Abstract
The current analysis considers the HIV prevention research record in the social sciences. We do so with special reference to what has been termed “AIDS Exceptionalism”— departures from standard public health practice and prevention research priorities in favor of alternative approaches to prevention that, it has been argued, emphasize individual rights at the expense of public health protection. In considering this issue, we review the historical context of the HIV epidemic; empirically demonstrate a pattern of prevention research characterized by systematic neglect of prevention interventions for HIV-infected persons; and articulate a rationale for “Prevention for Positives,” supportive prevention efforts tailored to the needs of HIV+ individuals. We then propose a social psychological conceptualization of processes that appear to have influenced developments in HIV prevention research and directed its focus to particular target populations. Our concluding section considers whether there are social and research policy lessons to be learned from the record of HIV prevention research that might improve our ability to addresses effectively, equitably, and in timely fashion future epidemics that play out, as HIV does, at the junction of biology and behavior.
At the first quarter century of the AIDS epidemic, it is important to weigh our accomplishments against our failures in the fight against AIDS…Future historians will conclude that we cannot escape responsibility for our failure to use effective, scientifically proven strategies to control the AIDS epidemic…They will also likely regard as tragic those instances when we allowed scarce resources to be used to support ideologically driven “prevention” that only served a particular political agenda.
Editorial: A Quarter Century of AIDS. American Journal of Public Health. (Stall & Mills, 2006, p. 961)
Social, clinical, and health psychologists and allied social scientists responded to the HIV epidemic rapidly, in considerable numbers, and very often effectively, crafting, evaluating, and disseminating theory- and research-based HIV prevention interventions from the early 1980s onwards. (For early contributions to HIV prevention efforts see Coates, Morin, & McKusick, 1987; De Jarlais & Friedman, 1988; Kelley and St. Lawrence, 1986;, and the American Psychologist, 1988, special issue on AIDS). As we reflect on the record of HIV prevention research in the social sciences, however, we are struck by an interesting and important fact. For the first two decades of the HIV epidemic, social scientists conducting HIV prevention research focused on the promotion of preventive behavior among members of the general public and members of so-called “high risk groups,” without reference to the HIV− or HIV+ status of target populations. (See systematic reviews of HIV prevention research since the inception of the epidemic by Albarracin et al., 2005; W. Johnson et al., 2002; Noar, 2008; and Semaan et al., 2002). Correspondingly, for the first two decades of the HIV epidemic, social scientists directed exceedingly little attention to creating and evaluating HIV prevention interventions specifically designed to address the prevention needs of HIV+ individuals who were capable of communicating infection to others. (See systematic reviews of research concerning HIV prevention for HIV+ individuals by B. Johnson, Carey, Chaudoir, and Reid, 2006, and Crepaz, Lyles, Wolitski, Passin, Rama et al., 2006).
The current discussion reviews the HIV prevention research record in the social sciences. We do so with special reference to what has been termed “AIDS Exceptionalism” — departures from standard public health practice and prevention research priorities in favor of alternative approaches to prevention that, it has been argued, emphasize individual rights at the expense of public health protection. In considering this issue, we review the historical context of the HIV epidemic; empirically demonstrate a pattern of prevention research characterized by absence of prevention interventions for HIV-infected persons; and articulate a rationale for “Prevention for Positives,” supportive prevention efforts tailored to the needs of HIV+ individuals. We then propose a social psychological conceptualization of processes that appear to have influenced developments in HIV prevention research and directed its focus to particular target populations. Our concluding section considers whether there are social and research policy lessons to be learned from the record of HIV prevention research that might improve our ability to addresses effectively, equitably, and in timely fashion future epidemics that play out, as HIV does, at the junction of biology and behavior.
The Context: A Brief History of the HIV Epidemic
A number of individuals involved in early efforts to track the AIDS epidemic, treat the first patients, and establish programs of prevention, have provided accounts of the development of the epidemic from the silent spread of HIV, the virus that causes AIDS, to the visible appearance of the AIDS epidemic in the 1980s, to the current status of the AIDS pandemic (e.g., Bayer & Oppenheim, 2000; Darrow, 2004; Gottlieb, 2001; Mann & Tarantola, 1996; Sepkowitz, 2001; see also the National Institute of Health, 2008, AIDS history website).
The “silent spread” of HIV has been identified retrospectively as the initial stage of the AIDS epidemic (Darrow, 2004). According to research by Hahn and colleagues (Hahn, Shaw, De Cock, and Sharp, 2000), simian immunodeficiency virus is the probable source of HIV and appears to have crossed from primates to humans in west and central Africa on multiple occasions between 1910 and 1950 (Korber, Muldoon, Theiler, et al., 2000). Retrospective research has detected evidence of HIV-like virus infection in human beings in central Africa as early as 1959 (Nahmias, Weiss, Yao et al., 1986), and the virus appears to have spread, possibly via Haiti, to North America (Chin, 2007). Widespread behaviorally driven infection among men who have sex with men and injection drug users in developed nations is thought to have begun in the 1970s (Chin, 2007).
The AIDS epidemic began to become visible on June 15, 1981, with the publication of a brief article in Morbidity and Mortality Weekly Report (1981) concerning unusual opportunistic infections among five homosexual men in Los Angeles. By September, 1982, the Centers for Disease Control and Prevention had identified the disease as “acquired immunodeficiency syndrome” and labeled it with the acronym “AIDS,” and researchers speculated vigorously about the etiologic agent or agents that might be implicated. Some thought AIDS was caused by cytomegalovirus, as AIDS patients had high rates of infection with this pathogen; others thought that the nitrate inhalants popular among gay men might be responsible, and still others thought that repeated exposure to another’s sperm was triggering an immune system collapse (Sepkowitz, 2001).
Biomedical discoveries, though seeming slow at the time, actually occurred at a rapid pace after recognition of AIDS as a clinical entity and initial epidemiologic description of the distribution of the disease. Watershed events in the AIDS epidemic in the mid-1980s included the identification of HIV as the pathogen responsible for AIDS by Dr. Robert Gallo and Dr. Luc Montagnier in 1984 (National Institutes of Health, 2008). Development, approval, and commercial availability of a blood test to identify antibodies to HIV that indicate infection with the virus was achieved by 1985 (Sepkowitz, 2001). Additional critical events early in the AIDS epidemic included the first reports, in 1983, of the infection of female partners of men with AIDS (National Institutes of Health, 2008) and advances in epidemiology that began to clarify the incidence, prevalence, and differing patterns of HIV infection worldwide (Mann, Tarantola, & Netter, 1992). The mid-1980s also saw development of a drug, AZT, that proved capable of effectively preventing maternal—fetal transmission of HIV (Bayer & Oppenheimer, 2000). AZT also seemed to be a promising treatment for AIDS, but the drug eventually failed to be effective, leading to great disappointment (Bayer & Oppenheimer, 2000). Another significant discovery in this era, of considerable relevance to HIV prevention and to fears of casual contagion, involved the finding that in couples in which one partner had HIV and the other did not, HIV transmission to the uninfected partner rarely took place if the couple was using condoms for birth control, despite all manner of other casual contact between them (Fischl et al., 1987).
During the first decade of the visible epidemic, AIDS deaths occurred at a terrible rate (Bayer & Oppenheimer, 2000; Centers for Disease Control and Prevention, 2001; Karon, Fleming, Steketee & De Cock, 2001). No effective treatment for AIDS was available (Sepkowitz, 2001); physicians were trapped in what has been termed an era of “therapeutic impotence” (Bayer & Oppenheimer, 2000), and affected communities such as homosexual men on both US coasts were decimated (Shilts, 1987). Characteristics that included homosexual orientation, intravenous drug use, poverty, racism, and fear of contagion led to stigma and rejection of people with AIDS and institutional isolation of the health care providers who were struggling to treat them. (See Herek & Capitano, 1999, for discussion of AIDS stigma; Crawford, 1996, for discussion of AIDS stigma compared to stigma of other medical conditions; and Bayer & Oppenheimer, for discussion of the marginalization of AIDS physicians). AIDS self-help groups emerged as important sources of support for people with AIDS and the health professionals who cared for them during an era of enormous prejudice and rejection (Bay Area Physicians for Human Rights, 2008; God’s Love We Deliver, 2008). AIDS activism, occasionally adopting direct action tactics of the civil-rights and Vietnam-era antiwar movements, exerted influence on the US government and on the pharmaceutical industry to provide care and to facilitate drug approval, testing, and availability (See, for example, Gay Men’s Health Crisis, 2008, and ACT Up, the AIDS Coalition to Unleash Power, 2008). Frustration with foundational methods such as placebo controlled drug trials, quite understandable in the face of a relentless and fatal illness, was expressed by a number of individuals and organizations (Sepkowitz, 2001).
Historians of the AIDS epidemic in the 1980s note that extreme views were not uncommon during this difficult time (Bayer & Oppenheimer, 2000; Darrow, 2004). Some feared that members of so-called “high risk groups” (homosexuals, intravenous drug users, and of course, people with AIDS) would be sent to concentration camps, and others demanded that children with AIDS be forbidden from attending school. At least one AIDS activist of the 1980s was quoted as saying that “Nobody’s listened to us. What we need is a few assassinations” (Bayer & Oppenheimer, 2000, p. 139). AIDS care physicians of this era, it has also been noted, appear to have been a highly self-selected group. Bayer and Oppenheimer’s (2000) sizable social history sample of AIDS doctors active during the first decade of the epidemic was young and white; nearly half were Jewish; 40% were gay or lesbian; and 30% were women. Although systematic data are not available concerning characteristics of HIV prevention researchers in the social sciences during this time, anecdotal observations support the view that they were self-selected as well on the basis of empathy, tolerance, and liberal values. Social science researchers in this area are also able to recount more than a few war stories of their own institutional rejection and isolation.
Attitudes towards HIV testing, which became available in the mid-1980s, remained ambivalent among some individuals and organizations during the first decade of the epidemic (Bayer, 1989). On one hand, reluctance to undergo or to advocate HIV testing can be seen as entirely understandable in an era of virtually guaranteed stigma and social exclusion for persons living with HIV (Bayer, 1989; Crawford, 1996; Herek & Capitano, 1999). Moreover, with no effective treatment available, testing positive for HIV represented a personal catastrophe and the certainty of impending death (Bayer, 1989). On the other hand, reluctance to undergo or to advocate HIV testing may have eliminated for some the possibility of recognizing one’s status as an infectious individual with the definitive need to practice prevention to avoid infecting others. It is also the case, however, that an individual could practice prevention consistently and proactively without any knowledge of his or her HIV status, and many did exactly this. Also understandable in an era of “therapeutic impotence” and near-certain mortality from HIV infection, American AIDS policy in the 1980s was built on a medical model that focused primarily on the search for effective therapies and on development of an HIV vaccine (Darrow, 2004). Although US Department of Health and Human Services Secretary Margaret Heckler promised in 1985 that an HIV vaccine would be developed within the coming two years, this has not yet occurred a full quarter-century later. (See International AIDS Vaccine Initiative, 2008 for information concerning vaccine progress).
Alongside developments in the US AIDS epidemic, a global mobilization against the disease took shape during the 1980s and intensified over time, involving international efforts to characterize the epidemiology of AIDS and to promote prevention worldwide. Project SIDA, an early example of international efforts to address AIDS on the African continent, was established in Zaire in 1983 by the US National Institute of Allergy and Infectious Disease, the Centers for Disease Control and Prevention, the Belgian Institute for Tropical Medicine, and the Zaire Ministry of Health,. The UN World Health Organization established the Global Program on AIDS in 1986, which was succeeded in 1996 by the United Nations Joint Program on HIV and AIDS. The International AIDS Conference, which brought together biomedical and behavioral scientists from around the world, held its first meeting in Atlanta in 1985, and has continued to meet every two years since. The International AIDS Conference held in 1996 in Vancouver welcomed announcement of the success of antiretroviral therapies that slowed or stopped viral replication and dramatically changed HIV infection from a nearly always fatal disease into a manageable chronic condition. Strategic positioning of the International AIDS Conference in Durban, South Africa in 2000 focused world attention on the African AIDS epidemic and accelerated recognition of the sub-Saharan AIDS crisis and access to HIV testing and antiretroviral therapy in that region. The AIDS Impact Conference, which provides a complementary forum for social and behavioral science efforts to fight HIV/AIDS, will soon have its own ninth gathering in Botswana. Another recent and economically massive contribution to global mobilization in the fight against AIDS involves the US President’s Emergency Plan for AIDS Relief, which in 2008 committed $39 billion dollars to international efforts in HIV/AIDS related research, prevention, and care, with a portion of this funding going to the fight against malaria and tuberculosis as well (President’s Emergency Plan for AIDS Relief, 2008). The Gates and Clinton Foundations have also contributed substantially and specifically to the global fight against HIV/AIDS.
The current state of the global HIV/AIDS epidemic is defined by the availability (or unavailability) of antiretroviral therapy, and differential patterns of infection among men who have sex with men, intravenous drug users, and heterosexual individuals (in the West) and among heterosexual individuals and via perinatal transmission (in Africa and the developing world). The spread of HIV infection into relatively newer geographical areas including China, India, and the former Soviet Union is also being watched closely as the HIV epidemic concludes its third decade. According to recent estimates (UNAIDS, 2008a), there are some 33 million adults and children living with HIV/AIDS worldwide, with major centers of the epidemic in North America (1.3 million people living with HIV/AIDS), Latin America (1.6 million infected persons), South and Southeast Asia (4.0 million), and sub-Saharan Africa (22.5 million). Some 2.7 million new HIV infections are occurring annually. The number of persons presently living with HIV/AIDS worldwide is increasing as a function of newly occurring HIV infections together with decreases in AIDS mortality due to the success of antiretroviral therapy in halting the progression from HIV infection to AIDS (UNAIDS, 2008a). Given the prevalence of HIV and the uneven availability of antiretroviral therapy worldwide, however, it is the case that some 2.1 million adults and children died of HIV/AIDS in 2007 (UNAIDS, 2008a).
Of considerable significance to the current discussion of HIV prevention, we note that between 2.7 and 3.0 million new HIV infections worldwide have occurred annually over the past five years (UNAIDS, 2008b). New HIV infections in the US – some 56,000 per year – have also been occurring at a relatively stable and unchanging rate from 2000 to the present (Hall, Song, Rhodeset al., 2008; CDC 2008a). The proportion of HIV+ individuals in the US who are aware of their HIV status has increased to approximately 79% of all HIV infected persons, and there are currently some 1,106,400 persons living with HIV/AIDS in the US (CDC, 2008b).
It is important to note that social and behavioral scientists have been heavily involved in responding to each stage of the HIV epidemic. The influence of social and behavioral science and science-based advocacy was impactful, if indirectly so, during the silent spread of HIV over the decades of the 1960s and 1970s, and its influence has been both direct and impactful during later stages of the epidemic.
Among the contributions of social and behavioral scientists during the era of the silent spread of HIV were research and advocacy that helped depathologize and destigmatize homosexuality, an enormously and entirely welcome and scientifically well-justified development. At the same time, such progress may have indirectly contributed to a coming out process that included opportunities for sexual expression in a biobehavioral context that was in retrospect an exceedingly efficient one for HIV transmission. (For a broad discussion of sexual orientation, see Hyde, DeLamater, and Byers, 2001; for a review of research on sexual orientation and mental health, see Meyer, 2003, and for discussion of sexual activity in the gay male community in the context of gay liberation in the 1970s, see Shilts, 1987). Significantly as well, theoretical and empirical work in social and health psychology that preceded the HIV epidemic—including work on the Theory of Reasoned Action (Fishbein & Ajzen, 1975; Fishbein & Middlestadt, 1989; see also Albarracin, Johnson, Fishbein et al., 2001), the Theory of Planned Behavior (Ajzen, 1985; see also Albarracin, Johnson, Fishbein et al., 2001), Social—Cognitive Theory (Bandura, 1986, 1989), the Transtheoretical Model (Prochaska & DiClemente, 1983; Catania, Kegeles, & Coates, 1990), and social influence and reference group theory (J. Fisher, 1988; Kelly et al., 1991) – has been very broadly and effectively applied to HIV prevention efforts across the epidemic. Other contributions of behavioral science taking place prior to the visible HIV epidemic, and later applied directly and widely to HIV prevention efforts, involved research undertaken during the 1970s aimed at understanding and promoting contraceptive behavior, including condom use (e.g., Byrne & Fisher, 1983; Jaccard & Davidson, 1972).
Later stages of the HIV epidemic have seen the application of theoretically- and empirically-based HIV prevention intervention research, originally conducted in North America and other developed nations, in low-resource AIDS pandemic countries. Within the framework of the President’s Emergency Plan for AIDS Relief, for example, theory-based AIDS prevention interventions are being deployed in multiple locations in Africa, including Mozambique, Uganda, and Ethiopia (President’s Emergency Plan for AIDS Relief, 2008; D. Cornman, personal communication, November 8, 2008). Current HIV prevention efforts in the West feature vigorous efforts to disseminate and apply approaches to HIV prevention that have been empirically validated (see, for example, the Center for Disease Control and Prevention’s Compendium of HIV Prevention Interventions with Evidence of Effectiveness 2008d, 2008e, 2009a, 2009b); focus on adherence to antiretroviral therapy and psychological interventions to promote adherence (e.g., Bangsberg, Perry, Charlebois et al., 2001; Chesney, 2000; J. Fisher, Fisher, Amico, & Harman, 2006); and work on HIV prevention interventions that address and support the prevention needs of persons living with HIV (see, for example, individual studies by J. Fisher, Fisher, Cornman, Amico, Bryan, & Friedland, 2006 and Kalichman, Rompa, Cage, DiFonzo, Simpson, et al. 2001, and meta-analytic reviews of this literature by B. Johnson, Carey, Chaudoir, and Reid, 2006, and Crepaz, Lyles, Wolitski, Passin, Rama et al., 2006 ).
With some sense of the historical context of the HIV epidemic, then—including the profound stigma attached to HIV early in the epidemic and the transition of HIV from fatal disease to chronic condition—we turn to discussion of HIV exceptionalism in public health practice and research policy.
HIV Exceptionalism: Public Health Policy and Efforts to Contain the HIV Pandemic
Although human immunodeficiency virus (HIV) infection has killed more than half a million people in the United States, a comprehensive public health approach that has stopped other epidemics has not been used to address this one. When HIV infection first emerged among stigmatized populations (homosexual men, injection-drug users and immigrants from developing countries), the discriminatory responses ranged from descriptions of AIDS as “retribution” to violence and proposals for quarantine, universal mandatory testing, and even tattooing of infected persons. This response led to HIV exceptionalism, an approach that advocated both for special resources and increased funding and against the application of standard methods of disease control. The need for extra resources remains essential, but the failure to apply standard disease-control methods undermines society’s ability and responsibility to control the epidemic.
Sounding Board, New England Journal of Medicine (Frieden, Das-Douglas, Kellerman, & Henning, 2005, p. 2397)
We now consider the controversial topic of HIV exceptionalism, or departures from standard public health practice and prevention research priorities in favor of approaches to prevention that, it is argued, emphasize individual rights at the expense of public health priorities (Bayer, 1989, 1991; Bayer & Fairchild, 2006; Frieden et al., 2005; Stall & Mills, 2006). The assertion that HIV exceptionalism characterized prevention research and practice across the epidemic and had unintended but significant negative effects on individual and public health is reviewed in the discussion that follows.
Standard public health practice for containing sexually transmitted infection places very high priority on the identification of infected individuals, via screening and testing, and notification of partners of infected individuals, so that they may seek testing themselves. In this fashion, affected individuals may become aware of their status and act to avoid transmitting infection to others (Aral, Douglas &, Lipshutz, 2007; Bayer, 1991; Frieden et al., 2005). Another absolutely standard public health practice in containing sexually transmitted infection—rapid and effective treatment of infected individuals and their contacts—was not an option for HIV infected persons until relatively late in the epidemic. At the same time, however, identification of infected individuals and their partners can provide opportunity and motivation, even in a context lacking treatment or cure, for the practice of preventive behavior and avoidance of transmission to uninfected others. Preventive behavior can also help HIV+ individuals avoid contracting other pathogens themselves through risky sexual behavior or intravenous drug use and further compromising their health. We note that meta-analytic evidence (Marks, Crepaz, Senterfitt, & Janssen, 2005) indicates that individuals who become aware of their HIV infected status dramatically decrease their HIV transmission risk behavior. An alternative open to all individuals, of course, is the preemptive practice of prevention (which was a centerpiece of HIV prevention efforts throughout the epidemic) without the necessity for HIV testing or learning one’s HIV status
Discussions of HIV exceptionalism suggest that, in an epidemic context that was the embodiment of prejudice and stigmatization of those with HIV/AIDS, more weight was accorded to protection of individual privacy and individual rights than to protection of public health (see Bayer, 1989, 1991; Frieden et al., 2005). Ambivalence and outright resistance to HIV testing that was expressed early in the epidemic by some activists, some members of “at risk” groups, and some public health personnel (Bayer, 1989, 1991). Legitimate fears about violation of privacy, limitation of individual rights, and further stigmatization of already marginalized groups also provided an understandable basis for ambivalence about contact tracing, the closing of venues such as bathhouses associated with high risk behavior, and similar public health approaches, particularly at earlier points in the HIV epidemic. Moreover, fear of “driving the disease underground” and recognition of the absolute need for voluntary and widespread testing and behavior change among large numbers of people combined to provide a rational basis for approaching HIV differently than had been the case in other epidemic situations. Accordingly, approaches to prevention developed that involved strictly voluntary HIV testing following mandatory and detailed informed consent procedures, hesitancy about nominal reporting of infected individuals, reluctance to close venues associated with risky sexual behavior, and inconsistencies in the practice of partner notification (Bayer, 1989, 1991).
While approaches to HIV control during the first decade of the epidemic have been referred to as exceptional, they could also be seen as adaptive responses to an epidemic that was itself entirely novel in character. Some argue, however, that the disease containment efficiency of nonexceptional implementation of standard public health practices—including very widespread testing and screening, focused and supportive safer sex counseling of those infected, and partner notification—would have been significant and could have averted considerable infection and mortality (e.g., Frieden et al., 2005). Others, as noted, regard the development of exceptional public health efforts to contain HIV as at least an understandable response to the social, political, and biological situation on the ground at the time (see Bayer, 1989, Private acts, social consequences. AIDS and the politics of public health, for comprehensive discussion of the tensions that occured in relation to balancing individual rights with public health during the first decade of the HIV epidemic).
The history of what has been referred to as “HIV exceptionalism” in public health efforts to contain the epidemic, like the history of the epidemic itself, has been described as involving a sequence of eras, including the emergence of exceptionalism (1981–1985), the consolidation and consistent practice of exceptionalism (1986–1991), the crumbling of hegemonic exceptionalism (1991–1996), and the move to normalization of public health approaches to HIV (1996-present; Rosenbrock et al., 2000). Advocates of normalization in HIV prevention have asserted that HIV exceptionalism, based upon very understandable concerns about marginalization and the violation of individual liberties, has lost its legitimacy in the era of effective treatment for HIV infection, since failure to identify HIV infected individuals though routine screening eliminates access to effective treatment for those infected as well as posing a public health challenge (Bayer, 1991; Bayer & Fairchild, 2006; Frieden et al., 2005).
HIV Exceptionalism in Prevention Research in the Social Sciences
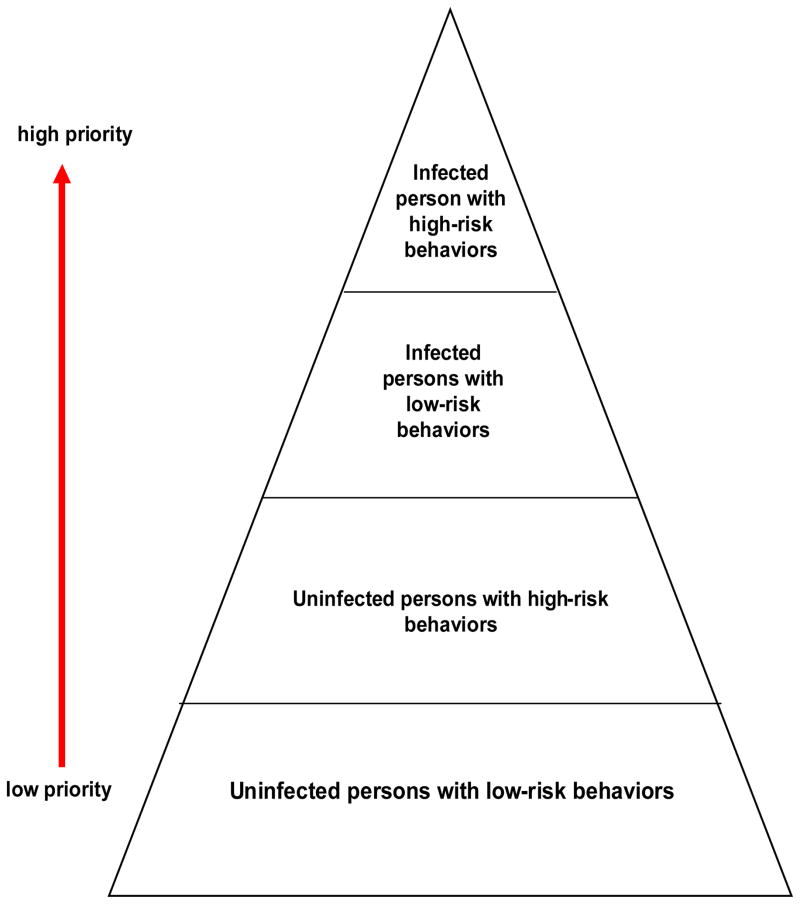
In addition to discussion of HIV exceptionalism in public health practice, the current analysis addresses the possibility that HIV exceptionalism has characterized HIV prevention research in the social sciences. Specifically, we note that the textbook approach to prevention of sexually transmitted disease would place prevention interventions for HIV infected individuals as the very highest priority (Aral, Lipshutz, & Douglas, 2007; Janssen, Holtgrave, Valdiserri, Shepherd, Gayle, & DeCock, 2001; Slater, 1994; see Figure 1). HIV prevention research in the social sciences, however, historically focused on the development, implementation, and evaluation of HIV prevention interventions without specific focus on the prevention needs of HIV+ individuals. It is the case that hundreds of single studies and well over a dozen meta-analytic reviews of HIV prevention interventions, directed at populations selected for characteristics other than HIV infection status, have been published over the course of the epidemic (Albarracin, Gillette, Earl, Glasman, Durantini, & Ho, 2005; Johnson, Hedges, Ramirez, Semaan, Norman et al., 2002; Noar, 2008; Semaan, Kay, Strouse, Sogolow, Mullen et al., 2002) In contrast, HIV prevention intervention research specifically addressing HIV prevention for HIV+ individuals has come very much later in the history of the epidemic and is sparse in scope and number (Crepaz, Lyles, Wolitski, Passin, Rama et al., 2006; B. Johnson, Carey, Chaudoir, & Reid, 2006). As but one, albeit striking, example of differential emphasis in the targeting of HIV prevention research efforts, consider that a review in Social Science and Medicine, in the year 2000, almost two decades into the HIV epidemic, described attention to risk behaviors among HIV infected persons as a “new issue,” and indicated that a conference held in 1998 was “To our knowledge…the first scientific forum where the question of sexual behaviors and risk taking by HIV positive persons has been openly debated.” (Moatti & Souteyrand, 2000, p. 1524; see also Schiltz & Sandfort, 2000).
Figure 1.
Hierarchy of intervention subpopulation targets, assigning highest priority to intervention with infected individuals. After Aral, Douglas, & Lipshutz (2007), Behavioral Interventions for Prevention and Control of Sexually Transmitted Diseases.
The case for HIV prevention intervention research to strengthen prevention efforts among HIV infected individuals is straightforward (Crepaz et al., 2006; B. Johnson et al., 2006; J. Fisher et al., 2006; Kalichman, 2005; Kalichman et al., 2001; Stall, 2007). Early in the HIV epidemic, it would have been possible to develop and deploy theory-based and empirically-validated interventions to support preventive behavior among individuals who became aware that they were HIV+ and capable of transmitting infection to others. While it is the case that it is not necessary to know that one is HIV+ in order to practice prevention, and that interventions focused on so-called “high risk” group members undoubtedly included many HIV+ persons, social science intervention research and application addressing the specific sensitivities, dynamics, and needs of HIV+ individuals did not, for the most part, take place until relatively recently (see Crepaz et al., 2006; B. Johnson et al., 2006).
Later in the HIV epidemic, following the introduction of effective antiretroviral therapies in the mid-1990s, the case for social science research concerning prevention for HIV infected individuals becomes clearer still. Specifically, we note that antiretroviral therapy has been an incredibly welcome and lifesaving individual health victory that has changed HIV infection from a mortal illness to chronic and manageable disease. HIV infected individuals with access to antiretroviral therapy are living relatively healthy lives across a relatively normal lifespan and the number of HIV infected individuals is increasing steadily because AIDS-related mortality has thankfully dropped dramatically in settings in which antiretroviral therapy is available. From a public health perspective, however, there is the challenge of a growing population of relatively healthy HIV+ individuals who comprise (with apologies for the unfeeling language of epidemiology) an increasing number of potential vectors of infection. Although the infectivity of HIV+ persons on antiretroviral therapy may be lessened (Porco, Martin, Page-Shafer, Cheng, Charlebois, Grant, & Osmond, 2004), HIV infected individuals clearly deserve effective prevention support based on the best theoretical and empirical efforts of the social and behavioral sciences.
Stall (2007), Janssen et al.(2001) and others (see Crepaz et al., 2006; B. Johnson et al., 2006; J. Fisher et al., 2006; Kalichman, 2005) have helped establish the following rational basis for HIV prevention interventions for HIV-infected individuals, or what is now termed “Prevention for Positives:”
All new HIV infections begin with an HIV infected person and some HIV+ individuals who are aware of their status nevertheless engage in transmission risk behaviori.
It is more efficient to intervene with the small minority of persons who are HIV+ than with the general public (Stall, 2007; J. Fisher et al., 2006), although both intervention approaches remain important.
HIV prevention interventions with HIV+ persons can be successful in reducing transmission risk behavior (Crepaz et al., 2006; B. Johnson et al., 2006; Marks, Crepaz, Senterfitt, & Johnson, 2005).
In the era of antiretroviral therapy, prevalence rates for HIV infection will continue to increase as will the number of persons capable of transmitting infection (Stall, 2007; Hall, Song, Rhodeset al., 2008; CDC 2008a,b, UNAIDS 2008a).
In the era of antiretroviral therapy, imperfect adherence and other causes will result in the development of drug resistant HIV which may be transmitted to uninfected others and which amplifies the public health importance of prevention for positives (Bangsberg, Moss, & Deeks, 2006; Janssen et al., 2001; Kozol, Amico, Chiarella et al., 2006; Wainberg & Friedland, 1998).
The critical question, then, is whether HIV prevention research in the social and behavioral sciences, tailored to meet the needs of HIV+ individuals, has answered this challenge in a timely and effective fashion.
HIV Prevention Research in the Social Sciences
As noted in preceding discussion, social scientists responded early and effectively in the course of the HIV epidemic and contributed conceptually based and empirically validated HIV prevention interventions that generally targeted populations not known to be composed of HIV infected individuals. (See meta-analyses, identifying rigorous HIV prevention interventions and their target groups, by Albarracin, Gillette, Earl, Glasman, Durantini, & Ho, 2005; W. Johnson, Hedges, Ramirez, Semaan, Norman et al., 2002; Semaan, Kay, Strouse, Sogolow, Mullen et al., 2002; see also Noar’s 2008 meta-analysis of meta-analysis results in this area). Semaan et al’s (2002) profile of trials of HIV prevention interventions in the US, for example, identified 99 experimental and quasi-experimental HIV prevention trials since 1988, but noted that HIV+ persons “were not the focus (target) of any of the 99 studies” (p. S32). Also showing this pattern is W. Johnson et al’s (2002) meta-analysis of HIV prevention research focusing on men who have sex with men, which found only a single study of HIV+ men who have sex with men meeting inclusion criteria. Similarly, Albarracin et al.’s (2005) comprehensive meta-analysis of HIV prevention interventions since the beginning of the epidemic identified 354 interventions that qualified for inclusion. Of the 354 HIV prevention interventions in Albarracin et al.’s (2005) sample, the investigators note, under the heading “Limited data about HIV positive individuals,” that only 22 intervention groups in their research synthesis even provided information about the HIV infection status of participants. This problem “…restricted consideration of intervention effectiveness among HIV-positive individuals, those capable of transmitting HIV.” (p. 888).
In a related illustration of differential intervention research emphasis in the social sciences, Noar (2008) reviewed and synthesized 18 meta-analyses of the HIV prevention intervention literature and found that only two of the 18 (Crepaz et al., 2006; B. Johnson et al., 2006) were meta-analyses of HIV prevention interventions for HIV+ persons. One of the two (B. Johnson et al., 2006) included 12 single studies of the effectiveness of an HIV prevention intervention for an HIV+ sample, and the other (Crepaz et al., 2006) also included 12 single studies of an HIV prevention intervention for an HIV+ sample. Nine of the studies included in the two meta-analyses overlapped, for a total of only 15 studies in the literature that consisted of an HIV prevention intervention for HIV+ persons and met study inclusion requirements. Significantly, we note that both B. Johnson et al. (2006) and Crepaz et al (2006) reported meta-analytic evidence of intervention effectiveness with respect to HIV+ participants’ rates of condom use or unprotected sex, and Crepaz et al. (2006) also reported decreased acquisition of sexually transmitted infections in HIV+ intervention (versus HIV+ control) participants.
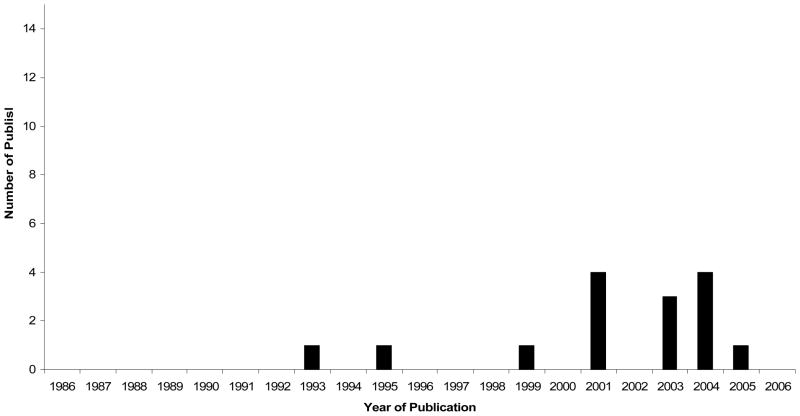
A chronological presentation of the publication dates of the studies of HIV prevention for HIV+ persons included in the B. Johnson et al. (2006) and Crepaz et al. (2006) meta-analyses (see Figure 2) demonstrates that this literature was both very late in developing in the course of the epidemic and very limited in number. The total of 15 studies of HIV prevention for HIV+ persons reported by B. Johnson et al. (2006) and Crepaz et al. (2006) compares poorly with the 354 HIV prevention interventions included in Albarracin et al.’s (2005) meta-analysis of the overall HIV prevention literature. Additional relevant evidence concerning the record of HIV prevention research focusing on HIV+ individuals may be found in the Center for Disease Control and Prevention’s (2008d, e) listing of “Best Evidence” and “Promising Evidence” prevention interventions. As of November, 2008, only three of 30 (10%) “Best Evidence” HIV prevention interventions listed were developed to support HIV+ persons’ efforts to avoid transmission risk behavior and only 2 of 18 (11%) “Promising Evidence” HIV prevention interventions were developed for HIV+ persons.
Figure 2.
Publication dates of 15 HIV prevention interventions directed at HIV+ persons included in the B. Johnson et al. (2006) and Crepaz et al. (2006) meta-analyses.
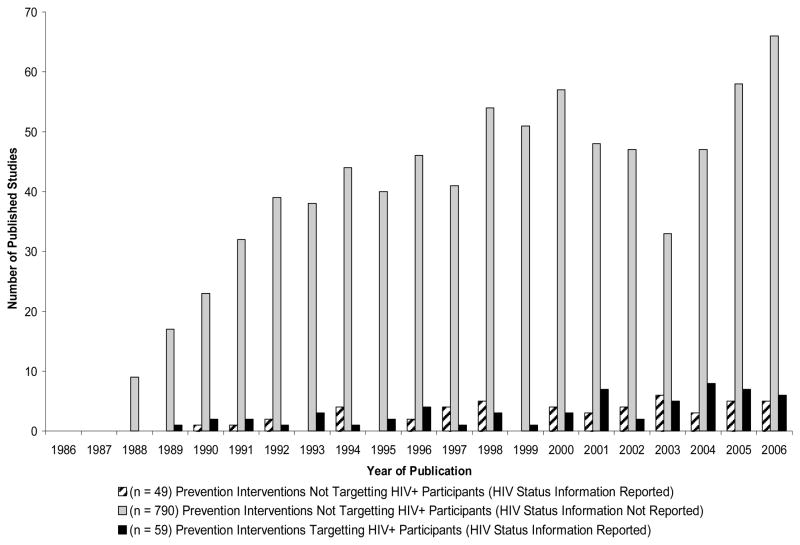
To gain the broadest possible empirical overview of the record of HIV prevention intervention research for HIV+ individuals, across the course of the epidemic, we conducted a novel analysis of the extensive database of the Prevention Research Synthesis project of the Centers for Disease Control and Prevention (N. Crepaz, Personal Communication, January 31, 2008). Casting the widest possible net to identify HIV prevention interventions focusing on HIV+ participants, we reviewed the abstracts of each of the 1,465 reports in this dataset. We included in our analysis all HIV prevention interventions, directed at any population, with any HIV prevention related endpoint, broadly defined to include intervention-induced changes in HIV prevention information, motivation, HIV risk behavior, or acquisition of sexually transmitted infections. We eliminated studies without such endpoints and studies published after 2006, since coverage in the dataset after this date was not complete. A total of 898 relevant studies, reported between 1988 and 2006, were thus identified. Of these 898 studies, 790 HIV prevention interventions neither targeted HIV+ individuals nor provided information about the HIV status of participants; an additional 49 HIV prevention interventions did not target HIV+ individuals but did provide information about the HIV status of participants; and 59 studies reported HIV prevention research targeting HIV+ participants with any prevention-relevant endpoint (see Figure 3). Thus, 59 of 898 of all HIV prevention interventions identified from 1988 to 2006, or 6.6% of HIV prevention interventions, were directed at HIV+ individuals capable of communicating infection to others. As can be seen in Figure 3 as well, the majority of HIV prevention interventions for HIV+ individuals were reported during or after the year 2000, two decades or more into the HIV epidemic.
Figure 3.
Publication dates of 898 HIV prevention intervention with samples of HIV+, HIV−, and HIV status unknown persons, with any HIV prevention relevant endpoint, 1980–2006.
In interpreting evidence of late-developing and sparse HIV prevention intervention research for HIV+ individuals, we are reminded of Wolitski, Flores, O’Leary, Bimbi and Gomez’s (2006) conceptualization of HIV+ persons’ perceptions of responsibility for prevention of HIV infection. In Wolitski et al’s (2006) work, a two-factor approach is used to suggest that HIV+ individuals may be relatively high or low in the belief that they, personally, are responsible for prevention of HIV transmission, and they may also vary in their relatively high or low belief that their partners are responsible for prevention of HIV infection. These investigators examined reports of unprotected sexual contacts of HIV+ men who have sex with men with HIV− or HIV status unknown partners, and found that in general and as predicted, HIV+ men who have sex with men with high self—low partner responsibility reported the lowest level of HIV transmission risk behavior. HIV+ men who have sex with men with low self—high other responsibility had the highest level of HIV transmission risk behavior. In further research with HIV+ men who have sex with men, Wolitski, Bailey, O’Leary, Gomez, Parsons et al. (2003) report that some 66% of HIV+ men who have sex with men viewed themselves as having personal responsibility to protect others from infection, while 24% perceived other responsibility only and 12% perceived shared self—other responsibility for preventing infection. In conducting research that has neglected prevention for HIV+ individuals, we appear to have failed to address the need to support what HIV+ persons themselves most often regard as personal or shared responsibility for prevention of infection.
HIV Normalization in Public Health Policy and HIV Prevention Research: The Crumbling of HIV Exceptionalism
We have considered evidence of “HIV exceptionalism”—departures from standard practice and the sensitive (some have argued overly sensitive) treatment of HIV+ individuals’ to the exclusion of sound public health practice and prevention research priorities (Bayer, 1989, 1991; Bayer & Fairchild, 2006; Frieden et al., 2005; Stall and Mills, 2006). We would now like to bring forward evidence of a sea change towards what has been termed the “normalization” of HIV public health practice and HIV prevention research, starting near the beginning of the new millennium (Rosenbrock et al., 2000). This change occurred, not at all incidentally, soon after the successful introduction of antiretroviral therapy which “normalized” HIV as a chronic disease and facilitated normalization of public health practice and prevention research in the HIV domain.
With respect to evidence of the normalization of public health practice in HIV prevention, we report that the Centers for Disease Control and Prevention (2003), the U.S. National Institutes of Health (1997), the Global HIV Prevention Working Group (2004), and United Nations Joint Program on HIV and AIDS (UNAIDS, 2008c) have now all designated HIV prevention interventions for HIV+ persons as a critical priority in containing the HIV pandemic. As early as 2001, the Centers for Disease Control and Prevention adopted the strikingly “normalized” Serostatus Approach to Fighting the HIV Epidemic:
Through the Serostatus Approach to Fighting the Epidemic (SAFE), the Centers for Disease Control and Prevention is now expanding prevention programs, especially for individuals with HIV, to reduce the risk of transmission as a supplement to current programs that primarily focus on reducing the risk of acquisition of the virus.
For individuals with HIV, SAFE comprises action steps that focus on diagnosing all HIV-infected persons, linking them to appropriate high-quality care and prevention services, helping them adhere to treatment regimens, and supporting them in adopting and sustaining HIV risk reduction behavior. SAFE couples traditional infectious disease control focus on the infected person with behavioral interventions that have been standard for HIV prevention programs. (Janssen, Holtgrave, Valdeisseri, Shephard, Gayle, & De Cock, 2001, p. 1019).
With respect to evidence of the normalization of HIV prevention research in the social sciences, we note that the Centers for Disease Control’s compendium of “Best Evidence” and “Promising Evidence” interventions for HIV+ individuals increased from 5 of 48 prevention interventions overall to 9 of 67 prevention interventions overall from November 2008 to the July 2009 prepublication update of this manuscript. This represents a rapid increase of 80% in the small but growing number of HIV prevention interventions for HIV+ persons in the Centers for Disease Control and Prevention endorsement list (Centers for Disease Control and Prevention, 2008d, 2008e, 2009a, 2009b).
To illustrate “normalized” social science research in this area, we review work on the Options Project (J. Fisher, Cornman, Norton, & Fisher, 2006; J. Fisher, Fisher, Cornman, Amico, Bryan, & Friedland, 2006;), a collaborative endeavor of physicians, behavioral scientists, and HIV+ patients that resulted in the development a successful HIV prevention intervention designed to support HIV prevention among HIV infected persons.
The Options Project (J. Fisher, Cornman, Norton, & Fisher, 2006; J. Fisher, Cornman, Osborn, Amico, Fisher, & Friedland, 2004; J. Fisher, Fisher, Cornman, Amico, Bryan, & Friedland, 2006; see also Cornman, Kiene, Christie, Fisher, Shuper et al., 2008) was designed “from the ground up” as an intervention to be delivered during routine HIV medical care and on an ongoing basis, since this provides the most universal and continuous contact with HIV+ individuals possible. The Options Project was also based upon early and ongoing collaboration and exchange among researchers, clinicians, and HIV+ patients because it was clear that this was the most effective means to create an acceptable, feasible, equitable, and supportive prevention intervention to take place in the clinician—patient interaction. In order to create such an intervention, HIV prevention researchers brought to the table a well-validated model for understanding and promoting HIV risk behavior change, the Information—Motivation—Behavioral Skills model (J. Fisher & Fisher, 1992, 2000), and a collaborative, patient-centered intervention approach, Motivational Interviewing (Rollnick, Mason, & Butler, 1999). The Information—Motivation—Behavioral Skills model asserts that HIV prevention information, motivation to act on this information, and behavioral skills for acting on it effectively, are crucial determinants of HIV preventive behavior. Individuals who possess information that is easy to translate into preventive behavior, who have personal attitudes favorable to prevention and perceive normative support for prevention, and who possess behavioral skills for avoiding or managing risky situations, are, in the view of the model, likely to initiate the practice HIV preventive behavior and to maintain such behavior over time. Accordingly, model based interventions seek to identify and address HIV prevention information deficits, motivational obstacles, and behavioral skills limitations (and to mobilize information, motivation, and behavioral skills assets) to promote preventive behavior. The Information—Motivation—Behavioral Skills model approach calls for the conduct of elicitation research, to clarify relevant information, motivation, and behavioral skills limitations and assets that may be related to risky behavior. This is followed by delivery of tailored prevention interventions that are empirically based upon elicitation research findings, and evaluation of intervention effectiveness, preferably in a fashion uninfluenced by the interveners themselves. The Motivational Interviewing approach was employed as an intervention delivery channel that is patient-centered rather than top-down and that permits the clinician, in conversation with the patient, to fairly rapidly discern information, motivation, and behavioral skills obstacles to HIV prevention. The clinician then initiates a process, consulting the patient as the foremost expert in what would be required for his or her behavior change, directed at achieving movement toward risk reduction and maintenance of change over time.
Elicitation research with HIV care clinicians and HIV infected persons in clinical care, involving focus groups, individual interviews, and other methods, assessed clinician and patient perspectives on what a supportive HIV prevention intervention for HIV+ patients might involve, how it could be structured so as to be feasible for busy clinicians to learn and to deploy, and how it could be crafted so as to be patient-centered as opposed to top-down or coercive (J. Fisher et al., 2004). As a result of this formative research, a theory-based, patient-centered intervention was developed, involving collaborative conversations between physicians and patients concerning HIV prevention at each routine HIV clinical care visit. A preliminary version of the intervention was designed and commented on by all stakeholders, the intervention was refined on the basis of these comments, and a pilot test of the intervention was implemented and revised based upon further input from the behavioral scientists, clinicians, and patients involved.
Working with a quasi-experimental design at the two largest HIV care clinics in Connecticut, the Options Project was implemented and evaluated between 2000 and 2003. Assessment of 490 HIV+ patients indicated that at baseline, 114/490 (23%) participants reported engaging in unprotected vaginal, anal, or insertive oral sex during the past three months. HIV+ participants’ unprotected sexual contacts during this time were substantial, involving 2,408 unprotected vaginal, anal, or insertive oral sex events. Of these, there were 1,785 unprotected vaginal or anal sex events with a total of 351 different partners (J. Fisher, Fisher, Cornman et al., 2006). Subsidiary unpublished analyses of baseline data indicate that 52/490 (11%) HIV+ patients in clinical care in the study reported 1,072 unprotected vaginal or anal sexual events with 197 different HIV− or HIV-status unknown partners during the past three months.
Within the Options Project intervention condition, HIV care clinicians were trained to engage in brief, theory-based, patient-centered HIV prevention intervention activities at each clinical visit. In these visits, clinicians verbally assessed patients’ safer and risky sexual and injection drug use behaviors, evaluated patients’ readiness to change or to maintain safer behaviors, and elicited strategies from the patient concerning how best to change risky or to maintain safer patterns of behavior. Clinician and patient then negotiated an agreed-upon and realistic goal or plan of action in this respect and the clinician gave the patient a “Prevention Prescription” upon which this agreed-upon goal was written.
Over the course of Options Project research, 23 HIV care clinicians were trained to deliver the intervention, and fidelity and feasibility analyses showed that the intervention was delivered with considerable fidelity in 73% of all HIV clinical care visits over an extended period of time (J. Fisher et al., 2004). Results indicated that HIV+ patients who received the intervention reported significant reductions in total unprotected insertive and receptive vaginal and anal intercourse and insertive oral sex over a follow-up interval of up to 18 months. Results also showed that there was a significant increase in risky sexual behavior among HIV+ patients in a standard of care comparison research arm, suggesting the potential costs of not providing HIV risk reduction support to HIV+ persons. The investigators concluded that an HIV prevention intervention delivered in the context of clinical care provided the widest possible access to HIV infected individuals and assisted HIV+ persons in meeting the challenges of HIV transmission risk reduction over time.
In the context of the current discussion of the subject of HIV exceptionalism, one might consider the Options Project research and the small but significant number of other reported HIV prevention interventions for HIV+ persons (see Crepaz et al., 2006; B. Johnson et al., 2006; Centers for Disease Control and Prevention, 2009a, 2009b) to be both “good news” (that is, examples of effective HIV prevention research reaching individuals capable of transmitting infection and perpetuating the epidemic) and “bad news” (that is, critical research with an important target group which has nonetheless taken place quite late in the course of the epidemic).
Reflections, Analysis, and Lessons Learned
“What went wrong?”
William W. Darrow, Chief, Behavioral and Prevention Research Branch, Division of STD/HIV Prevention, Centers for Disease Control, during early years of the HIV epidemic (Darrow, 2004)
The current analysis has considered the subject of HIV exceptionalism, a policy of treating HIV differently, such that standard public health and prevention research priorities gave way to novel approaches that appear to have accorded more weight to the protection of individual rights than to protection of individual and public health. What, then, went wrong?
What follows are four divergent attempts to account for the record of public health policy and prevention research that we have reviewed. After considering these explanations, we propose a more integrated social psychological analysis of determinants and processes that influenced the course of public health practice and prevention research across the HIV epidemic. We then consider implications of this model, and the history that it reflects, for the creation of public health and social science research policy that adapts as well as possible to future epidemic threats.
Nothing Went Wrong
One credible view of the history of public health practice and prevention research during the HIV epidemic involves the assertion that nothing went wrong. This perspective holds that public health policy and prevention research were highly appropriate and highly adapted to the situation on the ground as the epidemic developed. This view recalls that early in the epidemic, there was no test for HIV infection and no treatment for it, and that there was tremendous discrimination against gay men and injection drug users even before the epidemic began, not to mention afterwards. Most people discovered they had HIV when they became very ill or on their deathbeds, when sexual behavior, safer or otherwise, was clearly not an issue. The primary concern among professionals and the general public at the time, then, was fear of a population-wide epidemic. Accordingly and appropriately, social scientists contributed early on and effectively with HIV prevention interventions targeting the general public and so-called “high risk” groups in an effort to contain a frightening and poorly understood epidemic. As HIV testing and treatment for opportunistic infections became available, more public health and community based support for HIV testing developed and more individuals got tested. And, very soon after the development of antiretroviral therapy and the survival of a large number of relatively healthy and long-lived HIV+ persons, work on HIV prevention for HIV+ individuals did appear, also appropriate to realities on the ground, and it continues, together with priority on public health policy and social science research on prevention for positives, today.
Plenty Went Wrong: The Road to Hell Was Paved with Good Intentions
Another, plausible account of the history of public health practice and prevention research at focus asserts that a range of highly prosocial values contributed to the development of HIV exceptionalism and its unintended negative consequences. This view asserts that public health policy and prevention research neglect of HIV+ individuals—the very individuals biologically capable of perpetuating and expanding the HIV epidemic—resulted in failure to address the prevention needs of the critical target group that should have been enlisted in containing the spread of infection. This view also asserts that, in effect, the road to hell was paved with good intentions, and that empathy and tolerance were root causes of efforts to treat HIV with special sensitivity, with the unintended result of underweighting public health concerns and rational research priorities. According to this perspective, HIV exceptionalism emerged at a time when it was critical to avoid revictimizing the already-victimized and mortally ill persons who were afflicted with HIV/AIDS, and critically important to stem the wave of stigma and demonization of people with this disease. Empathy- and tolerance-driven efforts to avoid further harm to those suffering from HIV prompted unwillingness to single out HIV+ persons as a specific target group for prevention intervention research and application. Focusing on HIV+ persons for special prevention attention would have reinforced the view that infected individuals should be treated as Typhoid Marys responsible for perpetuating a deadly and widening epidemic. It was feared that a “prevention for positives” approach would have assisted those committed to blaming the victim and given strength to extremist calls for mandatory testing and quarantine or tattooing of HIV infected persons (see Bayer, 1989, for evidence of widespread hostility to persons living with HIV/AIDS). This view recalls as well that it was self-selected, well-intentioned, empathic, and tolerant individuals who chose to take part in the fight against this disease within medicine, public health, and the social sciences. The empathy and tolerance that these individuals brought to HIV care, public health practice, and prevention research inhibited focus on the risk reduction needs of HIV-infected individuals because it was believed to be inhumane to add demonization to their existing burden of stigma, disease, and death. Prosocial values of empathy and tolerance thus delayed the conduct of HIV prevention research for HIV+ individuals during the first two decades of the epidemic.
Plenty Went Wrong: The Road to Hell Was Paved with Cynicism and Fear
A third account of the record of public health policy and prevention research asserts that self-interest, cynicism, and fear heavily influenced policy and prevention in the HIV domain. As unpalatable as it may seem, this account suggests that what has been referred to as “the HIV research industry” knew very well that promoting fear of a widespread epidemic and focusing prevention efforts on the general public would produce unprecedented research dollars, accelerated academic careers, and professional fame. The cynical view reminds us as well that fear of radical backlash from direct-action groups such as ACT UP, whose tactics ranged from the merely unsettling to implicit threats of violence, also deterred researchers from focusing on the prevention needs of people with HIV some of whom, it was feared, would engage in direct action against researchers themselves (see Bayer & Oppenheimer, 2000). And, cynical or not, this explanation will not permit us to forget that that anti-gay and anti-injection drug user prejudice deterred prevention focus on HIV affected groups in accord with the view, loathsome to us, that these individuals were unworthy of assistance with the tragedy that they had brought upon themselves.
Plenty Went Wrong: But Not As Much as You Think, and Not All for One Reason
Still another view, more balanced and closer to the authors’ own, is that plenty went wrong, but not as much one might think, and not all for a single reason. Specifically, this view asserts that early in the AIDS epidemic, and prior to the advent of HIV testing, empathy and tolerance for those with an untreatable fatal disease was the only humane course of action possible. Moreover, in the context of a poorly understood and widening epidemic, prevention interventions targeting essentially everyone were the only reasonable focus for public health and prevention research. With the advent of HIV testing and treatments for opportunistic infections in the mid-1980s and beyond, however, empathy and tolerance, and the protection of individual rights—always needed—began to loose some of their precedence. It was at this juncture that voluntary but much more proactive HIV testing, identification of HIV infected individuals and bringing them into medical care, and the development of interventions for prevention of HIV transmission from HIV+ persons to uninfected others, were critically needed. That a number of these actions, including the development of prevention interventions for HIV+ persons, were neglected until later in the course of the epidemic was a costly error that was most probably the result of good intentions and good values, however, rather than bad.
Prejudice, Fear, and Victim Blame Meet Empathy, Tolerance, and Altruism: A Preliminary Social Psychological Analysis of Processes Influencing Public Health Practice and Prevention Research in the HIV Epidemic
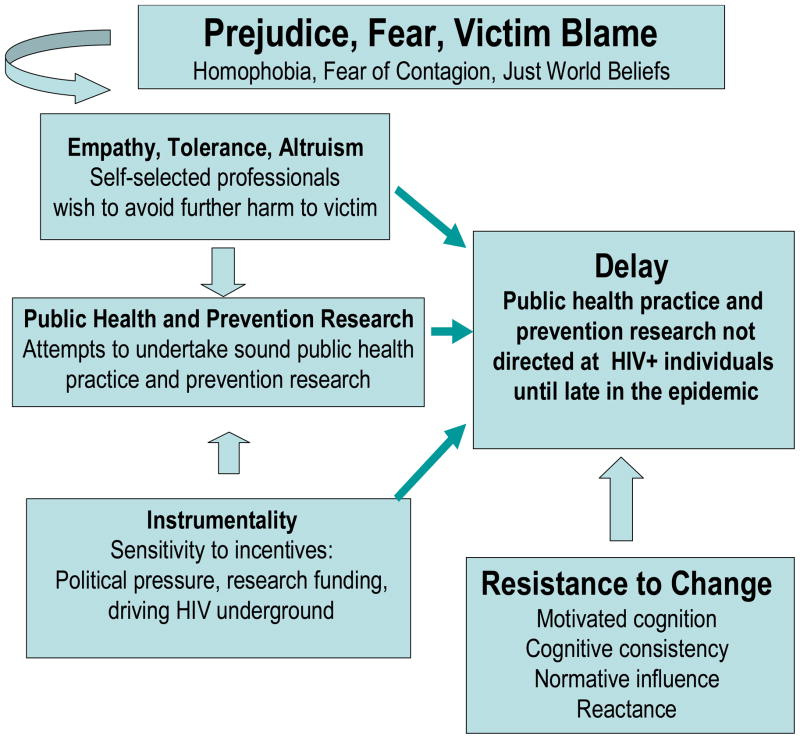
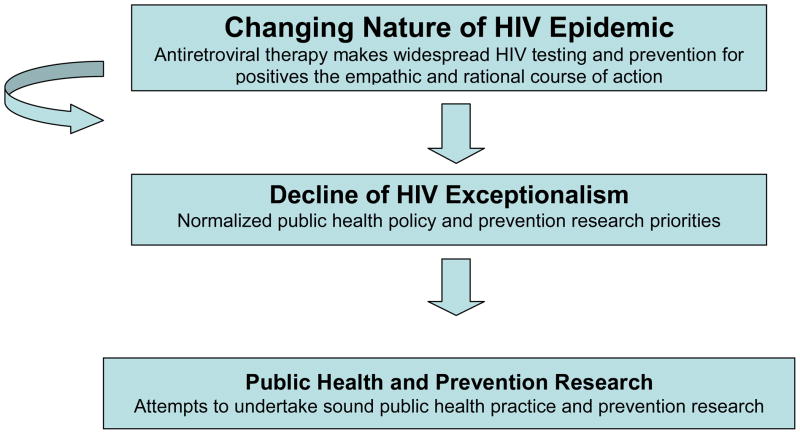
A somewhat more integrated social psychological analysis of factors that may have influenced public health policy and prevention research in the HIV epidemic is presented in Figure 4.
Figure 4.
A preliminary social psychological conceptualization of determinants and processes influencing the development and targeting of HIV prevention research in the social sciences.
At the very top of Figure 4, as an overarching construct. we suggest that prejudice, fear, and victim blame (Allport, 1954; Bayer, 1989; Crandall & Eshelman, 2003; Devine, Monteith, Zuwerink, & Elliot, 1991; Lerner, 1980; Maes, 1994) saturated and defined the social context in which public health policy and prevention research priorities developed during the first decade of the HIV epidemic. Homophobia, prejudice, and aggression against groups and individuals affected by HIV (Herek & Capitano, 1996; Crawford, 1996) was “justified” (to employ Crandall and Eshelman’s “suppression—justification” theory of prejudice) by fear of widespread contagion and directly expressed against “high risk” group members and HIV-infected persons. Accompanying the “justified” expression of prejudice against those affected by HIV (Crandall & Eshelman, 2003), widespread belief in a just world (Lerner, 1980; Maes, 1994) provided a basis for blaming the victims of HIV infection as responsible for their own plight and devaluing their suffering.
As indicated by the curved arrow at the top of Figure 4, within the atmosphere of prejudice, fear, and victim blame of the early years of the HIV epidemic (Bayer, 1989), self-selected empathic, tolerant, and altruistic professionals (Bayer & Oppenheimer, 2000) attempted to undertake sound public health practice and prevention research. These well-intentioned professionals made decisions that were tempered by the desire to avoid anything—such as specifically targeting HIV+ persons for prevention interventions—that might strengthen existing patterns of prejudice, fear of contagion, and blaming the victim (see Batson, 1990, and Batson, Polycarpou, Harmon-Jones, Imhoff, Mitchener et al., 1997, for discussion of empathy, attitudes, and altruism). Added to this, as noted in the lower left corner of Figure 4, instrumental considerations, including fear of backlash from direct action groups, fear of “driving the disease underground,” and desire to acquire or maintain research funding associated with public fears of a generalized epidemic, also contributed to HIV exceptionalism in public health practice and prevention research (see Rotter, Chance, and Phares, 1972, and Fishbein and Ajzen, 1975, among others, for discussion of the role of expectancies for outcomes on motivation to act). The combination of empathy, tolerance, altruism, and instrumental concerns affected the nature of public health and prevention research priorities formed early in the HIV epidemic. Together they contributed to HIV exceptionalism and resulted in delay of implementation of nonexceptional public health practice and prevention priorities until late in the epidemic.
As suggested in the lower right hand portion of Figure 4, several well recognized social psychological processes created inertia and resistance to change in positions adopted early in the epidemic and short-circuited feedback that might have resulted in more rapid normalization of public health practice and prevention research. Such inertia-promoting processes may have included motivated reasoning to neutralize evidence that change was necessary (Kunda, 1990; see also Bersoff, 1999), reactance to outside pressures to change prevention policy (Brehm & Brehm, 1981), motivation to maintain cognitive consistency with positions to which commitments had originally and very publicly been made (Festinger, 1957; Elliot & Devine, 1994), and reluctance to oppose what had emerged early in the epidemic as appropriate and politically correct professional and social norms (Fishbein & Ajzen, 1975; J. Fisher, 1988).
As can be seen in the top portion of Figure 5, the advent of effective antiretroviral therapy resulted in profound change in the nature of the HIV epidemic and in the social and biomedical context of HIV prevention. Empathic, tolerant, and altruistic professionals could now craft policy and prevention research agendas in which widespread and proactive HIV testing and research on prevention for positives made a tremendous amount of sense. HIV became “normalized” as a treatable chronic illness, HIV testing as a means of bringing HIV-infected individuals into effective care became a priority, and the promotion of prevention for healthy, long-lived, but potentially infectious HIV+ persons became an empathic and rational objective. Accordingly, incentives and normative pressures changed became more favorable to these activities. Within the reframing of HIV as a treatable chronic disease and as a simple function of familiarity with the HIV epidemic over time, prejudice, victim blame, and fear of contagion were lessened, and a tipping point was reached. Social psychological forces no longer inhibited change and normalization of public health practice and research on prevention for positives both advanced.
Figure 5.
Factors affecting the normalization of HIV prevention public health and prevention research priorities.
We note that while this analysis brings social psychological concepts to the history of policy and research developments in the HIV epidemic, it is a highly speculative one and it would require considerable ingenuity to test the proposed relationships empirically. Such work, possibly utilizing qualitative analyses of textual records from the history of the HIV epidemic, could, however, be quite illuminating.
Lessons Learned: Policy Implications for Research and Practice
What lessons can we learn from the history of HIV prevention public health practice and prevention research in the social sciences? From the perspective of the current analysis, the major lesson to be learned concerns the interaction of social context, individual values, and social psychological processes that contribute to the early formation of policy and research priorities, and processes that contribute to inertia and resistance to change. It is highly likely that public health and prevention research priorities in future epidemic settings will need to be developed under circumstances of social context that will again involve prejudice, fear, victim blame, and the need to balance individual rights and public health concerns. It is also likely that individuals with prosocial motivation will elect to work in public health and social science research efforts to address epidemic disease. And, while it has always been clear that bad values can drive bad science, the story we have recounted reminds us that good values can also potentially misdirect science and policy and inhibit reflection and change. The best of empathy-tolerance- and altruism-related impulses may have contributed to a delay in normalization of public health practice and prevention research in the context of the HIV epidemic and could do so again in future epidemic settings.
The current analysis suggests that work in the HIV epidemic, and in future epidemics, will have to very consciously take into account generalized societal influence (prejudice? fear? victim blame?), the instrumentality and incentives that may influence decision making, the blend of prosocial motives and professional action that may be required for sound public health and prevention research policy, and social psychological processes that may strongly inhibit needed reflection and required change. It should however be possible to conduct dispassionate scientific research—such as rational focus on HIV prevention for HIV+ persons capable of transmitting infection, before 20 years of pandemic have elapsed—and at the same time passionately to insist upon prosocial values of individual rights and protections for affected individuals. We must also remember the fact that we live in a multivariate ethical universe, in which univariate ethical principles (“protection of individual rights” and “protection of the health of others”) provide little guidance when considered in isolation and in which the uncomfortable but necessary integration and prioritization of ethical principles into hierarchies may be required. Whatever else we may have learned, it seems clear that our responses to what Bayer (1989) has called the challenge of “Private Acts, Social Consequences” will require sober and self-questioning second looks and careful sensitivity to multiple potential social influences we have noted on research, policy, and practice.
Epilogue
We close this discussion by recalling the clarion call of activists of the early days of the HIV/AIDS epidemic: “Silence = Death” (The Body. The Complete HIV/AIDS Resource. 2009). This call to action reminds us that at the end of the day, the social psychological processes we have outlined resulted, quite simply, in protracted silence concerning HIV prevention for HIV+ persons. A major policy lesson learned involves the need for active and self-reflective assessment, sensitive to social psychological processes at play, of the balance between individual rights and public health in future epidemics that unfold, as does HIV, at the intersection of human biology and human behavior.
As of this writing, each of the social forces represented in our model is still very much in evidence. On one hand, we hear echoes of the prejudice and fear that drive empathic public health policymakers and prevention scientists to act to protect victims from further harm. Within days of this writing, for example, California, the most populous US state, voted to amend its constitution to outlaw same-sex marriage. On the other hand, echoes of HIV exceptionalism are heard as well. Commenting on the case of an HIV+ individual who is alleged to have knowingly infected 12 women, two of whom have died, the physician who cared for the individual stated “Our focus is him and his health. But I did have a safer sex discussion…but the focus is…his health.” (Globe and Mail, October 22, 2008, A5, emphasis in original). It remains clear that the struggle for balance in public health policy and prevention research will continue to require attention to prejudice, empathy, norms, incentives, individual rights, public welfare, and above all, the creation and maintenance of a self-questioning feedback loop, sensitive to the pressures of motivated reasoning, cognitive consistency, normative pressure, and other factors contributing to silence and antagonistic to change.
Acknowledgments
The authors wish to thank Nicole Crepaz of the Centers of Disease Control and Prevention and her research staff for assisting us with access to the Prevention Research Synthesis project database, and Blair Johnson for providing access to a database of HIV prevention interventions.
Footnotes
Not all new HIV infections originate from individuals who are aware of their HIV status, of course, and not every occasion of transmission risk behavior results in a new infection. See Marks, Crepaz, and Janssen’s (2006) estimate that half of new sexually transmitted HIV infections in the US originate in the 25% of HIV+ Americans who are unaware of their HIV status; see also Marks, Crepaz, Senterfitt, & Johnson’s (2005) meta-analysis of HIV risk behavior by HIV+ persons aware and unaware of their HIV status, and Kalichman et al. 2001, for discussion of rates of unprotected sexual activity by HIV+ individuals).
Contributor Information
William A. Fisher, University of Western Ontario
Taylor Kohut, University of Western Ontario.
Jeffrey D. Fisher, University of Connecticut
References
- ACT UP. AIDS Coalition to Unleash Power. ACT UP; New York: n.d. Retrieved November 8, 2008, from http://www.actupny.org. [Google Scholar]
- Ajzen I. From intentions to actions. A theory of planned behavior. In: Kuhl J, Beckman J, editors. Action control from cognition to behavior. New York: Springer-Verlag; 1985. pp. 11–39. [Google Scholar]
- Albarracin D, Gillette JC, Earl AN, Glasman LR, Durantini MR, Ho M. A test of major assumptions about behaviour change: A comprehensive look at the effects of passive and active HIV-prevention interventions since the beginning of the epidemic. Psychological Bulletin. 2005;131:856–897. doi: 10.1037/0033-2909.131.6.856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albarracin D, Johnson BT, Fishbein M. Theories of reasoned action and planned behavior as models of condom use: A meta-analysis. Psychological Bulletin. 2001;127:142–161. doi: 10.1037/0033-2909.127.1.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allport GW. The nature of prejudice. Reading, MA: Adison-Wesley; 1954. [Google Scholar]
- American Psychologist. Special issue on AIDS [Special Issue] American Psychologist. 1988;43(11) [Google Scholar]
- Aral SO, Douglas JM, Lipshutz JA. Behavioral interventions for prevention and control of sexually transmitted diseases. New York: Springer; 2007. [Google Scholar]
- Bandura A. Social foundations of thought and action. A social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- Bandura A. Perceived self-efficacy in the exercise of control over AIDS infection. In: Mays VE, Albee GW, Schneider SF, editors. Primary prevention of AIDS. Psychological approaches. Primary prevention of psychopathology. XIII. Thousand Oaks, CA: Sage; 1989. pp. 128–141. [Google Scholar]
- Bangsberg DR, Perry S, Charlebois ED, Clark RA, Robertson M, et al. Non-adherence to highly active antiretroviral therapy predits progression to AIDS. AIDS. 2001;15:1181–1183. doi: 10.1097/00002030-200106150-00015. [DOI] [PubMed] [Google Scholar]
- Batson CD. American Psychologist. 1990. Mar, How social an animal? The human capacity for caring; pp. 336–346. [Google Scholar]
- Batson CD, Polycarpou MP, Harmon-Jones E, Imhoff HJ, Mitchener EC, Bednar LL, et al. Empathy and attitudes: Can feeling for a member of a stigmatized group improve feelings toward the group? Journal of Personality and Social Psychology. 1997;72:105–118. doi: 10.1037//0022-3514.72.1.105. [DOI] [PubMed] [Google Scholar]
- Bay Area Physicians for Human Rights. BAPHR. 2008 Retrieved November 8, 2008 from http://www.baphr.org.
- Bayer R. AIDS and the politics of public health. New York: The Free Press; 1989. Private acts, social consequences. [Google Scholar]
- Bayer R. Public health policy and the AIDS epidemic. An end to HIV exceptionalism? New England Journal of Medicine. 1991;234:1500–1504. doi: 10.1056/NEJM199105233242111. [DOI] [PubMed] [Google Scholar]
- Bayer R, Fairchild AL. Changing the paradigm for HIV testing—The end of exceptionalism. New England Journal of Medicine. 2006;355:647–649. doi: 10.1056/NEJMp068153. [DOI] [PubMed] [Google Scholar]
- Bayer R, Oppenheim GM. AIDS doctors: Voices from the epidemic. Oxford: Oxford University Press; 2000. [Google Scholar]
- Bersoff DM. Why good people sometimes do bad things: Motivated reasoning and unethical behavior. Personality and Social Psychology Bulletin. 1999;25:28–39. [Google Scholar]
- The Body. The Complete HIV/AIDS Resource. 2009 Retreived July 24, 2009 from http://www.thebody.com/content/art14040.html.
- Brehm SS, Brehm JW. Psychological reactance: a theory of freedom and control. New York: Academic Press; 1981. [Google Scholar]
- Byrne D. Sex without contraception. In: Byrne D, Fisher WA, editors. Adolescents, sex, and contraception. Hillsdale, NJ: Lawrence Erlbaum Associates; 1983. pp. 3–32. [Google Scholar]
- Catania JA, Kegeles SM, Coates TJ. Towards an understanding of risk behavior. An AIDS risk reduction model (AARM) Health Education Quarterly. 1990;17:53–72. doi: 10.1177/109019819001700107. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. AIDS cases and deaths, by year and age group, through December 2001. 2001 Retrieved November 8, 2008, from http://www.cdc.gov/hiv/topics/surveillance/resources/reports/2001report/table21.htm.
- Centers for Disease Control and Prevention. Incorporating HIV prevention into the medical care of persons living with HIV: Recommendation of the CDC, the Health Resources and Service Administration, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. Morbidity and Mortality Weekly Report. 2003;52(RR-12) [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. HIV Incidence. 2008a Retrieved November 8, 2008, from http://www.cdc.gov/hiv/topics/surveillance/incidence.htm.
- Centers for Disease Control and Prevention. New Evidence of US HIV Prevalence, 2006. 2008b Retrieved November 8, 2008 from http://www.cdc.gov/hiv/topics/surveillance/resources/factsheets/prevalence.htm.
- Centers for Disease Control and Prevention. Compendium of HIV Prevention Interventions with Evidence of Effectiveness. 2008c Retrieved November 8, 2008, from http://www.cdc.gov/hiv/resources/reports/hiv_compendium/
- Centers for Disease Control and Prevention. Best-Evidence Interventions. 2008d Retrieved November 8, 2008, from http://www.cdc.gov/hiv/topics/research/prs/best-evidence-intervention.htm.
- Centers for Disease Control and Prevention. Promising-Evidence Interventions. 2008e Retrieved November 8, 2008 from http://www.cdc.gov/hiv/topics/research/prs/promising-evidence-interventions.htm.
- Centers for Disease Control and Prevention. HIV and AIDS in the United States: A picture of today’s epidemic. 2008f Retrieved November 8, 2008, from http://www.beataids.org/files/CDC_HIV_US_Facts.pdf.
- Centers for Disease Control and Prevention. Best Evidence Interventions. 2009a Retrieved July 24, 2008 from http://www.cdc.gov/hiv/topics/research/prs/best-evidence-intervention.htm.
- Centers for Disease Control and Prevention. Promising Evidence Interventions. 2009b Retrieved July 24, 2008 from http://www.cdc.gov/hiv/topics/research/prs/promising-evidence-interventions.htm.
- Chesney MA. Factors affecting adherence to antiretroviral therapy. Clinical Infectious Diseases. 2000;30:S171–S176. doi: 10.1086/313849. [DOI] [PubMed] [Google Scholar]
- Chin J. The AIDS pandemic. The collision of epidemiology with political correctness. Oxford: Radcliffe Publishing; 2007. [Google Scholar]
- Coates TJ, Morin SF, McKusick L. Behavioral consequences of AIDS antibody testing among gay men. Journal of the American Medical Association. 1987;258:1989. [PubMed] [Google Scholar]
- Cornman D. personal communication. 2008. Nov 8,
- Cornman DH, Kiene SM, Christie S, Fisher WA, Shuper PA, Pillay S, et al. Clinic-based intervention reduces unprotected sexual behavior among HIV-infected patients in KwaZulu-Natal, South Africa: Results of a pilot study. Journal of Acquire Immune Deficiency Syndromes. 2008;48:553–560. doi: 10.1097/QAI.0b013e31817bebd7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crandall CS, Eshleman A. A justification—suppression model of the expression and experience of prejudice. Psychological Bulletin. 2003;129:414–446. doi: 10.1037/0033-2909.129.3.414. [DOI] [PubMed] [Google Scholar]
- Crawford AM. Stigman associated with AIDS: A meta-analysis. Journal of Applied Social Psychology. 1996;26:398–416. [Google Scholar]
- Crepaz N. Personal Communication. 2008. Jan 31,
- Crepaz N, Lyles CM, Wolitski RJ, Passin WF, Rama SM, Herbst JH, et al. Do prevention interventions reduce HIV risk behaviours among people living with HIV? A meta-analytic review of controlled trials. AIDS. 2006;20:143–157. doi: 10.1097/01.aids.0000196166.48518.a0. [DOI] [PubMed] [Google Scholar]
- Darrow WW. Public health and HIV prevention. Old, new, and not. Paper presented at the Center for Health, Intervention, and Prevention, University of Connecticut; Storrs, CT. 2004. Apr 4, [Google Scholar]
- Des Jarlais D, Friedman SR. The psychology of preventing AIDS among intravenous drug users. A social learning conceptualization. American Psychologist. 1988 Nov;:865–870. doi: 10.1037/0003-066X.43.11.865. [DOI] [PubMed] [Google Scholar]
- Devine PG, Monteith MJ, Zuwerink JR, Elliot AJ. Prejudice with and without compunction. Journal of Personality and Social Psychology. 1991;60:817–830. [Google Scholar]
- DiClemente RJ, Boyer CB, Mills SJ. Prevention of AIDS among adolescents: Strategies for the development of comprehensive risk reduction health education programs. Health Education Resarch Theory and Practice. 1987;2:287–291. [Google Scholar]
- Elliot AJ, Devine PG. On the motivational nature of cognitive dissonance. Dissonance as psychological discomfort. Journal of Personality and Social Psychology. 1994;67:382–398. [Google Scholar]
- Emmons C, Joseph JG, Kessler RC, Wortman CB, Montgomery SB, Ostrow DG. Psychosocial predictors of reported behavior change in homosexual men at risk for AIDS. Health Education Quarterly. 1986;13:331–345. doi: 10.1177/109019818601300405. [DOI] [PubMed] [Google Scholar]
- Festinger L. A theory of cognitive dissonance. Evanston, IL: Row Peterson; 1957. [Google Scholar]
- Fischl MA, Dickinson GM, Scott GB, Kimas N, Fletcher MA, Parks W. Evaluation of heterosexual partners, children, and household contacts of adults with AIDS. Journal of the American Medical Association. 1987;257:640–644. [PubMed] [Google Scholar]
- Fishbein M, Ajzen I. An introduction to theory and research. Reading, MA: Addison-Wesley; 1975. Belief, attitude, intention, and behavior. [Google Scholar]
- Fishbein M, Middlestadt SE. Using the Theory of Reasoned Action as a framework for understanding and changing AIDS-related behaviors. In: Mays VE, Albee GW, Schneider SF, editors. Primary prevention of AIDS. Psychological approaches. Primary prevention of psychopathology. XIII. Thousand Oaks, CA: Sage; 1989. pp. 93–110. [Google Scholar]
- Fisher JD. Possible effects of reference group-based social influence on AIDS-risk behavior and AIDS prevention. American Psychologist. 1988;43:914–920. doi: 10.1037//0003-066x.43.11.914. [DOI] [PubMed] [Google Scholar]
- Fisher JD, Cornman DH, Norton WE, Fisher WA. Involving behavioral scientists, health care providers, and HIV-infected patients as collaborators in theory-based HIV prevention and antiretroviral adherence interventions. Journal of Acquired Immune Deficiency Syndromes. 2006;43:10–17. doi: 10.1097/01.qai.0000248335.90190.f9. [DOI] [PubMed] [Google Scholar]
- Fisher JD, Cornman DH, Osborn CY, Amico KR, Fisher WA, Friedland GA. Clinician-initiated risk reduction intervneton for HIV-positive persons. Formative research, acceptability, and fidelity of the Options Project. Journal of Acquired Immune Deficiency Syndromes. 2004;37:S78–S87. doi: 10.1097/01.qai.0000140605.51640.5c. [DOI] [PubMed] [Google Scholar]
- Fisher JD, Fisher WA. Changing AIDS risk behavior. Psychological Bulletin. 1992;111:455–474. doi: 10.1037/0033-2909.111.3.455. [DOI] [PubMed] [Google Scholar]
- Fisher JD, Fisher WA. Theoretical approaches to individual-level change in HIV risk behavior. In: Peterson JL, DiClemente RJ, editors. Handbook of HIV prevention. New York: Kluwer Academic; 2000. pp. 3–55. [Google Scholar]
- Fisher JD, Fisher WA, Amico KR, Harman JJ. An Information–Motivation–Behavioral Skills Model of adherence to antiretroviral therapy. Health Psychology. 2006;25:462–473. doi: 10.1037/0278-6133.25.4.462. [DOI] [PubMed] [Google Scholar]
- Fisher JD, Fisher WA, Cornman DH, Amico KR, Bryan A, Friedland GH. Clinician-delivered intervention during routine clinical care reduces unprotected sexual behavior among HIV-infected patients. Journal of Immune Deficiency Syndromes. 2006;41:44–52. doi: 10.1097/01.qai.0000192000.15777.5c. [DOI] [PubMed] [Google Scholar]
- Fisher WA, Fisher JD. A general social psychological model for changing AIDS risk behavior. In: Pryor J, Reeder G, editors. The social psychology of HIV infection. Hillsdale, NJ: Erlbaum; 1993. pp. 127–153. [Google Scholar]
- Frieden TR, Das-Douglas M, Kellerman SE, Henning KJ. Applying public health principles to the HIV epidemic. New England Journal of Medicine. 2005;353:2397–2402. doi: 10.1056/NEJMsb053133. [DOI] [PubMed] [Google Scholar]
- Gay Men’s Health Crisis. GMHC: Gay Men’s Health Crisis. 2008 Retrieved November 8, 2008, from http://www.gmhc.org.
- Global HIV Prevention Working Group. HIV prevention in the era of expanded treatment access. 2004 Retrieved November 8, 2008, from http://www.kff.org/hivaids/upload/HIV-Prevention-in-the-Era-of-Expanded-Treatment-Access.pdf.
- Globe and Mail. The Globe and Mail. 2008. Oct 22, p. A5. [Google Scholar]
- God’s Love We Deliver. God’s Love We Deliver. 2008 Retrieved November 8, 2008, from http://www.godslovewedeliver.org.
- Gottlieb MS. AIDS—past and future. New England Journal of Medicine. 2001;344:1788–1791. doi: 10.1056/NEJM200106073442312. [DOI] [PubMed] [Google Scholar]
- Hahn BH, Shaw GM, De Cock KM, Sharp PM. AIDS as a zoonosis: Scientific and public health implications. Science. 2000;287:607–614. doi: 10.1126/science.287.5453.607. [DOI] [PubMed] [Google Scholar]
- Hall HI, Song R, Rhodes P, Prejean J, An Q, Lee LM, et al. Estimation of HIV incidence in the United States. Journal of the American Medical Association. 2008;30:520–529. doi: 10.1001/jama.300.5.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herek GM, Capitano JP. AIDS stigma and sexual prejudice. American Behavioral Scientist. 1999;42:1126–1143. [Google Scholar]
- Hyde JS, DeLamater JD, Byers ES. Human sexuality. Toronto: McGraw Hill Ryerson; 2001. Canadian edition. [Google Scholar]
- International AIDS Vaccine Initiative. IAVI.ORG Homepage. 2008 Retrieved November 8, 2008, from http://www.iavi.org/
- Jaccard JJ, Davidson AR. Towards an understanding of family planning behaviour: An initial investigation. Journal of Applied Social Psychology. 1972;2:228–235. [Google Scholar]
- Janssen RS, Holtgrave DR, Valdeisseri RO, Shephard M, Gayle HD, De Cock KM. American Journal of Public Health. 2001;91:1019–1024. doi: 10.2105/ajph.91.7.1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson BT, Carey MP, Chaudoir SR, Reid AE. Sexual risk reduction for persons living with HIV. Research synthesis of randomized controlled trials, 1993–2005. Journal of Acquired Immune Deficiency Syndromes. 2006;41:642–650. doi: 10.1097/01.qai.0000194495.15309.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson WD, Hedges LV, Ramirez G, Semaan S, Norman LR, Sogolow E, et al. HIV prevention research for men who have sex with men: A systematic review and meta-analysis. Journal of Acquired Immune Deficiency Syndromes. 2002;30:S118–S129. [PubMed] [Google Scholar]
- Kalichman SC, editor. Reducing HIV transmission among people living with HIV/AIDS. New York: Kluwer; 2005. Positive prevention. [Google Scholar]
- Kalichman JE, Andrew ME. HIV risk behavior reduction following intervention with key opinion leaders of population: an experimental analysis. American Journal of Public Health. 1991;81:168–171. doi: 10.2105/ajph.81.2.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Rompa D, Cage M, DiFonzo K, Simpson D, Austin J, et al. Effectiveness of an intervention to reduce HIV transmission risks in HIV-positive people. American Journal of Preventive Medicine. 2001;21:84–92. doi: 10.1016/s0749-3797(01)00324-5. [DOI] [PubMed] [Google Scholar]
- Karon JM, Fleming PL, Steketee RW, De Cock KM. HIV in the United States at the turn of the century: An epidemic in transition. American Journal of Public Health. 2001;91:1060–1068. doi: 10.2105/ajph.91.7.1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelley JA, St Lawrence JS. Behavioral intervention and AIDS. The Behavior Therapist. 1986;6:121–125. [Google Scholar]
- Kelley JA, St Lawrence JS. Psychological and social interventions. New York: Plenum; 1988. The AIDS health crisis. [Google Scholar]
- Kelly JA, St Lawrence JS, Diaz YE, Stevenson LY, Hauth AC, Brasfield TL, et al. HIV risk behavior reduction following intervention by key opinion leaders in population: An experimental analysis. American Journal of Public Health. 1991;81:168–171. doi: 10.2105/ajph.81.2.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JA, St Lawrence JS, Diaz YE, Stevenson LY, Hauth AC, Brasfiedd TL, et al. Timing the ancestor of the HIV-1 pandemic strains. Science. 2000;288:1789–1796. doi: 10.1126/science.288.5472.1789. [DOI] [PubMed] [Google Scholar]
- Kozol MJ, Amico R, Chiarella C, Cornoman D, Fisher WA, Fisher JD, et al. A population-based and longitudinal study of sexual behavior and multidrug resistant HIV among patients in clinical care. eJournal of the International AIDS Society. 2006;8:72. [PMC free article] [PubMed] [Google Scholar]
- Kunda Z. The case for motivated reasoning. Psychological Bulletin. 1990;108:480–498. doi: 10.1037/0033-2909.108.3.480. [DOI] [PubMed] [Google Scholar]
- London Free Press. London Free Press; 2008. Nov 6, p. C1. [Google Scholar]
- Maes J. Blaming the victim: Belief in control or belief in justice. Social Justice Research. 1994;7:69–90. [Google Scholar]
- Mann JM, Tarantola DJM, Netter TW, editors. AIDS in the world. New York: Oxford University Press; 1992. [Google Scholar]
- Mann JM, Tarantola DJM, editors. AIDS in the world II. Global dimensions, social roots, and responses. New York: Oxford University Press; 1996. [Google Scholar]
- Marks G, Crepaz N, Janssen RS. Estimating sexual transmission of HIV from persons aware and unaware that they are infected with the virus in the USA. AIDS. 2006;20:1447–1450. doi: 10.1097/01.aids.0000233579.79714.8d. [DOI] [PubMed] [Google Scholar]
- Marks G, Crepaz N, Senterfitt JW, Janssen RS. Meta-analysis of high-risk sexual behavior in persons aware and unaware the are infected with HIV in the United States: Implications for HIV prevention programs. Journal of Acquired Immune Deficiency Syndromes. 2005;39:446–453. doi: 10.1097/01.qai.0000151079.33935.79. [DOI] [PubMed] [Google Scholar]
- Mays VE, Albee GW, Schneider SF, editors. Primary prevention of psychopathology. XIII. Thousand Oaks, CA: Sage; 1989. Primary prevention of AIDS. Psychological approaches. [Google Scholar]
- Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations. Conceptual issues and research evidence. Psychological Bulletin. 2003;129:674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moatti JP, Souteyrand Y. Editorial: HIV/AIDS social and behavioural research: Past advances and thoughts about the future. Social Science and Medicine. 2000;50:1519–1532. doi: 10.1016/s0277-9536(99)00462-1. [DOI] [PubMed] [Google Scholar]
- Morbidity and Mortality Weekly Report. CDC. Morbidity and Mortality Weekly Report. Vol. 30. Los Angeles: 1981. Jun 15, Pneumocystis pneumonia; pp. 250–52. [PubMed] [Google Scholar]
- Nahmias AJ, Weiss J, Yao X, Lee F, Kodsi R, Schanfield M, et al. Evidence for human infection with an HTLV III/LAV-like virus in Central Africa, 1959. Lancet. 1986;31:1279–80. doi: 10.1016/s0140-6736(86)91422-4. [DOI] [PubMed] [Google Scholar]
- National Institutes of Health. National Institutes of Health Consensus Development Statement on Interventions to Prevention HIV Risk Behaviors. Bethesda, MD: NIH Office of Medical Applications Research; 1997. [Google Scholar]
- National Institutes of Health. AIDS history website. 2008 Retrieved November 8, 2008, from http://history.nih.gov/NIHInOwnWords/index.html.
- Noar S. Behavioral interventions to reduce HIV-related sexual risk behavior: Review and synthesis of meta-analytic evidence. AIDS and Behavior. 2008;12:335–353. doi: 10.1007/s10461-007-9313-9. [DOI] [PubMed] [Google Scholar]
- Porco TC, Martin JN, Page-Shafer KA, Cheng A, Charlebois E, Grant RM, et al. Decline in HIV infectivity following the introduction of highly active antiretroviral therapy. AIDS. 2004;18:81–88. doi: 10.1097/01.aids.0000096872.36052.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- President’s Emergency Plan for AIDS Relief. Reauthorizing PEPFAR. 2008 doi: 10.1097/QAD.0b013e32833cbb41. Retrieved November 8, 2008, from http://www.pepfar.gov/press/107735.htm. [DOI] [PubMed]
- Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: Toward an integrative model of change. Journal of Consulting and Clinical Psychology. 1985;51:390–395. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- Rollnick S, Mason P, Butler C. A guide for practitioners. London: Churchill Livingstone; 1999. Health behavior change. [Google Scholar]
- Rosenbrock R, Dubois-Arber F, Moers M, Pinell P, Schaeffer D, Setbon M. The normalization of AIDS in Western European countries. Social Science and Medicine. 2000;50:1607–1629. doi: 10.1016/s0277-9536(99)00469-4. [DOI] [PubMed] [Google Scholar]
- Rotter J, Chance JE, Phares EJ. Applications of a social learning theory of personality. New York: Holt, Rinehart & Winston; 1972. [Google Scholar]
- Schiltz MA, Sandfort ThGM. HIV-positive people, risk, and sexual behavior. Social Science and Medicine. 2000;50:1607–1629. doi: 10.1016/s0277-9536(99)00466-9. [DOI] [PubMed] [Google Scholar]
- Semaan S, Kay L, Strouse D, Sogolow E, Mullen PD, Neumann MS, et al. A profile of U.S.-based trials of behavioral and social interventions for HIV risk reduction. Journal of Acquired Immune Deficiency Syndromes. 2002;30:S30–S50. [PubMed] [Google Scholar]
- Sepkowitz KA. AIDS—the first 20 years. New England Journal of Medicine. 2001;344:1764–1772. doi: 10.1056/NEJM200106073442306. [DOI] [PubMed] [Google Scholar]
- Shilts R. And the band played on. People, politics, and the AIDS epidemic. New York: St. Martin’s Press; 1987. [Google Scholar]
- Slater P. Sutton’s law and AIDS prevention in Israel. Public Health Review. 1994;21:285–291. [PubMed] [Google Scholar]
- Solomon MZ, DeJong W. Recent sexually transmitted disease prevention efforts and their implications for AIDS health education. Health Education Quarterly. 1986;13:301–316. doi: 10.1177/109019818601300403. [DOI] [PubMed] [Google Scholar]
- Stall R, Mills TC. Editorial. A quarter century of AIDS. American Journal of Public Health. 2006;96:959–961. doi: 10.2105/AJPH.2006.089086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stall R. Prevention with positives. A critical literature review; Paper presented at the New York HIV Consortium; New York. 2007. Nov, [Google Scholar]
- UNAIDS. Global Summary of the AIDS Epidemic. 2008a Dec;284:1. Retrieved November 8, 2008 from http://data.unaids.org/pub/GlobalReport/2008/20080715_globalreport_coreslides_enppt#. [Google Scholar]
- UNAIDS. Substantial increases in HIV prevention efforts producing results, but not enough to turn back the epidemic. 2008b Retrieved November 8, 2008, from http://data.unaids.org/pub/GlobalReport/2008/080725_GR08_pressrelease_en.pdf.
- UNAIDS. Practical Guidelines for Intensifying HIV Prevention. Towards Universal Access. 2008c Retrieved November 8, 2008, from http://data.unaids.org/pub/Manual/2007/20070306_Prevention_Guidelines_Towards_Universal_Access_en.pdf.
- Wainberg MA, Friedland G. Public health implications of antiretroviral therapy and HIV drug resistance. Journal of the American Medical Association. 1998;379:1977–1983. doi: 10.1001/jama.279.24.1977. [DOI] [PubMed] [Google Scholar]
- Wolitski RJ, Bailey C, O’Leary A, Gomez C, Parsons J the Seropositive Urban Men’s Study Gourp. Self-perceived responsibility of HIV-seropositive men for preventing HIV transmission to sex partners. AIDS and Behavior. 2003;7:363–372. doi: 10.1023/b:aibe.0000004728.73443.32. [DOI] [PubMed] [Google Scholar]
- Wolitski RJ, Flores SA, O’Leary A, Bimbi DS, Gomez CA. Beliefs about personal and social responsibility among HIV-seropositive men who have sex with men: Measurement and association with transmission risk behaviour. AIDS and Behavior. 2006;11:676–686. doi: 10.1007/s10461-006-9183-6. [DOI] [PubMed] [Google Scholar]