Abstract
Clostridium perfringens sepsis with intravascular haemolysis is a catastrophic process with a reported mortality of between 90 to 100%. We successfully treated a case of severe clostridial infection with a liver abscess following laparoscopic cholecystectomy, the first to our knowledge. A 59-year-old man presented one week after an uneventful laparoscopic cholecystectomy with jaundice, peritonism, sepsis and acute renal failure. He was found to have a haemolytic anaemia, unconjugated hyperbilirubinemia and blood cultures grew Clostridium perfringens. A CT revealed a large gas forming abscess in the gallbladder fossa and right lobe of liver. He was treated with directed antibiotic therapy and underwent emergency laparotomy, drainage of the abscess and peritoneal washout. He required intensive care support, parenteral nutrition and inotropic support for a limited period. CT liver angiogram post op was normal. Continued renal dysfunction necessitated protracted haemofiltration. This resolved and the patient was discharged home at 2 months.
INTRODUCTION
Clostridium perfringens sepsis with intravascular haemolysis is a catastrophic process with a reported mortality of between 70 to 100%. (1)
Cases of clostridial infections following conventional biliary surgery first appear in the literature in 1960’s (2). Graybeal summarised 3 cases of clostridial sepsis and highlighted a reported total of 24 in 1982 (3). It is around this time that laparoscopic surgery began to explode onto the scene. Despite the ubiquitous practice of this operation there have been fortunately few reports of clostridial sepsis as a sequelae. The first report was in 1996 (4)and there have been few since (5) (4 in total).
The clinical pattern varies in the cases observed – sepsis, peritonitis and emphysematous myonecrosis being the variants to date. Rapid deterioration, haemolysis, septic shock and renal dysfunction are common to all (2-6). We observed a case of severe clostridial infection with a liver abscess following laparoscopic cholecystectomy, the first to our knowledge.
CASE REPORT
A 59 year old man with non-insulin dependent diabetes was initially admitted with gallstone pancreatitis. He underwent an Endoscopic retrograde cholangiopancreatography (ERCP) to clear a single stone from the common bile duct and a papillotomy was performed. After convalescing he proceeded to laparoscopic cholecystectomy at a 6 month interval. No cholangiogram was indicated given the recent papillotomy and he was discharged within 24hours without event.
One week later he re-presented with jaundice, peritonism, sepsis and acute renal failure. On arrival his Haemoglobin measured 9.1 but fell to 6.8g/dl within 12hours. Initial blood samples were haemolysed and a blood film revealed marked red cell spherocytes and occasional nucleated red cell – in keeping with haemolysis. Blood cultures grew Clostridium perfringens.
Initial treatment comprised intravenous fluid resuscitation, high flow oxygen and broad spectrum antibiotics (Tazocin, Gentamicin and Metronidazole). He proceeded to CT scan which demonstrated a gas filled cavity in and under the right lobe of liver. A laparotomy was performed, revealing a large abscess cavity in the right lobe of liver emanating from the gallbladder fossa. This contained pockets of gas. The bile duct was found intact and the cystic duct clips secure. The pus was drained and a generous peritoneal lavage performed. Large bore (32Fr) sub-hepatic and sub-phrenic drains were placed.
Post-operatively the patient was ventilated, continued on broad spectrum antibiotics, transfused packed red cells, fed parenterally initally, and haemofiltered for acute renal failure. Ventilatory and inotropic support were able to be weaned quickly and the jaundice improved over the following week. The abdominal drains were removed sequentially once dry.
There was a protracted recovery period thereafter with bilateral pleural effusions and persistent renal dysfunction. At 3 weeks post re-admission a repeat CT revealed a persistent small collection in the gallbladder fossa and CT guided drainage was attempted through the right 8th intercostal space. This yielded minimal debris only. A massive haemothorax developed after the patient was heparinised for haemofiltration later that day. Intercostal chest drain yielded over 2 litres of blood and clot and a mini-thoracotomy was later required to clear the pleural cavity completely.
Fig 1.
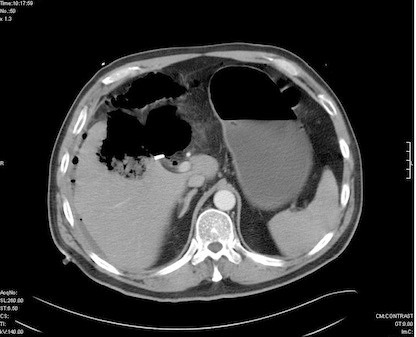
CT at re-admission 1 week post lap chole - Free intraperitoneal gas abscess in gallbladder fossa
Fig 2.

Findings at laparotomy - Purulent slough and emphysema in the gallbladder fossa
Fig 3.
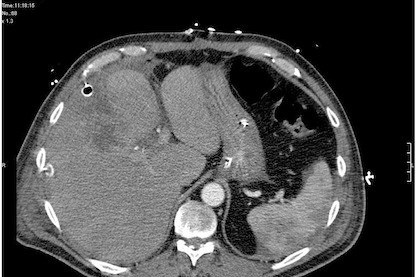
Repeat CT post-laparotomy and lavage showing large bore peritoneal drains
The patient was transferred to the care of the renal physicians. The renal function improved, diuresis resumed and the patient eventually weaned from dialysis. He was discharged at 2 months.
DISCUSSION
Infectious complications of laparoscopic cholecystectomy most commonly consist of port site infection and intra-abdominal abscess. The risk of these complications has been noted to be reduced from an incidence of 2.8 to 0.5% by the administration of peri-operative antibiotics.
In a 10-year study of pyogenic liver abscess, Clostridium perfringens was cultured in only one of 79 cases (7) making it a relative rarity as a cause of primary liver abscess. The organism is widely distributed in the intestinal flora of the majority of humans and a small percentage of normal and inflamed gallbladders. Positive cultures for Clostridium perfringens have been reported to be found in 1 to 19% of surgically removed gallbladders (8). The question of the pathogenesis of clostridial sepsis post cholecystectomy remains unanswered given that such a low incidence is reported in the face of a relatively high rate existence of the bacteria.
There are various theories as to the development of bactobilia; entero-hepatic, ascending & haematogenous routes.
The diagnosis of Clostridium perfringens sepsis following laparoscopic cholecystectomy requires a high index of suspicion. The number of reported cases is too few to allow analysis of the common presenting factors. The mode of presentation does however comprise anecdotally consistent findings; abdominal pain, jaundice, haemolysis, renal dysfunction, confusion and occasionally crepitus, if gas gangrene is present. Haemodynamic parameters may be falsely re-assuring initially. Significantly the patients are almost always diabetic.
The mode of presentation is often similar to necrotising fascitiis, which has been more widely reported following laparoscopic surgery and is most often the result of mixed bacteriological agents, commonly gram negative enteric bacilli, staphlococcal and streptococcal species.
It is thought that Clostridium perfringens sepsis presents in three different modes – simple contamination, clostridial crepitant cellulitis and finally as gas gangrene.
Our case is unique not only as Clostridium perfingens sepsis following laparoscopic cholecystectomy is rarely seen, but for being the first to report an associated gas forming liver abscess. That the patient survived is surprising and attributed to the rapid and aggressive intervention to remove the nidus of infection.
REFERENCES
- 1.Rogstad B, Ritland S, Lunde S, Hagen AG. Clostridium Perfringens septicaemia with massive hemolysis. Infection. 1993. 21:60–2 [DOI] [PubMed] [Google Scholar]
- 2.Turner FP. Fatal Clostridium Welchii Septicemia Following Cholecystectomy. Am J Surg. 1964. Jul. 108:3–7 [DOI] [PubMed] [Google Scholar]
- 3.Graybeal GE. Clostridial sepsis following biliary surgery: a report of three patients and a review of the literature. Del Med J. 1982. Sep. 54(9):493–8 [PubMed] [Google Scholar]
- 4.Bush GW, Clements RH, Phillips M, Kent RB., Jr Clostridium perfringens sepsis with intravascular hemolysis following laparoscopic cholecystectomy: a newly reported complication. Am Surg. 1996. Apr. 62(4):326–7 [PubMed] [Google Scholar]
- 5.Samel S, Post S, Martell J, Becker H. Clostridial gas gangrene of the abdominal wall after laparoscopic cholecystectomy. J Laparoendosc Adv Surg Tech A. 1997. Aug. 7(4):245–7 [DOI] [PubMed] [Google Scholar]
- 6.Mittermair RP, Schobersberger W, Hasibeder W, Allerberger F, Peer R, Bonatti H. Necrotizing fasciitis with Clostridium perfringens after laparoscopic cholecystectomy. Surg Endosc. 2002. Apr. 6(4):716 Epub 2001 Nov 30 [DOI] [PubMed] [Google Scholar]
- 7.Hansen PS, SchØnheyder HC. Pyogenic hepatic abscess. A 10-year population-based retrospective study. APMIS. 1998. Jan. 106(1–6): 396–402 [DOI] [PubMed] [Google Scholar]
- 8.Magee HR. Clostridium Perfringens Infection of the Biliary Tract. ANZ Journal of Surgery. 1967. Nov. 37(2): 177–183 [DOI] [PubMed] [Google Scholar]


