Abstract
Precise assessment of the biological behavior and progression of squamous epithelial lesions of the larynx with a view to predict the prognosis and therapeutic challenges remains an elusive goal. The knowledge and data regarding the expression of proliferative markers indicating the biological activity in different histological grades of squamous epithelial lesions are lacking till date. To evaluate the relationship between Ki67, p27 and p53 expression as well as topographic distribution of Ki67 with the histological subtypes or grades of laryngeal squamous intraepithelial and invasive lesions. Sixty-two consecutive cases with histologically documented intraepithelial and invasive squamous lesion were studied for Ki67, p27 and p53 expression. Mann–Whitney U, Kruskal–Wallis and Spearman’s correlation tests were used for statistical analysis. The mean Ki67 labeling index in hyperplasia, dysplasia and carcinoma were 12.15, 22.03 and 35.53 % respectively and this difference was statistically significant (P < 0.05). There was strong positive correlation between Ki67 labeling index and increasing grades of squamous lesions. p27 expression was progressively decreased and p53 expression was progressively increased as the lesions progressed from hyperplasia to dysplasia and dysplasia to carcinoma. The topographic distribution of Ki67 positive cells increased with progressive grades of dysplasia. The Ki67 labeling index correlates well with the histological grade of both intraepithelial and invasive lesions of the larynx. And the topographic distribution of Ki67 expression depends on the grade of the dysplasia. Hence, Ki67 expression has a definite role in predicting the biological behavior of the lesions.
Keywords: Ki67, p53, p27, Larynx, Immunohistochemistry, Dysplasia
Introduction
Spectrums of epithelial alterations are seen in the larynx. They range from hyperplasia, atypical hyperplasia, dysplasia, carcinoma in situ to invasive carcinoma. As the degree of dysplasia increases from mild to severe, so does the risk of malignant transformation [1].
It would be of great clinical value to be able to predict which patients with laryngeal dysplasia are at greater risk of progressing to frank carcinoma. The management of these identified patients may include chemo-preventive approaches, local surgical therapies such as cord stripping, or laser treatment, in addition to intensive smoking cessation programmes in an effort to prevent the subsequent development of cancer [2–4].
The diagnostic histological parameters deciding the progression of dysplasia to carcinoma include abnormal mitotic figures, mitotic activity, stromal inflammation, maturation level and nuclear pleomorphism. However, the histological assessment of the degree of laryngeal epithelial dysplasia is still largely subjective and there does not seem to be a sufficiently accurate means of predicting the evolution of laryngeal preneoplastic lesions to infiltrative carcinoma [5].
One of the most important issues of squamous intraepithelial lesions is the risk of malignant transformation. The prediction of clinical outcome, recurrence and discrimination of laryngeal hyperplasia to dysplasia to frank neoplasia is often difficult with the help of histological criteria alone [6].
Though histology is important in categorizing these pathological conditions, other ancillary techniques can improve the diagnostic skills by predicting the biological behavior. Several newer prognostic markers are increasingly being studied now-a-days. Among these, proliferative markers like Ki67 [7–13], proliferative cell nuclear antigen (PCNA) [7, 8, 12], epidermal growth factor receptor (EGFR) [7], Cyclin D1 [13], apoptotic factors (BCL-2, bax) [10], p53 [9–11, 13], p16 [9], p27 [14, 15], MDM-2 [13] have been studied by different groups.
The study was conducted to evaluate the relationship between Ki67, p27 and p53 expression as well as topographic distribution of Ki67 with the histological subtypes or grades of laryngeal squamous intraepithelial and invasive lesions.
Materials and Methods
This 2 year prospective study was performed on 62 cases of squamous (intraepithelial and invasive) lesions of the larynx after obtaining the proper approval from ethical committee and informed consent from the patient party who came to our ENT department during the study period (01.09.2009–31.08.2011).
Inclusion Criteria
-
(i)
All the clinically suspected cases of squamous intraepithelial and invasive lesions of the larynx and who had undergone laryngoscopic biopsy in the department of ENT within the study period.
-
(ii)
Patients who gave the consent and fully co-operated during study procedure.
-
(iii)
Patients with full prebiopsy clinical history.
Exclusion Criteria
-
(i)
The clinically suspected patients who are diagnosed as inflammatory lesions or non-squamous lesions after histopathological examination.
-
(ii)
Patients having history of previous chemotherapy or radiotherapy for head and neck region lesions.
Clinical profiles as well as gross and microscopic findings of biopsy specimens were noted. Histological categorization and grading was done following the WHO guidelines [16] in Haematoxylin and eosin (H&E) stained sections of formalin-fixed, paraffin-embedded tissue. The histological features and grades were independently evaluated by two examiners.
Immunohistochemical Analysis
All the specimens were fixed in 10 % formalin and routine paraffin sections were made and stained with H&E. Sections were cut at 3–4 micrometer thickness and mounted on poly-L-Lysine coated slides. The sections were deparaffinized in xylene and rehydrated in alcohol. Antigen retrieval was done. Endogenous peroxidase was blocked with 3 % H2O2. Then the sections were incubated in humidifying chamber with primary antibodies (Ki67, p27, p53) for 60 min. Antibodies used were pre diluted antibody from Bio Genex (San Ramon, USA). The slides were then washed with tris buffer and secondary antibody was applied for 30 min. Then polymer HRP was added and incubated for 30 min. Thereafter the chromogen, di-amino benzidine (DAB) was added for 10 min as a substrate chromogen solution to produce a brown color. Finally the slides were immersed in Harris Haematoxylin for counterstaining.
Evaluation of Immunohistochemical Stain
For Ki-67, all identifiable nuclear staining was recorded as positive regardless of intensity. At least 5,000 cells were observed under a microscope (objective lens 40×) & counted vertically from one corner to another [7, 10]. The percentage of stained cells was evaluated three times independently by two examiners. Thus the result of Ki67 immunostaining index was interpreted as labeling index (Ki67 LI) = Number of nuclei showing positive staining (brown color)/Total number of nuclei × 100 %.
Results of p53 & p27 were considered positive when more than 10 % of cells exhibited immunopositivity & considered negative when less than 5 % cells exhibited immunopositivity. At least 6 high power fields (400×) were counted with a total of at least 500 cells including superficial, central & deep areas throughout the epithelium in intraepithelial lesions or tumor area of invasive lesions [13].
Statistical Analysis
The data was analyzed by Spearman’s correlation, Mann–Whitney U and Kruskal–Wallis tests using IBM SPSS statistics version 19. P value of 0.05 or less was considered to be statistically significant.
Results
Histopathological examination of these 62 cases revealed squamous hyperplasia in 7 cases, dysplastic epithelium (including mild, moderate, severe dysplasia or carcinoma in situ) in 23 cases and invasive squamous cell carcinoma (SCC) in 32 cases (including well, moderately and poorly differentiated carcinomas).
All the clinical parameters are summarized in Table 1. The mean age of presentation was 52.23 years for squamous intraepithelial and 59.38 years for squamous invasive lesions of larynx. There was male predominance (85.5 %; 53 out of 62 cases) in both squamous intraepithelial and invasive lesions. Majority of the cases (87.1 %; 54 out of 62 cases) of squamous lesions had a history of tobacco smoking. The commonest anatomical location of involvement for both squamous intraepithelial & invasive lesions was glottic/vocal cord region (59.7 %; 37 out of 62 cases).
Table 1.
Clinical variables of the study population
| Squamous lesions (n = 62) | Squamous intraepithelial lesions (n = 30) | Squamous invasive lesions (n = 32) | |
|---|---|---|---|
| Age (years) Mean ± SD |
55.85 ± 14.74 | 52.23 ± 16.99 | 59.38 ± 11.55 |
| Male patients | 53 (85.5 %) | 26 (86.67 %) | 27 (84.4 %) |
| Positive H/O tobacco smoking | 54 (87.1 %) | 25 (83.3 %) | 29 (90.6 %) |
| Location (supraglottic, glottic, subglottic) | 12 (19.3 %), 37 (59.68 %), 13 (20.97 %) | 7 (23.3 %), 16 (53.4 %), 7 (23.3 %) | 5(15.6 %), 21 (65.6 %), 6 (18.8 %) |
(SD Standard deviation)
Most common type of invasive lesion observed in our study was moderately differentiated SCC accounting for 59.4 % (19 out of 32 cases), whereas well differentiated SCC found in 8 out of 32 cases (25.0 %) and poorly differentiated SCC found in 5 out of 32 cases (15.6 %) (Table 2).
Table 2.
Distribution of cases according to histopathological diagnosis
| Histopathological diagnosis | Squamous lesions (n = 62) (%) | Squamous intraepithelial lesions (n = 30) (%) | Squamous invasive lesions (n = 32) (%) |
|---|---|---|---|
| Hyperplasia (HYP) | 7 (11.3) | 7 (23.3) | – |
| Mild dysplasia (MID) | 6 (9.7) | 6 (20.0) | – |
| Moderate dysplasia (MOD) | 7 (11.3) | 7 (23.3) | – |
| Severe dysplasia/carcinoma in Situ (SD/CIS) | 10 (16.1) | 10 (33.3) | – |
| Well differentiated SCC (WDSCC) | 8 (12.9) | – | 8 (25.0) |
| Moderately differentiated SCC (MDSCC) | 19 (30.6) | – | 19 (59.4) |
| Poorly differentiated SCC (PDSCC) | 5 (8.1) | – | 5 (15.6) |
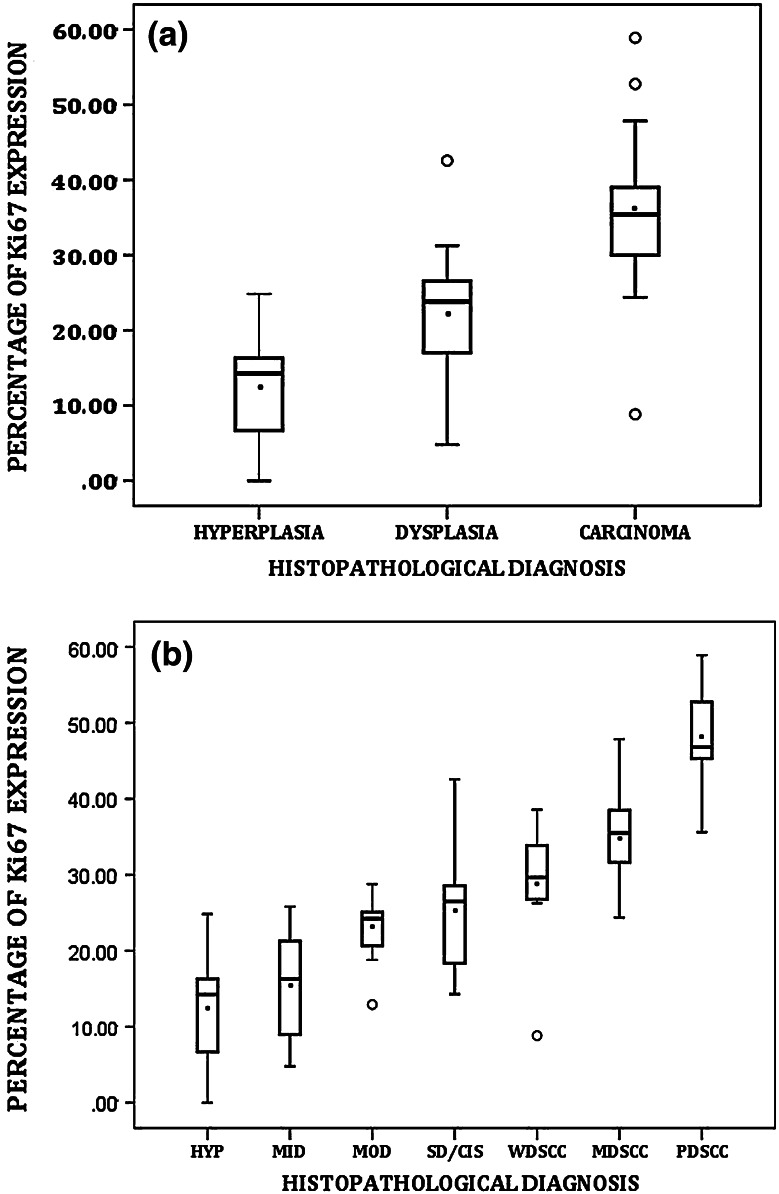
We determined Ki67 LI in all of the 62 cases of both squamous intraepithelial and invasive lesions. The mean Ki67 LI in hyperplasia, dysplasia and carcinoma were 12.15, 22.03 and 35.53 % respectively (Table 3; Fig. 1). It was also observed that Ki67 LI progressively increased from hyperplasia through increasing grades of dysplasia, to progressive grades of carcinoma and this difference was also statistically significant (P value <0.001) (Figs. 2, 3, 4).
Table 3.
Percentage (%) of Ki67 expression (Ki67LI) in different histopathological categories
| Histopathological Category | Histopathological diagnosis | Mean ± SD | Mean rank | Test statistics |
|---|---|---|---|---|
| Hyperplasia (12.15 ± 8.95) | Hyperplasia (HYP) | 12.15 ± 8.95 | 9.14 | Kruskal–Wallis = 40.656 Degree of freedom, df = (7–1) = 6 P value < 0.001, very highly significant |
| Dysplasia (22.03 ± 8.2) | Mild dysplasia (MID) | 15.57 ± 7.8 | 12.33 | |
| Moderate dysplasia (MOD) | 22.50 ± 5.2 | 20.43 | ||
| Severe dysplasia/carcinoma in Situ (SD/CIS) | 25.59 ± 8.3 | 27.25 | ||
| Squamous cell carcinoma (SCC) (35.53 ± 9.4) | Well differentiated SCC (WDSCC) | 28.50 ± 8.9 | 33.81 | |
| Moderately differentiated SCC (MDSCC) | 35.25 ± 6.3 | 44.37 | ||
| Poorly differentiated SCC (PDSCC) | 47.89 ± 8.7 | 57.20 |
(SD Standard deviation)
Fig. 1.
a Box-Whisker plot showing distribution of Ki67 expression in hyperplasia, dysplasia and carcinoma. b Box-Whisker plot showing distribution of Ki67 expression in hyperplasia, three grades of dysplasia and three types of carcinoma
Fig. 2.
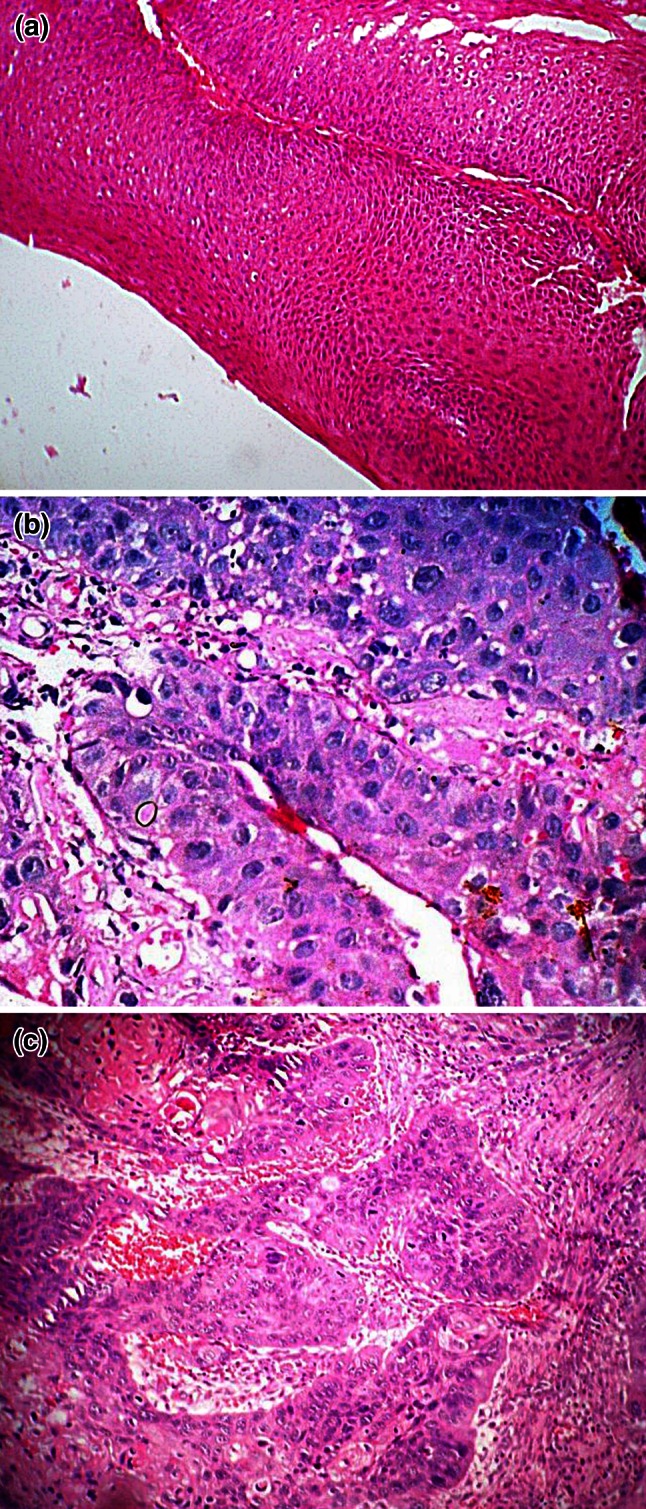
a Photomicrograph showing low power view of hyperplasia (H&E, ×100). b Photomicrograph showing high power view of severe dysplasia (H&E, ×400). c Photomicrograph showing high power view of moderately differentiated squamous cell carcinoma (H&E, ×400)
Fig. 3.
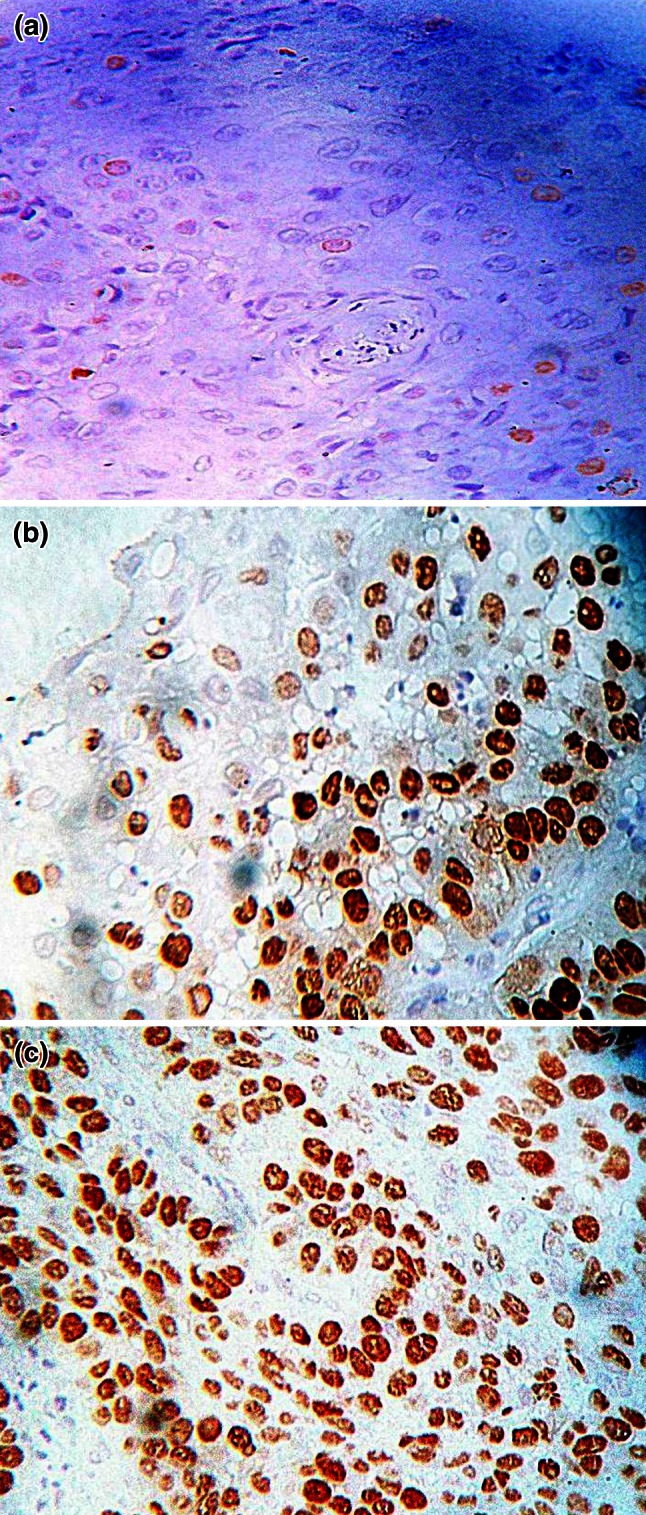
a Photomicrograph showing low level of Ki67 expression in hyperplasia (IHC, ×100). b Photomicrograph showing high level of Ki67 expression in severe dysplasia (IHC, ×400). c Photomicrograph showing higher level of Ki67 expression in moderately differentiated SCC (IHC, ×400)
Fig. 4.
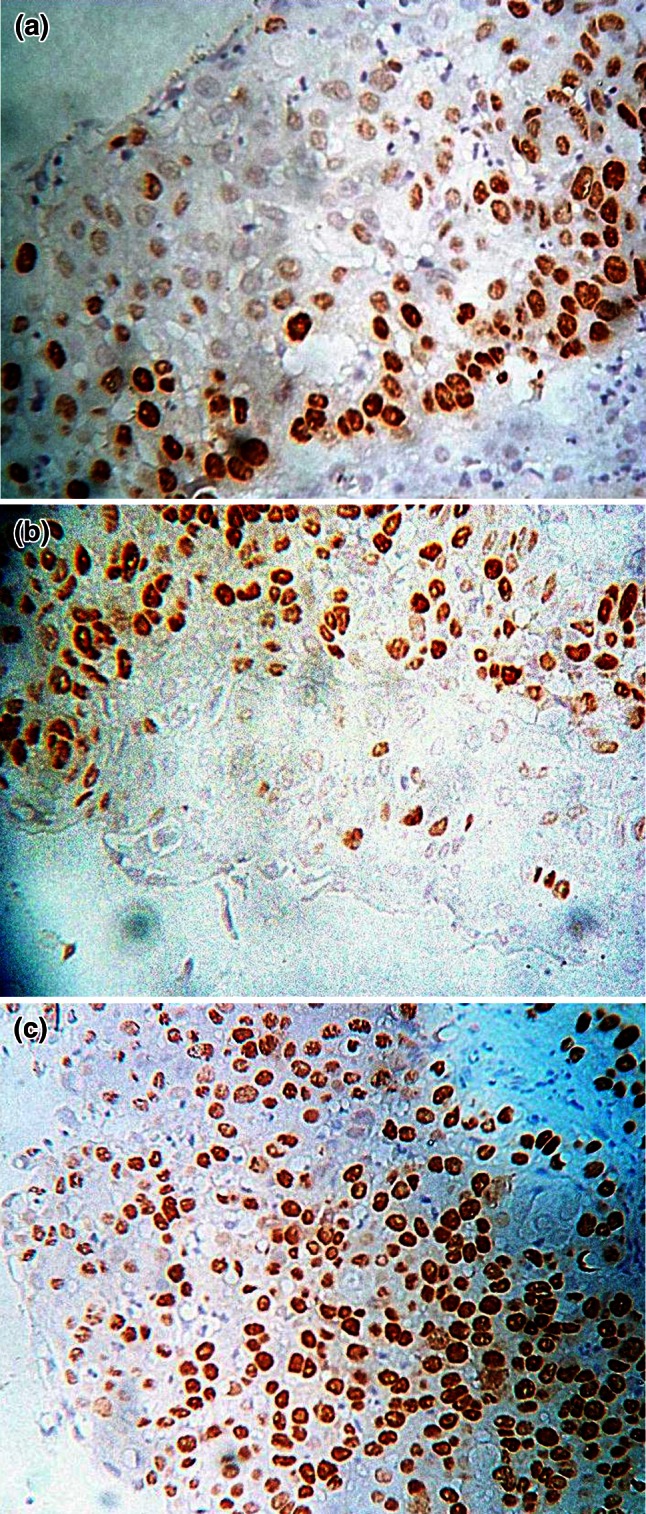
a Photomicrograph showing topographic distribution of Ki67 immuno-staining located within lower one-third in case of mild dysplasia (IHC, ×100). b Photomicrograph showing topographic distribution of Ki67 immuno-staining occupying more than ½ thickness of epithelium in case of moderate dysplasia (IHC, ×100). c Photomicrograph showing topographic distribution of Ki67 immuno-staining occupying entire thickness of the epithelium in case of severe dysplasia/CIS (IHC, ×100)
We have also studied the topographic distribution of Ki67 expression in squamous intraepithelial lesions (Table 4), it was seen that in most of the cases of hyperplasia and mild dysplasia, the Ki67 positive cells were confined to the lower portion of mid epithelial zone. In most of the cases of moderate dysplasia, the Ki67 positive cells extended to the mid epithelial zone. In majority of the cases of severe dysplasia/carcinoma in situ (CIS) the Ki67 positive cells involved the more superficial strata (Fig. 4). There was significant strong positive correlation (Spearman’s correlation coefficient, ρ = 0.606, P value = 0.000) between topographic distribution of Ki67 expression and histopathological category.
Table 4.
Topographic distribution of Ki67 expression in squamous intraepithelial lesions (n = 30)
| Pattern category | Hyperplasia (n = 7) | Mild dysplasia (n = 6) | Moderate dysplasia (n = 7) | Severe dysplasia/carcinoma in situ (n = 10) | |
|---|---|---|---|---|---|
| 0 | No staining | 1 (14.3) | 0 (0.00) | 0 (0.00) | 0 (0.00) |
| 1 | Scattered positive cells in the basal layer | 1 (14.3) | 1 (16.7) | 0 (0.00) | 0 (0.00) |
| 2 | Scattered positive cells not encroaching mid-epithelial zone | 3 (42.9) | 2 (33.3) | 1 (14.3) | 1 (10.0) |
| 3 | Focal collections of positive cells extending to the mid-epithelial zone | 2 (28.6) | 2 (33.3) | 4 (57.1) | 3 (30.0) |
| 4 | Widespread positive activity involve more superficial strata | 0 (0.00) | 1 (16.7) | 2 (28.6) | 6 (60.0) |
(Figures in parenthesis are column percentages)
It was observed that expression of p53 progressively increased when squamous cell lesions converted from intraepithelial to invasive lesions and the expression of p27 progressively decreased as the condition progressed (Table 5).
Table 5.
p53 and p27 expression in cases of laryngeal hyperplasia, dysplasia and carcinoma
| Histopathological diagnosis | p53 expression | p27 expression | ||
|---|---|---|---|---|
| Positive | Negative | Positive | Negative | |
| Hyperplasia (n = 7) | 4 (57.0) | 3 (43.0) | 5 (71.4) | 2 (28.6) |
| Dysplasia (n = 23) | 14 (61.0) | 9 (39.0) | 7 (30.4) | 16 (69.6) |
| Carcinoma (n = 32) | 23 (72.0) | 9 (28.0) | 4 (12.5) | 28 (87.5) |
| Total | 41 (66.1) | 21 (33.9) | 16 (25.8) | 46 (74.2) |
(Figures in parenthesis are column percentages)
Regarding the comparative evaluation among Ki67 LI, p53 and p27 expression, it was observed that when the Ki67 LI increased progressively, the positivity of p27 expression progressively decreased and the positivity of p53 expression progressively increased (Table 6). Weak negative correlation (Spearman’s Correlation Coefficient, ρ = − 0.201) was found in between p53 and p27 expression, however it did not reach the statistical significance (P value = 0.117).
Table 6.
Results of Mann–Whitney U test in between two (positive and negative) groups –p53 or p27 positive and p53 or p27 negative depending on Ki67 expression
| p53 expression | No. of cases | Mean rank | Sum of ranks | Test statistics | |
|---|---|---|---|---|---|
| Percentage of Ki67 expression (Ki67 LI) | Positive | 41 | 35.15 | 1441 | Mann–Whitney U = 281 P value = 0.026, significant |
| Negative | 21 | 24.38 | 512 | ||
| p27 expression | No. of cases | Mean rank | Sum of ranks | Test statistics | |
| Positive | 16 | 20.75 | 332 | Mann–Whitney U = 196 P value = 0.006, highly significant | |
| Negative | 46 | 35.24 | 1621 |
Discussion
Many studies have been undertaken so far to analyze the role of Ki67, p53 and p27 in squamous intraepithelial and invasive lesions of the larynx and also to assess their significance as prognostic factors in predicting behavior of these lesions. Clinicopathological studies have mainly targeted carcinomas of high incidence and mortality, such as gastric carcinomas, colorectal carcinomas, and lung carcinomas, but clinicopathological studies on laryngeal carcinomas are scarce. The study of proliferative markers and tumor suppressors is an important field of research in the biology of cancer. In this study, we found a statistically significant correlation between Ki67, p27 and p53 expression with the different histological types of laryngeal squamous lesions.
In our study distribution of Ki67 staining in cancer was related to the level of cell differentiation. This finding supports the hypothesis that dysplastic lesions are the results of abnormal proliferation of the epithelial cell. Although there is limited literature available on topographic distribution, Krecicki et al. [7] found that in cases with mild and moderate dysplasia, Ki67 immuno positive cells were mainly located in the basal and suprabasal layers and in cases with severe dysplasia there was a significant increase in the number of positive cells above the basal layer. In a study by Zidar et al. [8], there was a significant increase in the number of positive cells above the basal cell layer corresponding to the augmented immature basaloid cells in abnormal and atypical hyperplasias which occupied the lower third in abnormal hyperplasia and occupied from two-thirds to the entire epithelial thickness in atypical hyperplasia. Wayne and Robinson [9] found that the height of Ki67 staining was similar in normal epithelium, keratotic/hyperplastic lesions and mildly dysplastic lesions. Ki67 staining height increased with increasing degree of dysplasia, being predominantly located within the lower one-third of the epithelium in mild dysplasia, within the lower and middle thirds in moderate dysplasia and within the middle and upper thirds in severe dysplasia/carcinoma in situ.
We have demonstrated a significant correlation between Ki67 expression and tumor grading. Izawa et al. [10], in a study of 67 cases with laryngeal SCC and 22 cases of squamous dysplasia, found that the expression of Ki67 in the poorly differentiated SCCs was significantly higher than that observed in the well differentiated SCCs. They also observed that the mean Ki67 index was 7.66 in the cases of well differentiated SCC and 20.79 in poorly differentiated SCC and the mean Ki67 index was 6.45 % for the dysplasias and 11.19 % for the SCCs, respectively. Krecicki et al. [7], observed that Ki67 staining increased markedly from well differentiated carcinoma to poorly differentiated carcinoma with a mean of 22.61 for grade I, 38.29 for grade II and 44.11 for grade III carcinomas. The study on 54 patients of laryngeal SCC done by Ashraf et al. [11], revealed that most grade I tumors (WDSCC) had a Ki67 labeling index <50 % and a labeling index ≥50 % was found mainly in high grade tumors, tumoral Ki67 expression correlated significantly with tumor grade. Sarafoleanu et al. [12] observed that Ki67 expression strongly correlated with the histological grading in a study on 71 cases of laryngeal SCC.
The present study revealed that p27 expression was gradually decreased as the severity of squamous histopathological lesions increased. Therefore it seems plausible that p27 is a negative regulator of the cell cycle in the larynx and that reduced expression of p27 protein reflects the potentiality of the malignant transformation in laryngeal precancerous lesion. This result was similar to the finding of Hirai et al. [14] and Salerno et al. [15]. Hirai and colleagues [14], observed positive p27 immunostaining in 60 % cases of hyperplasia, 31 % cases of dysplasia and 12 % cases of carcinoma on a study of 56 cases of laryngeal precancerous or cancerous lesions.
In our study of laryngeal lesions, p53 expression in laryngeal intraepithelial lesions was not significantly different from that in carcinoma but it tended to be higher in carcinoma and this finding was similar to that of Gallo et al. [17], Barbatis et al. [18], Gorgoulis et al. [19] and Oliveria et al. [20]. Gallo and colleagues [17] found that p53 was expressed in 66.7 % cases of preneoplastic lesion and in 73.3 % cases of laryngeal SCC. Barbatis et al. [18] found that among the 41 cases of invasive SCC of the larynx, 78 % cases regardless of histological grade, overexpressed p53 compared to only 30 % of cases of mild dysplasia. A gradual increase in p53 expression from mild to severe dysplasia (60 %) was also observed.
The results of p53 immunostaining on squamous epithelial lesions of the larynx is however controversial. In a study of 114 cases of untreated dysplasia of the larynx, Jeannon et al. [21] found that expression of p53 was not associated with cancer progression. In their study, Hirai et al. [14] revealed that p53 immunostaining was observed in 6 out of 20 cases of hyperplasia, 3 out of 19 cases of dysplasia and 7 out of 17 cases of carcinoma, no significant association was found between p53 and the histopathological findings.
Conclusions
The Ki67 labeling index correlates well with the histological grade of both intraepithelial and invasive lesions of the larynx. And the topographic distribution of Ki67 expression depends on the grade of the dysplasia. Hence, Ki67 expression has a definite role in predicting the biological behavior of the lesions. The expression of p53 was similar to that of Ki67 and its expression increased with progressive grades of dysplasia and carcinoma. Reduced expression of p27 was associated with progression of laryngeal squamous intraepithelial lesions to squamous invasive lesions.
Acknowledgments
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Lingen MW. Head and neck. In: Kumar V, Abbas AK, Fausto N, Aster JC, editors. Robbins and Cotran: pathologic basis of disease. 8. Philadelphia: Saunders Elsevier; 2009. pp. 739–762. [Google Scholar]
- 2.Mirza S, Jeannon JP, Soames J, Wilson JA. Is Ki67 a marker for the transformation of laryngeal dysplasia to carcinoma? Acta Otolaryngol. 2006;126:418–421. doi: 10.1080/00016480500416785. [DOI] [PubMed] [Google Scholar]
- 3.Plch J, Pár I, Navrátilová I, Bláhová M, Zavadil M. Long term follow-up study of laryngeal precancer. Auris Nasus Larynx. 1998;25:407–412. doi: 10.1016/S0385-8146(98)00041-8. [DOI] [PubMed] [Google Scholar]
- 4.Hirano M, Sato K. Laser surgery for epithelial hyperplasia of the vocal fold. Ann Otol Rhinol Laryngol. 1993;102:85–91. doi: 10.1177/000348949310200202. [DOI] [PubMed] [Google Scholar]
- 5.Blackwell KE, Fu YS, Calcaterra TC. Laryngeal dysplasia. A clinicopathologic study. Cancer. 1995;75:457–463. doi: 10.1002/1097-0142(19950115)75:2<457::AID-CNCR2820750208>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 6.Gale N, Michaels L, Luzar B, Poljak M, Zidar N, Fischinger J, et al. Current review on squamous intraepithelial: lesions of the larynx. Histopathology. 2009;54:639–656. doi: 10.1111/j.1365-2559.2008.03111.x. [DOI] [PubMed] [Google Scholar]
- 7.Krecicki T, Jeleń M, Zalesska-Krecicka M, Rak J, Szkudlarek T, Jeleń-Krzeszewska J. Epidermal growth factor receptor (EGFR), proliferating cell nuclear antigen (PCNA) and Ki-67 antigen in laryngeal epithelial lesions. Oral Oncol. 1999;35:180–186. doi: 10.1016/S1368-8375(98)00100-6. [DOI] [PubMed] [Google Scholar]
- 8.Zidar N, Gale N, Cör A, Kambic V. Expression of Ki-67 antigen and proliferative cell nuclear antigen in benign and malignant epithelial lesions of the larynx. J Laryngol Otol. 1996;110:440–445. doi: 10.1017/S0022215100133924. [DOI] [PubMed] [Google Scholar]
- 9.Wayne S, Robinson RA. Upper aerodigestive tract squamous dysplasia: correlation with p16, p53, pRb, and Ki-67 expression. Arch Pathol Lab Med. 2006;130:1309–1314. doi: 10.5858/2006-130-1309-UATSDC. [DOI] [PubMed] [Google Scholar]
- 10.Izawa H, Yonemitsu N, Shin T, Sugihara H. Histopathological analysis of apopotosis, and expression of p53, bcl-2, bax, and Ki-67 in laryngeal squamous cell carcinomas and dysplasia. Auris Nasus Larynx. 1999;26:317–330. doi: 10.1016/S0385-8146(99)00005-X. [DOI] [PubMed] [Google Scholar]
- 11.Ashraf MJ, Maghbul M, Azarpira N, Khademi B. Expression of Ki67 and p53 in primary squamous cell carcinoma of the larynx. Indian J Pathol Microbiol. 2010;53:661–665. doi: 10.4103/0377-4929.72019. [DOI] [PubMed] [Google Scholar]
- 12.Sarafoleanu D, Postelnicu V, Iosif C, Manea C, Sarafoleanu C. The role of p53, PCNA and Ki67 as outcome predictors in the treatment of laryngeal cancer. J Med Life. 2009;2:219–226. [PMC free article] [PubMed] [Google Scholar]
- 13.Pignataro L, Capaccio P, Pruneri G, Carboni N, Buffa R, Neri A, et al. The predictive value of p53, MDM-2, cyclin D1 and Ki67 in the progression from low-grade dysplasia towards carcinoma of the larynx. J Laryngol Otol. 1998;112:455–459. doi: 10.1017/S0022215100140769. [DOI] [PubMed] [Google Scholar]
- 14.Hirai T, Hayashi K, Takumida M, Ueda T, Hirakawa K, Yajin K. Reduced expression of p27 is correlated with progression in precancerous lesions of the larynx. Auris Nasus Larynx. 2003;30:163–168. doi: 10.1016/S0385-8146(03)00007-5. [DOI] [PubMed] [Google Scholar]
- 15.Salerno G, Di Vizio D, Staibano S, Mottola G, Quaremba G, Mascolo M, et al. Prognostic value of p27Kip1 expression in basaloid squamous cell carcinoma of the larynx. BMC cancer. 2006;6:146. doi: 10.1186/1471-2407-6-146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barnes L, Eveson JW, Reichart P, Sidransky D (eds) (2005) Pathology and genetics of head and neck tumours. IARC Press, Lyon, pp 107–162 (Kleihues P, Sobin LH, eds. World health organization classification of tumours series)
- 17.Gallo O, Franchi A, Chiarelli I, Porfirio B, Grande A, Simonetti L, et al. Potential biomarkers in predicting progression of epithelial hyperplastic lesions of the larynx. Acta Otolaryngol Suppl. 1997;527:30–38. doi: 10.3109/00016489709124030. [DOI] [PubMed] [Google Scholar]
- 18.Barbatis C, Loukas L, Grigoriou M, Nikolaou I, Tsikou-Papafragou A, Marsan N, et al. p53 overexpression in laryngeal squamous cell carcinoma and dysplasia. Clin Mol Pathol. 1995;48:M194–M197. doi: 10.1136/mp.48.4.M194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gorgoulis V, Zoumpourlis V, Rassidakis G, Karameris A, Barbatis C, Spandidos DA, et al. Molecular analysis of p53 gene in laryngeal premalignant and malignant lesions. p53 protein immunohistochemical expression is positively related to proliferating cell nuclear antigen labeling index. Virchows Arch. 1995;426:339–344. doi: 10.1007/BF00191341. [DOI] [PubMed] [Google Scholar]
- 20.de Oliveira DE, Bacchi MM, Macarenco RS, Tagliarini JV, Cordeiro RC, Bacchi CE. Human Papillomavirus and Epstein-Barr Virus Infection, p53 expression, and cellular proliferation in laryngeal carcinoma. Am J Clin Pathol. 2006;126:284–293. doi: 10.1309/UU2JADUEHDWATVM9. [DOI] [PubMed] [Google Scholar]
- 21.Jeannon JP, Soames JV, Aston V, Stafford FW, Wilson JA. Molecular markers in dysplasia of the larynx: expression of cyclin-dependent kinase inhibitors p21 and p27, and p53 tumour suppressor gene in predicting cancer risk. Clin Otolaryngol Allied Sci. 2004;29:698–704. doi: 10.1111/j.1365-2273.2004.00859.x. [DOI] [PubMed] [Google Scholar]