages and referral systems between programs, to delivering multiple services at the same points, to actually integrating the services so they are provided together as a package at the same service delivery point. In the context of chronic and acute malnutrition, different types of integration may be feasible and needed in different settings, depending on the relative prevalence of the 2 conditions, the implementing partners at play, their geographic overlap, and the established implementation models and programming platforms.
Adjusting investments to the size and nature of the problem.
Striking the right balance between the incidence of SAM and the capacity to respond is an important consideration. Some countries rarely experience significant bouts of acute malnutrition, but when they occur, the consequences can be far reaching if they are unprepared, as demonstrated by the crisis in the Corredor Seco in Guatemala in 2008. In other locations such as Niger or Sudan, the fight against SAM requires constant attention, so well-established systems are required to respond on an ongoing basis. As a general rule, investments in CMAM programs should be proportional to the size of the acute malnutrition problem. Several “ratcheted” modalities can be envisioned. At a minimum, all countries need: 1) the ability to monitor and detect problems as they surface; 2) national and local medical staff adequately trained in treatment protocols for SAM; 3) sufficient support for TFC and outpatient care when the need emerges; and 4) the ability to store and distribute key products like F75, F100, RUTF, antihelminths, and antibiotics when needed. At a higher level of need, many countries require CMAM structures to be in place permanently.
Integration through community platforms.
The community focus of both programs offers opportunities for synergy and integration, especially to the extent that CHW and other community-based service providers have the opportunity to engage in screening, SBCC, and referral services for both acute and chronic malnutrition. However, in practical terms, such integration is constrained by the limited time, capacity, incentives, and in some cases reach of community-based service providers. Overburdening CHW can be counterproductive. Considerable scope exists to strengthen both programs’ explicit emphasis on high-quality, community-based actions. For example, although CMAM programs’ out-/in-patient care systems operate effectively in many settings, community outreach and active case-finding can be enhanced and expanded (35). Despite recognition of the importance of community mobilization, this component is often not adequately supported by budgets and policies, perhaps because the urgency of cultivating community leadership in responding to acute malnutrition problems is less than the urgency of saving lives through treatment.
Breadth of interventions.
Programs to prevent chronic malnutrition are helped in their efforts at building community capacity and support structures by the fact that they are usually long term and multi-sectoral, and that they bring an array of assets and activities that can extend beyond nutrition into food security, health care, agriculture, water and sanitation, income generation, and women’s empowerment. However, the multi-sectoral nature of these programs also means that they cast a wider net of interventions and as a result the contours, protocols, and standards used by preventive programs are less precise and well defined than acute malnutrition programs. This can make it more difficult to monitor and ensure quality implementation and can pose challenges for the integration of the 2, quite heterogeneous types of programs.
Capacity building and sustainability.
Local capacity building and sustainability of services remain critical areas for both types of programs. Most countries affected by serious malnutrition problems rely on external entities for funding, staff expertise, logistics systems, procurement of medical supplies, etc. International organizations can be stretched thin on the ground when responding to nutrition emergencies, such as the recent crises in the Sahel (36).
Policy and standards.
Lastly, policy issues may at times need clarification to support effective programming. One case in point: concerns have been raised that promoting the use of LNS to prevent chronic malnutrition may displace breastfeeding, and interpretations of the Marketing Code for Breastfeeding Substitutes have led some to resist the marketing and commercialization of LNS for children < 24 mo (37). Controversies such as this are deep seated and need to be resolved in such a way that ensures that all products promoted are safe and that any marketing is responsible while not paralyzing needed action in the long run.
Scientific issues
In addition to program implementation issues, there remain many scientific gaps in the evidence base that informs optimal program interventions. We do not attempt to identify all such gaps here but emphasize a few that seem to be priorities from a practitioner’s perspective.
Treatment of SAM in children #x003C 6 mo.
One dimension requiring greater evidence is the management of acute undernutrition among children <6 mo of age. As mentioned already in this issue (1, 2), the 0- to 6-mo age group is the one most likely to suffer from acute malnutrition, a fact that gives particular urgency to the problem given the vulnerability of this age group. But the scientific evidence on appropriate treatment of acutely malnourished children who are in the age group for exclusive breastfeeding is still not conclusive, so guidance to field programs remains imprecise (38).
Treatment of MAM.
Another dimension of management of acute malnutrition that would benefit from greater evidence is the nutrient needs of children with MAM. Unlike SAM, the evidence base for nutrient needs to address MAM is more limited, as is corresponding international guidance on protocols for management of MAM (39).
Treatment of chronic malnutrition.
The treatment of chronic malnutrition, i.e., stunting, is another area with a considerable gap in knowledge. Although prevention will probably remain front and center in the fight against chronic malnutrition, more needs to be known about how to support children who are already stunted. For instance, whereas it is still largely thought that past 24 mo of age, stunted children cannot achieve catch-up growth, evidence is emerging that some (not all) of the impairments brought about by chronic malnutrition may be redressed at later ages (see Piwoz, this issue). Understanding what can be done at later stages in the life cycle, e.g., during preschool and school years, can lead to better intervention design, possibly restoring some of the functional abilities that would otherwise affect individuals for the rest of their lives.
Streamlined CMAM.
The outpatient care component of CMAM has enabled decentralization of many acute malnutrition services. Evidence about the necessity of specific aspects of the outpatient protocol, such as antibiotic prophylaxis or safe monitoring or discharge using MUAC, would inform possible further simplification of the protocol for clients without medical complications. If the evidence supports it, such simplification could expand the reach and coverage of CMAM services as well as improve cost efficiency.
Specialized food products.
More scientific evidence is needed regarding the specialized food products used to prevent chronic malnutrition. Although recently developed specialized food products have demonstrated promising results (24, 38), the extent to which products such as micronutrient powders, LNS, or CSB++ can prevent chronic malnutrition remains to be fully demonstrated. More work in delivery science is also required in this area; although international standards exist for the use of specialized food products for some purposes, additional job aids, local adaptations, and staff training to guide implementers’ use of products would help improve the quality of implementation.
Indicators.
Further research is also needed with regards to indicators. It should be a common practice for all nutrition and child health programs to screen children for both acute and chronic malnutrition. The fact that there is no simple-to-use indicator for the detection of chronic malnutrition (like MUAC for acute malnutrition) has hampered the capacity to rapidly and effectively screen children for this condition. Until such an indicator is identified, it may be advisable to use proxies, such as the crucial triggers for stunting (e.g., repeated illness, no breastfeeding, alternate caregivers, etc.), when screening children to signal when more elaborate measurements may be warranted and to take steps that may be needed to avoid further deterioration in growth patterns.
Steps and conditions toward convergence
Although considerable progress has been achieved, critical gaps continue to hamper the programmatic ability to address undernutrition in developing countries. This paper has argued that divergences between programs focused on acute malnutrition and those focused on chronic malnutrition constitute important impediments to the effective delivery of comprehensive services. In this final section, we highlight actions that can help foster programmatic integration and convergence of approaches.
A key strategic condition for convergence is to enhance, consolidate, and link the community-based components of the 2 types of programs. Although both CMAM and preventive programs have facility-based components, both acknowledge the critical role of community-based platforms and recognize the preeminence of the community as a central locus of mobilization and action (32). This common platform offers opportunities for greater integration to support CHW and other community-based delivery mechanisms to address the continuum of nutrition care. Promising recent experience in Bangladesh suggests that CMAM services can be incorporated into community case management services delivered by CHW (41). The challenge is often to introduce such services without overburdening the time or capacity of CHW and community systems that are often already stretched. Because both CMAM and preventive programs take steps to boost their community-based approaches, consideration can be given to work jointly to exploit synergies and seek opportunities for integration.
As such opportunities for integration are considered, it must be recognized that service integration is not a dichotomous condition; various degrees of integration are possible as described above. Nor is integration always an unqualified good, because situations exist in which it may be preferable to keep services separate and unintegrated. In different contexts, different degrees of integration are called for and factors such as the prevalence and geographic overlap of each type of malnutrition, cost, capacity of health system and providers, service delivery mechanisms, enabling environment, and the mandate for available resources all need to be considered in determining what degree and type of integration is appropriate. Regardless of the degree of integration, at a minimum, communication and basic coordination between acute and chronic malnutrition programs operating in the same geographic area are beneficial. Such coordination may focus on issues such as the content of CHW services and community mobilization efforts, logistics and commodity supply, coverage, training schedules, MOH roles, and managing external factors that affect operation.
One factor to consider in determining optimal levels of integration is cost effectiveness. In an era of constrained donor resources, cost considerations are increasingly relevant when deciding whether and how to integrate services. Costing tools have been developed for CMAM to assess the budgetary implications of such programs and support planning (42). Similar tools should be developed for preventive programs and possibly for integrated approaches spanning treatment and prevention. The World Bank has produced initial materials to support costing of nutrition programming (43), which can be adapted and extended for specific contexts and programmatic needs.
Another step toward integration is to develop common tools such as guidelines, job aids, and standardized protocols that cover both acute and chronic malnutrition. Although such a process may to some extent dilute the focus on specific interventions, the benefits from more comprehensive services and consistent messages across programs are likely to outweigh such concerns. On a related note, there is also the need for operations research about how to most effectively transition between curative and preventive modes at both the individual and program levels. Advances on these fronts will help improve coverage and enable nutrition programs to more comprehensively address the range of undernutrition conditions that are present in the households and communities with which they work.
Acknowledgments
The authors thank Jean Pierre Habicht and Marie Ruel for their comments. All authors read and approved the final manuscript.
Footnotes
Published as a supplement to Advances in Nutrition. Presented at a symposium titled “Building Convergence among Scientific, Programmatic, and Policy Communities: Working on Childhood Undernutrition in Developing Countries” given at the annual Experimental Biology meeting, Monday, April 11, 2011, in Washington, DC. The symposium was partly supported by the American Society for Nutrition. The symposium was chaired by Purnima Menon and Rebecca Stoltzfus. Guest Editors for this symposium publication were Rebecca J. Stolzfus and Edward A. Frongillo. Guest Editor disclosures: Rebecca J. Stolzfus had no conflicts to disclose. Edward A. Frongillo had no conflicts to disclose.
Supported by the United States Agency for International Development through the Food and Nutrition Technical Assistance-II Project.
Author disclosures: G. Bergeron and T. Castleman, no conflicts of interest.
We follow common standards in defining malnutrition: acute malnutrition in children 6–59 mo old refers to W/H < −2 Z-scores or MUAC < 125 mm or bilateral pitting edema. MAM refers to W/H −2 and −3 Z-scores. SAM refers to W/H < −3 Z-scores or MUAC < 115 mm or bilateral pitting edema. Chronic malnutrition in children 6–59 mo old refers to H/A < −2 Z-scores.
Related to this, many programs treating SAM do not address the less severe but much more common problem of MAM.
Abbreviations used: CHW, community health worker; CMAM, community-based management of acute malnutrition; CSB, corn-soy blend; FBF, fortified blended food; H/A, height for age; LNS, lipid-based nutrient supplement; MAM, moderate acute malnutrition; MOH, ministries of health; MUAC, mid-upper arm circumference; NGO, nongovernmental organization; PM2A, preventing malnutrition in children under 2 approach; RUTF, ready-to-use therapeutic food; SAM, severe acute malnutrition; SBCC, social and behavior change and communication; TFC, therapeutic feeding center; W/A, weight for age; W/H, weight for height.
Literature Cited
- 1.Menon P, Stoltzfus RJ. Building convergence in science, programs, and policy actions on child undernutrition: symposium rationale and overview. Adv Nutr. 2012;3:224–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Richard SA, Black RE, Checkley W. Revisiting the relationship of weight and height in early childhood Adv Nutr. 2011;3:250–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Piwoz E, Sundberg S, Rooke J. Promoting healthy growth: what are the priorities for research and action? Adv Nutr. 2011;3:234–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yip R, Sharp TW. Acute malnutrition and high childhood mortality related to diarrhea. JAMA. 1993;270:587–90 [PubMed] [Google Scholar]
- 5.Rowland MGM, Cole TJ, Whitehead RG. A quantitative study into the role of infection in determining nutritional status in Gambian village children. Br J Nutr. 1977;37:441–50 [DOI] [PubMed] [Google Scholar]
- 6.Reddy VP. Bhaskaram, N Raghuramulu, RC Milton, V Rao, J Madhusudan, KV Krishna. Relationship between measles, malnutrition, and blindness: a prospective study in Indian children. Am J Clin Nutr. 1986;44:924–30 [DOI] [PubMed] [Google Scholar]
- 7.Müller O, Krawinkel M. Malnutrition and health in developing countries. CMAJ. 2005;173:279–86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Black RE, Allen LH, Bhutta ZA, Caulfield LE, de Onis M, Ezzati M, Mathers C, Rivera J, Maternal and Child Undernutrition Study Group Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. 2008;371:243–60 [DOI] [PubMed] [Google Scholar]
- 9.Pelletier DL, Frongillo EA, Jr, Schroeder DG, Habicht JP. A methodology for estimating the contribution of malnutrition to child mortality in developing countries. J Nutr. 1994;124 Suppl:S2106–22 [DOI] [PubMed] [Google Scholar]
- 10.Blossner M, de Onis M. Malnutrition: quantifying the health impact at national and local levels. Environmental burden of disease series. Geneva: WHO; 2005.
- 11.Hoddinott J, Maluccio JA, Behrman J, Flores R, Martorell R. Effect of a nutrition intervention during early childhood on economic productivity in Guatemalan adults. Lancet. 2008;371:411–6 [DOI] [PubMed] [Google Scholar]
- 12.WHO. Management of severe malnutrition: a manual for physicians and other senior health workers. Geneva: WHO; 1999.
- 13.WHO/WFP/UNICEF. Community-based management of severe acute malnutrition. A Joint Statement by the World Health Organization, the World Food Programme, the United Nations System Standing Committee on Nutrition and the United Nations Children’s Fund. Geneva: WHO; 2007.
- 14.The World Bank. Repositioning nutrition as central to development: a strategy for large-scale action. Washington DC: The World Bank; 2006.
- 15.FANTA-2. Title II technical reference materials. TRM-01: preventing malnutrition in children under 2 approach (PM2A): a food-assisted approach. Revised November 2010. Washington, DC: Food and Nutrition Technical Assistance II Project (FANTA-2), AED; 2010.
- 16.Myatt M, Khara T, Collins S. A review of methods to detect cases of severely malnourished children in the community for their admission into community-based therapeutic care programs. Food Nutr Bull. 2006; 27 Suppl 3:S7–23 [DOI] [PubMed] [Google Scholar]
- 17.Collins S. Changing the way we address severe malnutrition during famine. Lancet. 2001;358:498–501 [DOI] [PubMed] [Google Scholar]
- 18.Perra A. de L Costello AM. Efficacy of outreach nutrition rehabilitation centers in reducing mortality and improving nutritional outcome of severely malnourished children in Guinea Bissau. Eur J Clin Nutr. 1995;49:353–9 [PubMed] [Google Scholar]
- 19.Manary MJ, Ndkeha MJ, Ashorn P, Maleta K, Briend A. Home-based therapy with RUTF for severe malnutrition with ready-to-use food. Arch Dis Child. 2004;89:557–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Briend A. Highly nutrient-dense spreads: a new approach to delivering multiple micronutrients to high-risk groups. Br J Nutr. 2001;85 Suppl 2:S175–9 [PubMed] [Google Scholar]
- 21.Webb P, Rogers B, Rosenberg I, Schlossman N, Wanke C, Bagriansky J, Sadler K, Johnson Q, Tilahun J, Reese Masterson A, et al. Delivering improved nutrition: recommendations for changes to U.S. food aid products and programs. Boston: Tufts University; 2011.
- 22.Zlotkin SH, Schauer C, Christofides A, Sharieff W, Tondeur MC, Hyder SM. Micronutrient sprinkles to control childhood anaemia. PLoS Med. 2005;2:e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nestel P, Briend A, de Benoist B, Decker E, Ferguson E, Fontaine O, Micardi A, Nalubola R. Complementary food supplements to achieve micronutrient adequacy for infants and young children. J Pediatr Gastroenterol Nutr. 2003;36:316–28 [DOI] [PubMed] [Google Scholar]
- 24.Ruel MTP. Menon JP, Habicht C, Loechl G, Bergeron G, Pelto M, Arimond J, Maluccio L, Michaud B. Hankebo Age-based preventive targeting of food assistance and behaviour change and communication for reduction of childhood undernutrition in Haiti: a cluster randomised trial. Lancet. 2008;371:588–95 [DOI] [PubMed] [Google Scholar]
- 25.Lundeen E, Schueth T, Toktobaev N, Zlotkin S, Hyder SM, Ziauddin, Houser R. Daily use of Sprinkles micronutrient powder for 2 months reduces anemia among children 6 to 36 months of age in the Kyrgyz Republic: a cluster-randomized trial. Food Nutr Bull. 2010;31:446–60 [DOI] [PubMed] [Google Scholar]
- 26.Menon P, Ruel MT, Loechl CU, Arimond M, Habicht JP, Pelto G, Michaud L. Micronutrient Sprinkles reduce anemia among 9- to 24-mo-old children when delivered through an integrated health and nutrition program in rural Haiti. J Nutr. 2007;137:1023–30 [DOI] [PubMed] [Google Scholar]
- 27.Adu-Afarwuah S, Lartey A, Brown KH, Zlotkin S, Briend A, Dewey KG. . Randomized comparison of 3 types of micronutrient supplements for home fortification of complementary foods in Ghana: effects on growth and motor development. Am J Clin Nutr. 2007;86:412–20 [DOI] [PubMed] [Google Scholar]
- 28.de Pee S, T van den Briel, J van Hees, MW Bloem. Introducing new and improved food products for better nutrition. In: WFP: revolution: from food aid to food assistance. WFP: ROME; 2010
- 29.Collins S, Sadler K. Outpatient care for severely malnourished children in emergency relief programmes: a retrospective cohort study. Lancet. 2002;360:1824–30 [DOI] [PubMed] [Google Scholar]
- 30.Deconinck H, Swindale A, Grant F, Navarro-Colorado C. Review of community-based management of acute malnutrition (CMAM) in the post-emergency context: synthesis of lessons on integration of CMAM into national health systems. Washington, DC: FANTA Project, Academy for Educational Development; 2008.
- 31.Clinton H.2011. 1,000 days: change a life, change the future [cited 2010 Oct 21]. Available from: http://www.state.gov/secretary/rm/2010/09/147512.htm.
- 32.Marini AL, Bassett, Bortman M, Flores R, Griffith M, Salazar M. Promocion del crecimiento para prevenir la desnutricion cronica: estrategias con base comunitaria en Centro America. Washington, DC: The World Bank; 2009
- 33.UNICEF. Strategy for improved nutrition of children and women in developing countries. New York: UNICEF; 1990.
- 34.Ashraf H, Alam NH, Chisti MJ, Mahmud SR, Hossain MI, Ahmed T, Salam MA, Gyr N. A follow-up experience of 6 months after treatment of children with severe acute malnutrition in Dhaka, Bangladesh. J Trop Pediatr. Epub 2011 Oct 11 [DOI] [PubMed] [Google Scholar]
- 35. Forsythe V, Sharawy R, Sorkatti S, Albalula SA, Hassan E, Deconinck H, De Bernardo D, El Badawi AN. Community outreach for community-based management of acute malnutrition in Sudan. Washington, DC: AED; 2010.
- 36.Loewenberg S. Niger’s hunger crisis: a legacy of lessons unlearned. Lancet. 2010;376:579–81 [DOI] [PubMed] [Google Scholar]
- 37.Latham MU, Jonsson E, Sterken G, Kent. RUTF stuff. Can the children be saved with fortified peanut paste? World Nutr 2011;2, 2:62–85 [Google Scholar]
- 38. Inter-Agency Standing Committee, Action Contre La Faim, UCL Centre for International Health and Development, Emergency Nutrition Network. Management of Acute Malnutrition in Infants (MAMI) project technical review: current evidence, policies, practices and programme outcomes. 2010. ENN: London.
- 39.WHO, UNICEF, WFP, UNCHR. WHO, UNICEF, WFP and UNHCR. Consultation on the dietary management of moderate malnutrition in under-5 children. Food Nutr Bull. 2009;30, No. 3. (Suppl) [DOI] [PubMed] [Google Scholar]
- 40.Phuka JC, Maleta K, Thakwalakwa C, Cheung YB, Briend A, Manary MJ, Ashorn P. Complementary feeding with fortified spread and incidence of severe stunting in 6- to 18-month-old rural Malawians. Arch Pediatr Adolesc Med. 2008;162:619–26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sadler K, Puett C, Mothabbir G, Myatt M. Community case management of severe acute malnutrition in southern Bangladesh. Boston: Tufts University; 2011.
- 42.FANTA-2. User’s guide to the CMAM costing tool: a tool for costing community-based management of acute malnutrition at the national, subnational, and district levels. Washington, DC: FANTA-2, AED; 2011.
- 43.Horton S, Shekar M, McDonald C, Mahal A, Brooks JK. Scaling up nutrition: what will it cost? Washington, DC: The World Bank; 2010.