Abstract
Cystic artery pseudoaneurysm (CAP) is a very rare complication of acute cholecystitis. We present the unruptured cystic artery pseudoaneurysm of an oedematous, thick-walled gallbladder in a 71-year old gentleman admitted with acute calculus cholecystitis. This was managed by radiological microcoil embolisation, percutaneous drainage of pericholic fluid and conservative treatment with antibiotics.
INTRODUCTION
In 95% of cases of acute cholecystitis the cause is a gallstone blocking the cystic duct subsequently leading to inflammation of the gallbladder by chemicals or bacteria (1). This is otherwise known as calculous cholecystitis. The remaining 5% occur without gallstones (acalculous cholecystitis). The localised peritonitis that ensues means patients characteristically present with a history of severe, sudden onset, constant or colicky pain in the right upper quadrant (RUQ) with systemic upset such as nausea, vomiting and sweating (2). Complications of this condition include gangrenous cholecystitis, gallbladder perforation, cholecysto-enteric fistula, gallstone ileus (3) and, very rarely, cystic artery pseudoaneurysms (CAP), which can be associated with intra-abdominal and gastrointestinal haemorrhage (4).
CASE REPORT
A 71-year old Caucasian gentleman with a background of known gallstones and hypertension presented to the emergency department with a two-day history of sudden onset, severe RUQ pain associated with non-bilious vomiting. He had no fever, sweats, rigors or clinical jaundice. His past surgical history included an appendicectomy, bilateral inguinal herniae repair as well as a L5 laminectomy several years previously. Clinical examination revealed RUQ and epigastric tenderness with a slightly distended abdomen. Bowel sounds were normal. Cardiovascular and respiratory examinations were unremarkable. Blood tests revealed the following: Haemoglobin 12.7g/dL, leucocytes 23 x 109/L, neutrophils 20.7 x 109/L, Na 141mmol/L, bilirubin 36µmol/L, ALT 25u/L, ALP 101u/L, amylase 35u/L and CRP 332mg/L.
An abdominal ultrasound scan (USS) was performed the next day and reported multiple large gallstones with significant thickening of the gallbladder wall. The patient was treated with oxygen therapy, analgesia, intravenous piperacillin/tazobactam & metronidazole and a stat dose of gentamicin after discussion with the Consultant Microbiologist.
His condition remained stable; however, over the course of the next 7 days, he began spiking temperatures along with persistent RUQ pain and increasing leucocyte count. An abdominal USS was repeated which now demonstrated a single large calcified gallstone within a contracted gallbladder and a pulsatile mass around Hartman’s pouch with a large amount of free fluid around the liver. This fluid was extending into the right paracolic gutter and down to the right iliac fossa. A CT angiogram (Fig.1a & 1b) was done to delineate this pulsatile mass which confirmed a 3cm x 1.5cm cystic artery pseudoaneurysm (A) and a large collection (C) extending from the gall bladder fossa, surrounding the liver and extending down to the right paracolic gutter and into the pelvic brim. There was no suspicion of gallbladder perforation or empyema from the images obtained.
Figure 1a.
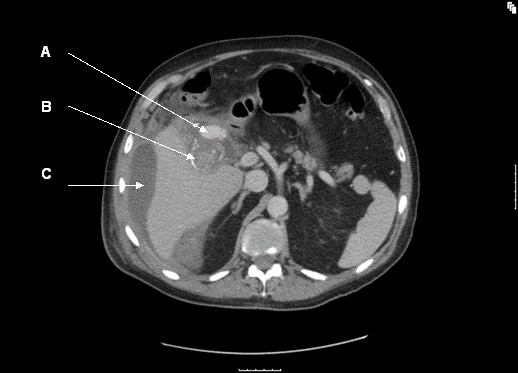
CT angiogram (A = cystic artery pseudoaneurysm; B = calcified gallstone; C = perihepatic fluid)
Figure 1b.
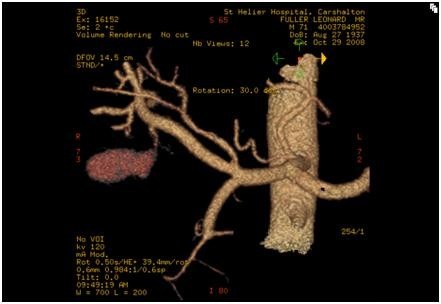
3d reconstruction of CT angiogram
The next step was for embolisation of the CAP. A transfemoral approach was employed and a microcoil placed successfully in the cystic artery (Fig. 2). A right sub-hepatic drain was placed, which drained a total of 1130ml of dark inflammatory fluid, in the first 24 hours. The patient clinically improved over the next 7 days, his inflammatory markers normalised and the drain was removed when dry. The patient was discharged home and laparoscopic cholecystectomy was arranged electively.
Figure 2.

Transfemoral microcoil embolisation of the cystic artery.
DISCUSSION
Unruptured CAP is a very rare complication of acute calculus cholecystitis. Our literature search struggled to find a similar case with concurrent acute inflammation without haemoperitoneum. Most cases of CAP are invariably associated with haemoperitoneum or haemobilia (5), and although colour doppler can be used to diagnose CAP, CT angiogram seems to yield a better diagnostic image.
Inflammation of the gallbladder may lead to changes in the cystic artery as a result of inflammation and fibrosis encasing the arterial wall and weakening it; resulting in aneurysm formation. These aneurysms are likely to rupture when the tamponising effect of the surrounding inflammatory fluid tension is lost, which is why drainage of the pericholic fluid was delayed until after embolisation was done.
We report here a conservative treatment after microcoil embolisation with antibiotics and percutaneous drainage of pericolic fluid. Our regime of antibiotics is intravenous piperacillin/tazobactam and metronidazole with a one off dose of gentamicin. The patient was kept nil orally, accurate fluid balance maintained and we noticed rapid improvement from a septic to non-septic picture. In conclusion, our experience with this case suggests that if a CAP is demonstrated, microcoil embolisation is effective in its management followed by percutaneous drainage of any pericholic fluid and intravenous antibiotics; saving the patient an emergency surgery.
REFERENCES
- 1.Indar AA, Beckingham IJ. Acute cholecystitis. BMJ 2002;325:639–643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Clinical knowledge Summaries 2008 Available from: http://cks.library.nhs.uk/cholecystitis_acute#-340132 [accessed 1st 2010]
- 3.Chen LE, Halpin V, Whinney R. Acute cholecystitis. Clinical Evidence. London: BMJ Publishing Group Ltd., 2006 [Google Scholar]
- 4.Saluja SS, et al. Acute cholecystitis with massive upper gastrointestinal bleed: a case report and review of the literature. BMC Gastroenterology 2007;7:12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kaman L, Kumar S, Behera A, Katariya RN. Pseudoaneurysm of the cystic artery: a rare cause of haemobilia. Am J Gastroenterol 1998;93:1535–1537 [DOI] [PubMed] [Google Scholar]


