Abstract
Oesophageal carcinosarcoma is a rare type of oesophageal cancer composed of both squamous cells and sarcomatous cells. We report a case of a 71 year old man presenting with dysphagia and weight loss. Oesophagogastroduodenoscopy revealed a bulky mass with a preliminary diagnosis of only oesophageal carcinoma, and the oesophageal mass was resected with a transhiatal oesophagectomy. On surgical pathology, it was discovered that the tumor had both squamous cell and sarcomatous cell components, and the final diagnosis was changed to oesophageal carcinosarcoma. We discuss the presentation, differential diagnosis, treatment, and prognosis of this unique entity.
INTRODUCTION
Two commonly known oesophageal cancers are oesophageal squamous cell carcinoma and oesophageal adenocarcinoma, both of which exhibit a single histologic cell type. A rare oesophageal cancer, which is mixed with two different cell types, is oesophageal carcinosarcoma. It is comprised of both squamous and sarcomatous cells and occurs with an incidence of about 0.1-1.5 % of all oesophageal tumors. In this article, we describe a patient with this unusual type of oesophageal cancer.
CASE REPORT
A 71 year old man with a past medical history of hypertension and chronic renal insufficiency presented to a local gastroenterologist complaining of a three month history of progressively worsening dysphagia and weight loss of twenty pounds. The patient underwent upper endoscopy, and a near obstructing mass in the oesophagus was discovered roughly 20 cm from the incisors, as seen in Figure 1. At that time, biopsy revealed only squamous cells and the preliminary diagnosis was oesophageal carcinoma. The patient’s chest and abdomen CT scan as well as a PET scan showed no radiological evidence of metastatic disease. He was then taken to the operating room where an exploratory laparotomy was done and no intraperitoneal metastasis was seen. Thus, for curative treatment, a transhiatal oesophagectomy with primary anastomosis was performed. The patient had an uneventful postoperative course and was discharged from the hospital without any issues.
Figure 1.

Gross specimen: obstructive exophytic mass in the oesophagus
Surgical pathology report of the specimen from the operating room demonstrated in situ and invasive squamous cell carcinoma, which was previously identified in the endoscopic specimen, but there were also sarcomatous areas. This is depicted inFigure 2. The tumor measured 6 cm, was exophytic and high grade, and invaded into the submucosa but not the muscularis propria. The surgical margins and a resected celiac lymph node were negative, and there was no lymphovascular invasion. Based on the findings of both squamous cell and sarcomatous cell types, the final diagnosis was oesophageal carcinosarcoma, and it was classified as stage T1 N0 M0.
Figure 2.
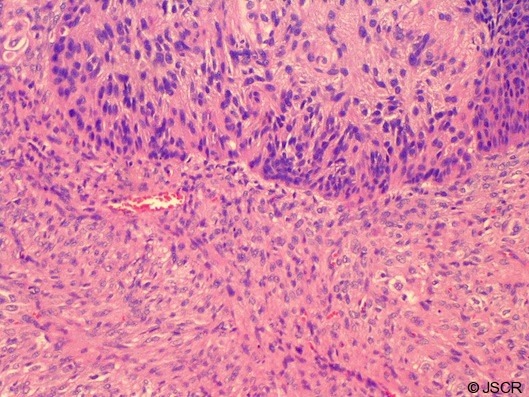
Surgical pathology: squamous cell and sarcomatous cell components of oesophageal carcinosarcoma, hematoxylin and eosin stain at 100x magnification
DISCUSSION
In 1865, Virchow named the rare malignant neoplasm of squamous cell and sarcomatous cell types “carcinosarcoma”. Since then, it has also been called pseudosarcoma, spindle cell carcinoma, and sarcomatoid carcinoma. This mixed type of tumor with a combination of carcinomatous and sarcomatous cell types has been found in cancers of the uterus, vagina, lungs, oral cavity, larynx, thyroid, urinary tract, and oesophagus.
Two main theories exist on the origin of carcinosarcomas. The predominant one, the metaplastic theory, postulates that there is a common ancestor cell, and through metaplasia of the original squamous cell carcinoma, the sarcomatous component arises. As the two cell types intermingle, transitional zones emerge. The second theory, the collision theory, points to the possibility of two separate individual stem cells; that is, both a carcinoma and a sarcoma occurred coincidentally and simultaneously.
Like other oesophageal cancers, oesophageal carcinosarcoma is more prevalent in men (1,2), especially those with a history of tobacco and alcohol use (3). It is characterized by rapid growth that exerts a mass effect, so the prominent complaints by the patient are dysphagia 80% of the time, and weight loss 61% of the time (4). Other complaints include pain on swallowing and anorexia.
On endoscopic examination, the lesion is a bulky, polypoid, gray-white mass with margins that are smooth, lobulated or scalloped. Mucosal ulceration or a pedicle may also be present. A barium swallow study sometimes reveals the cupola sign, which refers to the domelike appearance of the intraluminal filling defect from the lesion. The location of the mass is most commonly in the middle third of the oesophagus 59% of the time, followed by the lower third 28% of the time, and the upper third 13% of the time (4).
The differential diagnosis for such an oesophageal mass has a wide range of possibilities from the benign to the malignant. Benign lesions include the fibrovascular polyp, myofibroma, pedunculated lipoma, and leiomyoma; malignant lesions include adenocarcinoma from Barrett’s oesophagus, squamous cell carcinoma, leiomyosarcoma, fibrosarcoma, rhabdomyosarcoma, melanoma, oat cell carcinoma, and lymphoma. It is difficult to distinguish these lesions radiographically. Furthermore, endoscopic biopsy only captures the superficial aspect of the mass, often showing the squamous cell component but not the deeper sarcomatous cell component. Thus, the final diagnosis rests on the surgical pathology after removal of the mass in its entirety with surgery.
The operations for oesophageal carcinosarcoma are transhiatal oesophagectomy with gastric interposition, and Ivor Lewis oesophagectomy, coupled with adequate lymph node dissection. On pathology, the squamous cell component has a range of differentiation from moderate to poor, and grows in cords and intracellular bridges with keratin formation. It may stain positively for antikeratin antibody for epithelial cells or cytokeratin (5,6). The sarcomatous cell component is typically fibrosarcoma, and the spindle cells tend to grow in fascicles in a whorled pattern. The sarcomatous cell component may stain positively for collagen, alpha smooth muscle actin stain and vimentin (1,3,6).
In terms of prognosis for oesophageal carcinosarcoma, not only the squamous cell component but also the sarcomatous cell component can metastasize. The routes of metastasis can be direct invasion, lymphatic invasion, as well as hematogenous invasion. In some ways though, oesophageal carcinosarcoma behaves like oesophageal squamous cell carcinoma. The rate of lymph node metastasis in oesophageal carcinosarcoma is about 50-67%, which is comparable to that of oesophageal squamous cell carcinoma (7). Patient mortality is ultimately attributed to distant metastasis to the liver, brain, lung, and bone, and the five year survival for patients with oesophageal carcinosarcoma is 27% (7) which is similar to that of oesophageal squamous cell carcinoma.
In conclusion a rare type of oesophageal cancer is oesophageal carcinosarcoma, and it is unique for being not purely of a single cell type, but instead mixed with both squamous cell and sarcomatous cell components. Its characteristic rapid growth into an exophytic mass leads to symptoms of dysphagia and weight loss. Treatment is primarily surgical resection, whereupon surgical pathology of the mass in its entirety will reveal both cell types and the final diagnosis. Prognosis is based on distant metastasis and survival rates are similar to that of oesophageal carcinoma.
REFERENCES
- 1.Iascone C, Barreca M. Carcinosarcoma and Pseudosarcoma of the esophagus: Two Names, One Disease-Copmrehensive Review of the Literature. World Journal of Surgery 1999; 23:153–157 [DOI] [PubMed] [Google Scholar]
- 2.Xu LT, Sun CF, Wu LH, Chang ZR, Liu TH. Clinical and pathological characteristics of carcinosarcoma of the esophagus: report of four cases. Annals of Thoracic Surgery 1994; 37:197–203 [DOI] [PubMed] [Google Scholar]
- 3.Perch SJ, Soffen EM, Whittington R, Brooks JJ. Esophageal sarcomas. Journal of Surgical Oncology 1991; 48:194–198 [DOI] [PubMed] [Google Scholar]
- 4.Lieberman MD, Francheschi D, Marsan B, Burt M. Esophageal carcinoma: The unusual variants. Journal of Thoracic and Cardiovascular Surgery 1994; 108:1138–1146 [PubMed] [Google Scholar]
- 5.Agha FP, Keren DF. Spindle cell squamous carcinoma of the esophagus: a tumor with biphasic morphology. American Journal of Roenterology 1985; 145:541–545 [DOI] [PubMed] [Google Scholar]
- 6.Kanamoto A, Nakanishi Y, Ochiai A, Shimoda T, Yamaguchi H, Tachimori Y, Kato H, Watanabe H. A case of polypoid esophageal carcinoma with multidirectional differentiation including neuroendocrine, squamous, ciliated glandular, and sarcomatous components. Archives of Pathology and Labarotory Medicine 2000; 124:1685–1687 [DOI] [PubMed] [Google Scholar]
- 7.Iyomasa S, Kato H, Tachimori Y, Watanabe H, Yamaguchi H, Itabashi M. Carcinosarcoma of the esophagus: a twenty case study. Japanese Journal of Clinical Oncology 1990; 20:99–106 [PubMed] [Google Scholar]


