Abstract
Lactating adenoma is one of the breast tumours associated with pregnancy. A case of lactating adenoma, unusual on account of its huge size, is presented. Large size and history of rapid growth can lead to a mistaken diagnosis of malignancy. A review of the literature of this particular tumour with the different views on its histogenesis and the differential diagnoses are also discussed.
INTRODUCTION
Lactating adenoma is a rare breast tumor, most often associated with pregnancy. It can rarely grow rapidly to large size and result in diagnostic dilemma.
CASE REPORT
A twenty one year old primi gravida at six months gestation presented with a history of rapidly enlarging lump in the left breast associated with pain. On examination, a mass approximately measuring 20 x 14 cm was present in the upper and lower quadrants of the left breast. The skin was hyperpigmented and distended veins were seen over the skin. There was no tethering to the skin. Nipple and areola were normal There were no palpable axillary nodes. A provisional diagnosis of phyllodes tumor was made. Enucleation of the lump was done under general anaesthesia. The specimen received by the pathology laboratory measured 16 X 10 X 5cms and weighed 750 gm (Fig.1).
Figure 1.

The enucleated specimen: Note the smooth outer surface denoting the well circumscribed nature of the mass.
The external surface was lobulated and the cut surface was nodular with focal white areas. Representative samples were taken and routinely processed. Haematoxylin and eosin stained four-micron sections showed a well circumscribed tumor composed of hyperplastic acini retaining the configuration of normal breast lobules (Fig.2). There was no evidence of atypia or malignancy. There was stromal hyalinisation.
Figure 2.
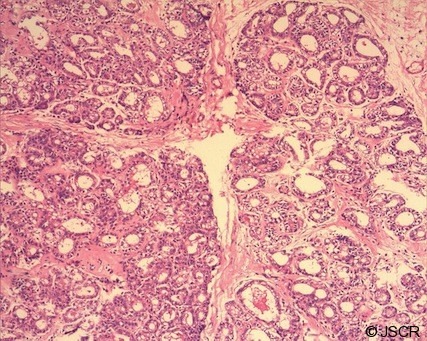
H&E, X 100. Hyperplastic acini retaining normal lobular configuration.
DISCUSSION
Lactating adenomas present as small, well circumscribed, freely mobile masses during pregnancy or lactation. Benign breast tumors associated with pregnancy can be of different types. In a study of 37 cases of benign breast tumors associated with pregnancy by O’ Hara et al, only eight cases were lactating adenomas.(1) The others were fibroadenomas with lactational changes and tubular adenomas.
Lactating adenoma is a rare tumor and there are differing views on its histogenesis. James et al considered lacating adenoma to be a pure and readily recognisable morphological form clearly distinguishable from tubular adenoma and fibroadenoma that is always related to current or recent pregnancy.(2) According to them, most tumors diagnosed as lactating adenomas are diagnosed during pregnancy and do not have lactational secretion. The secretory changes seen are similar to the physiological changes of pregnancy in the adjacent breast tissue. Hence they proposed the name “tumor of pregnancy”. The microscopic finding in our case is in accordance with this view. This is also supported by Slavin et al, who in a study of 30 cases of nodular breast lesions of pregnancy, described 12 lesions that fitted with the description of lactating adenoma. According to Slavin et al, lactating adenomas are nodules of physiologic lobular proliferation which become more prominent than the adjacent breast tissue and appear clinically to be a distinct mass and histologically resemble focal exaggerated physiological hyperplasia.(3)
Hertel et al however proposed that lactating adenomas arise in preexisting adenomas.(4) In a study by Hertel et al, five of the seven postpartum patients with tubular adenomas, first observed the lump during pregnancy, leading to the authors’ conclusion that tubular adenomas and lactating adenomas are two ends of a spectrum, the latter with secretory changes associated with physiological states of pregnancy. Both the views are given in the latest WHO fascicle on breast tumors, that is to say that a lacating adenoma is considered as a tubular type adenoma that may show extensive secretory changes in the epithelial cells during pregnancy and lactation.(5) It has also been suggested that such lesions represent focal accumulation of hyperplastic lobules.
Usually, lactating adenomas are slow growing tumors which are smaller than 5cm in size and are well demarcated from the surrounding breast tissue.(6) In a series of 14 lactating adenomas by James et al, most of the tumors were 2.5 – 3.5cm in size. The largest tumor in that series measured 7.8cms. The largest case reported in literature was by Reeves at al. They reported a giant breast mass which grew to a maximum size of 25 X 18cms.(7) The present case measured 16cms in diameter and qualifies for the second largest reported case of lactating adenoma.
Sonologically, lactating adenomas are oval, sharply circumscribed, solid hypoechoic mass which can have a prominent central tubular structure presumed to be a dilated duct.(8)
Lactating adenomas are characterised by glands with a tubuloalveolar architecture and florid secretory features. They resemble aggregates of lobules exhibiting secretory hyperplasia. The histologic changes relate to the stage of pregnancy and approximate the changes in the adjacent breast. If removed during pregnancy, the secretory changes are much less pronounced than in the tumor removed postpartum (6) as was observed in the present case.
The characteristic microscopic features of the tumors that come in the differential diagnosis is discussed by O’Hara, James and Slavin.(1,2,3) Tubular adenomas are characterised by uniform closely approximated tubular structures lined by epithelial and myoepithelial cells with little or no cytoplasmic vacuolisation. Fibroadenoma with secretory hyperplasia should be distinguished from lactating adenoma; the latter lacks the characteristic stroma in a fibroadenoma.
Rapid increase in size in a lactating adenoma can be due to infarction.(9) Reeves et al have also described rapid increase in size in their report of giant lactating adenoma. (7) Even though there was a history of pain and rapid growth, there was no evidence of infarction in the present case. Huge size and rapid increase in size can lead to a mistaken clinical diagnosis of malignancy. This is an important point to bear in mind. Histopathological examination easily distinguishes the two.
Enucleation is the recommended treatment for lactating adenomas as there is a low risk of recurrence. Bromocriptine, a dopamine agonist can be used to shrink the tumor before surgery. (7) Bromocriptine can suppress lactation, the benefits of tumor shrinkage must be weighed against the cessation of lactation in a mother who is breast feeding.
In summary we report a case of a lactating adenoma presenting as a giant breast mass. In a case of rapidly enlarging breast mass in a pregnant lady, lactating adenoma has to be considered in the differential diagnosis.
REFERENCES
- 1.O’Hara M F, Page D L. Adenomas of the breast and ectopic breast under lactational influences. Hum Pathol 1985;16:707–712 [DOI] [PubMed] [Google Scholar]
- 2.James K, Bridger J, Anthony PP. Breast tumour of pregnancy (‘Lactating adenoma’). Journal of Pathol 1988;156:37–44 [DOI] [PubMed] [Google Scholar]
- 3.Slavin JL, illson V R, Ostor AG. Nodular breast lesions during pregnancy and lactation. Histopathology 1993;22:481–485 [DOI] [PubMed] [Google Scholar]
- 4.Hertel BF, Zaloudek C, Kempson RL. Breast adenomas. Cancer 1976;37:2891–905 [DOI] [PubMed] [Google Scholar]
- 5.Bussolati G, Tavassoli FA, Nielsen BB, Ellis IO, MacGrogan G. Benign epithelial proliferations. Chapter in WHO Pathology and genetics of tumors of the breast and female genital system. Tavassoli FA, Devilee P. eds. Lyon: IARC press; 2000. p81–88 [Google Scholar]
- 6.Rosen PP.andOberman HA. Benign Epithelial lesions. Chapter in tumors of the mammary gland. Atlas of Tumor Pathology. Rosai J.andSobin LH. eds. Washington D.C: ARP press AFIP;1992. p67–96 [Google Scholar]
- 7.Reeves ME, Tabuenca A. Lactating adenoma presenting as a giant breast mass. Surgery 2000;127:586–8 [DOI] [PubMed] [Google Scholar]
- 8.Sumkin FH, Perrone AM, Harris KM, Nath ME, Amortegui AJ, Weinstein BJ. Lactating adenoma: US features and literature review. Radiology 1998;206:271–274 [DOI] [PubMed] [Google Scholar]
- 9.Behrndt VS, Barbakoff D, Askin FB, Brem RF. Infarcted lactating adenoma presenting as rapidly enlarging breast mass. Am J roentgenol 1999;173:933–935 [DOI] [PubMed] [Google Scholar]


