Abstract
Objective
Case management–based interventions aimed at improving quality of care have the potential to narrow racial and ethnic disparities among people with chronic illnesses. The aim of this study was to assess the equity effects of assertive community treatment (ACT), an evidence-based case management intervention, among homeless adults with severe mental illness.
Methods
This study used baseline, three-, and 12-month data for 6,829 black, Latino, and white adults who received ACT services through the ACCESS study (Access to Community Care and Effective Services and Support). Zero-inflated Poisson random regression models were used to estimate the adjusted probability of use of outpatient psychiatric services and, among service users, the intensity of use. Odds ratios and rate ratios (RRs) were computed to assess disparities at baseline and over time.
Results
No disparities were found in probability of use at baseline or over time. Compared with white users, baseline intensity of use was lower for black users (RR=.89; 95% confidence interval [CI]=.83–.96) and Latino users (RR=.65; CI=.52–.81]). Intensity did not change over time for whites, but it did for black and Latino users. Intensity increased for blacks between baseline and three months (RR=1.11, CI=1.06–1.17]) and baseline and 12 months (RR=1.17, CI=1.11–1.22]). Intensity of use dropped for Latinos between baseline and three months (RR=.83, CI=.70–.98).
Conclusions
Receipt of ACT was associated with a reduction in service use disparities for blacks but not for Latinos. Findings suggest that ACT’s equity effects differ depending on race-ethnicity.
Racial and ethnic differences in service use that may not be attributable to differences in need for services have been consistently documented. However, less is known about service disparities among people with severe mental illness who are homeless. The high level of unmet need (1,2) and the over-representation of persons from minority groups (3) in this population heighten the importance of identifying and eliminating racial and ethnic service disparities. In prior research we assessed differences between blacks or Latinos and whites in probability and intensity of use of outpatient psychiatric, housing, and case management services under conditions of usual care (4). Our only disparity finding was that blacks had fewer visits for routine outpatient psychiatric services than whites with comparable needs.
A key contributor to racial and ethnic disparities is the lower frequency of use of evidence-based practices and poorer quality of care for persons from minority groups (5). Consequently, efforts aimed at expanding use of evidence-based practices to all who can benefit from them have gained currency as a promising approach to reducing disparities while improving quality of care (6). In mental health, however, little is known about the equity effects of quality improvement interventions (7), and most studies of these effects have focused on depressed populations (8,9). A review of quality improvement interventions for patients with depression and other chronic health conditions identified case management as a key ingredient of multicomponent approaches that improved quality and reduced disparities (10).
Although case management programs for individuals with severe mental illness are a staple of public mental health systems, case management is typically offered through approaches of little or unknown effectiveness (11). A notable exception is assertive community treatment (ACT), an evidence-based practice for adults with severe mental illness that integrates health and social services through intensive case management (11,12). Core features of ACT include a multidisciplinary team approach, frequent and intensive contacts, small caseloads, and assertive outreach (13). Policy makers and administrators are committed to increasing access to ACT (14), and evidence about its equity effects would provide them with a more complete assessment of its value. The purpose of our study was to determine whether receipt of ACT is associated with a reduction in service use disparities for black and Latino adults with severe mental illnesses who are also burdened by homelessness. We hypothesized that disparities in intensity of use of outpatient psychiatric services observed before receipt of ACT (4) would be reduced during the course of ACT treatment.
We reanalyzed data collected as part of the Access to Community Care and Effective Services and Support (ACCESS) program, a federally funded demonstration of the effectiveness of a systems-integrating strategy in the treatment of homeless adults with severe mental illness that was implemented in nine states in the 1990s (15). Although these data are more than a decade old, the ACCESS study remains unparalleled in the size and racial and ethnic diversity of its sample. The results of these analyses provide a baseline for the equity effects that may be expected from the implementation of an evidence-based case management intervention in a complex patient population. Conceptually and methodologically our study adheres to the definition of disparities proposed by the Institute of Medicine: differences in patterns of service use that may not be explained by differences in need for services or treatment preferences (16).
Methods
Overview
We investigated the equity effects of ACT among homeless adults with severe mental illnesses by conducting disparities analyses of baseline and longitudinal utilization data collected for ACCESS study participants. We used zero-inflated Poisson (ZIP) regressions to model the highly right-skewed service use data as a function of race-ethnicity and time while controlling for several potential confounding variables. The ZIP regressions modeled probability of service use and, for those who used services, intensity of use. Parameter estimates from these regressions were used to assess racial and ethnic disparities at baseline and during the course of the 12-month intervention.
Data sources and study population
We used data originally collected by the ACCESS study, and we focused only on black, Latino, and white participants. The methodology and findings of the ACCESS study have been described in detail elsewhere (15,17). An encouragement design was used to evaluate the effectiveness of a systems integration intervention among participants receiving ACT for 12 months at 18 sites located in nine metropolitan areas. Although the fidelity of implementation of the ACT model varied across the study sites, fidelity scores were generally comparable to scores earned by real-world ACT programs (18,19). Further, a multisource study of the sites’ fidelity showed that all sites provided outreach, medication management, and assistance with housing and entitlements, and most also provided counseling and employment assistance (18). Our study was granted exempt status by the University of Pittsburgh Institutional Review Board because we used previously collected data that had no personal identifiers.
Key variables
ACCESS investigators collected a large amount of information on their study population at assessments conducted at baseline and during the course of the intervention (three and 12 months). Our disparities models included selected service use, demographic, and need variables. Because the systems integration intervention was not associated with service use (20), our analyses did not adjust for quasi-experimental status.
Outcome variable
Our outcome variable was use of outpatient psychiatric services. We focused on these services because of their critical importance for this population and because of our previous finding of a disparity in intensity of use of these services under conditions of usual care (4). Data to construct this variable were obtained from responses to three questions that focused on professional services received in the previous 60 days, whether provided by ACT clinicians or not: “Did you meet with a doctor, nurse, social worker, psychologist, or counselor to talk about a psychological or emotional problem you were having?” “Did you attend a day hospital program or a day treatment center?” “Did you receive any other kind of help for a psychological or emotional problem?” Participants who answered yes to any of these questions were asked for a count of visits.
Patterns of use of outpatient psychiatric services were described through measures of probability of use and measures of intensity of use. Probability of use is the proportion of participants who had at least one visit in the 60-day period preceding each of the three assessments. Intensity of use, assessed only among those who used services at least once, represents the mean number of visits in the 60-day period preceding each of the three assessments; visits to obtain any of the services investigated in the three questions had the same weight in the count.
Explanatory variables
Our main explanatory variable was self-reported black, Latino, or non-Latino white race or ethnicity. To ensure that the racial and ethnic groups were comparable in terms of their need for ACT services, our primary multivariate model included age (continuous), sex, marital status (married or not), four measures of mental health need (psychiatric symptoms, psychotic symptoms, psychiatric burden, and a substance use disorder diagnosis), a measure of general health need (medical burden), and two measures of social need (chronic unemployment and chronic homelessness).
The measure of psychiatric symptoms was the composite psychiatric score from the Addiction Severity Index (21); possible scores range from 0 to 1. The measure of psychotic symptoms was a scale adapted from the Diagnostic Interview Schedule (22) and the Psychiatric Epidemiology Research Interview Schedule (23); possible scores range from 0 to 40. Psychiatric burden was a count of all clinician-formulated psychiatric diagnoses; possible values range from 0 to 11. On all these measures, higher values indicate greater mental health need. Substance use disorder diagnosis was a dichotomous variable based on clinician-formulated diagnoses.
Medical burden was a four-level categorical variable that grouped self-reported general medical conditions into zero, one or two, three or four, or five to 17 conditions.
Chronic homelessness was a dichotomous variable indicating whether participants had one or more years of lifetime homelessness and had not lived in a residence of their own in the past 60 days. Chronic unemployment was a dichotomous variable indicating that participants were unemployed or subemployed during most of the previous year (24).
Given the longitudinal nature of our data set, our explanatory model included a time variable. Because we did not want to make unwarranted assumptions about linearity of time effects, we treated time as a categorical variable (0, three, and 12 months) and implemented it by including dummy variables indicating three- and 12-month time points in the ZIP models.
Education, defined as years of schooling, was also included in a secondary model intended to explain our findings.
Statistical analyses
We created one cohort composed of blacks and whites and another composed of Latinos and whites; the same white participants were included in both cohorts. Each cohort was analyzed separately.
We used a ZIP distribution to model the service use data collected at each of the three time points. We used a ZIP distribution in lieu of a standard Poisson distribution because of the large proportion of individuals with zero visits. The ZIP distribution treats the data from a particular service use variable as arising from a mixture of subjects: those who do not use services (nonusers) and those who do (users). ZIP regressions allowed us to model probability of use and intensity of use among users as a function of race-ethnicity and time. Our models adjusted for age, sex, marital status, psychiatric symptoms, psychotic symptoms, psychiatric burden, chronic unemployment, chronic homelessness, a substance use disorder diagnosis, and medical burden. We also included an interaction term between race-ethnicity and time to allow probability of use and intensity of use among users to vary over time as a function of race-ethnicity. Within-subject correlation of responses across time was accounted for by including a subject-level random intercept in the ZIP model. We compared the racial and ethnic groups at baseline and longitudinally; longitudinal trends were assessed for the early part of the intervention (baseline to three months) and for the entire study period (baseline to 12 months).
White race was the reference category for the race-ethnicity coefficients, and 0 months (baseline) was the reference category for time. The reference category for the interaction terms between race-ethnicity and time was the time trend for whites. By way of example, the reference category for the interaction term where time was the 12-month assessment was the trend for whites over the entire study period.
We computed odds ratios (ORs) by exponentiating coefficients related to probability of use and computed rate ratios (RRs) by exponentiating coefficients related to intensity of use. Rate ratios are proportional differences in the mean number of visits between the categories or levels being compared. Statistical significance was set at p≤.05. We present both sets of coefficient estimates along with their 95% confidence intervals (CIs). We used the WinBUGS software package (R, Version 2.9.0; www.r-project.org) to develop and implement this mixed-effects ZIP regression model (25).
Because the ACCESS study used state as a design variable, we accounted for state effects by using state as a stratification variable: we estimated disparities within each state separately and subsequently combined results across all states using inverse variance-weighted averages of regression parameter estimates.
Rates of missing data at any of the three time points were low for most variables, and they were quite comparable across racial and ethnic groups. The highest rates of missing data were observed for medical burden and age. Maximum rates of missing data at the baseline, three-month, and 12-month time points were 13%–14% for blacks, 16% for Latinos, and 12%–13% for whites. We used the SAS program Proc MI with MCMC (SAS, version 9.1) to create five imputed data sets, which we analyzed separately by using complete-data methods. We combined parameter estimates across data sets using standard rules (26).
Results
Characteristics of the racial and ethnic groups
The ACCESS study recruited 6,829 homeless adults with severe mental illnesses who were of black (N= 3,394), Latino (N=381), and non-Latino white (N=3,054) race-ethnicity. Sixteen percent of Latinos (N=61) spoke only Spanish. Attrition by the three- and 12-month time points was moderate (15% and 20%, respectively). Latinos had the highest rates of attrition at those time points (23% and 30%, respectively), and blacks had the lowest rates (12% and 17%); corresponding rates for whites were 17% and 22%.
With the exception of medical burden, the groups differed on all variables included in the multivariate model. The proportions of males and married individuals were larger among Latinos than for the other groups, and mean age was lowest among blacks. Whites scored lowest across the four mental health variables (psychiatric symptoms, psychotic symptoms, psychiatric burden, and a substance use disorder diagnosis), indicating better mental health. Whites also had the lowest levels of social need, with the lowest rates of chronic homelessness and chronic unemployment. Although all groups were unequally distributed across the nine states, Latinos had the highest degree of geographic clustering. Blacks and Latinos had less formal education than whites, but the difference was significant only between Latinos and whites. [A table summarizing data on baseline characteristics of the sample is available in an online appendix to this article at ps.psychiatryonline.org.]
Eighteen percent of blacks (N= 625), 28% of Latinos (N=105), and 21% of whites (N=646) reported no outpatient psychiatric visits at all three time points. For all groups the unadjusted probability of use of outpatient psychiatric services increased from baseline to the three-month time point but dropped from the three- to the 12-month time points. Among service users, longitudinal patterns of intensity of use varied across the groups. For blacks and Latinos intensity changed little between baseline and three months, increasing at 12 months for blacks and dropping at 12 months for Latinos. However, intensity of use among whites dropped from baseline to three months and remained stable thereafter.
Multivariate results
As shown in Figure 1, the adjusted probability of use of outpatient psychiatric services at baseline was .66 (CI=.61–.71) for blacks, .66 (CI=.53–.76) for Latinos, and .65 (CI=.60–.69) for whites. Baseline probability of use did not differ between blacks and whites and Latinos and whites (Table 1). Probability of use increased over time for all participants, peaking at three months. Three- and 12-month estimates were .84 (CI=.80–.87) and .74 (CI=.70–.78) for blacks, respectively, .80 (CI=.67–.88) and .67 (CI= .54–.78) for Latinos, and .83 (CI= .79–.85) and .78 (.74–.81) for whites (Figure 1). As shown in Table 1, there were no differences in time trends between the groups.
Figure 1.
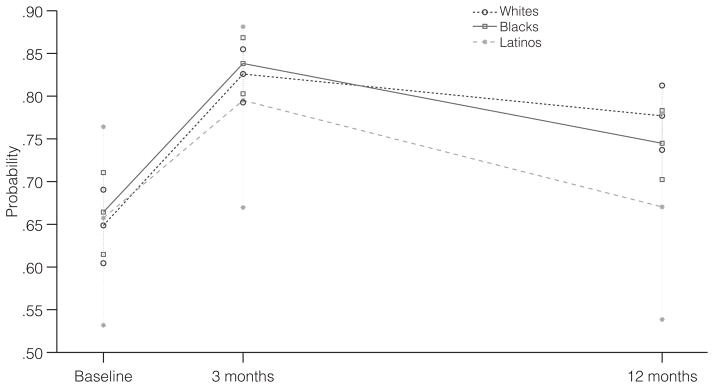
Adjusted probability of use of psychiatric outpatient services in the past 60 days among 6,829 adults receiving assertive community treatment, by assessment timea
a Outlying symbols for each group indicate 95% confidence intervals. Adjustment variables were age, sex, marital status, psychiatric symptoms, psychotic symptoms, psychiatric burden, chronic unemployment, chronic homelessness, a substance use disorder diagnosis, and medical burden.
Table 1.
Differences at three time points in probability and intensity of use of outpatient psychiatric services between blacks and whites and Latinos and whites receiving assertive community treatment (N=6,829)
| Time point and group | Black and white cohort
|
Latino and white cohort
|
||||||
|---|---|---|---|---|---|---|---|---|
| Probability of use
|
Intensity of use
|
Probability of use
|
Intensity of use
|
|||||
| OR | 95% CI | RRa | 95% CI | OR | 95% CI | RRa | 95% CI | |
| Baseline: minority group (reference: whites) | 1.05 | .89–1.24 | .89* | .83–.96 | 1.29 | .82–2.04 | .65* | .52–.81 |
| Baseline to 3 months | ||||||||
| Whites | 2.58* | 2.12–3.13 | .99 | .96–1.03 | 2.94* | 2.43–3.55 | 1.03 | .99–1.09 |
| Minority group (reference: whites) | 1.03 | .78–1.35 | 1.11* | 1.06–1.17 | .60 | .29–1.22 | .83* | .70–.98 |
| Baseline to 12 months | ||||||||
| Whites | 1.91* | 1.55–2.36 | .96 | .91–1.01 | 2.16* | 1.80–2.59 | 1.00 | .96–1.04 |
| Minority group (reference: whites) | .82 | .66–1.02 | 1.17* | 1.11–1.22 | .53 | .27–1.04 | .92 | .79–1.07 |
Rate ratio
p<.05
Among outpatient psychiatric service users, the adjusted analyses of intensity of use of indicated differences across the groups. At baseline the mean numbers of visits for blacks, Latinos, and whites were 2.29 (CI= 1.96–2.67), 1.42 (CI=1.06–1.91), and 2.49 (CI=2.21–2.81), respectively (Figure 2). As shown in Table 1, intensity of use was lower for black users (RR=.89) and Latino users (RR=.65) than for white users. Time trends of intensity of use also differed by race-ethnicity. Intensity of use did not change over time for white users (Table 1 and Figure 2). For blacks, however, intensity of use trended upward over time; the mean number of visits at three and 12 months were 2.53 (CI=2.27–2.83) and 2.65 (CI= 2.26–3.12), respectively (Figure 2). As shown in Table 1, intensity of use increased more for black than for white users over the first three months (RR=1.11) and over the 12-month study period (RR=1.17). For Latinos, intensity of use followed a U-shaped curve, dropping in the early part of the intervention and recovering thereafter. The mean number of visits at three and 12 months were 1.20 (CI=.94–1.53) and 1.57 (CI= 1.19–2.06), respectively (Figure 2). As shown in Table 1, although intensity of use dropped for Latinos compared with whites in the first three months of the study (RR=.83), there were no differences between the groups over the 12-month study period (RR=.92).
Figure 2.
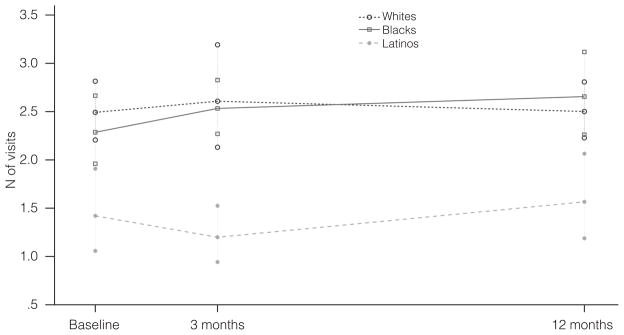
Adjusted intensity of use of psychiatric outpatient services in the past 60 days among 6,829 adults receiving assertive community treatment, by assessment timea
a Outlying symbols for each group indicate 95% confidence intervals. Adjustment variables were age, sex, marital status, psychiatric symptoms, psychotic symptoms, psychiatric burden, chronic unemployment, chronic homelessness, a substance use disorder diagnosis, and medical burden.
When the analysis adjusted for education, the baseline disparity in intensity of use between black and white users was no longer significant; otherwise, the results were unchanged (data not shown).
Discussion
This study found mixed evidence of the equity effects of an evidence-based case management intervention for homeless people with severe mental illnesses, and the results provided only partial support for our hypothesis. The study found that receipt of ACT was associated with an equitable increase in the probability of use of outpatient psychiatric services for all racial and ethnic groups and with a reduction in the preexisting disparity in intensity of use among black and white users. However, the study also showed that this disparities-narrowing effect did not extend to Latinos. Indeed, the preexisting disparity in intensity of use of outpatient services among Latino users became larger in the early part of the intervention.
The only effect of including education level in our ZIP models was that the black-white disparity observed at baseline was no longer significant. This finding suggests that although differences in education may have contributed to a disparity associated with care as usual, they did not account for disparities in longitudinal trajectories observed during the intervention. Because the probability of use of services increased over time for all groups and participants who had not used services at baseline used services during the course of the intervention, a possible explanation for the observed racial and ethnic differences in intensity trajectories is that intensity of use among new users differed across the groups. However, we did not find evidence that this phenomenon accounted for our results (data not shown).
Although it is not always true that greater use of services is in patients’ best interests, the high unmet need of homeless adults with severe mental illnesses and their notoriously tenuous connections to the health care system (1) suggest that higher intensity of use is beneficial in this population.
The observed difference in equity effects between blacks and Latinos may be explained by the fact that ACT was not augmented with enhancements aimed at meeting the specific cultural and linguistic needs of Latinos. Although the language barrier faced by many Latinos may have contributed to our results, we were not able to empirically evaluate its role because of the small number of Latinos in our sample. That intensity of use among Latino users recovered to the baseline level by the 12-month time point suggests that any factors that may have complicated Latinos’ transition to ACT were eventually partially resolved. It is therefore possible that use of a longer follow-up period might have led to different results.
Case management–based interventions that have successfully narrowed disparities in other patient populations are multicomponent interventions that have simultaneously targeted health care system, provider, and patient factors through a chronic disease management approach (27). Thus ACT’s equity effects could be strengthened if features of the chronic care model (28) that are not considered core elements of ACT were added to it.
An extensive body of research exists for ACT’s effectiveness, yet little is known on its equity effects (29). To our knowledge, only three studies have found evidence of differences in racial and ethnic patterns of service utilization among homeless persons with severe mental illness who were receiving ACT services. Lehman and colleagues (30) found that ACT increased the ratio of outpatient to acute-care utilization for both blacks and whites; however, contrary to our findings, they did not find racial differences in the mean number of out-patient psychiatric visits among ACT patients. Our studies are not directly comparable, however, because Lehman and colleagues’ study did not aim to systematically evaluate racial and ethnic service disparities, and it did not use a ZIP model to address the skewness of service use data. Two previous studies based on ACCESS data evaluated several outcomes for blacks and whites (31) and for Latinos and whites (32). Neither study found racial and ethnic differences in mean change scores for use of outpatient psychiatric services between baseline and 12 months. Our study differs from those ACCESS-based studies in that we used all four years of data from the demonstration. In addition, we used data from the three time points, which we modeled longitudinally, and a disparities approach to the modeling.
The dearth of evidence on ACT’s equity effects has meant that resource allocation decisions in the public mental health system have rested solely on considerations of effectiveness and cost. This is problematic because the health care system should aim to deliver care that is both effective and equitable (33). If the target population is as diverse and as poorly served as homeless adults with severe mental illness, incorporating equity evidence into key policy decisions becomes an imperative.
This study had some limitations. Because of the quasi-experimental nature of the ACCESS study, the groups may not have been optimally comparable with regard to all the dimensions affecting need for services. Second, because our outcome measure was constructed with self-reported data, our findings may not reflect true use. Although this is a valid concern, evidence suggests that people with severe mental illness provide reliable data (34), and no evidence exists that reliability varies by race-ethnicity. Third, although our state-stratified analyses controlled for state policies that may contribute to disparities, the study was not powered to control for study site (that is, ACT team). Thus it is possible that site differences in quality of care may have contributed to our findings. Last, because of the ACCESS study design, changes in use of outpatient psychiatric services observed during the course of the intervention may have constituted regression to the mean (20). However, the focus of our study was not ACT’s effects on service use but rather its equity effects.
Conclusions
A critical question in the disparities field is whether quality improvement interventions narrow disparities. If broader use of evidence-based practices and other improvements in services have a greater effect on minority groups than on whites, these improvements will be particularly attractive to policy makers because they can improve both the effectiveness and the equity of the health care system. Our results indicate that ACT, the only evidence-based case management intervention for homeless people with severe mental illnesses, has variable equity effects depending on race-ethnicity. More research is needed to replicate and understand these findings.
Acknowledgments
This research was supported by grants P50-MH073469 and K25-MH076981 from the National Institute of Mental Health and grant P60-MD002261 from the National Center for Minority Health and Health Disparities. The authors are grateful to Robert Rosenheck, M.D., principal investigator of the ACCESS study (client outcomes evaluation), for his assistance and support.
Footnotes
When this work was done, she was with the Department of Psychiatry, University of Pittsburgh.
Disclosures
The authors report no competing interests.
Contributor Information
Dr. Marcela Horvitz-Lennon, Email: mhorvitz@rand.org, RAND Corporation, 4570 Fifth Avenue, Suite 600, Pittsburgh, PA 15213
Dr. Dongli Zhou, Department of Statistics, University of Pittsburgh
Dr. Sharon-Lise T. Normand, Department of Health Care Policy, Harvard Medical School, and the Department of Biostatistics, Harvard School of Public Health, Boston
Dr. Margarita Alegría, Department of Psychiatry, Cambridge Health Alliance, Somerville, Massachusetts
Dr. Wes K. Thompson, Department of Psychiatry, University of California, San Diego
References
- 1.Padgett D, Struening EL, Andrews H. Factors affecting the use of medical, mental health, alcohol, and drug treatment services by homeless adults. Medical Care. 1990;28:805–821. doi: 10.1097/00005650-199009000-00010. [DOI] [PubMed] [Google Scholar]
- 2.Stein JA, Andersen RM, Koegel P, et al. Predicting health services utilization among homeless adults: a prospective analysis. Journal of Health Care for the Poor and Underserved. 2000;11:212–230. doi: 10.1353/hpu.2010.0675. [DOI] [PubMed] [Google Scholar]
- 3.Burt M, Aron LY. Helping America’s Homeless: Emergency Shelter or Affordable Housing? Washington, DC: Urban Institute Press; 2001. [Google Scholar]
- 4.Horvitz-Lennon M, Frank RG, Thompson W, et al. Investigation of racial and ethnic disparities in service utilization among homeless adults with severe mental illnesses. Psychiatric Services. 2009;60:1032–1038. doi: 10.1176/appi.ps.60.8.1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smedley BD, Stith AY, Nelson AR. Un-equal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press; 2003. [PubMed] [Google Scholar]
- 6.Smedley B, Alvarez B, Panares R, et al. Identifying and Evaluating Equity Provisions in State Health Care Reform. New York: Commonwealth Fund; 2008. [Google Scholar]
- 7.Beach MC, Cooper LA, Robinson KA, et al. Strategies for Improving Minority Healthcare Quality. Evidence Report/Technology Assessment 90. Rockville, Md: Agency for Healthcare Research and Quality; Jan, 2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arean PA, Ayalon L, Hunkeler E, et al. Improving depression care for older, minority patients in primary care. Medical Care. 2005;43:381–390. doi: 10.1097/01.mlr.0000156852.09920.b1. [DOI] [PubMed] [Google Scholar]
- 9.Miranda J, Duan N, Sherbourne C, et al. Improving care for minorities: can quality improvement interventions improve care and outcomes for depressed minorities? Results of a randomized, controlled trial. Health Services Research. 2003;38:613–630. doi: 10.1111/1475-6773.00136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chin MH, Walters AE, Cook SC, et al. Interventions to reduce racial and ethnic disparities in health care. Medical Care Research and Review. 2007;64(suppl 5):7S–28S. doi: 10.1177/1077558707305413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mueser KT, Bond GR, Drake RE, et al. Models of community care for severe mental illness: a review of research on case management. Schizophrenia Bulletin. 1998;24:37–74. doi: 10.1093/oxfordjournals.schbul.a033314. [DOI] [PubMed] [Google Scholar]
- 12.Drake RE, Goldman HH, Leff HS, et al. Implementing evidence-based practices in routine mental health service settings. Psychiatric Services. 2001;52:179–182. doi: 10.1176/appi.ps.52.2.179. [DOI] [PubMed] [Google Scholar]
- 13.Dixon L. Assertive community treatment: twenty-five years of gold. Psychiatric Services. 2000;51:759–765. doi: 10.1176/appi.ps.51.6.759. [DOI] [PubMed] [Google Scholar]
- 14.Ganju V. Implementation of evidence-based practices in state mental health systems: implications for research and effectiveness studies. Schizophrenia Bulletin. 2003;29:125–131. doi: 10.1093/oxfordjournals.schbul.a006982. [DOI] [PubMed] [Google Scholar]
- 15.Randolph F, Blasinsky M, Morrissey JP, et al. Overview of the ACCESS Program: Access to Community Care and Effective Services and Supports. Psychiatric Services. 2002;53:945–948. doi: 10.1176/appi.ps.53.8.945. [DOI] [PubMed] [Google Scholar]
- 16.McGuire TG, Alegría M, Cook BL, et al. Implementing the Institute of Medicine definition of disparities: an application to mental health care. Health Services Research. 2006;41:1979–2005. doi: 10.1111/j.1475-6773.2006.00583.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goldman HH, Morrissey JP, Rosenheck RA, et al. Lessons from the evaluation of the ACCESS program: Access to Community Care and Effective Services. Psychiatric Services. 2002;53:967–969. doi: 10.1176/appi.ps.53.8.967. [DOI] [PubMed] [Google Scholar]
- 18.Johnsen M, Samberg L, Calsyn R, et al. Case management models for persons who are homeless and mentally ill: the ACCESS demonstration project—Access to Community Care and Effective Services and Supports. Community Mental Health Journal. 1999;35:325–346. doi: 10.1023/a:1018761807225. [DOI] [PubMed] [Google Scholar]
- 19.Teague GB, Drake RE, Ackerson TH. Evaluating use of continuous treatment teams for persons with mental illness and substance abuse. Psychiatric Services. 1995;46:689–695. doi: 10.1176/ps.46.7.689. [DOI] [PubMed] [Google Scholar]
- 20.Rosenheck RA, Lam J, Morrissey JP, et al. Service systems integration and outcomes for mentally ill homeless persons in the ACCESS program: Access to Community Care and Effective Services and Supports. Psychiatric Services. 2002;53:958–966. doi: 10.1176/appi.ps.53.8.958. [DOI] [PubMed] [Google Scholar]
- 21.McLellan AT, Luborsky L, Woody GE, et al. An improved diagnostic evaluation instrument for substance abuse patients: the Addiction Severity Index. Journal of Nervous and Mental Disease. 1980;168:26–33. doi: 10.1097/00005053-198001000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Robins LN, Helzer JE, Croughan J, et al. National Institute of Mental Health Diagnostic Interview Schedule: its history, characteristics, and validity. Archives of General Psychiatry. 1981;38:381–389. doi: 10.1001/archpsyc.1981.01780290015001. [DOI] [PubMed] [Google Scholar]
- 23.Dohrenwend BP. Psychiatric Epidemiology Research Interview (PERI) New York: Columbia University, Social Psychiatry Research Unit; 1982. [Google Scholar]
- 24.Pickett-Schenk SA, Cook JA, Grey D, et al. Employment histories of homeless persons with mental illness. Community Mental Health Journal. 2002;38:199–211. doi: 10.1023/a:1015211622877. [DOI] [PubMed] [Google Scholar]
- 25.Lunn DJ, Thomas A, Best N, et al. Win-BUGS—a Bayesian modeling framework: concepts, structure, and extensibility. Statistics and Computing. 2000;10:325–337. [Google Scholar]
- 26.Little RJA, Rubin DB. Statistical Analysis With Missing Data. 2. New York: Wiley; 2002. [Google Scholar]
- 27.Van Voorhees BW, Walters AE, Prochaska M, et al. Reducing health disparities in depressive disorders outcomes between non-Hispanic whites and ethnic minorities: a call for pragmatic strategies over the life course. Medical Care Research and Review. 2007;64(suppl 5):157S–194S. doi: 10.1177/1077558707305424. [DOI] [PubMed] [Google Scholar]
- 28.Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Quarterly. 1996;74:511–544. [PubMed] [Google Scholar]
- 29.Coldwell CM, Bender WS. The effectiveness of assertive community treatment for homeless populations with severe mental illness: a meta-analysis. American Journal of Psychiatry. 2007;164:393–399. doi: 10.1176/ajp.2007.164.3.393. [DOI] [PubMed] [Google Scholar]
- 30.Lehman AF, Dixon L, Hoch JS, et al. Cost-effectiveness of assertive community treatment for homeless persons with severe mental illness. British Journal of Psychiatry. 1999;174:346–352. doi: 10.1192/bjp.174.4.346. [DOI] [PubMed] [Google Scholar]
- 31.Chinman MJ, Rosenheck RA, Lam JA. Client–case manager racial matching in a program for homeless persons with serious mental illness. Psychiatric Services. 2000;51:1265–1272. doi: 10.1176/appi.ps.51.10.1265. [DOI] [PubMed] [Google Scholar]
- 32.Ortega AN, Rosenheck R. Hispanic client–case manager matching: differences in outcomes and service use in a program for homeless persons with severe mental illness. Journal of Nervous and Mental Disease. 2002;190:315–323. doi: 10.1097/00005053-200205000-00008. [DOI] [PubMed] [Google Scholar]
- 33.IOM. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- 34.Goldberg RW, Seybolt DC, Lehman A. Reliable self-report of health service use by individuals with serious mental illness. Psychiatric Services. 2002;53:879–881. doi: 10.1176/appi.ps.53.7.879. [DOI] [PubMed] [Google Scholar]


