Abstract
Household food insecurity has been previously hypothesized to promote dependence on inexpensive, highly palatable foods that are energy dense. Such dependence, and the cyclical nature of having enough food in the beginning of the month followed by food scarcity at the end of the month, could lead to weight gain over a short period of time. Such dependence on energy-dense foods and weight gain may play a direct role in the development of chronic conditions. Other compounding factors that result from exposure to household food insecurity have been well described, including pathways by which stress promotes visceral fat accumulation and chronic disease. This symposium review paper summarizes the literature on the link between food insecurity and the following: 1) diet, 2) weight gain, and 3) chronic disease, especially among women. This paper also proposes a framework for considering how the lived experience of household food insecurity may potentiate the development of chronic disease by activating the stress response among individuals at critical developmental periods in a food-impoverished environment.
Introduction
There has been recent speculation about whether food insecurity causes chronic disease. In cross-sectional analysis, a number of findings suggest that household food insecurity is linked to chronic disease. In particular, food insecurity has been significantly associated with type 2 diabetes, even after controlling for a number of covariates (1–3). Household food insecurity has been previously hypothesized to promote dependence on inexpensive, highly palatable foods that are energy dense. Such dependence, and the cyclical nature of having enough food in the beginning of the month followed by food scarcity at the end of the month, could lead to weight gain over a short period of time. This hypothesized mechanism depends on the following assumptions: 1) that households are dependent on inexpensive energy-dense foods, 2) that households experience a cyclic pattern of food consumption, and 3) that this mechanism happens over enough time to alter metabolism and result in a positive energy balance. Other compounding factors have been well described, including pathways by which stress can influence visceral fat accumulation and chronic disease. Under severe stress conditions, both the hypothalamus-pituitary-adrenal axis and reward pathways can contribute to the release of cortisol, neuropeptide Y, and other substances, causing a desire to consume high energy-dense foods and altered metabolism (4–7). In particular, these pathways can promote accumulation of the visceral fat that plays a critical role in chronic disease (8). Seligman and Schillinger (9) proposed a model of the Cycle of Food Insecurity and Chronic Disease that incorporates constrained dietary options, compensatory eating behaviors and strategy, and subsequent changes in health status and stress that work in a cyclical way to both increase disease onset and disease progression. Further compounding the story is the finding that if household food insecurity is experienced at critical developmental periods, then an individual may be particularly prone to metabolic syndrome (10). This symposium review paper summarizes the literature on the link between food insecurity and the following: 1) diet, 2) weight gain, and 3) chronic disease, especially among women. This paper also proposes a framework for considering how the lived experience of household food insecurity may potentiate the development of chronic disease by activating the stress response among individuals at critical junctures in their life course in a food impoverished environment.
Current status of knowledge
Food insecurity and compromised dietary intake and nutritional status
Evidence from animal models subjected to food scarcity as a stressor suggests that food intake is altered and a preference for high-fat, high-sugar foods is activated under stress conditions (4, 8, 11). Exposure to household food insecurity is associated with stress and depression (12–15), episodic food availability (16), household food shortages (17), and reliance on high energy-dense foods (18). A “new” model of comfort foods (8) suggests that stress activates the hypothalamic-pituitary-adrenal axis, releasing cortisol which can alter metabolic processes. In addition to the stress pathway being activated, 2 other systems are activated: the hedonic (reward) pathway and memory. This comfort food model is based on observations that within a very short time period, animals learn that the high-fat, high-sugar foods are rewards that dampen the stress response. As a result, the animal seeks the same food the next time stress is introduced, even with much lower stress stimuli.
Inherent in the definition and measure of household food security is the notion of compromised food quantity and/or food quality. This notion was largely born out of the qualitative research finding that women and families reported compromising on portion sizes, skipping meals, or eating the same foods throughout the day or over a period of time (16, 19). Findings from quantitative studies later confirmed this finding. Using the Cornell/Radimer measure of household food security, Kendall et al. (20) found that among a small sample (n = 193) of women in rural upstate New York living in food-insecure households had lower quantity of foods in the house compared with food-secure households. Household food availability was also characterized as cyclical during the month among low-income food-insecure households. Taren et al. (16) found that servings of food increased with participation in food programs, household size, and more sources of income. However, they also found that servings of food decreased in the last week of the month. In addition to lower quantity and poorer quality of foods, women living in food-insecure households also had a significant increase in disordered eating pattern scores characterized as binge eating (20).
Several observational studies using a convenience sample have shown associations between household food insecurity and inadequate intake of fruits, vegetables, and micronutrients (17, 20–22). Kendall et al. (20) found significantly lower levels of fruit, potassium, and fiber intake among food-insecure groups than among food-secure groups. The percentage of respondents consuming less than the RDA for vitamin C and <5 fruits and vegetables per day was significantly greater among food-insecure respondents than food-secure respondents. Tarasuk and Beaton (23) found that among a small sample of women (n = 153) receiving emergency food benefits in Toronto, Canada, women from very low food-secure households had lower energy intake and inadequate intakes in excess of 15% for vitamin A, folate, iron, and magnesium. The 15% cutpoint was used to indicate a sufficient reduction in essential nutrients that may put women at risk of nutrient deficiencies. Tarasuk (17) again studied the influence of household food insecurity on women’s health in the same sample and found a lower intake of fruits and vegetables and meat among women from food-insecure households compared with food-secure households. An array of coping mechanisms were identified in the same study, which included delaying or shuffling bill payment, discontinuing services, pawning possessions, or sending children to other houses to eat meals. Together, these descriptive studies suggest that household food insecurity is associated with decreased intake of fruits and vegetables and some nutrients.
Several observation studies using a representative sample have been conducted using the 1-item food insufficiency question (22, 24–27). Using data from the Current Population Study, Rose and Oliveira (24) assessed the association between food insufficiency and 15 nutrients and found that women and elderly adults from food-insufficient households had significantly lower mean intakes for the majority of nutrients assessed. Furthermore, women from food-insufficient households had greater odds of intake <50% of the RDA for energy; vitamins A, E, C, and B-6; magnesium; thiamin; and niacin, whereas the elderly had lower intakes of protein; vitamins A and B-6; calcium; phosphorus; thiamin; riboflavin; and niacin. In the same study, preschooler diets were found to be no more likely to have lower intake of any nutrients when comparing preschoolers from food-insufficient with those from food-sufficient households. Using data from NHANES III, Lee and Frongillo (26) found significantly lower intake of energy, protein, saturated fat, carbohydrates, B vitamins (niacin, riboflavin, B-6, and B-12), and minerals (magnesium, iron, and zinc) and significantly lower skinfold thickness among elderly adults from food-insufficient compared with those from food-sufficient households, after adjusting age, sex, race, income, education, living arrangement, food program participation, disease, and functional impairment. Dixon et al. (22), using data from NHANES III, reported that in age-stratified models of household food insufficiency, after adjustment for family income and other important covariates, younger adults (aged 20–59 y) from food-insufficient families had lower intakes of calcium and higher risk of calcium and vitamin E intakes below 50% of the RDA compared with young adults from food-sufficient households. Younger adults from food-insufficient families also reported lower 1-mo frequency of consumption of milk/milk products, fruits/fruit juices, and vegetables. They also had lower serum concentrations of total cholesterol, vitamin A and 3 carotenoids (α-carotene, β-cryptoxanthin, and lutein/zeaxanthin) compared with younger adults from food-sufficient families. In the same study, older adults (≥60 y) from food-insufficient families had lower intakes of energy, vitamin B-6, magnesium, iron, and zinc and were more likely to have iron and zinc intakes <50% of the recommended amount on a given day. Based on clinically relevant nutrient markers, older adults also had lower serum concentrations of HDL cholesterol, albumin, vitamin A, β-cryptoxanthin, and vitamin E. Both younger and older adults from food-insufficient families were more likely to have very low serum albumin (<35 g/L) than adults from food-sufficient families. The findings showed that adults from food-insufficient families have diets that may compromise their health.
In addition to identifying lower micronutrient intake associated with food insufficiency, several studies have found food insufficiency associated with poor dietary intake and significantly lower diet quality scores. Using a representative sample from Oregon, Cunningham et al. (27) found maternal food insufficiency was associated with lower fruit and vegetable intake and higher soda intake (but not candy or cookies, French fries, fast food, water, milk, other drinks) among 2-y-old children. Basiotis and Lino (25), using NHANES III data, calculated the Healthy Eating Index, a composite diet quality measure totaling 100 points consisting of 10 components including servings of grains, fruits, vegetables, milk, and meat and the percentage of energy from fat, saturated fat, cholesterol, and sodium intake as well as a food variety score. They found that women from food-insufficient households had a significantly lower Healthy Eating Index score than women from food-sufficient households (58.8 vs. 62.7, respectively), although scores for both indicated that both groups needed to improve dietary intake. Bhattacharya et al. (21), using NHANES III data, extended these analysis by assessing the association among food insufficiency, poverty, and nutritional status for all age groups and by race. Considering their data on the Healthy Eating Index, BMI (kg/m2) and an index of serum nutrient levels, the authors found that poverty is a better predictor of nutritional status for very young preschool children than household food insufficiency; however, both poverty and household food insufficiency were independent predictors of nutritional status for adults. Neither poverty nor household food insufficiency was associated with nutritional status among older children.
Two studies used the NHANES 1999–2002, which assessed household food insecurity using the 18-item Food Security Core Module (28). This module provides 4 categories of food insecurity: secure, marginally secure, insecure without hunger, and insecure with hunger. Lorson et al. (29) found no association with decreased fruit and vegetable intake among children by food security category. Zizza et al. (30) found no association with energy intake, carbohydrate intake, or total energy from meals for men or women by food security category. They found, however, that women and men from food-insecure households had fewer meal occasions compared with adults from food-secure households. Also, women had significantly higher total grams of fat and saturated fat, whereas men had lower grams of protein and a lower energy-dense diet, who were from households characterized as food insecure with hunger compared with adults from food-secure households. The authors concluded that meal occasions, or skipping meals, may be an important dietary factor for the overall health and well-being of individuals from food-insecure households.
Many studies have shown an association between household food insecurity and lower fruit and vegetable intake and a lower dietary intake of a number of micronutrients across studies for women (16, 17, 20, 23, 24) and older Americans (21, 22, 26, 31). Although many of these studies used inconsistent measures of food security status and nutrition outcomes, used small nonrepresentative sample sizes, or may have relied on cross-sectional study designs, their findings have been remarkably consistent. There is also evidence that households do go through episodic and cyclical food shortages (16, 23). Finally, the evidence that can demonstrate an association between household food insecurity and increased caloric, added sugar, high fat, or processed foods intake is either nonexistent or finds no association (22, 30). Future studies will need to substantiate the role that household food insecurity may play in promoting energy-dense foods. Longitudinal studies are needed to demonstrate a causal relationship between household food security status and duration on dietary intake.
Food insecurity and weight gain
A second possible pathway between household food insecurity and diet-related chronic disease is through weight gain and obesity. In 1995, a medical case report by Dietz (32) hypothesized that food insecurity might influence weight gain through dependence on high-fat foods or physiologic response to cyclical food shortages. Overall, the literature on the association between household food insecurity and weight status is inconsistent. Two reviews of the literature focusing on food insecurity and child weight status (33, 34) came to the same conclusion, that only a limited number of studies support the association between household food insecurity and overweight or obesity among children. Eisenmann et al. (34) reviewed the literature that focused on children and categorized studies based on the analytical methods used to assess the food insecurity and weight status relationship. A consistent finding was that food insecurity and overweight status in children do coexist, but there is limited research that can support a causal relationship. Most studies either found a statistically significant association between household or child food insecurity and higher weight status or a nonsignificant yet elevated relationship.
The relationship between exposure to household food insecurity and weight status among children may need a life course framework within which to interpret findings and direct future studies. Borrowing from animal studies of bonnet macaque monkeys, a species of Old World monkeys, a biological mechanism is provided that may offer additional insight into the relationship between household food insecurity and weight status. In 1984, the variable foraging demand (VFD) protocol was developed to assess maternal-child attachment and anxiety disorders (35). The protocol consisted of 3 groups of mother macaques that were subjected to 3 conditions: low foraging demands that were basically ad libitum feeding, high foraging demands (HFDs) in which food was hidden in the environment but the mother needed to work to find enough food, and variable foraging demands (VFDs) that alternated every 2 wk between low and high conditions for a period of 16 wk. This initial study found that under the low foraging demand condition, the mother macaques attended to their offspring, engaged in grooming activities, and showed less dominant behaviors, whereas mother macaques exposed to VFD displayed the highest level of dominant behaviors and the lowest level of grooming activities. Offspring of the mother macaques exposed to VFD clung more to their mothers and played less. These findings suggest that the rapid changes in the availability of food, even when calories were not restricted, led to dramatic behavior changes and disruptions in maternal-offspring interactions. Using the same protocol, a series of studies demonstrate that the VFD condition leads to a stress response in mothers and offspring (10, 36–38). Kaufman et al. (10) equated the VFD condition to household food insecurity experienced by humans and found that maternal exposure to VFD during offspring infancy was associated at 3–4 y with greater weight gain, higher BMI, greater abdominal circumference, and indicators of insulin resistance, with females showing more signs of insulin resistance and metabolic syndrome. Kaufman et al. concluded that maternal food insecurity, a significant source of early life stress, experienced for a relatively short duration but at a critical developmental stage for offspring, may lead to the development of obesity and metabolic syndrome during the prepubertal period. In humans, it is therefore hypothesized that maternal food insecurity may lead to the manifestation of child weight gain, especially visceral adiposity, during the prepubertal or pubertal period.
Using NHANES data, a significant interaction between household food security and maternal stress was associated with elevated weight among 3- to 10-, but not 11- to 17–y-old children among a sample of low-income yet food-secure households (39). Conversely, Lohman et al. (40) found that the interaction between household food insecurity and maternal stress was associated with elevated weight among 10- to 15-y old children in a sample of urban-dwelling low-income families using data from the Three Cities Study (40). Longitudinal studies are needed that can account for the level and intensity of food insecurity, the developmental period during which food insecurity was experienced, as well as the type of additional stress exposures to demonstrate causal linkages between household food insecurity and weight status among children and subsequent chronic disease development.
The review article by Larson and Story (33) concluded that the association between household food insecurity and weight status among men is inconclusive, with most studies finding no relationship and 2 studies showing a decreased risk of overweight among men from food-insecure compared with food-secure households. Among adult women, although mixed, there are more consistent findings for an association between household food insecurity and overweight or obesity (33). More recently, a population-based study with pooled data from the 2009 Behavioral Risk Factor Surveillance System from 12 states found that in sex-stratified models, women with food insufficiency had a significant (48%) greater risk of obesity [adjusted OR=1.48 (95% CI: 1.27,1.72)] among adults reporting food sufficiency after controlling for a number of socioeconomic characteristics. A study by Gooding et al. (41), using data from wave 4 of the National Longitudinal Study of Adolescent Health (2007–2008), a large representative sample, found that food insufficiency was associated with a significantly higher BMI among women (β = 0.89, SE = 0.44, P < 0.05) but not among men compared with young adults from food-sufficient households, after controlling for a number of socioeconomic, health behavior characteristics, and food stamp use. Although the last 2 studies were also cross-sectional studies and used the 1-item food sufficiency question, they are notable because they used large population-based samples, were reported findings since the economic down turn, and found an association among women but not men. In the case of the Gooding et al. article, the sample focused on women of reproductive age and found a clinically meaningful and significantly higher BMI, which may have implications for pregnancy. Longitudinal studies have also resulted in mixed findings (33). The question remains whether these 2 conditions are causally linked or whether they simply coexist.
Among pregnant women, food insecurity is associated with higher levels of perceived stress, anxiety, and depression and lower levels of self-esteem and mastery (12). One study found that food insecurity was not associated with substantial weight gain (>4.5 kg) during pregnancy; however, being obese and experiencing food insecurity during pregnancy was associated with greater risk of major gestational weight gain (42). This suggests that food insecurity may exacerbate weight gain among women who are more prone to store energy as weight. Another study found that household food insecurity was associated with greater gestational weight gain compared with gestational weight gain in pregnant women from food-secure households (43).
Food insecurity and prevalence of chronic disease and chronic disease risk factors
In the general population, household food insecurity has been shown to be associated with markers of chronic disease risk and chronic conditions. Food insecurity among low-income families is associated with a significantly higher percentage of diabetes in community samples (1, 44) and studies with representative samples in the United States and Canada (2, 3, 45), especially among women (44, 45). In addition to diabetes, results from analyses using NHANES indicate that household food insecurity was associated with markers of dyslipidemia among women but not men (46). Although there are consistent findings for an association between household food insecurity and chronic disease prevalence, the measure used for household food insecurity, sample restrictions, and clinical markers varied with each study. Some studies, such as that by Seligman et al. (2), restricted the sample to low-income households to better compare the association of food insecurity among only those who were at risk of the exposure, whereas others compared individuals from food-insecure households with the general population (45, 46). Comparing individuals from food-insecure households with those from wealthier families, even when controlling for income, may overestimate the association. Table 1 reviews the literature on the association between household food insecurity and chronic disease prevalence.
Table 1.
A summary of published studies on food insecurity and prevalence of diabetes and dyslipidemia1
| Study2 | Chronic disease or risk factor | Study sample and setting | Measurement and level of food insecurity | Results |
| Holben and Pheley, 2006 (1) | Diabetes risk factors | Rural Appalachia | 18-item HFSSM | Higher prevalence of self-reported diabetes among adults reporting food insecurity compared with food security (37.9% vs. 25.8%). BMI and percentage of obese were higher among food insecure, especially women. No other associations were found. |
| Self-report diabetes | n = 2580 | 4 levels | ||
| BMI | Adults >18 y | |||
| Diastolic blood pressure | ||||
| Total cholesterol | ||||
| Random blood glucose | ||||
| Hemoglobin A1c | ||||
| Seligman et al., 2007 (2) | Diabetes prevalence | NHANES 1999–2002 | 18-item HFFSM | Diabetes prevalence by food insecurity category: secure, 11.7%; mild, 10.0%; severe, 16.1% |
| Self-report diabetes or | n = 4423 <300% poverty | 3 levels of food insecurity: secure, mild, severe | Higher odds [AOR = 2.2 (95% CI: 1.1, 4.0)] persisted after adjusting for socioeconomic variables and BMI | |
| fasting serum glucose >126 mg/dL | Adults >20 y | |||
| Gucciardi et al., 2009 (45) | Diabetes prevalence | Canada Community Health Survey Cycle 3.1 (2005) | 18-item HFFSM | Food insecurity higher among those with diabetes (9.3% vs. 6.8%), especially women age 12–45 y (25%) |
| n = 6237 | ||||
| Tayie and Zizza, 2009 (46) | Dyslipidemia | NHANES 1999–2002 | 10-item adult food security | No association with any clinical marker for men. |
| Total cholesterol | n = 2695 | 4 levels: secure, marginal, insecure, insecure with hunger | Marginal food security associated with LDL and TGs/HDL ratio, food insecurity associated with TGs among women | |
| TG, LDL, HDL ratios | (1268 men, 1427 women) | |||
| Laraia et al., 2010 (43) | Gestational diabetes | Pregnancy, infection, nutrition study | 18-item HFSSM | 14% marginally food secure, 10% food insecure |
| Clinical diagnosis | n = 810 <400% poverty | 3 levels: secure, marginal, insecure | Higher odds of gestational diabetes among marginal [AOR = 2.76 (95% CI: 1.0, 7.66)] and with combined marginal/insecure [AOR = 2.38 (95% CI: 0.99–5.73)] | |
| Seligman et al., 2010 (3) | Chronic disease markers | NHANES 1999–2004 | 18-item HFSSM | Food insecurity self-report HTN [ARR = 1.2 (95% CI: 1.04, 1.38)], lipid [ARR: 1.3 (95% CI: 1.09,1.55)], not diabetes. Food insecurity-laboratory HTN [(ARR = 1.21, 95% CI: 1.04–1.41)], diabetes [ARR = 1.48 (95% CI: 0.94, 2.32)]. Using 6-item [ARR = 2.42 (95% CI: 1.44, 4.08)] |
| Self-report and lab markers: diabetes, TGs, hypertension | n = 5094 | 3 levels: secure, marginal, insecure | ||
| age 18–65y, <200% poverty | ||||
| Fitzgerald et al., 2011 (44) | Diabetes risk | Community-recruited sample | 6-item HFSSM | Very low food security associated with type 2 diabetes [AOR = 3.33 (95% CI: 1.34, 8.23)] |
| Self-reported diabetes | n = 201 | 3 levels: secure/low security/very low security | ||
| Adult Latinas 35–60 y | ||||
| Case-control study |
AOR, adjusted OR; ARR, adjusted risk ratio; HFSSM, household food security survey module; HTN, hypertension; TGs, triglycerides.
Studies are arranged by publication date.
Food insecurity and poor chronic disease management
Nelson et al. (47) published a seminal observational study characterizing the role of food insecurity among adult patients in an urban county hospital. They reported that among adults receiving insulin to treat diabetes, the majority (61%) reported hypoglycemic reactions, a serious event indicating poor diabetes management with short-term implications of blurred vision, agitation, anxiety, and, at the extreme, possibly causing a coma or seizure. Of these, half reported that an inability to afford food was the cause of the hypoglycemic event. Since this first report, there have been a number of studies that focus on both the association between household food insecurity and prevalent diabetes and between household food insecurity and poor diabetes management. Nelson et al. followed up this early study with a population-based analysis using data on adults with diabetes from NHANES and found that adults with diabetes were more likely to report fair or poor health and had significantly higher rates of health care use (48). Table 2 reviews the literature on the association between household food insecurity and markers of chronic disease management.
Table 2.
A summary of published studies on food insecurity and self-report or clinical marker of diabetes management1
| Study2 | Self-report or clinical marker | Study sample and setting | Measurement and level of food insecurity | Results |
| Nelson et al., 1998 (47) | Prevalence and risk factors of food insecurity in a patient population | Clinic population | Questions from Kendall et al. (55) and Hamilton et al. (56) | 103 (61%) of 170 diabetic patients reported hypoglycemic reactions, 32 (31%) reported inability to afford food |
| n = 709, 170 were receiving insulin | ||||
| Nelson et al., 2001 (48) | Doctor encounters | NHANES III | 1-item food Insufficiency | 6% of adults with diabetes reported food insufficiency. Diabetic patients who were food insufficient reported more doctors encounters. |
| n = 1503 | ||||
| Maddigan et al., 2006 (54) | Health-related quality of life among diabetic patients (4.1% of population) | Canadian Community Health Survey Cycle 1.1 (2000–2001) | 3 questions about financial access to a sufficient quantity and quality of food—any food insecurity | 15.5% experience some food insecurity. Food insecurity was negatively associated with quality of life among adults with diabetes [β = −0.07 (95% CI: 20.10, 20.04)] |
| n = 4678 | ||||
| Gucciardi et al., 2009 (45) | Diabetes management | Canada Community Health Survey Cycle 3.1 (2005) | 18-item HFI | 9.3% were food insecure. No association with diabetes management. Food insecurity was associated with lower fruit and vegetable intakes, smoking, unmet health care needs, overnight patient, mood disorder, stroke, lower life satisfaction, poor self-rated health, poor mental health, higher stress |
| Management services | n = 6237 | |||
| Self-care practices | Ontarians | |||
| Health status | n = 2523 | |||
| Seligman et al., 2010 (49) | Hypoglycemia | Clinic patients diagnosed with hypertension and diabetes in 2 urban settings | 6-item HFSSM | 45% were food insecure. Food insecure patients had lower self-efficacy scores, poor adherence to blood glucose monitoring, more emergency department visits for hypoglycemia, had higher HbA1c values. |
| Self-report lifetime experience with hypoglycemia | n = 40 adults | 2 levels: secure/insecure | ||
| Seligman et al., 2011 (50) | Hypoglycemia | Patients from 2 urban community health clinics | 6-item HFSSM | 46% were food insecure. Food insecure more likely (12.6% vs. 6.7%) to have 4+ hypoglycemia episodes (AOR = 2.0, 95% CI: 1.48–5.91) |
| Validated self-report | n = 782 adults | 2 levels: secure/insecure | ||
| 4+ severe episodes | ||||
| Marjerrison et al., 2011 (53) | Glycemic control | Families with a child receiving insulin for diabetes in Nova Scotia | 18-item HFSSM | 21.9% food insecure. |
| Hospitalization rates | n = 183 families | 2 levels: secure/insecure | Children from food insecure families had higher HbA1c (9.5% vs. 9.0%) and hospitalization rates (30% vs. 10.5%) compared with children from food-secure families. In adjusted models, food insecurity was not associated with ≥9.0% HbA1c, but was associated with being hospitalized the previous year (OR = 3.66; 95% CI: 1.54–8.66) | |
| Mean and ≥9.0% HbA1c | ||||
| Bawadi et al., 2012 (52) | Glycemic control | Clinic patients from major hospital | 6-item HFSSM | 51% were moderately secure and 27% food insecure. |
| Mean HbA1c value | n = 843 adults | 3 levels: secure/moderately secure/food insecure | BMI was greater among food-insecure patients compared with food secure (34.9 vs. 32.6, respectively). Both moderate and severe food insecurity were associated with a significantly higher mean HbA1c. | |
| Seligman et al., 2012 (51) | Glycemic control | Immigration, Culture and Health Care (ICHC) study in Chicago, IL, and San Francisco, CA | 6-item HFSSM | 46% were food insecure. |
| ≥8.5% HbA1c | n = 711 | 2 levels: secure/insecure | Food-insecure diabetic patients more likely (42% vs. 33%) to have poor glycemic control (HbA1c >8.5%), difficulty with diet (64% vs. 49%), lower self-efficacy, and higher emotional distress | |
| Follow diabetic diet | ||||
| Self-efficacy | ||||
| Emotional distress |
HbA1c, glycosylated hemoglobin; HFI, household food insecurity; HFSSM, household food security survey module.
Studies are arranged by publication date.
Rates of food insecurity among adults with diabetes are varied; in the studies reviewed here, the range is between 6% and 15.5% in population-based samples, and between 14% and up to 51% in clinic samples. Consistent findings from studies using clinic-based samples have repeatedly reported an association between household food insecurity and hypoglycemic events (47, 49, 50) and poor glycemic control, as measured by elevated glycosylated hemoglobin among adults (51, 52) and children with diabetes (53). Many of the reported studies to date focus on community clinics where the prevalence of food insecurity is high and of great concern to clinicians. Of the 2 population-based studies, 1 found a positive association (3), whereas 1 found no association between household food insecurity and indicators of poor diabetes management (45). Although food insecurity was not associated with poor diabetes management, it was associated with poor self-rated health, lower fruit and vegetable intake, higher smoking levels, and higher indicators of stress (45). This study and others may provide insight on the effects of food insecurity on health behavior and psychosocial factors that may lead to poor diabetes control and management. At the very least, household food insecurity compounds the challenges that adults and families with chronic conditions face. For example, among adults with diabetes, household food insecurity has been associated with lower scores for health-related quality of life (54), challenges with maintaining a nutritionally adequate diet, lower scores for self-efficacy, and higher emotional distress related to diabetes management (51).
Using data from NHANES, Seligman et al. (2) found that adults from food-insecure households who meet diagnostic criteria for diabetes, many of whom did not self-report having diabetes, were at significantly greater risk of having a measure of poor glycemic control compared with adults with diabetes from food-secure households. Seligman et al. (2) concluded that low-income adults with diabetes may be more likely to go undiagnosed or underreport a diabetes diagnosis. Increased attention is needed to assist low-income individuals with disease management and to improve their ability to afford high-quality nutritious foods.
A life course perspective
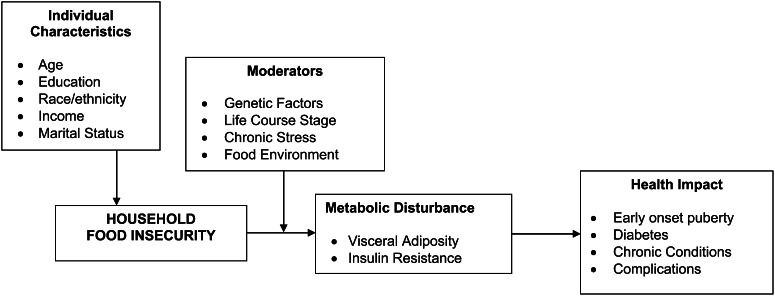
From both animal and human studies, there is evidence that supports the importance of studying the impact of household food insecurity on health outcomes using a life course framework. Exposure to food insecurity at 1 point in time can predispose an individual to poor health outcomes at a later point in time. Furthermore, the severity and duration of food insecurity need to be taken into consideration; however, more important may be the timing, the level of stress caused by food insecurity, and the interaction with the food environment. These factors—life course stage and stress—along with genetic factors and the food environment are depicted as moderators in Figure 1.
Figure 1.
Conceptual framework describing the influence of household food insecurity on chronic conditions and health outcomes.
The proposed model posits that conditions under which household food insecurity may lead to the development of metabolic syndrome and chronic disease outcomes are the following: 1) that household food insecurity is experienced as a chronic stressor (e.g., several months over a year), 2) that this will promote a stress response, 3) that the stress response results in a preference for and consumption of highly palatable foods, 4) that a stress response brought on by experiencing household food insecurity experienced during critical developmental states (e.g., in utero, infancy, peripubertal, pregnancy) is more damaging, and 5) that this leads to visceral fat accumulation, insulin resistance, or diet-induced obesity that may result in increased risk of chronic disease. Under these model conditions, there is an emphasis that food insecurity may have a more severe impact on individuals during critical developmental periods and on individuals with a certain phenotype that efficiently stores energy.
Conclusion
The aim of this mini symposium review was to summarize the relationship between food insecurity and chronic disease and postulate a conceptual framework. Food insecurity, whether at the household or individual level, is a social ill with clear health consequences. Understanding the extent to which food insecurity and chronic disease simply coexist, with poverty being the most obvious common causal mechanism, or whether food insecurity drives the development of chronic disease remains elusive. Reviewed in this paper were studies that link household food insecurity with diet, weight status, and chronic disease. The literature on the association between household food insecurity and dietary intake find that households do face episodic food shortages. Additionally, a modest association between household food insecurity and lower intake of fruits and vegetables, and several micronutrients has been found, although few studies find an association between household food insecurity and dietary fat, high energy-dense foods, or added sugar. With regard to weight status, a growing body of research finds inconclusive results for the association between household food insecurity and weight status for children or men; however, more consistent is the finding of an association between household food insecurity and higher weight status among women. Finally, there is a consistent association between household food insecurity and diabetes prevalence and poor diabetes control and management. Taken together, the studies to date represent a growing literature on the association between household food insecurity and diet, weight gain, and the development of chronic disease.
The review and framework presented in this paper suggest that the lived experience of food insecurity during critical periods of child development and pregnancy may result in the development of chronic disease. The framework also posits that an interaction between food insecurity and individuals who are more prone to store energy as weight or who are highly reactive may be a catalyst for visceral fat accumulation and chronic disease. Identifying family members who are particularly susceptible to this pathway will depend on their individual stress response, critical periods of growth and development, their stage in the life cycle, and their interaction with the food environment and consumption of highly palatable foods.
A major limitation is that the vast majority of the studies used a convenience sample or a cross-sectional study design, which is not sufficient to determine causal direction. Although longitudinal studies are still needed to assess the causal relationship between food insecurity and chronic disease, animal studies have shown that stress leads to weight gain, especially in the presence of highly palatable food. Furthermore, maternal food insecurity has an effect on offspring weight status and metabolic health (10). Longitudinal data analysis is needed to establish the temporal sequence between the exposure of household food insecurity and the development of chronic disease. Mediation analysis is also needed to identify the mechanism between household food insecurity and the development of chronic disease so that clinical and community interventions can best target modifiable risk factors. Finally, research is still needed to identify the intensity, duration, and level (i.e., household vs. individual) of food insecurity that is most associated with chronic disease development. Analyzing longitudinal data using a life course perspective will help identify critical developmental periods when food insecurity may be most damaging.
Acknowledgments
The sole author had responsibility for all parts of the manuscript.
Literature Cited
- 1.Holben DH, Pheley AM. Diabetes risk and obesity in food-insecure households in rural Appalachian Ohio. Prev Chronic Dis. 2006;3:A82. [PMC free article] [PubMed] [Google Scholar]
- 2.Seligman HK, Bindman AB, Vittinghoff E, Kanaya AM, Kushel MB. Food insecurity is associated with diabetes mellitus: results from the National Health Examination and Nutrition Examination Survey (NHANES) 1999–2002. J Gen Intern Med. 2007;22:1018–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr. 2010;140:304–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Adam TC, Epel ES. Stress, eating and the reward system. Physiol Behav. 2007;91:449–58 [DOI] [PubMed] [Google Scholar]
- 5.Kuo LE, Kitlinska JB, Tilan JU, Li L, Baker SB, Johnson MD, Lee EW, Burnett MS, Fricke ST, Kvetnansky R, et al. Neuropeptide Y acts directly in the periphery on fat tissue and mediates stress-induced obesity and metabolic syndrome. Nat Med. 2007;13:803–11 [DOI] [PubMed] [Google Scholar]
- 6.Groesz LM, McCoy S, Carl J, Saslow L, Stewart J, Adler N, Laraia B, Epel E. What is eating you? Stress and the drive to eat. Appetite. 2012;58:717–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Epel E, Lapidus R, McEwen B, Brownell K. Stress may add bite to appetite in women: a laboratory study of stress-induced cortisol and eating behavior. Psychoneuroendocrinology. 2001;26:37–49 [DOI] [PubMed] [Google Scholar]
- 8.Dallman MF, Pecoraro N, Akana SF, La Fleur SE, Gomez F, Houshyar H, Bell ME, Bhatnagar S, Laugero KD, Manalo S. Chronic stress and obesity: a new view of “comfort food”. Proc Natl Acad Sci U S A. 2003;100:11696–701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Seligman HK, Schillinger D. Hunger and socioeconomic disparities in chronic disease. N Engl J Med. 2010;363:6–9 [DOI] [PubMed] [Google Scholar]
- 10.Kaufman D, Banerji MA, Shorman I, Smith EL, Coplan JD, Rosenblum LA, Kral JG. Early-life stress and the development of obesity and insulin resistance in juvenile bonnet macaques. Diabetes. 2007;56:1382–6 [DOI] [PubMed] [Google Scholar]
- 11.Carr KD. Food scarcity, neuroadaptations, and the pathogenic potential of dieting in an unnatural ecology: binge eating and drug abuse. Physiol Behav. 2011;104:162–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Laraia BA, Siega-Riz AM, Gundersen C, Dole N. Psychosocial factors and socioeconomic indicators are associated with household food insecurity among pregnant women. J Nutr. 2006;136:177–82 [DOI] [PubMed] [Google Scholar]
- 13.Gundersen C, Mahatmya D, Garasky S, Lohman B. Linking psychosocial stressors and childhood obesity. Obes Rev. 2011;12:e54–63 [DOI] [PubMed] [Google Scholar]
- 14.Weinreb L, Wehler C, Perloff J, Scott R, Hosmer D, Sagor L, Gundersen C. Hunger: its impact on children's health and mental health. Pediatrics. 2002;110:e41. [DOI] [PubMed] [Google Scholar]
- 15.Hamelin AM, Habicht JP, Beaudry M. Food insecurity: consequences for the household and broader social implications. J Nutr. 1999;129:525S–8S [DOI] [PubMed] [Google Scholar]
- 16.Taren DL, Clark W, Chernesky M, Quirk E. Weekly food servings and participation in social programs among low income families. Am J Public Health. 1990;80:1376–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tarasuk VS. Household food insecurity with hunger is associated with women's food intakes, health and household circumstances. J Nutr. 2001;131:2670–6 [DOI] [PubMed] [Google Scholar]
- 18.Drewnowski A. Obesity, diets, and social inequalities. Nutr Rev. 2009;67:S36–9 [DOI] [PubMed] [Google Scholar]
- 19.Radimer KL, Olson CM, Campbell CC. Development of indicators to assess hunger. J Nutr. 1990;120:1544–8 [DOI] [PubMed] [Google Scholar]
- 20.Kendall A, Olson CM, Frongillo EA., Jr Relationship of hunger and food insecurity to food availability and consumption. J Am Diet Assoc. 1996;96:1019–24 [DOI] [PubMed] [Google Scholar]
- 21.Bhattacharya J, Currie J, Haider S. Poverty, food insecurity, and nutritional outcomes in children and adults. J Health Econ. 2004;23:839–62 [DOI] [PubMed] [Google Scholar]
- 22.Dixon LB, Winkleby MA, Radimer KL. Dietary intakes and serum nutrients differ between adults from food-insufficient and food-sufficient families: Third National Health and Nutrition Examination Survey, 1988–1994. J Nutr. 2001;131:1232–46 [DOI] [PubMed] [Google Scholar]
- 23.Tarasuk VS, Beaton GH. Household food insecurity and hunger among families using food banks. Can J Public Health. 1999;90:109–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rose D, Oliveira V. Nutrient intakes of individuals from food-insufficient households in the United States. Am J Public Health. 1997;87:1956–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Basiotis PP, Lino M. Food insufficiency and prevalence of overweight among adult women. Nutrition Insights, No. 26. USDA Center for Nutrition Policy and Promotion. 2002.
- 26.Lee JS, Frongillo EA., Jr Nutritional and health consequences are associated with food insecurity among U.S. elderly persons. J Nutr. 2001;131:1503–9 [DOI] [PubMed] [Google Scholar]
- 27.Cunningham TJ, Barradas DT, Rosenberg KD, May AL, Kroelinger CD, Ahluwalia IB. Is maternal food security a predictor of food and drink intake among toddlers in Oregon? Matern Child Health J. 2012;16:339–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bickel GNM, Price C, Hamilton W, Cook J. Guide to Measuring Household Food Security, Revised 2000. USDA, Food and Nutrition Services: Alexandria, Va. 2000.
- 29.Lorson BA, Melgar-Quinonez HR, Taylor CA. Correlates of fruit and vegetable intakes in US children. J Am Diet Assoc. 2009;109:474–8 [DOI] [PubMed] [Google Scholar]
- 30.Zizza CA, Duffy PA, Gerrior SA. Food insecurity is not associated with lower energy intakes. Obesity (Silver Spring). 2008;16:1908–13 [DOI] [PubMed] [Google Scholar]
- 31.Wolfe WS, Olson CM, Kendall A, Frongillo EA., Jr Hunger and food insecurity in the elderly: its nature and measurement. J Aging Health. 1998;10:327–50 [DOI] [PubMed] [Google Scholar]
- 32.Dietz WH. Does hunger cause obesity? Pediatrics. 1995;95:766–7 [PubMed] [Google Scholar]
- 33.Larson NI, Story MT. Food insecurity and weight status among U.S. children and families: a review of the literature. Am J Prev Med. 2011;40:166–73 [DOI] [PubMed] [Google Scholar]
- 34.Eisenmann JC, Gundersen C, Lohman BJ, Garasky S, Stewart SD. Is food insecurity related to overweight and obesity in children and adolescents? A summary of studies, 1995–2009. Obes Rev. 2011;12:e73–83 [DOI] [PubMed] [Google Scholar]
- 35.Rosenblum LA, Paully GS. The effects of varying environmental demands on maternal and infant behavior. Child Dev. 1984;55:305–14 [PubMed] [Google Scholar]
- 36.Coplan JD, Smith EL, Altemus M, Mathew SJ, Perera T, Kral JG, Gorman JM, Owens MJ, Nemeroff CB, Rosenblum LA. Maternal-infant response to variable foraging demand in nonhuman primates: effects of timing of stressor on cerebrospinal fluid corticotropin-releasing factor and circulating glucocorticoid concentrations. Ann N Y Acad Sci. 2006;1071:525–33 [DOI] [PubMed] [Google Scholar]
- 37.Coplan JD, Altemus M, Mathew SJ, Smith EL, Sharf B, Coplan PM, Kral JG, Gorman JM, Owens MJ, Nemeroff C, et al. Synchronized maternal-infant elevations of primate CSF CRF concentrations in response to variable foraging demand. CNS Spectr. 2005;10:530–6 [DOI] [PubMed] [Google Scholar]
- 38.Coplan JD, Smith EL, Altemus M, Scharf BA, Owens MJ, Nemeroff CB, Gorman JM, Rosenblum LA. Variable foraging demand rearing: sustained elevations in cisternal cerebrospinal fluid corticotropin-releasing factor concentrations in adult primates. Biol Psychiatry. 2001;50:200–4 [DOI] [PubMed] [Google Scholar]
- 39.Gundersen C, Lohman BJ, Garasky S, Stewart S, Eisenmann J. Food security, maternal stressors, and overweight among low-income US children: results from the National Health and Nutrition Examination Survey (1999–2002). Pediatrics. 2008;122:e529–40 [DOI] [PubMed] [Google Scholar]
- 40.Lohman BJ, Stewart S, Gundersen C, Garasky S, Eisenmann JC. Adolescent overweight and obesity: links to food insecurity and individual, maternal, and family stressors. J Adolesc Health. 2009;45:230–7 [DOI] [PubMed] [Google Scholar]
- 41.Gooding HC, Walls CE, Richmond TK. Food insecurity and increased BMI in young adult women. Obesity (Silver Spring). 2012;20:1896–901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Olson CM, Strawderman MS. The relationship between food insecurity and obesity in rural childbearing women. J Rural Health. 2008;24:60–6 [DOI] [PubMed] [Google Scholar]
- 43.Laraia BA, Siega-Riz AM, Gundersen C. Household food insecurity is associated with self-reported pregravid weight status, gestational weight gain, and pregnancy complications. J Am Diet Assoc. 2010;110:692–701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fitzgerald N, Segura-Pérez S, Pérez-Escamilla R. Food insecurity is related to increased risk of type 2 diabetes among Latinas. Ethn Dis. 2011;21:328–34 [PMC free article] [PubMed] [Google Scholar]
- 45.Gucciardi E, Vogt JA, DeMelo M, Stewart DE. Exploration of the relationship between household food insecurity and diabetes in Canada. Diabetes Care. 2009;32:2218–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tayie FA, Zizza CA. Food insecurity and dyslipidemia among adults in the United States. Prev Med. 2009;48:480–5 [DOI] [PubMed] [Google Scholar]
- 47.Nelson K, Brown ME, Lurie N. Hunger in an adult patient population. JAMA. 1998;279:1211–4 [DOI] [PubMed] [Google Scholar]
- 48.Nelson K, Cunningham W, Andersen R, Harrison G, Gelberg L. Is food insufficiency associated with health status and health care utilization among adults with diabetes? J Gen Intern Med. 2001;16:404–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Seligman HK, Davis TC, Schillinger D, Wolf MS. Food insecurity is associated with hypoglycemia and poor diabetes self-management in a low-income sample with diabetes. J Health Care Poor Underserved. 2010;21:1227–33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Seligman HK, Jacobs EA, Lopez A, Sarkar U, Tschann J, Fernandez A. Food insecurity and hypoglycemia among safety net patients with diabetes. Arch Intern Med. 2011;171:1204–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Seligman HK, Jacobs EA, Lopez A, Tschann J, Fernandez A. Food insecurity and glycemic control among low-income patients with type 2 diabetes. Diabetes Care. 2012;35:233–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bawadi HA, Ammari F, Abu-Jamous D, Khader YS, Bataineh S, Tayyem RF. Food insecurity is related to glycemic control deterioration in patients with type 2 diabetes. Clin Nutr. 2012;31:250–4 [DOI] [PubMed] [Google Scholar]
- 53.Marjerrison S, Cummings EA, Glanville NT, Kirk SF, Ledwell M. Prevalance and associations of food insecurity in children with diabetes mellitus. J Pediatr. 2011;158:607–11 [DOI] [PubMed] [Google Scholar]
- 54.Maddigan SL, Feeny DH, Majumdar SR, Farris KB, Johnson JA. Understanding the determinants of health for people with type 2 diabetes. Am J Public Health. 2006;96:1649–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kendall A, Olson CM, Frongillo EA., Jr Validation of the Radimer/Cornell measures of hunger and food insecurity. J Nutr. 1995;125:2793–801 [DOI] [PubMed] [Google Scholar]
- 56.Hamilton WL, Cook JT, Thompson WW, Burona LF, Frongillo EA, Olson CM, Wehler CA. Household Food Security in the United States, Summary Report of the Food Security Measurement Project. USDA, Food and Nutrition Services: Alexandria, VA. 1997.