Abstract
Specialized phagocytes are found in the most primitive multicellular organisms. Their roles in homeostasis and in distinguishing self from non-self have evolved with the complexity of organisms and their immune systems. Equally important, but often overlooked, are the roles of macrophages in tissue development. As discussed in this Review, these include functions in branching morphogenesis, neuronal patterning, angiogenesis, bone morphogenesis and the generation of adipose tissue. In each case, macrophage depletion impairs the formation of the tissue and compromises its function. I argue that in several diseases, the unrestrained acquisition of these developmental macrophage functions exacerbates pathology. For example, macrophages enhance tumour progression and metastasis by affecting tumour-cell migration and invasion, as well as angiogenesis.
A century after Metchnikoff's Nobel Prize for the discovery of macrophages and innate immunity, it is being increasingly appreciated that macrophages have many non-immunological trophic roles during development. In fact, Metchnikoff1 originally regarded the motile phagocytic cells that he first observed in Ascidians as homeostatic regulators that were involved in maintaining the integrity of an organism through a process he called `physiological inflammation'. He contrasted this term with `pathological inflammation' resulting from external challenges, which we now know as innate immunity1. In this Review, I discuss evidence indicating that the most ancient and still extremely important roles of macrophages relate to developmental processes. Furthermore, I illustrate how pathogenic processes such as cancer can subvert these developmental functions of macrophages, resulting in potentiation of disease.
Macrophage origin and classification
Macrophage lineages
The definition of a macrophage has challenged developmental biologists since these cells were first described. Originally, the emphasis was on phagocytosis, which led to the term macrophages (from the Greek for large eaters) to distinguish these cells from the polymorphonuclear microphages (from the Greek for small eaters; neutrophils). This study of phagocytosis identified two types of macrophage cell: cells that aligned the endothelium and amoeboid cells known as histiocytes2,3. This definition evolved into the reticuloendothelial system (RES) of classification, which suggested that these two types of cell had a common origin as they both cleared particles from the blood. However, as many cells can be phagocytic and because endothelial cells and histiocytes are morphologically and functionally distinct, the use of the RES to classify macrophages went out of favour and was replaced by a system that classified macrophages based on ontogeny and phagocytosis, which was named the mononuclear phagocytic system (MPS)3. It included bone-marrow-derived precursor cells, monocytes in the peripheral blood and mature macrophages in tissues, but excluded endothelial cells and other mesenchymal cells that are not obviously derived from the bone marrow. More recently, the classification of the MPS has been refined, as it has become clear that some dendritic cells (DCs) can differentiate from monocytes and macrophages4,5. The MPS has been prominent for the past four decades, but the recent identification of myeloid precursor cells that differentiate into endothelial cells6 indicates that a re-examination of the RES might be required7.
The MPS is largely an ontological definition for vertebrates and it is useful for classifying macrophages in adults. However, the origin of these phagocytic cells in embryos is more complex. In mice, the first population of macrophages is observed at the late head-fold stage (embryonic day (e)7.5) and is of maternal origin8. Embryonic macrophages (derived from the primitive endoderm of the yolk sac) are first found around e8 and invade the anterior structures of the embryo. These cells do not go through a monocytic stage but differentiate directly from mesenchymal progenitor cells7. Haematopoietic progenitor cells from the yolk sac of rats and mice first populate the primitive liver, which is the first site of definitive haematopoiesis, and at e10 are followed by a second wave of progenitor cells from the aorta–gonads–mesonephros region of the embryo9–11. By e10.5 to e11, the primitive liver is the main site of haematopoiesis and thereafter macrophages that have differentiated from monocytic progenitor cells are found throughout the embryo10,11. After birth, the bony structures are formed and as a result the main site of haematopoiesis is the bone marrow; at this stage, the MPS is established3 (FIG. 1).
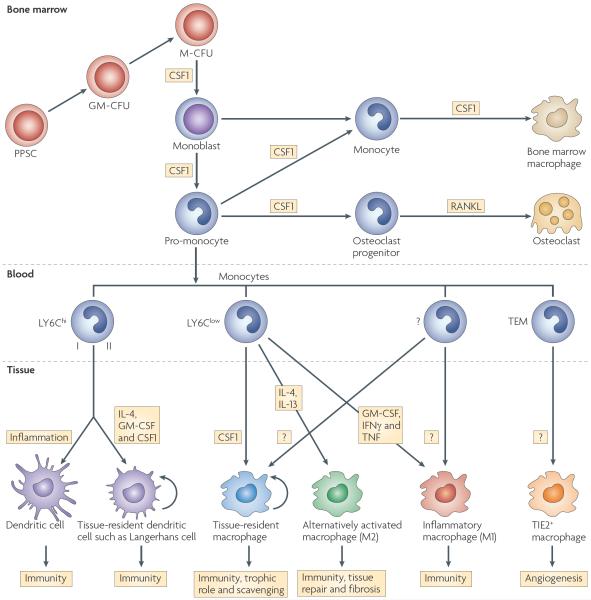
Figure 1. The mononuclear phagocytic lineage and the control of its development by growth factors.
Cells of the mononuclear phagocytic system (MPS) arise in the bone marrow, where they develop from pluripotent stem cells (PPSCs) through various multipotent progenitor stages: granulocyte/macrophage colony-forming unit (GM-CFU) to macrophage CFU (M-CFU) to monoblast to pro-monocyte. In the bone, osteoclast progenitors develop from these cells under the influence of colony-stimulating factor 1 (CSF1), and these differentiate in response to receptor activator of nuclear factor-κB ligand (RANKL) into osteoclasts. Another population differentiates into bone marrow macrophages also in response to CSF1, and the ex vivo culture of these cells and their progenitors is often used for macrophage studies. In addition, monocytes are released into the circulation. There is a growing body of evidence for an as yet undefined number of subpopulations of monocytes126 that have different developmental fates defined by the markers shown. LY6Chi monocytes consist of at least two types according to their expression of CXC-chemokine receptor 2 (CXCR2) and differentiate into dendritic cells of different types according to the state of inflammation and cytokine and/or growth factor exposure. Other as yet undefined types of monocytes are LY6Clow and differentiate into tissue-resident macrophages in response to CSF1; these have different names and functions according to their tissue residency (TABLE 1). Alternatively activated macrophages differentiate in response to parasitic infection, allergic conditions and during tissue repair through the effects of interleukin-13 (IL-13) and IL-4; these are also known as M2 macrophages. Inflammatory macrophages (also known as M1 macrophages) can also be found at sites of infection and injury, and these develop under the influence of GM-CSF, interferon-γ (IFNγ) and tumour necrosis factor (TNF). Immature macrophages can also differentiate into dendritic cells (not shown). In addition, TIE2-expressing monocytes (TEMs) give rise to TIE2+ macrophages that are involved in angiogenesis in tumours. It should also be noted that in addition to the growth factors shown here, many other ligands, particularly those that signal through Toll-like receptors, influence macrophage differentiation. In addition, the rigid lineage diagrams and growth factor assignments depicted here are for illustrative purposes only. In fact, there can be cross-differentiation of macrophage phenotypes during the evolution of an immune response, and tissue-restricted progenitors can expand within a tissue through proliferation. In addition, growth factors can act differently according to context and desired response, for example CSF1 receptor signalling is required for Langerhans-cell differentiation but CSF1 can act with IL-4 to inhibit dendritic-cell differentiation, at least in vitro. These complexities cannot be represented in such a simple lineage diagram but they are discussed in REFs 18,22,126.
In mammals, macrophages are found in all tissues after birth (TABLE 1). In some tissues, they constitute 10–20% of all cells — for example, microglial cells in the brain and Kupffer cells in the liver — whereas in other tissues, such as at the musculo–skeletal junctions, they are rare12,13. In addition, monocyte- or macrophage-derived DCs (FIG. 1) are often found in precise locations and are given distinct names; for example, Langerhans cells in the skin13–15.
Table 1.
Diversity of macrophages
| Tissue | Specific macrophage name | Function |
|---|---|---|
| Bone | Osteoclast | Bone remodelling and providing a stem cell niche |
| Bone marrow macrophage | Erythropoiesis | |
| Brain | Microglial cell | Neuronal survival and connectivity, and repair after injury |
| Epidermis | Langerhans cell | Immune surveillance |
| Eye | NA | Vascular remodelling |
| Intestine | Crypt macrophage | Immune surveillance |
| Kidney | NA | Ductal development |
| Liver | Kupffer cell | Clearance of debris from blood and liver tissue regeneration after damage; liver development? |
| Mammary gland | NA | Branching morphogenesis and ductal development |
| Ovary | NA | Steroid hormone production and ovulation |
| Pancreas | NA | Islet development |
| Testis | NA | Steroid hormone production; Leydig-cell development? |
| Uterus | Uterine DC | Angiogenesis and decidualization |
| Uterine macrophage | Cervical ripening |
DC, dendritic cell; NA, not applicable.
During development, the density of macrophages changes in many tissues14. The expression of green fluorescent protein (GFP) by the mononuclear phagocytic lineage under the control of the Csf1r (colony-stimulating factor 1 receptor) promoter13,16 has shown striking, organized patterns of macrophages in tissues. However, a caveat of these studies is that the transgenic reporter also marks neutrophils, although these are rare in most tissues and are also easily distinguished because of their polymorphonuclear morphology. using a truncated Csf1r promoter, the expression of which is more restricted to macrophages, similar patterns of macrophage tissue expression have been observed, which are consistent with F4/80-specific antibody staining for macro phages14,16,17. These analyses also show that there are marked morphological differences within and between macrophage populations, ranging from highly dendritic to round morphologies.
Macrophage classification
The diversity of macrophage functions has led to various classification attempts. Given the immune functions of macrophages, the first type to be described was the `classically activated' macrophage that responds to interferon-γ (IFNγ) by releasing pro-inflammatory cytokines, such as interleukin-12 (IL-12) and IL-23, and that is involved in the T helper 1 (TH1)-cell-mediated immune resolution of infection18. In contrast to this are the `alternatively activated' macrophages, which respond to TH2-type cytokines, such as IL-4 and IL-13, and are involved in fibrosis, tissue repair and humoral immunity19. These two opposite phenotypes have been designated by some as M1- and M2-type macrophages19. There was also an appreciation that some macrophages are involved in wound repair, and these cells were thought to be a subpopulation of M2-type macrophages20. In addition, macrophages that are associated with tumours have been proposed to be M2-type macrophages19, emphasizing the tissue trophic and repair functions of macrophages. However, I believe that the M1–M2 classification is overly restrictive. It ignores the different fates of macrophages that develop in response to CSF1 (also known as M-CSF) compared with those that develop in response to granulocyte/macrophage CSF (GM-CSF; also known as CSF2). The differential development of these macrophages gives rise to cells that are at opposite ends of the spectrum, with GM-CSF-regulated macrophages having mainly immunological roles and CSF1-regulated macrophages having trophic roles21.
Another more flexible classification has been suggested recently in which macrophages are part of a continuum and have a range of overlapping functions, with classically activated, wound-healing and regulatory macrophages occupying different points of the spectrum22. However, the developmentally important macrophages that are described in this and other reviews9 have not been specifically included in any of these classifications. They form another subpopulation that is grouped together with embryonic9 and wound-healing22 macrophages and with irreversibly differentiated osteoclasts. Each of these many different types of macrophage is specified by the microenvironment, although there is considerable plasticity between distinct types. This concept recalls Metchnikoff's original classification, which considered macrophages as part of a continuum, keeping the self whole in development and adulthood (physiological inflammation) and differentiating it from non-self and the environment (pathological inflammation).
Factors involved in macrophage differentiation
The development of macrophages from monocytes is regulated by several growth factors. In mice and rats at least, the most important of these is CSF1, which stimulates the differentiation of macrophages from progenitors as well as their proliferation and viability in vitro. CSF1R is expressed by all cells that are part of the MPS and helps to define them23. But macrophages can also be grown and differentiated in vitro from monocytic progenitors in the presence of GM-CSF and to a lesser extent in the presence of IL-3, which generates immature macrophages, or IL-3 in combination with CSF1, which generates mature macrophages21,24. In addition, the transcription factor PU.1, which among other functions controls the expression of CSF1R, regulates differentiation of progenitors to the macrophage lineage although its functions are not limited to cells that are part of the MPS.
Null mutations of the genes encoding all these factors have been generated or identified in mice. In the absence of environmental or immunological challenge, the phenotype is mild for both GM-CSF and IL-3 deficiency, with little effect on myeloid-cell density or function except for cells that reside in the lung25–27. By contrast, Pu.1-deficient mice have a depletion of B cells and granulocytes and also a significant decrease in the size of many macrophage populations; these mice die perinatally28–30. During embryogenesis, the development of macrophages from Pu.1-deficient mice is normal until they begin to progress through the monocyte precursor stage10. A Pu.1-related transcription factor, Spic, is also required for the development of population of splenic red pulp macrophages that removes red blood cells31.
Mice with the naturally occurring null mutation in the Csf1 gene, known as osteopetrotic (Csf1op)32, and mice that have a targeted null mutation in Csf1r are both severely depleted of most macrophage populations. However, some macrophage populations such as those that reside in the spleen are mostly unaffected, and there is little effect on other haematopoietic lineages in these mice32. All of the phenotypes found in Csf1op/op mice are also found in Csf1r−/− mice, which indicates that CSF1R is the only receptor for CSF1 (REF. 33). However, several phenotypes are more severe in Csf1r−/− mice, and these mice rarely live beyond a few weeks of age. More severe phenotypes of Csf1r−/− mice include the complete loss of epidermal langerhans cells15 and microglial cells (B. Erblich and J.W.P., unpublished observations). By contrast, the numbers and physiology of these cells are relatively normal in Csf1op/op mice14,34. Recently, another ligand, IL-34, has been identified that binds with greater affinity to CSF1R than does CSF1, which can support myeloid-cell development in vitro35. The biological functions of IL-34 remain to be determined but might explain the differences between the phenotypes of Csf1op/op and Csf1r−/− mice. The specific macrophage deficiencies observed in Csf1op/op mice confirm the important role of CSF1 in regulating macrophage survival, proliferation and differentiation. Furthermore, Csf1op/op mice on a mixed genetic background are viable, which has allowed for the analysis of the function of their macrophages. Strikingly, Csf1op/op mice have few immunological deficiencies except against pathogens that replicate in macrophages, such as Listeria monocytogenes and mycobacteria, to which the mice were more susceptible36,37. However, Csf1op/op mice have many developmental abnormalities that are attributable to the lack of individual macrophage populations32. These data show that an important activity of macrophages is their trophic functions during development, a topic that I discuss in the rest of this Review32.
Trophic functions of macrophages
Bone morphogenesis
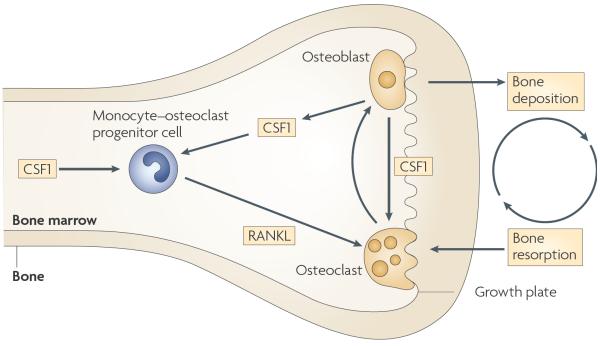
The most obvious phenotype of Csf1op/op mice is osteopetrosis, which is the result of the depletion of osteoclasts (FIG. 2). Osteopetrosis is also observed in Csf1−/− rats (known as toothless rats; tl rats) and in Pu.1-deficient mice32,38,39. Studies using Csf1op/op mice have shown that CSF1 is essential for the development of a common monocyte–osteoclast bone marrow progenitor cell that differentiates in response to receptor activator of nuclear factor-κB ligand (RANKl; also known as TNFSF11) to become a multi-nucleated functional osteoclast40 (FIG. 2). CSF1 also increases mature osteoclastic bone resorption41. Without functioning osteoclasts, the bone is not re-sculpted and removed at the growth plate and osteopetrosis ensues. Osteopetrosis causes a lack of a marrow cavity and consequently the elimination of much of the haematopoiesis that normally occurs in the bone marrow, although compensatory haematopoiesis still occurs in the liver and spleen42. It also results in a lack of teeth because the tooth buds, although formed, cannot erupt through the jaw32,39. In both Csf1op/op mice and tl rats, osteopetrosis and dental defects can be reversed by the systemic administration of CSF1 (REFs 43,44). This osteopetrotic phenotype is one of the best examples of the developmental requirement for a specialized type of macrophage and is iconic of the tissue-trophic role of macrophages, the malfunction of which results in tissue malformation and downstream physiological effects on haematopoiesis and tooth eruption.
Figure 2. The trophic role of macrophages in bone morphogenesis.
Colony-stimulating factor 1 (CSF1) is required for the formation of a common monocyte–osteoclast progenitor cell in the bone marrow that then proliferates and differentiates in the presence of receptor activator of nuclear factor-κB ligand (RANKL) to form multinuclear osteoclasts. These remodel the bone that is laid down by osteoblasts. To coordinate these processes, osteoblasts produce CSF1, which not only mediates the correct positioning of osteoclasts but also affects their local function.
Ductal branching
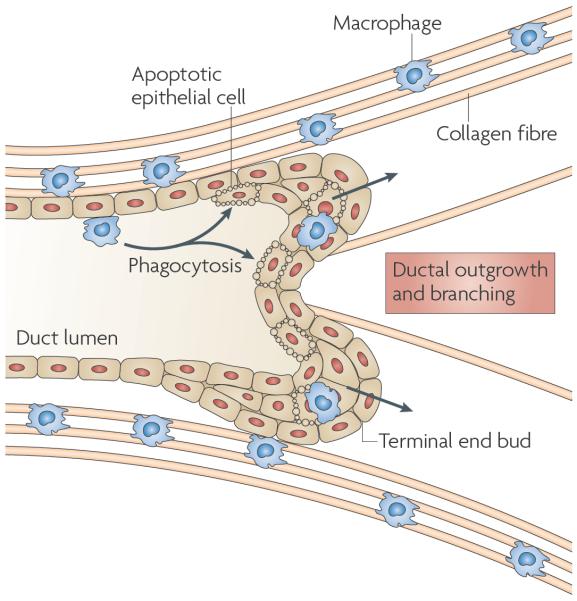
Many tissues are formed by the outgrowth of epithelial rudiments into an underlying mesenchyme, which specifies their identity. A well-studied example is the mammary gland: in mice that are at the beginning of puberty, the rudimentary mammary ducts develop multilaminate bulbous termini known as terminal end buds (TEBs) that grow out through the fat pad. While they do so, the mammary ducts divide to give rise to the branched ductal structures of the mature mammary gland. Similarly, during pregnancy there is further ductal outgrowth and extensive proliferation of the lobuloalveolar structures that produce milk during lactation. As soon as the TEBs begin to grow during puberty, macrophages are recruited and align along the TEB shaft45. In vivo imaging shows that these macrophages move rapidly around the shaft of the TEB and cross over at the invading front46. These movements are promoted by a collagenous cluster of fibres, mainly of collagen I, that run parallel to the direction of the TEB outgrowth46. In addition, macrophages are found within the TEB structure, where they phagocytose the apoptotic epithelial cells as the lumen is formed45 (FIG. 3). Studies in Csf1op/op mice showed that macrophages were not recruited to the TEB and the rate of outgrowth of these ductal structures and their branching was decreased45,47, resulting in an atrophic mammary gland. A similar defect was observed during the ductal outgrowth that occurs during pregnancy, although lobuloalveolar development was unaffected47. Importantly, the restricted transgenic expression of CSF1 in cells in the mammary epithelium resulted in the recruitment of macro phages, which are the only cells that express CSF1R, and the rescue of the branching defect, without correction of the other systemic defects observed in Csf1op/op mice48. This study showed that the defect was organ autonomous and macrophage specific. Although the mechanism behind these macrophage activities remains to be fully elucidated, the formation of collagen fibrils but not collagen I synthesis was inhibited in the Csf1op/op mice. Rescue of the macrophage deficiency resulted in the formation of normal fibrils and the restoration of ductal outgrowth and branching, which indicates that one function of macrophages is in matrix remodelling46 (FIG. 3).
Figure 3. The trophic role of macrophages in ductal branching.
In the mammary gland, macrophages are found in the stroma immediately adjacent to the growing terminal end bud (TEB) and are often associated with collagen fibres, which they help to form. Ablation of macrophages slows outgrowth and branching of the TEB into the fatty stroma, and this is associated with a disruption of collagen fibrillogenesis.
Another example of the role of macrophages in ductal development also comes from studies in Csf1op/op mice. Similarly to the mammary gland, macrophages are recruited adjacent to the epithelial tissue as pancreatic islets form. Their absence in Csf1op/op mice results in decreased mass of insulin-producing β-cells, abnormal post-natal islet morphogenesis and impaired pancreatic cell proliferation49. A similar phenomenon is found during the expansion of the pancreas in pregnancy49. In fact, macrophages are required throughout life for the development and remodelling of the pancreas49. Furthermore, the addition of CSF1 stimulated an increase in the number of insulin-producing cells in pancreas explant cultures, which was accompanied by an increase in the number of macrophages50. The effects of macrophages on branching morphogenesis probably apply to other tissues as well. Indeed macrophages are recruited to the developing kidney and to kidney explant cultures treated with CSF1 in the presence of low levels of lipopolysaccharide, and this results in a significant increase in the numbers of branch tips and nephrons9.
Neural networking
Csf1op/op mice have considerable reproductive defects51. Male mice have low libido and sperm counts, which are attributable to low testosterone levels52, and female mice have poor ovulation rates and extended oestrous cycles53. At first glance, these data are consistent with the role of macrophages in the development and maintenance of gonadal tissue, as defined by ablation studies. For example, in male mice, macrophages associate closely with the testosterone-producing leydig cells in the testis, and their ablation using liposome-encapsulated clodronate suppressed testosterone synthesis54. In female mice, macrophages are recruited to the interstitium of the developing ovarian follicle, with maximum numbers being present just before ovulation53, and a similar chemical ablation of macrophages affects steroidogenesis and inhibits ovulation55,56. In Csf1op/op mice, macrophage density is markedly decreased in gonadal tissues, interstitial structure is affected in the testes and the morphology of Leydig cells is distorted52,57. Nevertheless, the primary defect in the reproductive function of Csf1op/op mice occurs in the regulation of the hypothalamic–pituitary–gonadal axis. In male Csf1op/op mice, the level of circulating luteinizing hormone, which is the pituitary hormone that controls testosterone biosynthesis, is low and the negative feedback mediated by sex steroid hormones such as testosterone, which regulates the production of luteinizing hormone, is attenuated and inverted. As a result, the normal increase in luteinizing hormone that is associated with testosterone removal does not occur, and testosterone administration increases luteinizing hormone levels under conditions that would normally decrease them57. Furthermore, administration of a gonadotrophin-releasing hormone (GnRH) agonist that substitutes for endogenous GnRH production by the hypothalamus rescues the luteinizing hormone deficiency in Csf1op/op mice (which shows that the defect is at the level of the hypothalamus), and administration of luteinizing hormone restores testosterone levels57. In female Csf1op/op mice, there is also decreased negative feedback on the hypothalamic–pituitary–gonadal axis following oestrogen removal and a complete absence of the positive feedback to oestrogen that causes the surge in luteinizing hormone, which is required for ovulation. In addition, a delay in puberty has also been observed in these mice34.
Reconstitution of neonatal Csf1op/op mice with human recombinant CSF1 throughout their lifetime rescued these hypothalamic deficiencies, restoring both feedback control and the timing of puberty, and timed administration of CSF1 during the first 2 weeks of life almost entirely reversed the defects34. These data show that the reproductive defects are primarily, if not entirely, at the level of the hypothalamus or higher in the brain51 and that the absence of CSF1 signalling during the crucial period of development when the hypothalamus is sexualized results in a permanent impairment throughout life.
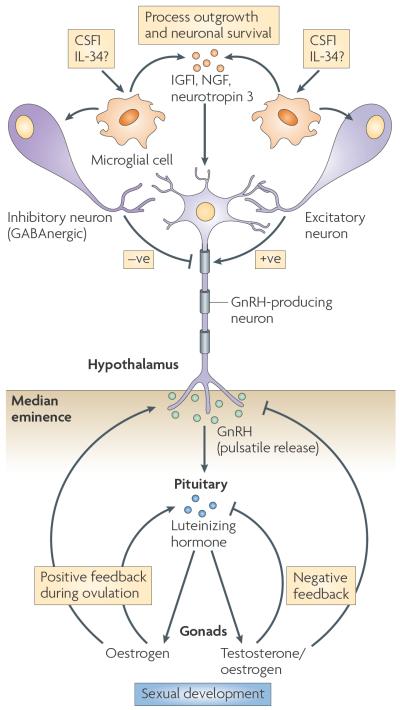
Evidence for neuronal defects in the brains of Csf1op/op mice has also come from studies assessing auditory or visual evoked potentials (VEPs) that showed that the mice have impaired auditory and visual processing58. Intracortical recordings of VEPs and multiple unit activities (a summation of action potentials during stimulation) were attenuated and persistent in the Csf1op/op mice compared with wild-type mice. By contrast, the time for retinal striate conductance was the same, indicating that the CSF1 deficiency does not block neuronal transmission. Furthermore, administration of a γ-aminobutyric acid A (GABAA) antagonist (which overrides inhibitory signals) into the intracortical region of the brain in Csflop/op mice resulted in attenuated but persistent firing, whereas in wild-type mice there was a robust excitatory response with subsequent inhibition58. These data show a primary neuronal deficit in Csf1op/op mice involving both excitatory and inhibitory signals (FIG. 4).
Figure 4. The trophic role of macrophages in neuronal patterning.
Microglial cells are a specialized type of macrophage found in the brain. These cells respond to colony-stimulating factor 1 receptor (CSF1R) signalling to produce factors that are required for the establishment of neuronal connectivity. Depletion of CSF1 shows that, among other things, microglial cells regulate the hypothalamic–pituitary–gonadal axis through negative signalling from neurons that respond to γ-aminobutyric acid A (GABAA neurons; known as GABAnergic) and positive signalling from excitatory neurons, which allows gonadotrophin-releasing hormone (GnRH) to be released in a pulsatile manner into the median eminence. This induces the release of luteinizing hormone by the pituitary, which controls testosterone and oestrogen biosynthesis in the gonads. IGF1, insulin-like growth factor 1; IL-34, interleukin-34; NGF, nerve growth factor.
The brain is populated by a large number of macrophages, known as microglial cells, which account for ~15% of the brain's cellularity. These cells express CSF1R in the brain during development and in adulthood13,59, and indeed seem to be the only cells that express CSF1R in the brain. They are therefore the only target cells of CSF1, which is also expressed in the brain throughout life in spatially and developmentally specific ways58. Nevertheless, the numbers of microglial cells in mice that are on a mixed genetic background are not decreased in the Csf1op/op mice (although their signalling in response to CSF1 is non-existent), despite a small developmental delay in their acquisition, and the brains of these mice have an overall normal morphology34,60. By contrast, there is a complete absence of microglial cells in Csf1r−/− mice (B. Erblich and J.W.P., unpublished observations) from birth and at all stages of post-natal development. This is associated with marked structural defects in the brain, including swollen ventricles, thinned cortex and decreased size of olfactory bulbs. The contrast in the severity of phenotype between the receptor- and ligand-deficient mice is particularly striking, and IL-34, acting as an alternative ligand for CSF1R, might account for this discrepancy in the brain. These data make a persuasive case for CSF1R-regulated microglial cells having an important role in the development of a functional neuronal circuitry. Further evidence for the involvement of microglial cells comes from in vitro studies of rat embryonic brains, in which CSF1 promotes process outgrowth and neuronal survival in mixed cell cultures but not in pure neuronal cultures58.
The molecular basis of the functions of microglial cells in brain development remains to be determined, but it is instructive that during brain injury, microglial cells are important in orchestrating wound repair61. For example, implantation of macrophages greatly promoted the regeneration of the spinal cord in paraplegic rats62, and in an ischaemia model, depletion of microglial cells increased the area of the infarction whereas administration of CSF1 stimulated microglial-cell proliferation and decreased infarct size63. Furthermore, in Csf1op/op mice, fewer microglial cells are recruited to the site of injury and neuronal survival is compromised compared with wild-type mice that have comparable injuries64. Microglial cells also metabolize steroid hormones65, and this function might have a role in sexualizing the brain during puberty. Microglial cells have also been shown to produce a wide range of growth factors, including insulin-like growth factor 1 (IGF1), and various neurotrophic and protective factors, such as nerve growth factor and neurotropin 3. It seems probable that these factors are involved in the establishment of normal neuronal circuitry during development.
Angiogenesis
Macrophages have been implicated in the regulation of angiogenesis during wound healing66,67, but there has been little focus on their roles in angiogenesis during development. Nevertheless, macrophage ablation using a suicide gene approach (that is, the expression of a gene that induces apoptosis) has definitively shown the importance of macrophages in vascular remodelling during eye development68. In this tissue, there are three connected but anatomically distinct vascular structures that are remodelled post-natally in mice (FIG. 5). In one of these, the hyaloid vessel system, macrophages are closely associated with the blood vessels, and their ablation, either using a suicide gene approach or through their loss in PU.1-deficient mice, results in a failure of remodelling and persistence of the vascular structure post-natally68. The mechanism of this macrophage-mediated effect is through their production of WNT7B, which stimulates adjacent vascular endothelial cells to enter the S phase of the cell cycle and to subsequently undergo apoptosis as a result of the lack of a survival signal from pericytes (mesenchymal cells that are associated with the walls of small blood vessels)69,70. This not only allows for vascular remodelling to occur, but also ensures that the macrophages are in place to phagocytose the resultant apoptotic endothelial cells69,70. Importantly, in another developmental context, the ablation of monocyte-derived DCs during embryo implantation in mice inhibited decidualization owing to defective angiogenesis, and this resulted in the termination of pregnancy. In this study, DCs seemed to regulate angiogenesis at the implantation site through the production of vascular endothelial growth factor (VEGF) and transforming growth factor-β1 (TGFβ1)71.
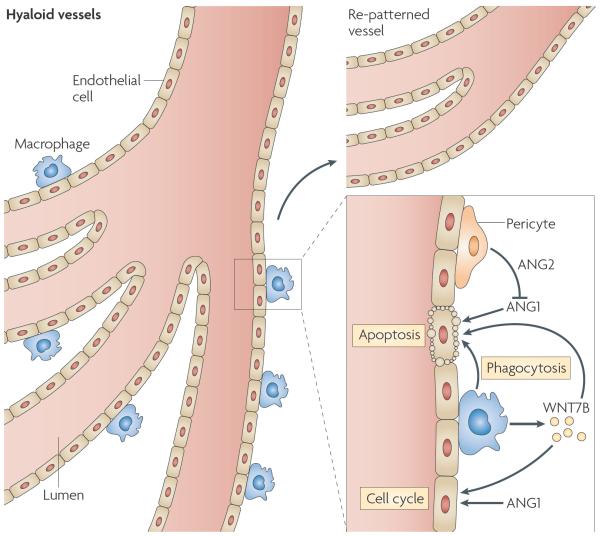
Figure 5. The trophic role of macrophages in angiogenesis and vascular remodelling.
During eye development, the hyaloid vessel system regresses and is re-patterned. Macrophages closely associated with the vessels synthesize WNT7B, which stimulates vascular endothelial cells to enter the DNA synthesis phase of the cell cycle. In the presence of pericyte-produced angiopoietin 2 (ANG2), the survival signal from ANG1 is blocked and the endothelial cells undergo apoptosis and are phagocytosed by the macrophages. In this manner, vascular regression and proper patterning is achieved69,70.
Further support for the role of macrophages in angiogenesis came from studies using tetracycline-regulated expression of VEGF in the heart and lungs of normal mice, which increased angiogenesis. VEGF recruited numerous bone-marrow-derived macrophages to the tissue through signalling by CXC-chemokine receptor 4 (CXCR4), the ligand for which is expressed by pericytes. These cells had all the characteristics of macrophages and secreted angiogenic molecules as assayed by an aortic ring sprouting assay72. These data indicate that VEGF not only causes endothelial-cell proliferation and permeability of vessels, but also acts with other angiogenic factors that are derived from macrophages to form patent vessels. A similar mechanism involving CXC-chemokine ligand 12 (CXCL12) signalling to CXCR4 has also been described, whereby CXCL12 was shown to guide these bone marrow progenitor cells to sites of vascular expansion in the embryo73. In addition, CXCR4 and CXCL12 were upregulated in response to hypoxia in ischaemic tissue, which resulted in the recruitment of similar myeloid cells73.
Other trophic functions
Macrophages are also involved in adipogenesis. Overexpression of CSF1 in rabbit adipose tissue increased the number of macrophages and fat mass, whereas administration of CSF1-specific antibody had the opposite effect74,75. Furthermore, Csf1op/op mice are smaller in size (as are tl rats)39,76 and have decreased fat mass, and this growth defect can be partially reversed by the administration of CSF1 (REF. 43). Interestingly, these mice completely fail to induce the formation of brown fat in the mammary gland during development because of a defect in their neuroendocrine system77.
Macrophages are also involved in the development and growth of myocytes. Specifically, they secrete growth factors and suppress the apoptosis of myocytes through cell-to-cell contact78,79. Furthermore, macrophages are recruited to the site of repair during muscle regeneration through the autocrine production of urokinase plasminogen activator, and there they stimulate the development of myocytes by producing IGF1 (REF. 80).
In addition, macrophages are crucial for erythrogenesis because they can identify ejected nuclei and degrade them. Indeed, genetic ablation of the nuclease enzyme DNase II, which is expressed by macrophages, resulted in peri-natal lethality owing to a macrophage failure to envelop and degrade the ejected nuclei of erythrocytes81, resulting in the blockage of erythrogenesis and lethal anaemia.
There are also many other deficiencies in Csf1op/op mice such as dermal atrophy that have been noted but have not yet been studied in detail, although this might simply be a reflection of the severe depletion of macrophages that normally constitute a large proportion of the cells in the skin82.
There is also evidence of a role for macrophages in the development of other organisms. For example, the ablation of macrophages in Xenopus laevis using a suicide gene approach resulted in severe developmental abnormalities, including disruption of limb morphogenesis and death at metamorphosis83.
These studies involving the in vivo depletion of macro phages or inhibition of CSF1-regulated signalling in this population indicate that macrophages have an important role in development in various species and tissues. These functional studies are also consistent with deductions made from recent transcriptional profiling assays in macrophages of mice and humans9,84. Below, I suggest that these developmental functions in matrix remodelling, epithelial proliferation and outgrowth, angio genesis and tissue organization are subverted in various pathological conditions.
Macrophages in disease
Macrophages are involved in almost every disease through their immunological and wound-healing functions. In addition, I argue that in some cases, particularly in chronic diseases such as cancer and obesity, the developmental activities of macrophages described above are dysregulated and that these activities contribute to disease pathology.
Cancer
All solid tumours recruit macrophages into their microenvironment (known as tumour-associated macrophages; TAMs). Originally it was thought that these cells were attempting to reject the immunologically `foreign' cancer; indeed, macrophages can kill tumour cells in vitro85. However, clinical and experimental evidence indicates that in most cases, macrophages promote the progression and malignancy of tumours86–88. For example, the density of TAMs in human tumours correlates with poor prognosis in more than 80% of cases89. Overexpression of CSF1 and other macrophage chemoattractants, such as CXCl2, correlates with poor prognosis in many types of cancer90–92. Experimental evidence in line with these clinical correlations comes from genetic experiments in which macrophages were removed from the polyoma middle T (PyMT) mouse model of breast cancer by crossing these mice with mice carrying the Csf1op mutation; this resulted in a delay of tumour progression and inhibition of metastasis93. This inhibition of malignancy could be reversed by the restricted transgenic expression of CSF1 by mammary tissues in Csf1op/op mice, which restored the macrophage population in the tumours93. Furthermore, overexpression of CSF1 in wild-type tumours recruited macrophages prematurely, which accelerated tumour progression and increased the metastatic potential of the tumours93. Similarly, macrophage ablation using Csf1op/op mice in a model of intestinal cancer that is caused by the APCΔ716 mutation suppressed tumour progression94. There are also several studies using tumour xenografts in which macrophage depletion decreased tumour growth86,95,96. In addition, antisense-RNA-mediated or antibody-mediated inhibition of either CSF1 or CSF1R in mice inhibited macrophage recruitment to the tumour and decreased tumour growth in human xenograft tumour models97,98. These data provide compelling evidence that tumours can direct the behaviour of macrophages from a potentially hostile antitumour phenotype to one that promotes malignancy. So, what is the precise nature and function of these tumour-promoting macrophages87?
As they become malignant, tumours acquire increased vasculature in a process known as the angiogenic switch99. This vasculature provides the sustenance and oxygen that is required for tumours to grow rapidly100. Macrophage ablation in the PyMT model of breast cancer inhibited this angiogenic switch and also decreased the density of the vasculature in malignant tumours. By contrast, the premature recruitment of macrophages into hyperplastic lesions through over-expression of CSF1 caused an angiogenic switch even in these non-malignant tumours101. Macrophages express many angiogenic molecules, including VEGF, in breast tumours of humans and mice102,103. This temporal and spatial presentation of VEGF is at least part of the tumour-promoting function of macrophages, as overexpression of VEGF in a regulated way in adenomas of Csf1op/op mice expressing the PyMT oncogene in the mammary epithelium caused extensive vascularization and accelerated tumour progression to malignancy to wild-type rates104. Furthermore, the depletion of macrophages through the inhibition of CSF1 or CSF1R in xenograft models, as described above, decreased angiogenesis, and this coincided with a decrease in the levels of VEGF97,98. Consistent with these observations, depletion of VEGF specifically in myeloid cells blocks the angiogenic switch. Paradoxically, this enhances tumour growth because the vessels have better flow characteristics in the absence of VEGF105. These data indicate that there is a complex interaction between many macrophage functions and the transition to carcinoma.
A subpopulation of mononuclear phagocytes has also been shown to be particularly angiogenic in ex vivo assays and in xenograft tumour assays. These cells express the endothelial-cell marker TIE2 receptor (also known as TEK) and are known as TIE2-expressing monocytes (TEMs). Their importance is shown by their ablation using a suicide gene approach, which blocks angiogenesis in xenografted tumours106.
Furthermore, macrophages are attracted to hypoxic areas of advanced tumours, and many chemoattractive signals have been identified92. At these sites, the hypoxia-induced transcription factor HIFα (hypoxia inducible factor α-subunit) is upregulated in macrophages, and this activates several genes, including angiogenic factors such as VEGF92. The activation of these angiogenic factors results in the revascularization of the hypoxic areas and the survival of the tumour cells that reside within them, thereby further contributing to malignancy92.
Intravital imaging of fluorescently labelled cells in mammary tumours has shown that, in most cases, tumour-cell motility occurs next to macrophages107,108. Moreover, intravasation of tumour cells also occurs next to clusters of macrophages on the vessel surface in vivo107. This concordant movement of macrophages and tumour cells depends on both cell types and requires epidermal growth factor (EGF) and CSF1 cross-signalling108, as inhibition of either pathway blocks the movement of both cell types and decreases the number of circulating cells that are derived from the tumour108. Further evidence for macrophage–tumour-cell crosstalk comes from co-culture experiments of MCF-7 breast cancer cells and macrophages, which result in enhanced invasiveness of the MCF-7 cells. This was caused by macrophage expression of WNT5A or tumour necrosis factor (TNF), which upregulated the expression of metalloproteases, the actions of which are required to remodel the extracellular matrix to facilitate tumour-cell migration109,110. In addition, by producing TNF, macrophages promote intestinal cancer, as TNF activates the WNT–β-catenin pathway, which is known to be essential for tumour progression in intestinal cells94.
In summary, macrophages promote malignancy by enhancing epithelial tumour-cell invasion and migration through the stroma and into the blood vessels and by stimulating angiogenesis, thereby increasing the number of targets for intravasating cells and supplying oxygen and nutrients. Consistent with these developmental functions, the TAM transcriptome is enriched in a set of mRNA transcripts, including angiogenic mediators, metalloproteases and growth factors, that also define embryonic macrophages111. By contrast, the expression of immune-activating transcripts is decreased, and this coincides with the upregulation of immunosuppressive transcripts112. These data suggest that the tumour environment is educating macrophages to carry out trophic functions and to adopt an M2-like macrophage phenotype (see above). In fact, macrophages that develop in the presence of growth factors such as CSF1 (REF. 21) or in response to molecules that signal through nuclear factor-κB (NF-κB)113,114 are non-immunogenic and trophic, which is consistent with a role for the cytokine environment in modulating macrophage development. It is important to point out that macrophages that are found in progressing tumours are different from those that are involved in chronic inflammatory responses to pathogens or irritants, which seem to be responsible for cancer initiation because they create a mutagenic and growth-promoting environment115,116. Instead, I think that the macrophages that are recruited to progressing tumours are functionally similar to those found in developing tissues117.
Rheumatoid arthritis
Many autoimmune diseases, including rheumatoid arthritis, involve inflammatory responses to autoantibodies that activate Fc receptors to trigger mast-cell and macrophage activation, and neutrophil invasion. This leads to an intense local inflammatory response and, if not resolved, to tissue damage over time with cycles of repair and destruction. In rheumatoid arthritis, CSF1 is produced constitutively by synovial fibroblasts and recruits tissue-infiltrating monocytes and macrophages21. In addition, locally produced CSF1, together with RANKl, induces the differentiation of monocytes to osteoclasts, which trigger bone loss40. Csf1op/op mice are resistant to collagen-induced arthritis, and CSF1 administration in wild-type mice exacerbated arthritis if administered after collagen treatment118. CSF1 also increased the severity of arthritis in a methylated albumin knee joint model that involved macrophage recruitment, and macrophage ablation inhibited disease progression21. These data show that macrophages are central to the pathogenesis of rheumatoid arthritis. Although the immune functions of macrophages are intricately involved in the initiation and propagation of this disease, it is also evident that the uncontrolled trophic and tissue-remodelling roles of macrophages are essential for much of the disease pathology. This includes the laying down of extracellular matrix, the formation of collagen fibrils and angiogenesis: macrophage functions that are similar to those seen during development21. In addition, much of the bone loss in rheumatoid arthritis can be ascribed to inappropriate and unrestrained osteoclastic function.
Lipid metabolism
Macrophages express various receptors for modified forms of lipid and they are one of the main scavengers for low-density lipoprotein. Indeed, during atherosclerosis, the continuous uptake of oxidized lipoproteins generates fat-laden macrophages in the arterial walls, which are known as foam cells21. These cells interact with endothelial cells, pericytes and platelets to form thrombi that eventually result in vascular occlusion. It is also appreciated that the build-up of lipid-filled thrombotic plaques in the arteries is a modified form of inflammation, in which monocyte-derived macrophages have a central role. Ablation of macrophages in a mouse model of atherosclerosis that is caused by a homozygous null mutation in the gene that encodes apolipoprotein E through crossing with Csf1op/op mice decreased the development of plaques, indicating the central role of macrophages in this process119. By contrast, treatment of hyperlipidaemic rabbits with CSF1 decreased atherosclerosis120. These observations suggest that macrophages have important roles in atherosclerotic disease, both during instigation and resolution.
Although these functions are clearly related to the scavenging roles of macrophages, they also indicate that macrophages have a normal physiological role in lipid metabolism. In this context an interesting story is evolving around the role of macrophages in adipogenesis and obesity. Macrophages are found in adipose tissue and are increased in obese mice and humans121. Here, they modulate angiogenesis for remodelling of the adipose tissue122. As mentioned above, the recruitment of macrophages to adipose tissue increases fat mass74, suggesting that these cells have an important developmental role in the regulation of obesity121,123. The production of monomeric tartrate-resistant acid phosphatase by macrophages stimulates fat-cell production and hyperplastic obesity (which involves the generation of many small fat cells) in a transgenic mouse model124. It is also evident that obesity causes a low-level inflammatory state that is in part responsible for insulin resistance123. Macrophages can account for this heightened inflammatory state121, as macrophage ablation reversed inflammation and insulin resistance in this model125. Therefore, overactivity of the normal developmental roles of macrophages seems to be, at least in part, responsible for the two important diseases of lipid metabolism, obesity and atherosclerosis.
Conclusions
Macrophages have important roles in the development of many and perhaps all tissues, as well as in their ongoing homeostasis. This is not an instructive role; macrophages do not change cell identity, but instead affect the regulation of rates of outgrowth, remodelling and organization of tissues. In this respect, these motile cells are well suited to this role, as they can be recruited as needed and disposed of at completion. I think that these are ancient roles of these primitive cells found in almost all metazoans and that as the immune system evolved, new functions were overlaid on these developmental and homeostatic functions, thereby exploiting the migratory, sensory and degradative properties of macrophages. This gradually led to the evolution of further subclasses, such as DCs. unfortunately, the trophic functions of these cells are dysregulated in many chronic diseases, some of which are associated with ageing, and their unrestrained activities can exacerbate pathology. Thus, a full appreciation of the developmental and tissue-maintenance roles of macrophages using methods such as temporal ablation of subpopulations of cells or macrophage-specific gene expression, will not only lead to deeper insights into macrophage biology but also allow the development of more precisely targeted anti-macrophage therapies. Some of these are in fact already being tested in clinical trials, for example, for the treatment of rheumatoid arthritis21.
Reticuloendothelial system
A classification system, the functional definition of which is based on phagocytosis, that groups macrophages and endothelial cells together.
Mononuclear phagocytic system
The current classification of macrophages, which is an ontological classification based on their bone marrow and monocyte origin.
Definitive haematopoiesis
Haematopoiesis that results in the generation of all blood cell types.
Osteopetrosis
A disease that is associated with the failure to remodel bone, resulting in occluded marrow cavities — literally, `rock-like' bones.
Growth plate
The area where osteoblasts initiate bone deposition and osteoclasts trigger bone remodelling.
Liposome-encapsulated clodronate
Clodronate (dichloromethylene bisphosphonate) that is encapsulated in liposomes and that is taken up preferentially by macrophages through phagocytosis. The clodronate then kills the macrophages.
Hypothalamic–pituitary–gonadal axis
The feedback system that regulates reproduction through the synthesis of sex steroid hormones in males and females. The highest level of control is in the hypothalamus, a region of the brain that secretes gonadotrophin-releasing hormone, which in turn stimulates the pituitary to produce gonadotrophins that act on the gonads to stimulate sex hormone synthesis.
Visual evoked potential
A neuronal response to repeated visual cues.
Retinal striate conductance
The pathway of neuronal impulses from the retina up the optic nerve to the striatum in the brain. The timing of this is a measure of neuronal conductance from a peripheral organ to the brain.
Hyaloid vessel system
A vessel system that is laid down during the development of the eye and needs to be remodelled to allow unobstructed vision.
Decidualization
The process of stromal transformation in response to an invading embryo in the uterus. The transformed stroma protects and provides sustenance to the embryo and converts into a portion of the placenta as embryonic development proceeds.
Aortic ring sprouting assay
An angiogenic assay that depends on vascular sprouting from small rings of aorta cultured ex vivo.
Brown fat
A type of fat involved in thermogenesis, so called because of the large number of mitochondria that give it its brown colour.
Polyoma middle T (PyMT) mouse model
A transgenic mouse model of breast cancer. The cancer is caused by the restricted expression of the polyoma middle T oncoprotein by mammary epithelial cells, which is under the control of the mouse mammary tumour virus promoter. This model is highly metastatic and recapitulates much of what is seen in human cancers.
Angiogenic switch
The marked increase in vascularization that is observed as benign tumours transition to malignancy.
Acknowledgements
I apologize to all authors whose work I could not cite because of space restrictions. J.W.P. is the Louis Goldstein Swan Chair in Women's Cancer Research. His research discussed in this Review is supported by National Institutes of Health grants HD30820, CA131270, CA100324 and the Cancer Center (CA P30-13,330). I thank R. Hynes, Koch Integrative Cancer Center, Massachusetts Institute of Technology, Boston, and C. Stewart, Institute of Molecular Biology, Singapore, for their hospitality towards me during my sabbatical, a period during which this article was written.
References
- 1.Tauber AI. Metchnikoff and the phagocytosis theory. Nature Rev. Mol. Cell Biol. 2003;4:897–901. doi: 10.1038/nrm1244. [DOI] [PubMed] [Google Scholar]
- 2.Kawai Y, Smedsrod B, Elvevold K, Wake K. Uptake of lithium carmine by sinusoidal endothelial and Kupffer cells of the rat liver: new insights into the classical vital staining and the reticulo-endothelial system. Cell Tissue Res. 1998;292:395–410. doi: 10.1007/s004410051069. [DOI] [PubMed] [Google Scholar]
- 3.van Furth R, et al. The mononuclear phagocyte system: a new classification of macrophages, monocytes, and their precursor cells. Bull. World Health Organ. 1972;46:845–852. [PMC free article] [PubMed] [Google Scholar]; This article formalizes the concept of the MPS.
- 4.Banchereau J, et al. Immunobiology of dendritic cells. Annu. Rev. Immunol. 2000;18:767–811. doi: 10.1146/annurev.immunol.18.1.767. [DOI] [PubMed] [Google Scholar]
- 5.Hume DA. Macrophages as APC and the dendritic cell myth. J. Immunol. 2008;181:5829–5835. doi: 10.4049/jimmunol.181.9.5829. [DOI] [PubMed] [Google Scholar]
- 6.Bailey AS, et al. Myeloid lineage progenitors give rise to vascular endothelium. Proc. Natl Acad. Sci. USA. 2006;103:13156–13161. doi: 10.1073/pnas.0604203103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hume DA. The mononuclear phagocyte system. Curr. Opin. Immunol. 2006;18:49–53. doi: 10.1016/j.coi.2005.11.008. [DOI] [PubMed] [Google Scholar]
- 8.Bertrand JY, et al. Three pathways to mature macrophages in the early mouse yolk sac. Blood. 2005;106:3004–3011. doi: 10.1182/blood-2005-02-0461. [DOI] [PubMed] [Google Scholar]
- 9.Rae F, et al. Characterisation and trophic functions of murine embryonic macrophages based upon the use of a Csf1r–EGFP transgene reporter. Dev. Biol. 2007;308:232–246. doi: 10.1016/j.ydbio.2007.05.027. [DOI] [PubMed] [Google Scholar]; This study examines the transcriptional profile of embryonic macrophages and suggests their trophic functions.
- 10.Lichanska AM, et al. Differentiation of the mononuclear phagocyte system during mouse embryogenesis: the role of transcription factor PU.1. Blood. 1999;94:127–138. [PubMed] [Google Scholar]; This paper examines the development of macrophages during embryogenesis.
- 11.Dzierzak E, Medvinsky A, de Bruijn M. Qualitative and quantitative aspects of haematopoietic cell development in the mammalian embryo. Immunol. Today. 1998;19:228–236. doi: 10.1016/s0167-5699(98)01258-4. [DOI] [PubMed] [Google Scholar]
- 12.Perry VH, Hume DA, Gordon S. Immunohistochemical localization of macrophages and microglia in the adult and developing mouse brain. Neuroscience. 1985;15:313–326. doi: 10.1016/0306-4522(85)90215-5. [DOI] [PubMed] [Google Scholar]
- 13.Sasmono RT, et al. A macrophage colony-stimulating factor receptor–green fluorescent protein transgene is expressed throughout the mononuclear phagocyte system of the mouse. Blood. 2003;101:1155–1163. doi: 10.1182/blood-2002-02-0569. [DOI] [PubMed] [Google Scholar]; This study uses a valuable reporter mouse strain for studying the mononuclear phagocytic system in development and disease.
- 14.Cecchini MG, et al. Role of colony stimulating factor-1 in the establishment and regulation of tissue macrophages during postnatal development of the mouse. Development. 1994;120:1357–1372. doi: 10.1242/dev.120.6.1357. [DOI] [PubMed] [Google Scholar]; This paper provides a detailed characterization of macrophage deficiencies in Csf1op/op mice.
- 15.Merad M, Ginhoux F, Collin M. Origin, homeostasis and function of Langerhans cells and other langerin-expressing dendritic cells. Nature Rev. Immunol. 2008;8:935–947. doi: 10.1038/nri2455. [DOI] [PubMed] [Google Scholar]
- 16.Ovchinnikov DA, et al. Expression of Gal4-dependent transgenes in cells of the mononuclear phagocyte system labeled with enhanced cyan fluorescent protein using Csf1r–Gal4VP16/UAS–ECFP double-transgenic mice. J. Leukoc. Biol. 2008;83:430–433. doi: 10.1189/jlb.0807585. [DOI] [PubMed] [Google Scholar]
- 17.Sasmono RT, et al. Mouse neutrophilic granulocytes express mRNA encoding the macrophage colony-stimulating factor receptor (CSF-1R) as well as many other macrophage-specific transcripts and can transdifferentiate into macrophages in vitro in response to CSF-1. J. Leukoc. Biol. 2007;82:111–123. doi: 10.1189/jlb.1206713. [DOI] [PubMed] [Google Scholar]
- 18.Gordon S. Alternative activation of macrophages. Nature Rev. Immunol. 2003;3:23–35. doi: 10.1038/nri978. [DOI] [PubMed] [Google Scholar]; This is a seminal review on the differences in macrophage phenotypes during immune responses.
- 19.Mantovani A, Sozzani S, Locati M, Allavena P, Sica A. Macrophage polarization: tumor-associated macrophages as a paradigm for polarized M2 mononuclear phagocytes. Trends Immunol. 2002;23:549–555. doi: 10.1016/s1471-4906(02)02302-5. [DOI] [PubMed] [Google Scholar]; The paper suggests that the M1- and M2-type classification for macrophages is applicable to those found in tumours.
- 20.Ricardo SD, van Goor H, Eddy AA. Macrophage diversity in renal injury and repair. J. Clin. Invest. 2008;118:3522–3530. doi: 10.1172/JCI36150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hamilton JA. Colony-stimulating factors in inflammation and autoimmunity. Nature Rev. Immunol. 2008;8:533–544. doi: 10.1038/nri2356. [DOI] [PubMed] [Google Scholar]
- 22.Mosser DM, Edwards JP. Exploring the full spectrum of macrophage activation. Nature Rev. Immunol. 2008;8:958–969. doi: 10.1038/nri2448. [DOI] [PMC free article] [PubMed] [Google Scholar]; This is a recent review emphasizing multiple and plastic phenotypes of macrophages, with an emphasis on wound-healing macrophages.
- 23.Chitu V, Stanley ER. Colony-stimulating factor-1 in immunity and inflammation. Curr. Opin. Immunol. 2006;18:39–48. doi: 10.1016/j.coi.2005.11.006. [DOI] [PubMed] [Google Scholar]; An important review of the action of CSF1-regulated macrophages in disease.
- 24.Fortier AH, Falk LA. Isolation of murine macrophages. Curr. Protoc Immunol. 2001;Chapter 14(Unit 14):1. doi: 10.1002/0471142735.im1401s11. [DOI] [PubMed] [Google Scholar]
- 25.Stanley E, et al. Granulocyte/macrophage colony-stimulating factor-deficient mice show no major perturbation of hematopoiesis but develop a characteristic pulmonary pathology. Proc. Natl Acad. Sci. USA. 1994;91:5592–5596. doi: 10.1073/pnas.91.12.5592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dranoff G, et al. Involvement of granulocyte-macrophage colony-stimulating factor in pulmonary homeostasis. Science. 1994;264:713–716. doi: 10.1126/science.8171324. [DOI] [PubMed] [Google Scholar]; In this study and in reference 25, the generation of a mouse lacking GM-CSF indicates that this growth factor does not have a role in the regulation of the myeloid lineage in normal physiological conditions.
- 27.Nicola NA, et al. Functional inactivation in mice of the gene for the interleukin-3 (IL-3)-specific receptor beta-chain: implications for IL-3 function and the mechanism of receptor transmodulation in hematopoietic cells. Blood. 1996;87:2665–2674. [PubMed] [Google Scholar]
- 28.Anderson KL, et al. Myeloid development is selectively disrupted in PU.1 null mice. Blood. 1998;91:3702–3710. [PubMed] [Google Scholar]
- 29.Tondravi MM, et al. Osteopetrosis in mice lacking haematopoietic transcription factor PU.1. Nature. 1997;386:81–84. doi: 10.1038/386081a0. [DOI] [PubMed] [Google Scholar]; References 28 and 29 show that the transcription factor PU.1 is important for myeloid-cell development and its absence results in osteopetrosis.
- 30.Simon MC. PU.1 and hematopoiesis: lessons learned from gene targeting experiments. Semin. Immunol. 1998;10:111–118. doi: 10.1006/smim.1998.0112. [DOI] [PubMed] [Google Scholar]
- 31.Kohyama M, et al. Role for Spi-C in the development of red pulp macrophages and splenic iron homeostasis. Nature. 2009;457:318–321. doi: 10.1038/nature07472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pollard JW, Stanley ER. Pleiotropic roles for CSF-1 in development defined by the mouse mutation osteopetrotic (op) Adv. Develop. Bioch. 1996;4:153–193. [Google Scholar]
- 33.Dai X, et al. Targeted disruption of the mouse CSF-1 receptor gene results in osteopetrosis, mononuclear phagocyte deficiency, increased primititive progenitor cell frequencies and reproductive defects. Blood. 2002;99:111–120. doi: 10.1182/blood.v99.1.111. [DOI] [PubMed] [Google Scholar]; In this paper, the phenotype of mice lacking Csf1r indicates the importance of CSF1R in regulating cells of the MPS.
- 34.Cohen PE, Zhu L, Nishimura K, Pollard JW. Colony-stimulating factor 1 regulation of neuroendocrine pathways that control gonadal function in mice. Endocrinology. 2002;143:1413–1422. doi: 10.1210/endo.143.4.8754. [DOI] [PubMed] [Google Scholar]
- 35.Lin H, et al. Discovery of a cytokine and its receptor by functional screening of the extracellular proteome. Science. 2008;320:807–811. doi: 10.1126/science.1154370. [DOI] [PubMed] [Google Scholar]
- 36.Guleria I, Pollard JW. Aberrant macrophage and neutrophil population dynamics and impaired Th1 response to Listeria monocytogenes in colony-stimulating factor 1- deficient mice. Infect. Immun. 2001;69:1795–1807. doi: 10.1128/IAI.69.3.1795-1807.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Teitelbaum R, et al. The M cell as a portal of entry to the lung for the bacterial pathogen for Mycobacterium tuberculosis. Immunity. 1999;10:641–650. doi: 10.1016/s1074-7613(00)80063-1. [DOI] [PubMed] [Google Scholar]
- 38.Wiktor-Jedrzejczak W, et al. Total absence of colony-stimulating factor 1 in the macrophage-deficient osteopetrotic (op/op) mouse. Proc. Natl Acad. Sci. USA. 1990;87:4828–4832. doi: 10.1073/pnas.87.12.4828. [DOI] [PMC free article] [PubMed] [Google Scholar]; This is the original characterization of mice lacking CSF1 because of an inactivating mutation in the Csf1 gene.
- 39.Van Wesenbeeck L, et al. The osteopetrotic mutation toothless (tl) is a loss-of-function frameshift mutation in the rat Csf1 gene: evidence of a crucial role for CSF-1 in osteoclastogenesis and endochondral ossification. Proc. Natl Acad. Sci. USA. 2002;99:14303–14308. doi: 10.1073/pnas.202332999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dougall W, et al. RANK is essential for osteoclast and lymph node development. Genes Develop. 1999;13:2412–2424. doi: 10.1101/gad.13.18.2412. [DOI] [PMC free article] [PubMed] [Google Scholar]; Discovery of the identity and function of the growth factor RANKL for the osteoclastic lineage.
- 41.Grey A, Chen Y, Paliwal I, Carlberg K, Insogna K. Evidence for a functional association between phosphatidylinositol 3- kinase and c-src in the spreading response of osteoclasts to colony- stimulating factor-1. Endocrinology. 2000;141:2129–2138. doi: 10.1210/endo.141.6.7480. [DOI] [PubMed] [Google Scholar]
- 42.Begg SK, et al. Delayed hemopoietic development in osteopetrotic (op/op) mice. J. Exp. Med. 1993;177:237–242. doi: 10.1084/jem.177.1.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wiktor-Jedrzejczak W, et al. Correction by CSF-1 of defects in the osteopetrotic op/op mouse suggests local, developmental, and humoral requirements for this growth factor. Exp. Hematol. 1991;19:1049–1054. [PubMed] [Google Scholar]
- 44.Marks SC, Jr, et al. Administration of colony stimulating factor-1 corrects some macrophage, dental, and skeletal defects in an osteopetrotic mutation (toothless, tl) in the rat. Bone. 1992;13:89–93. doi: 10.1016/8756-3282(92)90365-4. [DOI] [PubMed] [Google Scholar]
- 45.Gouon-Evans V, Rothenberg ME, Pollard JW. Postnatal mammary gland development requires macrophages and eosinophils. Development. 2000;127:2269–2282. doi: 10.1242/dev.127.11.2269. [DOI] [PubMed] [Google Scholar]
- 46.Ingman WV, Wyckoff J, Gouon-Evans V, Condeelis J, Pollard JW. Macrophages promote collagen fibrillogenesis around terminal end buds of the developing mammary gland. Dev. Dyn. 2006;235:3222–3229. doi: 10.1002/dvdy.20972. [DOI] [PubMed] [Google Scholar]
- 47.Pollard JW, Hennighausen L. Colony stimulating factor 1 is required for mammary gland development during pregnancy. Proc. Natl Acad. Sci. USA. 1994;91:9312–9316. doi: 10.1073/pnas.91.20.9312. [DOI] [PMC free article] [PubMed] [Google Scholar]; References 45 and 47 show that macrophages regulate branching morphogenesis in the mammary gland.
- 48.Nguyen AV, Pollard JW. Colony stimulating factor-1 is required to recruit macrophages into the mammary gland to facilitate mammary ductal outgrowth. Dev. Biol. 2002;247:11–25. doi: 10.1006/dbio.2002.0669. [DOI] [PubMed] [Google Scholar]
- 49.Banaei-Bouchareb L, et al. Insulin cell mass is altered in Csf1op/Csf1op macrophage-deficient mice. J. Leukoc. Biol. 2004;76:359–367. doi: 10.1189/jlb.1103591. [DOI] [PubMed] [Google Scholar]
- 50.Geutskens SB, Otonkoski T, Pulkkinen MA, Drexhage HA, Leenen PJ. Macrophages in the murine pancreas and their involvement in fetal endocrine development in vitro. J. Leukoc. Biol. 2005;78:845–852. doi: 10.1189/jlb.1004624. [DOI] [PubMed] [Google Scholar]
- 51.Cohen PE, Nishimura K, Zhu L, Pollard JW. Macrophages: important accessory cells for reproductive function. J. Leukoc. Biol. 1999;66:765–772. doi: 10.1002/jlb.66.5.765. [DOI] [PubMed] [Google Scholar]
- 52.Cohen PE, Chisholm O, Arceci RJ, Stanley ER, Pollard JW. Absence of colony stimulating factor-1 in osteopetrotic (csfmop/csfmop) mice results in male fertility defects. Biol. Reprod. 1996;55:310–317. doi: 10.1095/biolreprod55.2.310. [DOI] [PubMed] [Google Scholar]
- 53.Cohen PE, Zhu L, Pollard JW. The absence of CSF-1 in osteopetrotic (csfmop/csfmop) mice disrupts estrous cycles and ovulation. Biol. Reprod. 1997;56:110–118. doi: 10.1095/biolreprod56.1.110. [DOI] [PubMed] [Google Scholar]
- 54.Brigham DE, Little G, Lukyanenko YO, Hutson JC. Effects of clodronate-containing liposomes on testicular macrophages and Leydig cells in vitro. J. Endocrinol. 1997;155:87–92. doi: 10.1677/joe.0.1550087. [DOI] [PubMed] [Google Scholar]
- 55.Wu R, Van der Hoek KH, Ryan NK, Norman RJ, Robker RL. Macrophage contributions to ovarian function. Hum. Reprod. Update. 2004;10:119–133. doi: 10.1093/humupd/dmh011. [DOI] [PubMed] [Google Scholar]
- 56.Brännström M, Norman RJ. Involvement of leukocytes and cytokines in the ovulatory process and corpus luteum function. Human Reprod. 1993;8:1762–1775. doi: 10.1093/oxfordjournals.humrep.a137929. [DOI] [PubMed] [Google Scholar]
- 57.Cohen PE, Hardy MP, Pollard JW. Colony-stimulating factor-1 plays a major role in the development of reproductive function in male mice. Mol. Endocrinol. 1997;11:1636–1650. doi: 10.1210/mend.11.11.0009. [DOI] [PubMed] [Google Scholar]; This study shows that CSF1-regulated microglial cells help to establish the hypothalamic–pituitary–gonadal axis during development.
- 58.Michaelson MD, et al. CSF-1 deficiency in mice results in abnormal brain development. Development. 1996;122:1–12. doi: 10.1242/dev.122.9.2661. [DOI] [PubMed] [Google Scholar]; The first study to indicate that the lack of CSF1 signalling in microglial cells perturbs brain physiology.
- 59.Bulloch K, et al. CD11c/EYFP transgene illuminates a discrete network of dendritic cells within the embryonic, neonatal, adult, and injured mouse brain. J. Comp. Neurol. 2008;508:687–710. doi: 10.1002/cne.21668. [DOI] [PubMed] [Google Scholar]
- 60.Kondo Y, Lemere CA, Seabrook TJ. Osteopetrotic (op/op) mice have reduced microglia, no αβ deposition, and no changes in dopaminergic neurons. J. Neuroinflammation. 2007;4:31. doi: 10.1186/1742-2094-4-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Vilhardt F. Microglia: phagocyte and glia cell. Int. J. Biochem. Cell Biol. 2005;37:17–21. doi: 10.1016/j.biocel.2004.06.010. [DOI] [PubMed] [Google Scholar]
- 62.Rapalino O, et al. Implantation of stimulated homologous macrophages results in partial recovery of paraplegic rats. Nature Med. 1998;4:814–821. doi: 10.1038/nm0798-814. [DOI] [PubMed] [Google Scholar]
- 63.Lalancette-Hebert M, Gowing G, Simard A, Weng YC, Kriz J. Selective ablation of proliferating microglial cells exacerbates ischemic injury in the brain. J. Neurosci. 2007;27:2596–2605. doi: 10.1523/JNEUROSCI.5360-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Berezovskaya O, Maysinger D, Federoff S. The hematopoietic cytokine, colony stimulating factor 1, is also a growth factor in the CNS: congenital absence of CSF-1 in mice results in abnormal microglial response and increased neuron vulnerability to injury. Int. J. Dev. Neurosci. 1995;13:285–299. doi: 10.1016/0736-5748(95)00013-7. [DOI] [PubMed] [Google Scholar]
- 65.Gottfried-Blackmore A, Sierra A, Jellinck PH, McEwen BS, Bulloch K. Brain microglia express steroid-converting enzymes in the mouse. J. Steroid Biochem. Mol. Biol. 2008;109:96–107. doi: 10.1016/j.jsbmb.2007.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lingen MW. Role of leukocytes and endothelial cells in the development of angiogenesis in inflammation and wound healing. Arch. Pathol. Lab. Med. 2001;125:67–71. doi: 10.5858/2001-125-0067-ROLAEC. [DOI] [PubMed] [Google Scholar]
- 67.Bergmann CE, et al. Arteriogenesis depends on circulating monocytes and macrophage accumulation and is severely depressed in op/op mice. J. Leukoc. Biol. 2006;80:59–65. doi: 10.1189/jlb.0206087. [DOI] [PubMed] [Google Scholar]
- 68.Diez-Roux G, Argilla M, Makarenkova H, Ko K, Lang RA. Macrophages kill capillary cells in G1 phase of the cell cycle during programmed vascular regression. Development. 1999;126:2141–2147. doi: 10.1242/dev.126.10.2141. [DOI] [PubMed] [Google Scholar]
- 69.Lobov IB, et al. WNT7b mediates macrophage-induced programmed cell death in patterning of the vasculature. Nature. 2005;437:417–421. doi: 10.1038/nature03928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Rao S, et al. Obligatory participation of macrophages in an angiopoietin 2-mediated cell death switch. Development. 2007;134:4449–4458. doi: 10.1242/dev.012187. [DOI] [PMC free article] [PubMed] [Google Scholar]; References 69 and 70 show that macrophages are essential for vascular patterning in the eye.
- 71.Plaks V, et al. Uterine dendritic cells are crucial for decidua formation during embryo implantation. J. Clin. Invest. 2008;118:3954–3965. doi: 10.1172/JCI36682. [DOI] [PMC free article] [PubMed] [Google Scholar]; This paper identifies new functions for DCs in angiogenesis during early embryo implantation.
- 72.Grunewald M, et al. VEGF-induced adult neovascularization: recruitment, retention, and role of accessory cells. Cell. 2006;124:175–189. doi: 10.1016/j.cell.2005.10.036. [DOI] [PubMed] [Google Scholar]
- 73.Ceradini DJ, et al. Progenitor cell trafficking is regulated by hypoxic gradients through HIF-1 induction of SDF-1. Nature Med. 2004;10:858–864. doi: 10.1038/nm1075. [DOI] [PubMed] [Google Scholar]
- 74.Levine JA, Jensen MD, Eberhardt NL, O'Brien T. Adipocyte macrophage colony-stimulating factor is a mediator of adipose tissue growth. J. Clin. Invest. 1998;101:1557–1564. doi: 10.1172/JCI2293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wei S, et al. Modulation of CSF-1-regulated post-natal development with anti-CSF-1 antibody. Immunobiology. 2005;210:109–119. doi: 10.1016/j.imbio.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 76.Wiktor-Jedrzejczak W, et al. CSF-1 defeciency in the op/op mouse has differntial effects on macrophage populations and differentiation stages. Exp. Hematol. 1992;20:1004–1010. [PubMed] [Google Scholar]
- 77.Gouon-Evans V, Pollard JW. Unexpected deposition of brown fat in mammary gland during postnatal development. Mol. Endocrinol. 2002;16:2618–2627. doi: 10.1210/me.2001-0337. [DOI] [PubMed] [Google Scholar]
- 78.Sonnet C, et al. Human macrophages rescue myoblasts and myotubes from apoptosis through a set of adhesion molecular systems. J. Cell Sci. 2006;119:2497–2507. doi: 10.1242/jcs.02988. [DOI] [PubMed] [Google Scholar]
- 79.Chazaud B, et al. Satellite cells attract monocytes and use macrophages as a support to escape apoptosis and enhance muscle growth. J. Cell Biol. 2003;163:1133–1143. doi: 10.1083/jcb.200212046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bryer SC, Fantuzzi G, Van Rooijen N, Koh TJ. Urokinase-type plasminogen activator plays essential roles in macrophage chemotaxis and skeletal muscle regeneration. J. Immunol. 2008;180:1179–1188. doi: 10.4049/jimmunol.180.2.1179. [DOI] [PubMed] [Google Scholar]
- 81.Kawane K, et al. Requirement of DNase II for definitive erythropoiesis in the mouse fetal liver. Science. 2001;292:1546–1549. doi: 10.1126/science.292.5521.1546. [DOI] [PubMed] [Google Scholar]; This study identifies a new function for macrophages in erythropoiesis.
- 82.Dupasquier M, Stoitzner P, van Oudenaren A, Romani N, Leenen PJ. Macrophages and dendritic cells constitute a major subpopulation of cells in the mouse dermis. J. Invest. Dermatol. 2004;123:876–879. doi: 10.1111/j.0022-202X.2004.23427.x. [DOI] [PubMed] [Google Scholar]
- 83.Smith SJ, Kotecha S, Towers N, Mohun TJ. Targeted cell-ablation in Xenopus embryos using the conditional, toxic viral protein M2(H37A) Dev. Dyn. 2007;236:2159–2171. doi: 10.1002/dvdy.21233. [DOI] [PubMed] [Google Scholar]
- 84.Martinez FO, Gordon S, Locati M, Mantovani A. Transcriptional profiling of the human monocyte-to-macrophage differentiation and polarization: new molecules and patterns of gene expression. J. Immunol. 2006;177:7303–7311. doi: 10.4049/jimmunol.177.10.7303. [DOI] [PubMed] [Google Scholar]
- 85.Klimp AH, de Vries EG, Scherphof GL, Daemen T. A potential role of macrophage activation in the treatment of cancer. Crit. Rev. Oncol. Hematol. 2002;44:143–161. doi: 10.1016/s1040-8428(01)00203-7. [DOI] [PubMed] [Google Scholar]
- 86.Mantovani A, Bottazzi B, Colotta F, Sozzani S, Ruco L. The origin and function of tumor-associated macrophages. Immunol. Today. 1993;13:463–464. doi: 10.1016/0167-5699(92)90008-U. [DOI] [PubMed] [Google Scholar]; This is a ground-breaking review that suggests that TAMs help tumour growth.
- 87.Condeelis J, Pollard JW. Macrophages: obligate partners for tumor cell migration, invasion, and metastasis. Cell. 2006;124:263–266. doi: 10.1016/j.cell.2006.01.007. [DOI] [PubMed] [Google Scholar]
- 88.Mantovani A, Schioppa T, Porta C, Allavena P, Sica A. Role of tumor-associated macrophages in tumor progression and invasion. Cancer Metastasis Rev. 2006;25:315–322. doi: 10.1007/s10555-006-9001-7. [DOI] [PubMed] [Google Scholar]
- 89.Bingle L, Brown NJ, Lewis CE. The role of tumour-associated macrophages in tumour progression: implications for new anticancer therapies. J. Pathol. 2002;196:254–265. doi: 10.1002/path.1027. [DOI] [PubMed] [Google Scholar]
- 90.Lin EY, Gouon-Evans V, Nguyen AV, Pollard JW. The macrophage growth factor, CSF-1, in mammary gland development and tumor progression. J. Mammary Gland Biol. Neoplasia. 2002;7:147–162. doi: 10.1023/a:1020399802795. [DOI] [PubMed] [Google Scholar]
- 91.Scholl SM, et al. Anti-colony-stimulating factor-1 antibody staining in primary breast adenocarcinomas correlates with marked inflammatory cell infiltrates and prognosis. J. Natl Cancer Inst. 1994;86:120–126. doi: 10.1093/jnci/86.2.120. [DOI] [PubMed] [Google Scholar]
- 92.Murdoch C, Muthana M, Coffelt SB, Lewis CE. The role of myeloid cells in the promotion of tumour angiogenesis. Nature Rev. Cancer. 2008;8:618–631. doi: 10.1038/nrc2444. [DOI] [PubMed] [Google Scholar]
- 93.Lin EY, Nguyen AV, Russell RG, Pollard JW. Colony-stimulating factor 1 promotes progression of mammary tumors to malignancy. J. Exp. Med. 2001;193:727–740. doi: 10.1084/jem.193.6.727. [DOI] [PMC free article] [PubMed] [Google Scholar]; This paper shows that macrophages have an important role in promoting tumour progression and metastasis.
- 94.Oguma K, et al. Activated macrophages promote Wnt signalling through tumour necrosis factor-α in gastric tumour cells. EMBO J. 2008;27:1671–1681. doi: 10.1038/emboj.2008.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Kimura YN, et al. Inflammatory stimuli from macrophages and cancer cells synergistically promote tumor growth and angiogenesis. Cancer Sci. 2007;98:2009–2018. doi: 10.1111/j.1349-7006.2007.00633.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Gazzaniga S, et al. Targeting tumor-associated macrophages and inhibition of MCP-1 reduce angiogenesis and tumor growth in a human melanoma xenograft. J. Invest. Dermatol. 2007;127:2031–2041. doi: 10.1038/sj.jid.5700827. [DOI] [PubMed] [Google Scholar]
- 97.Aharinejad S, et al. Colony-stimulating factor-1 blockade by antisense oligonucleotides and small interfering RNAs suppresses growth of human mammary tumor xenografts in mice. Cancer Res. 2004;64:5378–5384. doi: 10.1158/0008-5472.CAN-04-0961. [DOI] [PubMed] [Google Scholar]
- 98.Paulus P, Stanley ER, Schafer R, Abraham D, Aharinejad S. Colony-stimulating factor-1 antibody reverses chemoresistance in human MCF-7 breast cancer xenografts. Cancer Res. 2006;66:4349–4356. doi: 10.1158/0008-5472.CAN-05-3523. [DOI] [PubMed] [Google Scholar]
- 99.Hanahan D, Folkman J. Patterns and emerging mechanisms of the angiogenic switch during tumorigenesis. Cell. 1996;86:353–364. doi: 10.1016/s0092-8674(00)80108-7. [DOI] [PubMed] [Google Scholar]
- 100.Folkman J. Role of angiogenesis in tumor growth and metastasis. Semin. Oncol. 2002;29:15–18. doi: 10.1053/sonc.2002.37263. [DOI] [PubMed] [Google Scholar]
- 101.Lin EY, Pollard JW. Tumor-associated macrophages press the angiogenic switch in breast cancer. Cancer Res. 2007;67:5064–5066. doi: 10.1158/0008-5472.CAN-07-0912. [DOI] [PubMed] [Google Scholar]
- 102.Leek RD, Harris AL. Tumor-associated macrophages in breast cancer. J. Mammary Gland. Biol. Neoplasia. 2002;7:177–189. doi: 10.1023/a:1020304003704. [DOI] [PubMed] [Google Scholar]
- 103.Lin EY, et al. Macrophages regulate the angiogenic switch in a mouse model of breast cancer. Cancer Res. 2006;66:11238–11246. doi: 10.1158/0008-5472.CAN-06-1278. [DOI] [PubMed] [Google Scholar]
- 104.Lin EY, et al. Vascular endothelial growth factor restores delayed tumor progression in tumors depleted of macrophages. Mol. Oncol. 2007;1:288–302. doi: 10.1016/j.molonc.2007.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Stockmann C, et al. Deletion of vascular endothelial growth factor in myeloid cells accelerates tumorigenesis. Nature. 2008;456:814–818. doi: 10.1038/nature07445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.De Palma M, Murdoch C, Venneri MA, Naldini L, Lewis CE. Tie2-expressing monocytes: regulation of tumor angiogenesis and therapeutic implications. Trends Immunol. 2007;28:519–524. doi: 10.1016/j.it.2007.09.004. [DOI] [PubMed] [Google Scholar]
- 107.Wyckoff JB, et al. Direct visualization of macrophage-assisted tumor cell intravasation in mammary tumors. Cancer Res. 2007;67:2649–2656. doi: 10.1158/0008-5472.CAN-06-1823. [DOI] [PubMed] [Google Scholar]
- 108.Wyckoff J, et al. A paracrine loop between tumor cells and macrophages is required for tumor cell migration in mammary tumors. Cancer Res. 2004;64:7022–7029. doi: 10.1158/0008-5472.CAN-04-1449. [DOI] [PubMed] [Google Scholar]
- 109.Pukrop T, et al. Wnt 5a signaling is critical for macrophage-induced invasion of breast cancer cell lines. Proc. Natl Acad. Sci. USA. 2006;103:5454–5459. doi: 10.1073/pnas.0509703103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Hagemann T, et al. Macrophages induce invasiveness of epithelial cancer cells via NF-κB and JNK. J. Immunol. 2005;175:1197–1205. doi: 10.4049/jimmunol.175.2.1197. [DOI] [PubMed] [Google Scholar]
- 111.Ojalvo LS, King W, Cox D, Pollard JW. High density gene expression analysis of tumor associated macrophages from mouse mammary tumors. Am. J. Pathol. 2009;174:1048–1064. doi: 10.2353/ajpath.2009.080676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Biswas SK, et al. A distinct and unique transcriptional program expressed by tumor-associated macrophages (defective NF-κB and enhanced IRF-3/STAT1 activation) Blood. 2006;107:2112–2122. doi: 10.1182/blood-2005-01-0428. [DOI] [PubMed] [Google Scholar]
- 113.Hagemann T, Biswas SK, Lawrence T, Sica A, Lewis CE. Regulation of macrophage function in tumors: the multifaceted role of NF-κB. Blood. 2009 Jan 26; doi: 10.1182/blood-2008-12-172825. doi:10.1182/blood-2008-12-172825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Hagemann T, et al. “Re-educating” tumor-associated macrophages by targeting NF-κB. J. Exp. Med. 2008;205:1261–1268. doi: 10.1084/jem.20080108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Balkwill F, Charles KA, Mantovani A. Smoldering and polarized inflammation in the initiation and promotion of malignant disease. Cancer Cell. 2005;7:211–217. doi: 10.1016/j.ccr.2005.02.013. [DOI] [PubMed] [Google Scholar]
- 116.Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420:860–867. doi: 10.1038/nature01322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Gouon-Evans V, Lin EY, Pollard JW. Requirement of macrophages and eosinophils and their cytokines/chemokines for mammary gland development. Breast Cancer Res. 2002;4:155–164. doi: 10.1186/bcr441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Campbell IK, Rich MJ, Bischof RJ, Hamilton JA. The colony-stimulating factors and collagen-induced arthritis: exacerbation of disease by M-CSF and G-CSF and requirement for endogenous M-CSF. J. Leukoc. Biol. 2000;68:144–150. [PubMed] [Google Scholar]
- 119.Babamusta F, et al. Angiotensin II infusion induces site-specific intra-laminar hemorrhage in macrophage colony-stimulating factor-deficient mice. Atherosclerosis. 2006;186:282–290. doi: 10.1016/j.atherosclerosis.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 120.Motoyoshi K. Biological activities and clinical application of M-CSF. Int. J. Hematol. 1998;67:109–122. doi: 10.1016/s0925-5710(98)00010-3. [DOI] [PubMed] [Google Scholar]
- 121.Weisberg SP, et al. Obesity is associated with macrophage accumulation in adipose tissue. J. Clin. Invest. 2003;112:1796–1808. doi: 10.1172/JCI19246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Pang C, et al. Macrophage infiltration into adipose tissue may promote angiogenesis for adipose tissue remodeling in obesity. Am. J. Physiol. Endocrinol. Metab. 2008;295:E313–E322. doi: 10.1152/ajpendo.90296.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Xu H, et al. Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. J. Clin. Invest. 2003;112:1821–1830. doi: 10.1172/JCI19451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Lang P, et al. Monomeric tartrate resistant acid phosphatase induces insulin sensitive obesity. PLoS ONE. 2008;3:e1713. doi: 10.1371/journal.pone.0001713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Patsouris D, et al. Ablation of CD11c-positive cells normalizes insulin sensitivity in obese insulin resistant animals. Cell. Metab. 2008;8:301–309. doi: 10.1016/j.cmet.2008.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]; Reference 121 and 125 link macrophages with obesity and insulin insensitivity.
- 126.Varol C, Yona S, Jung S. Origins and tissue-context-dependent fates of blood monocytes. Immunol. Cell Biol. 2009;87:30–38. doi: 10.1038/icb.2008.90. [DOI] [PubMed] [Google Scholar]