Abstract
The place of sugars in the U.S. diet is vigorously debated with much attention on added sugars, those added during processing or preparation of foodstuffs, particularly as they relate to obesity. Federal government agencies have different responsibilities related to the food supply including research, food safety, nutrition assistance, and labeling; therefore, the interpretation of evidence differs depending on the role of the agency. Some common references for government agency positions are the dietary reference intakes and the Dietary Guidelines for Americans, which together form the foundation for much of federal nutrition policy. Sugar consumption has increased in proportion to intake of other nutrients since 1980, when obesity began to increase substantially. Median intake of added sugars is ∼12% of energy, whereas total sugar intake is ∼22% of energy. Although there are differences in the way in which individual monosaccharides are metabolized, they are rarely consumed alone. A key issue related to obesity is likely the increased number of eating occasions and portion size for many indulgent foods; grain-based snacks have become the largest source of energy in the U.S. diet. There are currently insufficient data to justify a decision on regulation or taxation of sugar-containing foods and the like because the approach must be weighed against personal freedoms; the list of foods associated with obesity includes many commonly eaten items, and it is not likely that they are all causally related. Government should consider the totality of the evidence including the strength of the relationship of sugar intake with various health outcomes.
Although some federal agencies (e.g., some within the USDA) are responsible for fiscal support of food production or promotion of food purchases resulting from legislation enacted by Congress, other agencies of the government are responsible for research, public health, food assistance, food labeling, and advertising. At times, these 2 fundamental roles of government can be at odds with each other. The former responsibility is primarily a result of political decisions, whereas the latter functions are not. Ultimately, reliable and relevant scientific data are the primary drivers when federal agencies consider added sugars in the diet. Although each federal agency has its own needs based on different missions including research, public health, and food assistance, there are a number of general policies that all agencies refer to regarding all components of the diet. The primary documents are the dietary reference intakes (DRI) (1) and the Dietary Guidelines for Americans (DGA) (2). In addition to those 2 primary sources, federal agencies also consider changes in the food supply, time trends in dietary intake, the prevalence of obesity, and the relationship of these to chronic diseases. Some types of studies such as ecologic analyses have been wrong more than correct in linking nutrients or foods with chronic diseases and case–control studies have not fared much better in elucidating cause-and-effect relationships. Obesity has become a dominant issue for every federal agency that deals with any aspect of food production or consumption, whether from a perspective of economics, research, public health, policy, labeling, or education.
Current status of knowledge
The recommended dietary allowance for carbohydrates is 130 g/d for both adults and children, based on the average minimum amount of glucose used by the brain (1). This amount is generally exceeded with typical diets because starches are broken down primarily to glucose. In 2009–2010, the mean intake of carbohydrate for males older than the age of 2 y ranged from 216 to 335 g/d, and for females, the mean ranged from 206 to 250 g/d (3). The DRI panel considered multiple potential adverse effects of overconsumption of sugars and dismissed a causal relationship for changes in behavior, altered insulin sensitivity, increased type 2 diabetes, increased obesity, and risk of cancers of the lung, breast, prostate, colon, and rectum. The only adverse effects that the committee agreed on were increased dental caries and increased serum triglycerides. However, they did not identify a threshold level of sugar intake at which these adverse effects are seen. Although they did not set a tolerable upper limit for sugars, a maximum of 25% energy from added sugars was suggested based on decreased intake of micronutrients associated with diets containing that level of sugar. The WHO recommends a maximum of 10% of energy from total sugars (4), based on a different interpretation of mostly the same data.
The concept of added sugars was developed by the USDA Center for Nutrition Policy and Promotion for the primary purpose of making dietary recommendations for nutrient-rich foods as part of the DGA. This construct discourages high energy–density, low nutrient–density foods. Although fruit and 100% fruit juice with intrinsic sugars are recommended, it is assumed that all foods with added sugars contribute to micronutrient dilution. Given that so few Americans meet the nutrient and food serving guidelines detailed in the DGA, as well as low levels of physical activity prevalent in the population, there is little room in most diets for foods containing low micronutrient quantities, and, therefore, foods with added sugars are discouraged. But it should be acknowledged that such foods are not metabolically different from those containing intrinsic sugars. In addition, there are many nutrient-rich foods that contain added sugars such as fortified or enriched ready-to-eat breakfast cereals, whole-grain breads that require sugar to reduce perceived bitterness, and sweetened yogurt that represents the overwhelming majority of the product sold in the United States. In addition, there are nuances of food preparation or processing in which fruit juice might not be considered added sugar (as 100% juice) or would be added sugar (when added to a recipe as a sweetener or for other functional purposes). Finally, added sugars are not on the food label that provides proximate composition of major nutrients in processed foods mandated by the FDA. The FDA recently requested public comment on a proposal to collect consumer responses to changes in the Nutrition Facts label that could include a declaration of the amount of added sugars (5). The FDA requires appropriate methods of analysis, such as those approved by Association of Official and Analytical Chemists International, for any food ingredient that appears on the label. Because the amount of added sugars cannot be measured or differentiated from intrinsic sugars, they currently cannot be required on the food label. Some food companies are concerned that if this becomes required, their proprietary recipes could be discerned by their competitors. The only time that added sugars can be determined readily is when they are the only source of sugar in a product such as hard candy and soft drinks.
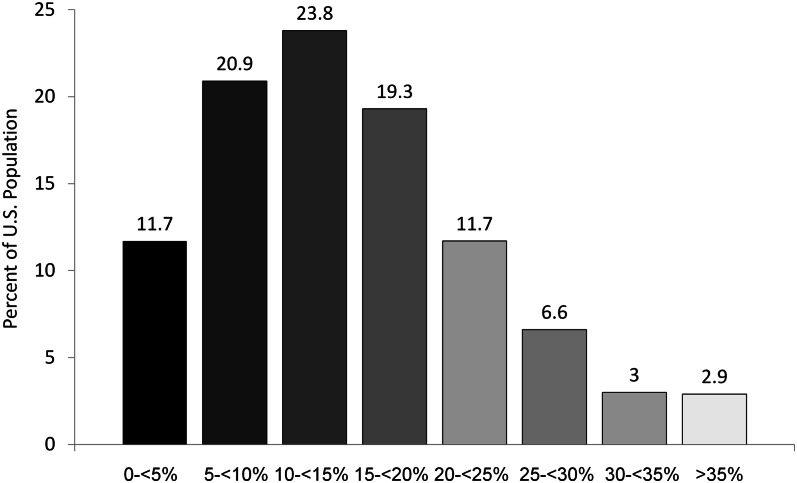
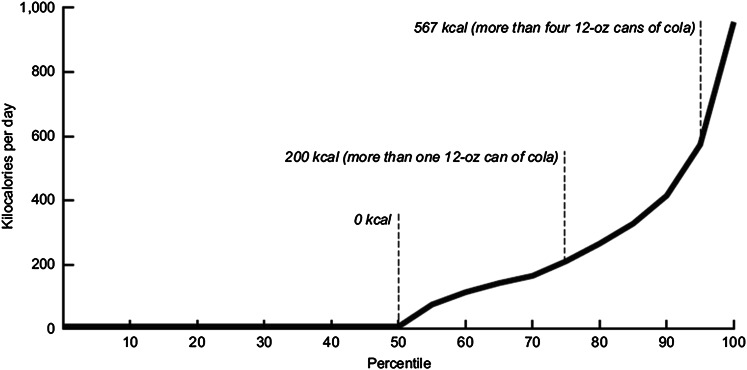
Data on nationally representative food intake comes from the What We Eat in America portion of the NHANES conducted jointly by the CDC’s National Center for Health Statistics and the USDA’s Agricultural Research Service. According to NHANES data collected for 2009–2010, total carbohydrate intake for adult (>20 y) men and women was 296 and 224 g/d, respectively. Total sugar intake in men and women was 131 and 103 g/d or 21% and 23%, respectively, of energy (3). Because added sugars are not included in the USDA National Nutrient Database for Standard Reference (6), it is more difficult to estimate those intakes, but Marriott et al. (7) generated what appear to be reliable estimates (Fig. 1). One third of the population consumes <10% energy from added sugars, and the median intake is ∼14% of energy, whereas 12.5% exceeds the 25% maximum from the Institute of Medicine. Figure 2 indicates part of the reason for this skewed distribution; in a given day, half of the population consumes no sugar-sweetened drinks, whereas 25% consume the equivalent of one 12-oz (355-mL) can or more and the 95th percentile of consumption is the equivalent of 4 or more 12-oz (355-mL) cans (8). Many of the controlled interventions that feed subjects 25% of energy from a single carbohydrate are, therefore, modeling intake of the top 10% to 12% of the population. This is analogous to studying a micronutrient at or above the tolerable upper limit and extrapolating to the normal intake range. It is important to remember that NHANES data are cross-sectional, and compiling multiple years provides larger numbers with better statistical power, but this does not equate to a prospective cohort nor does it enable ascertainment of causality, merely trends over time and an association. Dietary habits have, indeed, changed over time so that white bread used to be the largest single source of energy in the US diet, but that has been displaced by grain-based desserts, which include cakes, pies, cobblers, cookies, doughnuts, and pastries, contributing 13% of energy in the US diet (3).
Figure 1.
Percentage of the US population consuming added sugars as a percentage of energy for 15,190 subjects aged 4 y and older in NHANES surveys from 2003 to 2006. Adapted with permission from (7).
Figure 2.
Amount of sugar-drink consumption for individuals ages 2 y and older in NHANES surveys from 2005 to 2008. Reproduced from (8), which is a federal government publication without copyright restrictions.
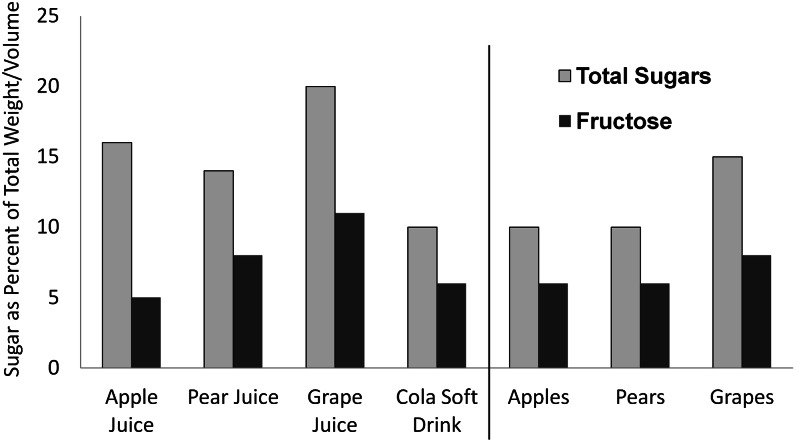
Because of the high public and scientific interest in the topic of added sugars and particularly because of the debate about high-fructose corn syrup versus sucrose, there is a lot of misinformation in the mass media, and, unfortunately, many scientists misunderstand the relative amounts of sugars and fructose in various foods and drinks. Figure 3 shows the average amount of total sugar and fructose in standardized servings of popular fruits and 100% fruit juices in comparison with a cola soft drink. The soft drink has less sugar than any fruit juice and no more than an equivalent weight serving of solid fruit; it is also among the lowest in fructose content.
Figure 3.
Total sugars and fructose in raw fruits, 100% fruit juices, and cola soft drink (g/100 mL or g). Actual sugar intake is, of course, dependent on the amount consumed. Adapted from (6), which is a federal database without copyright restrictions.
A question often debated in this area of nutrition is whether there is a metabolic difference after consumption of different sugars. It is obvious that this is the case, but individual sugars are seldom, if ever, consumed by themselves and rarely found in foods. In addition, the metabolic consequences of sugar consumption are modified by intake of other foods or nutrients; fat and fiber ingestion delays absorption and often reduces peak blood glucose levels and the area under the curve. In addition, because most starch is metabolized to glucose, there is almost always more of this monosaccharide than any other being metabolized. If glucose-yielding carbohydrates are not consumed, glucose is synthesized because it is the primary fuel for most somatic cells. Consumption of high amounts of sugars induces carbohydrate-metabolizing enzymes so that most people can easily tolerate large daily variation in carbohydrate intake while staying within the general limits outlined in the DRI for carbohydrates (1).
There are numerous small trials of sugar feeding in the literature. Rather than provide a narrative review of them, it is useful to refer to a number of systematic reviews and meta-analyses that have been published recently by Sievenpiper et al. (9–12). Most important to the current review is the analysis of body weight change in controlled feeding trials in which fructose was exchanged for other carbohydrates. In trials that substituted fructose isoenergetically, there was no overall effect on weight (9). However, when these trials were subdivided into studies on normal weight, overweight/obese, and subjects with diabetes, there was a small but statistically significant reduction of weight in overweight/obese subjects and no effects on either normal weight or diabetic subjects. In contrast, when fructose was tested in hypercaloric feeding trials, the result in both normal weight and overweight/obese individuals was a statistically significant increase in body weight. The amount of excess fructose in these trials ranged from 104 to 250 g/d (416–1000 kcal excess/d). These data strongly suggest that only the hypercaloric addition of fructose has an adverse effect on body weight and that isocaloric substitution may have some benefit in overweight or obese individuals. Analysis of low-dose (≤36 g/d) fructose feeding suggested that these amounts improved glycemic control as measured by serum glucose or hemoglobin A1c without adverse effects on body weight or serum triglycerides, serum insulin, or uric acid levels (10); the authors pointed out that there are relatively few trials in this analysis, and trials lasting at least 6 mo are needed to substantiate these results. Separate analysis of controlled feeding trials that examined effects of fructose exchange for other carbohydrates on uric acid by this same group revealed that overall isocaloric exchange had no effect; only high-dose fructose in energy excess increased serum uric acid (11). The fourth meta-analysis by this group examined the exchange of fructose for other carbohydrates in diabetic individuals and found that isocaloric exchange reduced glycated blood proteins and had no effect on fasting glucose of insulin (12). In summary, meta-analyses of exchange of fructose with other carbohydrates reveals no adverse effects on any endpoints except for weight gain when provided in excess of energy needs.
This problem has relevance to public health because of increasing portion sizes for a variety of sweetened drinks, which is typical of larger sizes of solid foods commonly eaten in the United States, particularly in restaurants. Sixty years ago, the standard serving size for a carbonated soft drink was 6.5 oz (192 mL), which provided 22 g of sugar and 88 kcal; this was supplanted in the 1960s by 12-oz (355-mL) cans when the pop-top lid was invented; 20-oz (591-mL) screw-cap bottles with 67 g of sugar and 260 kcal became the most common serving size in convenience stores; value pricing led to 32-oz (946-mL) and 64-oz (1893-mL) drinks that cost only slightly more than smaller drinks, with the latter providing a half gallon or 1.9 L of fluid and 182 g of sugar and 728 kcal. These examples are for different types of drinks that are most commonly sold in the United States. The 64-oz (1893-mL) example was recently discontinued at 1 chain of convenience stores, not for public health reasons, but because it did not fit in cup holders of automobiles and sales had suffered as a result. In fact, the widespread adoption of cup holders in American automobiles during the 1980s may have contributed to the social acceptance of eating and drinking throughout the day, in addition to the consumption of higher energy foods that are more convenient to eat with 1 hand while sitting in a vehicle. Of course, many other secular changes occurred simultaneously such as the spread of cable television with hundreds of channels that led to more sedentary behavior.
Although some have claimed that sugar and/or fructose is toxic (13, 14), that assertion does not pass the test of face validity. The principle that the dose makes the poison was promulgated 500 y ago by Paracelsus, sometimes referred to as the Father of Toxicology, to whom the following quote is attributed: “All substances are poisons; there is none which is not a poison. The right dose differentiates a poison and a remedy” (15). This is true for all nutrients, including water. There is little controversy that some Americans consume too much sugar (although the threshold remains undefined) and that this reflects an overall poor diet, which correlates with other unhealthy lifestyle choices. A reasonable response to overconsumption by a fraction of the population is not to prescribe zero intake by anyone. Moderation is a concept that does not resonate with consumers or most scientists.
Calls to reduce consumption of foods that have been associated with obesity or other health conditions lead to debate about regulation or taxation of sugary foods or specific nutrients such as highly saturated fat or trans fat that have been linked to adverse health outcomes. This is a political decision that scientists expect would be based on good science, but that may not be a primary concern for politicians making such choices. Existing taxes in various states range up to 7% of the price and have no effect on purchasing behavior. The rationale for higher taxes, as high as 18%, is based on modeling and extrapolation rather than on purchasing behaviors (16). In today’s economic climate, many of the local debates about taxing sugary foods have focused on how much revenue they could raise rather than what specific health benefit would accrue. Complicating this debate are related arguments that a single category of food is not responsible for obesity, that portion size and frequency of consumption are deciding factors in weight control, and that adequate physical activity can compensate for caloric indiscretions.
Conclusions
There is no single set of criteria that federal agencies consider in dealing with this issue, in part because there are multiple responsibilities of the different agencies that address this from research to nutrition assistance to regulatory aspects. Government is supposed to depend on the totality of the evidence. They do not rely solely on observational epidemiology due to confounding and covariates among health-related behaviors; cross-sectional epidemiology is never used to determine causality even though much of the data are based on such surveys, including NHANES, which is essentially a series of 2-y snapshots of dietary and health status of the United States. It is important for the relationship between any food and any health endpoint to be both biologically meaningful and statistically significant if changes in diet are to be recommended; these combined factors translate to the strength of the relationship; the RR for nutrition and disease are much weaker than other environmental effects, with risks almost always <2 and often much less. In the past, epidemiologists ignored such small differences, and most environmental epidemiologists use an RR of 4 to 5 as a lower cutoff for a meaningful difference.
Another issue considered by government is the overall diet and health pattern. If someone is physically active and in the desirable weight range, it is unlikely that any dietary indulgence will be a problem. Likewise, adding an unsweetened, nonfat, whole-grain food to a hypercaloric diet by an obese individual does not make the diet healthy. Although these issues should be self-evident, these points are often lost in the debate about whether there are good and bad foods and are part of the reason for why government should not be swayed by the emotional appeal of the simple fix despite considerable calls for action in the absence of evidence. Government also use public health factors in their decisions related to diet and health; that is, what are the relative benefits, risks, and costs? This equation includes costs to personal freedom, which many US citizens believe trumps government intervention. Many times there is insufficient evidence, and some in and out of government believe that actions should be taken with the best available evidence, no matter the quality, whereas others believe that very firm evidence is required. Most times the correct path is somewhere in between, and that requires experience and judgment.
In summary, there is no credible evidence that added sugar or any single saccharide is toxic or addictive or contributes to any disease independently of a diet that provides excess energy other than dental caries. Federal policy discourages excess consumption of added sugars primarily because of their potential for dilution of micronutrient content and provision of excess energy, even though their metabolism is no different from intrinsic sugars.
Acknowledgments
The sole author had responsibility for all parts of the manuscript.
Literature Cited
- 1.Institute of Medicine. Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids. Washington, DC: The National Academies Press. 2005.
- 2.U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2010. 7th ed. Washington, DC: U.S. Government Printing Office. 2010. [DOI] [PMC free article] [PubMed]
- 3.U.S. Department of Agriculture, Agricultural Research Service. Nutrient intakes from food: mean amounts consumed per individual, by gender and age, what we eat in America, NHANES 2009–2010. Available from: www.ars.usda.gov/ba/bhnrc/fsrg. Accessed August 6, 2012.
- 4.Joint WHO/FAO Expert Consultation. Diet, nutrition and the prevention of chronic diseases. Report no. 916. Geneva: World Health Organization; 2003. [PubMed]
- 5.Food and Drug Administration Agency information collection activities; proposed collection; common request; experimental study on consumer responses to nutrition facts labels with various footnote formats and declaration of amount of added sugars. Fed Regist. 2012;77:32120–2 [Google Scholar]
- 6. U.S. Department of Agriculture, Agricultural Research Service, USDA Nutrient Data Laboratory. USDA National Nutrient Database for Standard Reference, Release 24, 2011.
- 7.Marriott BP, Olsho L, Hadden L, Connor P. Intake of added sugars and selected nutrients in the United States, National Health and Nutrition Examination Survey (NHANES) 2003–2006. Crit Rev Food Sci Nutr. 2010;50:228–58 [DOI] [PubMed] [Google Scholar]
- 8.Ogden CL, Kit BK, Carroll MD, Park S. Consumption of sugar drinks in the United States, 2005–2008. NCHS data brief, no 71. Hyattsville, MD: National Center for Health Statistics; 2011. [PubMed]
- 9.Sievenpiper JL, de Souza RJ, Mirrahimi A, Yu ME, Carleton AJ, Beyene J, Chiavaroli L, Di Buono M, Jenkins AL, Leiter LA, et al. Effect of fructose on body weight in controlled feeding trials: a systematic review and meta-analysis. Ann Intern Med. 2012;156:291–304 [DOI] [PubMed] [Google Scholar]
- 10.Sievenpiper JL, Chiavaroli L, de Souza RJ, Mirrahimi A, Cozma AI, Ha V, Wang DD, Yu ME, Carleton AJ, Beyene J, et al. ‘Catalytic’ doses of fructose may benefit glycaemic control without harming cardiometabolic risk factors: a small meta-analysis of randomised controlled feeding trials. Br J Nutr. 2012;108:418–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang DD, Sievenpiper JL, de Souza RJ, Chiavaroli L, Ha V, Cozma AI, Mirrahimi A, Yu ME, Carleton AJ, Di Buono M, et al. The effects of fructose intake on serum uric acid vary among controlled dietary trials. J Nutr. 2012;142:916–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cozma AI, Sievenpiper JL, de Souza RJ, Chiavaroli L, Ha V, Wang DD, Mirrahimi A, Yu ME, Carleton AJ, Di Buono M, et al. Effect of fructose on glycemic control in diabetes: a systematic review and meta-analysis of controlled feeding trials. Diabetes Care. 2012;35:1611–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lustig RH, Schmidt LA, Brindis CD. Public health: the toxic truth about sugar. Nature. 2012;482:27–9 [DOI] [PubMed] [Google Scholar]
- 14.Bray GA. Fructose: pure, white, and deadly? Fructose, by any other name, is a health hazard. J Diabetes Sci Technol. 2010;4:1003–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Society of Toxicology Web site. Available from: http://www.toxicology.org/AI/EO/principl.asp. Accessed August 14, 2012.
- 16.Duffey KJ, Gordon-Larsen P, Shikany JM, Guilkey D, Jacobs DR, Jr, Popkin BM. Food price and diet and health outcomes: 20 years of the CARDIA Study. Arch Intern Med. 2010;170:420–6 [DOI] [PMC free article] [PubMed] [Google Scholar]