Abstract
Termed as a rare entity so far “abdominal cocoon” which is an encasing of the small bowel within the fibrous membrane is usually of unknown origin, although at times, it may be seen secondary to a variety of conditions. Though described in literature as a rare entity we report a case of tubercular abdominal cocoon in 15 year old boy. This case report emphasizes the importance of this surgical condition in a tuberculosis endemic region.
INTRODUCTION
Abdominal cocoon is a rare condition also known in the literature as ‘sclerosing encapsulating peritonitis’(1). The term “abdominal cocoon” was first applied by Foo et al in 1978 (2). It is characterized by partial or complete encapsulation of the small bowel by fibrocollagenous membrane called cocoon with local inflammatory infiltrate leading to acute or chronic small bowel obstruction. (1, 3)
CASE REPORT
A 15 year old male child, presented with complaint of cholicky abdominal pain since 7 days and distension since 3 days. He had a past history of pulmonary tuberculosis and was a defaulter. On examination, the abdomen was mildly distended and tenderness was present in the periumblical region. A firm to hard mobile mass approximately 5 cm. x 7 cm. in size was palpable in umbilical region. It was intra-abdominal and intra-peritoneal. Bowel sounds were exaggerated. Per rectal examination was normal. ESR was 110 mm in 1st hr. On plain X-ray examination, significant air fluid levels and dilated small bowel loops were found (Fig.1).
Figure 1.
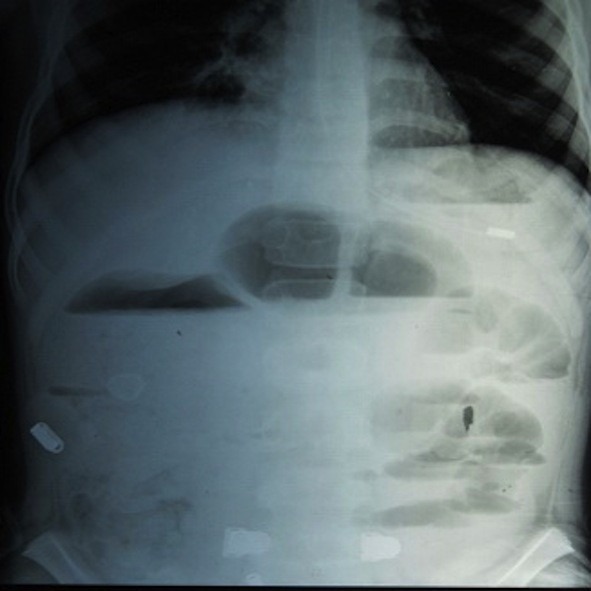
X-ray film showing significant air fluid levels and dilated small bowel loops.
USS examination showed features of intestinal obstruction with ascites. CT revealed small bowel obstruction with minimal fluid collection. On exploratory laparotomy, gut loops were found to be adherent and encased in a membrane (Fig.2).
Figure 2.

Intra operative Snapshot showing adherent gut loops encased in a membrane.
A stricture was also present in the jejunum. Mesentric lymph nodes were enlarged. The membrane was dissected and adhesilolysis was done along with sticturoplasty of the jejunal stricture. The white fibrous membrane and the enlarged lymph node were sent for histopathologcal examination. On histopathological examination of the lymph node showed characteristic granulomatous lesions showing caseous necrosis in the centre, and a prominent cuff of lymphocytes and plasma cells at the periphery. Acid-fast stain of the small granulomas was positive. Pieces from membrane showed loose connective tissue, infiltration by an admixture of lymphocytes, plasma cells, and giant cells. Patient was started on antitubercular treatment postoperatively and the outcome was satisfactory.
DISCUSSION
Tubercular abdominal cocoon, is a rare entity. To the best of our knowledge, the review of literature of abdominal cocoon due to tubercular etiology shows that only 22 cases have been reported which included only 9 male patients so far. The primary or idiopathic form is common in adolescent females from tropical and subtropical countries and is thought to be due to subclinical primary viral peritonitis as an immunological reaction to gynecological infections and retrograde menstrual flow. Since it is also seen in males, premenstrual females and children, the exact aetiology is thus unclear. Secondary cocoon occurs due to immunological disorders (like SLE, sarcoidosis), infections (tuberculosis), peritoneal shunts (Lee Veen Shunt for refractory ascites), chronic ambulatory peritoneal dialysis, intraperitoneal drug installation (the use of poviodine for abdominal wash-out), use of β-adrenergic blocker-Practolol and gynecological problems like leiomyoma of uterus, endometriotic cyst and tumors of ovary.
An abdominal mass may or may not be present. It is difficult to make preoperative diagnosis on the basis of barium follow-through and computed tomogram (CT) scan and the diagnosis is made at laparotomy when encasement of small bowel within the sac like cocoon is visualized. However the classic barium study findings are serpentine or concertina like configuration of dilated small bowel loops in a fixed U shaped cluster so called cauliflower like appearance and delayed transit of contrast medium and computed tomography findings of the abdomen include small bowel loops congregated to the center of the abdomen encased by a soft-tissue density mantle (1,4). However, preoperative diagnosis requires high index of clinical suspicion. Although the disease primarily involves the small bowel, it can extend to involve other organs like the large intestine, liver and stomach.
The treatment is usually excision of the covering membrane. Diagnostic laparoscopy in this era has a major role in the management of rare causes of intestinal obstruction such as abdominal cocoon (5). Surgery (membrane dissection and extensive adhesiolysis) is the treatment of choice.
In our case, the cocoon secondary to tuberculosis was reported in an adolescent male, who presented with a complete small bowel obstruction which was unresponsive to conservative management. At surgery, in addition to the covering membrane, there were dense interbowel adhesions that also needed to be freed in order to relieve the obstruction.
Other manifestations of abdominal tuberculosis include mesenteric abscesses, enlarged and caseating mesenteric lymph nodes, and tubercles over the bowel serosa are also commonly encountered, that may suggest a tubercular aetiology. Once the diagnosis of tuberculosis is established patient needs to be put on standard anti-tubercular treatment.
Tubercular abdominal cocoon is a rare cause of small bowel obstruction. The nonspecific clinical picture and benign imaging findings make the diagnosis difficult. A high index of suspicion is required in the absence of other possible causes of abdominal obstruction.
REFERENCES
- 1.Deeb LS, Mourad F, El-Zein Y, Uthman SM. Abdominal cocoon in a man: preoperative diagnosis and literature review. Clin Gastroenterol 1998:26;148–50 [DOI] [PubMed] [Google Scholar]
- 2.Foo KT, Ng KC, Rauff A, Foong WC, Sinniah R. Unusual small intestinal obstruction in girls: the abdominal cocoon. Br J Surg 1978;65:427–30 [DOI] [PubMed] [Google Scholar]
- 3.Cambria RP, Shamberger RC. Small bowel obstruction caused by the abdominal cocoon syndrome: possible association with LeVeen shunt. Surgery 1984;95:501–3 [PubMed] [Google Scholar]
- 4.Hur J, Kim KW, Park MS, Yu JS: Abdominal cocoon: preoperative diagnostic clues from radiologic imaging with pathologic correlation. Am J Roentgenol 2004;182:639–41 [DOI] [PubMed] [Google Scholar]
- 5.Qasaimeh GR, Amarin Z, Rawshdeh BN, El-Radaideh KM. Laparoscopic Diagnosis and Management of an Abdominal Cocoon: A Case Report and Literature Review. Surg Laparosc Endosc Percutan Tech. 2010;20(5):e169–171 [DOI] [PubMed] [Google Scholar]


