Abstract
Most deaths in the United States are preventable and related to nutrition. Although physicians are expected to counsel their patients about nutrition-related health conditions, a recent survey reported minimal improvements in nutrition medicine education in US medical schools in the past decade. Starting in 2006, we have developed an educational plan using a novel student-centered model of nutrition medicine education at Boston University School of Medicine that focuses on medical student–mentored extracurricular activities to develop, evaluate, and sustain nutrition medicine education. The medical school uses a team-based approach focusing on case-based learning in the classroom, practice-based learning in the clinical setting, extracurricular activities, and a virtual curriculum to improve medical students’ knowledge, attitudes, and practice skills across their 4-y period of training. We have been using objectives from the NIH National Academy Awards guide and tools from the Association of American Medical Colleges to detect new areas of nutrition medicine taught at the medical school. Although we were only able to identify 20.5 h of teaching in the preclerkship years, we observed that most preclerkship nutrition medicine objectives were covered during the course of the 4-y teaching period, and extracurricular activities provided new opportunities for student leadership and partnership with other health professionals. These observations are very encouraging as new assessment tools are being developed. Future plans include further evaluation and dissemination of lessons learned using this model to improve public health wellness with support from academia, government, industry, and foundations.
Background
For more than a decade, National Surveys have reported that most common deaths in the United States are preventable and related to nutrition (1). This is especially worrisome given the widening disparity in health care among minorities resulting in progressing rates of complications and shortened life expectancy. Healthy People 2010 (2) and the US Preventive Services Task Force (3) have recommended that physicians provide nutritional assessment and counseling to their patients, which should require at least 25 h of nutrition education as part of the standard medical curriculum (4, 5). Although physicians recognize deficiencies in nutrition knowledge and a lack of confidence in providing effective counseling (6), a recent survey from the University of North Carolina reported minimal improvements in U.S. medical schools in the past decade (7). As a result, a summit was organized by the American Society for Parenteral and Enteral Nutrition to address the shortage of physician nutrition specialists and nutrition medicine education in US medical schools (8, 9).
Given the study findings on nutrition medicine education in the past few decades (6, 7), reports from medical students at Boston University School of Medicine on their perception of nutrition medicine education, concerns about their knowledge in nutrition and obesity medicine, as well as concerns regarding their preparedness to counsel patients, it was critical to conduct a curricular assessment and create a Nutrition Vertical Integration Group (VIG)7.
Initiatives in Nutrition Medicine at Boston University
The integration of nutrition in the Boston University School of Medicine (BUSM) curriculum has been guided by former principles (10–12). More specifically, we incorporated Hark’s “Lessons Learned” (11) in the development of our initiatives. These consisted of the following: 1) be creative and think outside box when you are developing a nutrition curriculum, 2) gain support for nutrition at the highest political level possible, 3) establish a nutrition curriculum committee or task force, 4) focus on training more faculty in nutrition, and 5) always evaluate your programs. Hark cautions the reader that without longevity, a nutrition program was not worth designing and implementing (11). We immediately explored ways to support and sustain our efforts.
Grant support from the Physician Nutrition Specialist award (2006) was key in providing more nutrition education credibility at BUSM as the Associate Dean for Academic Affairs appointed a VIG to review nutrition medicine in the school curriculum in 2007 (Table 1). With Dr. Sharon Levine, Associate Dean of Academic Affairs, as their champion, the group activities are led by a physician nutrition specialist (C.L.) and coordinated by a dietitian (K.G.). The group consists of a core of faculty, students, and consultants. Faculty and consultants include physician nutrition specialists, physician educators, dietitians, and mental health specialists, while students include medical students, dietetic interns, and residents with the goals to 1) assess the status of nutrition education in the 4-y curriculum and identify areas for improvement, 2) enhance nutrition-related clinical skills of both faculty and medical students, and 3) identify opportunities in postgraduate training (residency) at Boston University Medical Center.
Table 1.
Nutrition medicine landmarks at BUSM: 2006–20121
| 2006 | Physician Nutrition Specialist Award from the ASN to assess and initiate nutrition medicine activities at BUSM |
| 2007 | The Associate Dean for Academic Affairs appoints a Nutrition VIG, consisting of faculty and medical students |
| 2008 | First student Clinical Nutrition Internship award from ASN and presentation of a new nutrition medicine education approach at ASN |
| 2009 | Creation of a new medical student group of interest in nutrition called SNAAC |
| 2010 | Creation of a paired medical and dietetic student activity, second CNIP award, and best presentation award at the John MacCahan Education Day, BUSM |
| 2011 | Students’ oral and poster presentations at the BNORC, John MacCahan Education Day, New England Summit of Nutrition Medicine Education (Boston), and Experimental Biology meetings (Washington, DC) and SNACC begins partnership with other Boston medical schools to offer city-wide nutrition seminars to medical students |
| 2012 | Presentations by the Nutrition VIG and SNAAC at the Experimental Biology meetings (San Diego) and at the Weight of the Nation (Washington, DC) |
BNORC, Boston Nutrition Obesity Research Center; BUSM, Boston University School of Medicine; SNAAC, Student Nutrition Awareness and Action Council; VIG, Vertical Integration Group.
An advanced nutrition elective with a focus on underserved populations was thus created, and major gaps in nutrition medicine education were identified. Further support from foundations such as the New Balance Foundation, the Red Sox Foundation, the Loomis and Sayles Fund, and more recently the Allen Foundation was key in the development phase of the project. Since its inception, the medical students have played a critical role in this education project.
As medical students were increasingly involved in the Nutrition VIG activities, the Student Nutrition Awareness and Action Council (SNAAC) was created in 2009 by 2 medical students (Medical Student, 2012): Hannah Milch (Founding Chair) and Ashley Decker (Co-Founding Chair). Its mission was to improve medical students’ understanding of nutrition and obesity medicine by providing extracurricular opportunities for SNAAC members (n = 36, year 2011) and to join the medical school in its efforts to vertically integrate nutrition medicine in the curriculum. SNAAC members are paired with dietetic interns, play an active role in regional nutrition- and obesity-related committees, and are involved in activities such as education, specialty rotations, community outreach, and advocacy. SNAAC obtained the best student presentation award at the John McCahan Medical Campus Education Day and became a featured program of BUSM’s Deans Service Learning Initiative and Wellness Initiative in 2010. This group of students is pivotal to the development of educational material and sustainability of the Nutrition VIG’s goals.
In an effort to expose the medical students at BUSM to the practice of medical nutrition therapy and the role of the registered dietitian on a health care team, a program was created to match a Boston University Sargent College dietetic intern with a BUSM medical student (2010). Through a variety of educational and extracurricular projects, the dietetic intern counsels the medical student regarding his or her diet and lifestyle habits and shares information regarding nutritional management of various chronic diseases and the role of the registered dietitian on the health care team. In turn, the medical student shares his or her knowledge in medical assessment and drug treatment of chronic diseases. As a result, this program is mutually beneficial because both the medical student and the dietetic intern start to appreciate each other’s role on the health care team and gain experience in working collaboratively, with the ultimate goal of improving wellness and diseases related to nutrition. This program, along with other multidisciplinary activities at Boston University Medical Center that focus on outpatient care and community wellness, fosters interprofessional development across areas including medicine, nutrition, public health, and mental health.
Quantity or quality of instruction?
In 1985, the National Academy of Sciences (4) recommended at least 25 h of nutrition education in the medical school, whereas the American Society for Nutrition recommended at least 44 h (13). We were able to identify >20 h of education in nutrition medicine during preclerkship courses (6 h in Integrated Problems, 6 h in Endocrinology, 6 h in Disease and Therapy (DRx), 3 h in Gastroenterology, 1.5 h in Pediatric Obesity in Human Behavior in Medicine, ½ h in Introduction to Clinical Medicine I, and ½ h in Introduction to Clinical Medicine II).
Nutrition instruction is also a large part of other preclerkship and clerkship courses such as biochemistry, renal, medicine, and pediatrics, but is more difficult to quantify. The Association of American Medical Colleges Curriculum Management and Information Tool (CurrMIT) is a password-protected online database that offers support services to help medical schools manage and report on curriculum information that is available to faculty, educators, and scientists. As opposed to hours of instruction in nutrition, which are difficult to estimate, CurrMIT may allow medical schools to better identify areas in preclerkship and clerkship courses where nutrition is covered.
Using the NIH National Academy Awards (NAAs) guide to identify appropriate objectives in nutrition, the Nutrition VIG and SNAAC updated the medical school objectives and competencies in nutrition medicine in 2010–2011. The CurrMIT software allowed the Nutrition VIG to identify current courses and their objectives as they related to nutrition medicine while students and faculty provided feedback on nutrition content in courses. As a result, we observed that most of the preclerkship objectives in nutrition medicine were identified as being included in the curriculum.
In addition to basic sciences and clinical disciplines, a total of 32 behavioral and socioeconomic subjects are recognized as important for full accreditation surveys reviewed by the Liaison Committee on Medical Education. This committee is a nationally recognized accrediting authority for medical education programs leading to an MD degree in US and Canadian medical schools and is sponsored by the Association of American Medical Colleges and the American Medical Association. The behavioral and socioeconomic subjects recognized for accreditation by the Liaison Committee on Medical Education include, among others, nutrition, prevention/health maintenance, epidemiology, medical genetics, and substance abuse. Nutrition was in the top 5 behavioral and socioeconomic subjects included in required courses at BUSM (2010–2011). These findings were very encouraging and may be due in part to the availability of new tools used to identify nutrition medicine objectives in preclerkship and clerkship courses.
Based on recommendations from several societies and groups of interest in nutrition, the National Board of Medical Examiners approved a subscore for the step 1 US Medical Licensing Examination (USMLE) in 2002. Medical educators from the NAA were also asked to review items to be included in the nutrition-related subscore for the 3-step examination. The USMLE step 1 provides a subscore for students’ performance in nutrition-related conditions, whereas the USMLE step 2 provides a subscore for students’ performance on questions related to nutrition and digestive conditions. As a result, Hark (11) recommends that medical nutrition educators be particularly aware of the availability of USMLE step 1 subscores. The general mean subscore for first-time examinees among accredited schools is ∼200 with an SD of ∼20 (14). Overall, nutrition subscores at BUSM were close to the national mean subscores for USMLE step 1 and showed an upward trend over the past decade.
Educational Plan
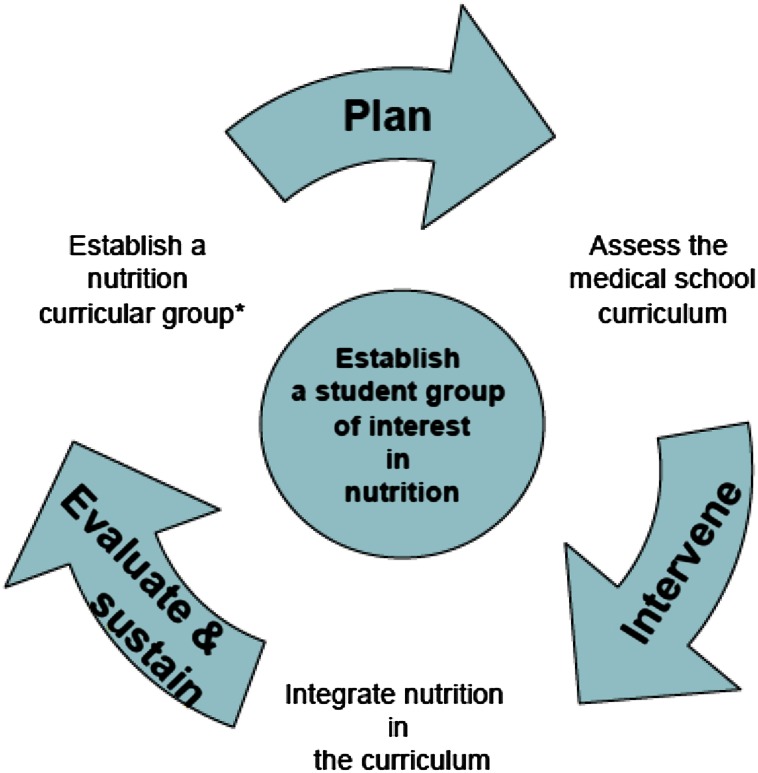
We have developed an educational plan based on a novel student-centered model of nutrition medicine education that focuses on student-mentored extracurricular activities to develop, evaluate, and sustain nutrition medicine education in addition to integrate material and lectures in the medical school curriculum (Fig. 1). The curriculum not only includes case-based and practice-based learning during the 4-y training period, but also the other principles of Harden’s SPICES and Bligh’s PRISMS (15). The SPICES model emphasizes a S tudent-centered approach, P roblem-based learning, and an I ntegrated curriculum. It is C ommunity oriented, uses E ffective modules, and has S ystematic curriculum planning (15). PRISMS encourages curricula to be P roduct focused and practice based, R elevant to outcomes planned, I nterprofessional in character, consist of S hort courses and small group learning, have M ultiple site offerings (e.g., hospitals, ambulatory clinics, community settings), and be S ymbiotic (15). With SNAAC, the Nutrition VIG is developing a novel integrative blackboard site to allow easier access and recognition of nutrition medicine, to facilitate the conduct of program process and content evaluations as well as student and faculty surveys, and to identify specific strategies to sustain the program and disseminate the model.
Figure 1.
Novel model to integrate nutrition medicine at the medical school. Plan: review literature and material, define curricular assessment strategies, conduct surveys. Intervene: define objectives and competencies; integrate modules, cases, and lectures; create a virtual curriculum with internal and external linkage; add extracurricular activities. Evaluate and sustain: develop process and content evaluations, as well as student/staff surveys, build in expert and committee feedback; at the end of its mandate, replace the Vertical Integration Group with a nutrition education subcommittee.
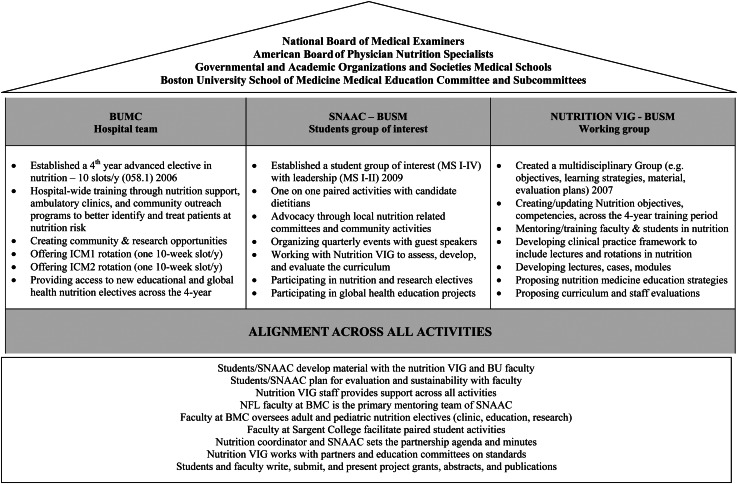
The nutrition medicine activities at BUSM are both specific to and integrated among SNAAC students, the Nutrition VIG, and the hospital team (Fig. 2) The nutrition medicine curriculum is based on competencies and objectives approved by the Medical Education Committee. A Web site is being developed at the medical school using the Blackboard 8 software to act as a virtual nutrition medicine curriculum. On this site, the various nutrition medicine objectives are linked to the nutrition medicine sessions covered in the preclerkship and clerkship courses taught at the medical school. As a result, medical students will be able to identify the content in nutrition medicine of the 4-y courses. They will also have access to updated material that is evidence based and peer reviewed, to a variety of mentors specialized in specific areas of nutrition and obesity medicine, and to events that will help foster learning and networking.
Figure 2.
Nutrition medicine activities. BMC, Boston Medical Center; BU, Boston University; ICM1, Introduction to Clinical Medicine I; ICM2, Introduction to Clinical Medicine II; MS, medical student; NFL, Nutrition & Fitness for Life; SNAAC, Student Nutrition Awareness and Action Council; VIG, Vertical Integration Group.
An example of SNAAC and the Nutrition VIG working together to add more nutrition content to the curriculum was the creation of a Dietary Self-Assessment module. The module was created by members of each group and piloted by ∼15 student volunteers in the Introduction to Clinical Medicine I course in spring 2011. The updated module has become a mandatory component for all 180 students enrolled in Introduction to Clinical Medicine I course in Spring 2012 and is accessible via the Nutrition Medicine Blackboard site. The Nutrition VIG and SNAAC have also worked with course directors to add nutrition components to courses including Integrated Problems, Introduction to Clinical Medicine II, Endocrinology, and Human Behavior in Medicine.
Finally, we plan to conduct several presentations to update faculty and students on the nutrition curriculum and progress of the Nutrition VIG. We expect that nutrition medicine will become highly visible, the quality of teaching material and teacher-student interactions will improve, and the medical students’ aptitude and confidence in counseling will increase.
Options for evaluation tools are being reviewed and tests and surveys will be further conducted within the next 3 y. We have included examples of evaluations and strategies for sustainability and dissemination (Fig. 1). We plan to use standardized measures to evaluate the breadth of nutrition topics covered at the medical school. We will use several instruments such as pre- and post-tests as well as student and staff surveys to evaluate change and students’ competencies in specific areas of nutrition medicine that have been identified as critical for the general health of the public. Tracking systems will be put in place on the blackboard site to identify how many students use the site, use specific material, and perform tests and surveys. Some tests will be mandatory. We will continue to monitor the USMLE nutrition subscores and plan to set up a system to collect students’ characteristics in addition to the USMLE subscores to allow for data adjustment.
Based on our student-centered model of nutrition medicine education, medical students are the agents of change. The medical school will continue to identify faculty and students with interest in nutrition medicine. Work with other groups of students, local education committees, as well as regional, national, and global initiatives will be key to further update the blackboard site and identify new methods of evaluation. We plan to share our experience with other medical schools, schools of nutrition and public health, as well as societies with a focus on nutrition medicine and on education to improve our approach and disseminate the benefits of this model. Further work at a regional and national level will be critical in refining the performance evaluation of medical students and detecting true improvement in US nutrition medicine education.
In summary, we expect that within the next 3 y, the intervention phase of this novel student-centered model will be completed as a subcommittee of nutrition education replaces the Nutrition VIG. We plan to report preliminary program data and strategies to initiate sustainability and dissemination of this model. We hypothesize that the following: 1) the majority of the students will use the virtual curriculum in nutrition medicine; 2) the students’ perception of nutrition medicine education, preparedness to counsel patients, and the subscores on the USMLE step 1 and 2 examinations will improve; and, 3) key strategies to initiate sustainability and dissemination of this model will be identified.
Discussion
We have developed a novel student-centered model of nutrition medicine education that focuses on student-mentored extracurricular activities to integrate, evaluate, and sustain nutrition medicine activities at the medical school in partnership with faculty and clinicians from the Boston University communities. Although the Nutrition VIG plans the implementation of this project, the medical school curricular committees (Medical Education Committee, Pre-Clerkship Curriculum and Clerkship Curriculum subcommittees) provide guidance, support, and reinforce new curricular activities. At present, a medical student group of interest in nutrition medicine is at the core of this model as a critical extracurricular force to improve medical students’ knowledge, attitudes, and skills at the medical school.
Integrating nutrition medicine in the BUSM curriculum has its challenges, but implementation of this project at BUSM has been possible because of grant support, a curricular champion,) curricular committees’ support, and, interested students and faculty. Relationships with the curricular leadership can take a few years to establish and requires opportunities regarding mutuality of interests and timing of curriculum reorganization (12). The process of integrating a curriculum is not only complex, but it is also experienced differently by students and faculty, making some topics easier to integrate than others (16). As described elsewhere (10–12, 17, 18), there are long-term benefits to the integration of nutrition medicine in the curriculum. Former NAA awardees believe that timing is on our side, but they view education efforts sustainability as a limitation. The NAA awardees strongly suggest training interested faculty in nutrition, providing support to a coordinator such as a dietitian, and focusing on advocacy. We further recommend medical students as the agents of change and sustainability in nutrition medicine education.
There is increasing evidence that students engaged in leadership roles benefit both students and the learning community (19). There is also evidence that student leadership in interprofessional education is associated with improved patient outcomes and health services (20). Therefore, there is no reason to believe that students’ participation in the integration of nutrition medicine in the medical school curriculum would not yield similar outcomes. In fact, many of the benefits and challenges faced by former interprofessional education initiatives remind us of our experiences. Similar benefits include the perception of the importance of collaborative care, ability to work in teams, knowledge of professional roles, and interest to participate in collaborative settings in future clinical work. We also notice common barriers such as a lack of funding, clinical placements, faculty guidance, and student leadership opportunities. Finally, and as summarized in their handbook (21), students’ interactions with their mentors are extremely important as they predict education outcomes. Given the current economic environment characterized by limited institutional resources, the participation of students in the development, piloting, and evaluation of education interventions with faculty support is key to student growth and to the sustainability of institutional programs.
Measuring the success of the vertical integration of nutrition in the curriculum has its challenges, too. Educators believe that the best way to evaluate improvement in training of medical students and residents is by assessing the competency of students and residents. In medicine, “competency” has been defined as “the habitual and judicious use of communication, knowledge, technical skills, clinical reasoning, emotions, values, and reflection in daily practice for the benefits of individuals and community being served” (22). Currently, students and residents are assessed in areas that include medical knowledge, patient care, professionalism, communication and interpersonal skills, practice-based learning and improvement, and systems-based practice. Assessment of student and resident competencies can be either formative (e.g., guide future learning) or summative (e.g., judgment about overall competence). Unfortunately, each method of assessment such as written examination, supervision, simulation, and multisource assessment has its strengths and limitations.
Currently, the assessment of medical students and residents is based for the most part on a model developed by the Accreditation Council for Graduate Medical Education) (11). Questions about content and format of nutrition in preclerkships and clerkships including nutrition electives used to be available on the Medical Graduation Questionnaire from the Association of American Medical Colleges and reported progress over time (11). Unfortunately, there are no longer questions related directly to nutrition. Former physician nutrition specialists suggested assessing residents’ competencies in nutrition by substituting nutrition objectives for existing disease-specific objectives (12, 23) using the toolbox at the Association of American Medical Colleges Web site (23). In summary, multiple methods need to be obtained to perform an accurate assessment and new tools need to be identified. (See Supplemental Table 1.)
For the past 2 decades, educators used the concept of number of hours of nutrition instruction for the 4-y period (7, 24) and the USMLE step 1 nutrition subscores (10, 11, 14, 25) to evaluate improvement in nutrition education among medical schools in the United States. Although we were only able to identify a little >20 h dedicated to nutrition in the preclerkship years, we observed that most of our nutrition preclerkship curriculum objectives were covered during the 4-y period using CurrMIT as well as students and course directors’ feedback. CurrMIT provides more information on areas of nutrition covered in the curriculum, but only if the course directors enter the nutrition objectives in the curriculum management system.
Although educators typically suggest using USMLE subscores to monitor student performance in select areas of medical education, Hecker and Violato (26) showed that the greatest variation in performance is among students within a school and not among schools, implying that the formal medical curriculum does not have much effect on USMLE performance (steps 1–3). In fact, nutrition subscores in a quasiexperiment (24) did not appear to be greatly affected by a specific nutrition education model. Thus, future research should focus on student characteristics, quality of medical educators, and areas of medical education that affect student-teacher relationships (26).
In conclusion, we have developed a novel student-centered model of nutrition medicine education that may be critical to students’ education, patient outcomes, and health services. We have described the limitations of current methods used to evaluate the coverage of nutrition education in the medical school curriculum and the competencies of medical students in nutrition medicine. We propose in the interim that medical schools conduct additional competency-based assessment and advocate for novel evaluation tools to detect true improvement in nutrition medicine.
Acknowledgments
We especially thank T. Ainsworth and R. Grochow, 2 medical students who conducted the first nutrition medicine needs assessment at BUSM in 2005. We especially thank Dr. S. Levine, Associate Dean of Academic Affairs, for her guidance, as well as Drs. C. Apovian, Professor of Medicine at BUSM and Director of the Nutrition and Weight management at BUMC, and B. Siegel, Professor of Pediatrics and Psychiatry at BUSM, who have been particularly instrumental in the initial phases of this project and continue to provide assistance in various areas of this project. Furthermore, this project would not have been possible without support from Dr. B. Zuckerman, Chair of the Department of Pediatrics, and Dr. R. Vinci, Vice Chair of Clinical Affairs and Co-Director of the Pediatric Combined Residency at Boston, as well as Dr. H. Oh, past Director of Community Medicine. We are very excited to partner with Dr. W. Lamorte, Assistant Dean of Education and Professor of Epidemiology at the BU School of Public Health and more recently with Ms. J. Salge-Blake, MS, RD, LDN, Clinical Associate Professor, and L. Judd, MS, RD, at the BU Sargent College, Boston. We also acknowledge center support from Dr. S. Fried, Professor of Medicine at BUSM, Director of the Graduate Program in Medical Nutrition Sciences at BUSM and Director of the Boston Nutrition Obesity Research Center (P30 DK46200), and Dr. Walker, Conrad Taff Professor of Nutrition and Pediatrics at the Harvard School of Medicine and Director of the Nutrition Center at Harvard Medical School (P30 DK40561). In addition, we thank Dr. C. Duggan, Associate Professor of Pediatrics at Harvard Medical School and Director of Clinical Nutrition Service at Children’s Hospital of Boston, and S. Collier, MEd, RD, LDN, Clinical Nutrition Director of the Clinical Nutrition Service at Children’s Hospital of Boston for including BU medical students in the Children’s Hospital of Boston nutrition activities. Finally, we thank R. Stein and J. Fleming from the Development Service at BMC for identifying outstanding organizations to support our work. All authors have read and approved the final version this paper.
Footnotes
Abbreviations used: BUSM, Boston University School of Medicine; CurrMIT, Curriculum Management and Information Tool; NAA, National Academy Award; SNAAC, Student Nutrition Awareness and Action Council; USMLE, US Medical Licensing Examination; VIG, Vertical Integration Group.
Literature Cited
- 1.McGinnis JM, Forge WH. Actual causes of death in the United States. JAMA. 1993;270:2207–12 [PubMed] [Google Scholar]
- 2.US Department of Health and Human Services, Office of Disease Prevention and Health Promotion Healthy people 2010: National Health promotion and disease prevention objectives. US Public Health Service. Washington, DC: US Government Printing Office; 1990 [Google Scholar]
- 3.US Preventive Services Task Force Guide to clinical preventive services. An assessment of the effectiveness of 169 interventions. Baltimore, MD: Williams & Wilkins, 1996 [Google Scholar]
- 4.National Academy of Sciences Nutrition education in U.S. medical schools. Washington, DC: National Academies Press; 1985 [Google Scholar]
- 5.American Medical Student Association Nutrition Curriculum Project Advisor Board Essentials of nutrition education in medical schools: a national consensus. Acad Med. 1996;71:969–71 [PubMed] [Google Scholar]
- 6.Spencer EH, Frank E, Elon LK, Hertzberg VS, Serdula MK, Galuska DA. Predictors of nutrition counseling behaviors and attitudes in US medical students. Am J Clin Nutr. 2006;84:655–62 [DOI] [PubMed] [Google Scholar]
- 7.Adams KM, Kohlmeier M, Zeisel SH. Nutrition education in U.S. medical schools: latest update of a national survey. Acad Med. 2010;85:1537–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McClave SA, Mechanick JI, Bistrian B, Graham T, Hegazi R, Jensen GL, Kushner RF, Merritt R. What is the significance of a physician shortage in nutrition medicine? JPEN J Parenter Enteral Nutr. 2010;34 Suppl:7S–20S [DOI] [PubMed] [Google Scholar]
- 9.Apovian CM, Shah MS, Ruth MR, August D, Kushner R, McMahon MM, Alger-Mayer S. Board certification and credentialing in nutrition. JPEN J Parenter Enteral Nutr. 2010;34 Suppl:78S–85S [DOI] [PubMed] [Google Scholar]
- 10.Hark LA, Morrison G. Development of case-based integrated nutrition curriculum for medical students. Am J Clin Nutr. 2000;72: suppl:890S–7S [DOI] [PubMed] [Google Scholar]
- 11.Hark LA. Lessons learned from nutrition curricular enhancements. Am J Clin Nutr. 2006;83 Suppl:968S–70S [DOI] [PubMed] [Google Scholar]
- 12.Krebs NF, Primak LE. Comprehensive integration of nutrition into medical training. Am J Clin Nutr. 2006;83 Suppl:945S–50S [DOI] [PubMed] [Google Scholar]
- 13.Weinsier RL, Boker JR, Brooks CM, Kushner RF, Visek WJ, Mark DA, Lopez-S A, Anderson MS, Block K. Priorities for nutrition content in a medical school curriculum: a national consensus of medical educators. Am J Clin Nutr. 1989;50:707–12 [DOI] [PubMed] [Google Scholar]
- 14.Walsh CO, Ziniel SI, Delichatsios HK, Ludwig DS. Nutrition attitudes and knowledge in medical students after completion of an integrated nutrition curriculum compared to a dedicated nutrition curriculum: a quasi-experimental study. BMC Med Educ. 2011;11:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nair M, Webster P. Education for health professional in the emerging market economies: a literature review. Med Educ. 2010;44:856–63 [DOI] [PubMed] [Google Scholar]
- 16.Woods MN. Nutrition Academic Award: nutrition education in graduate medical education. Am J Clin Nutr. 2006;83: suppl:971S–5S [DOI] [PubMed] [Google Scholar]
- 17.Muller JH, Jain S, Loevser H, Irvby DM. Lessons learned about integrating in a medical school curriculum: perceptions of students, faculty, and curriculum leaders. Med Educ. 2008;42:778–85 [DOI] [PubMed] [Google Scholar]
- 18.Van Horn L. The Nutrition Academic Award: brief history, overview, and legacy. Am J Clin Nutr. 2006;83: suppl:936S–40S [DOI] [PubMed] [Google Scholar]
- 19.Bicket M, Misra S, Wright SM, Shochet R. Medical student engagement and leadership within a new learning community. BMC Med Educ. 2010;10:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hoffman SJ, Rosenfield D, Gilbert JHV, Oandasan IF. Student leadership in interprofessional education: benefits, challenges and implications for educators, researchers, and policymakers. Med Educ. 2008;42:654–61 [DOI] [PubMed] [Google Scholar]
- 21.Komives SR, Dugan JP, Owen JE, Slack C. Wagner W. The handbook for student leadership development. 2nd ed. San Francisco, CA: John Wiley & Sons, Inc; 2006 [Google Scholar]
- 22.Epstein RM, Hundert EM. Defining and assessing professional competence. JAMA. 2002;287:226–35 [DOI] [PubMed] [Google Scholar]
- 23.Deen D. How can nutrition education contribute to competency-based resident evaluation. Am J Clin Nutr. 2006;83: suppl:976S–80S [DOI] [PubMed] [Google Scholar]
- 24.Adams KM, Lindell KC, Kohlmeier M, Zeisel SH. Status of nutrition education in medical schools. Am J Clin Nutr. 2006;83:941S–4S [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Conroy MB, Delichatsios HK, Hafler JP, Rigotti NA. Impact of a preventive medicine and nutrition curriculum for medical students. Am J Prev Med. 2004;27:77–80 [DOI] [PubMed] [Google Scholar]
- 26.Hecker K, Violato C. Medical school curricula: do curricular approaches affect competence in medicine? Fam Med. 2009;41:420–6 [PubMed] [Google Scholar]