Abstract
A 73-year-old lady presented with clinical features of gastric outlet obstruction. It was found to be secondary to a spontaneous haematoma in duodenal wall as a complication of warfarin therapy given for atrial fibrillation. The diagnosis was confirmed by abdominal CT scan and upper G I endoscopy. Warfarin was stopped and blood transfusions given. She recovered completely after three weeks of conservative treatment. Repeat CT scan and upper G I endoscopy done after two months showed complete resolution.
INTRODUCTION
We present a rare case of gastric outlet obstruction caused by intramural haematoma as a complication of warfarin therapy and there are hardly any case reports in the literature of gastric outlet obstruction with same etiology although cases of small bowel obstruction have been reported.
Spontaneous intestinal hematoma is a rare complication of anticoagulant therapy, and small bowel obstruction caused by intramural hematoma secondary to anticoagulant therapy is even rarer. The first symptom is usually abdominal pain, frequently accompanied by nausea and vomiting. A history of anticoagulant use with prolonged international normalized ratios in patients presenting with abdominal pain should alert physicians to search for this entity. Typical findings on abdominal computed tomography yield the diagnosis. Early diagnosis is crucial because most patients are treated non-operatively with a good outcome.
CASE REPORT
A 73-year-old woman was admitted via emergency to the medical unit with symptoms of abdominal pain, dysuria and persistent vomiting of three days duration. She was started on treatment for a presumed UTI, with IV fluids and antibiotics.
She had been on warfarin for atrial fibrillation for last three years with a target INR range of between 2 and 3 and her INR being 2.6 on admission. She had an extensive medical background including type II diabetes mellitus, hypertension, angina and COPD.
Shortly after admission she suffered an episode of coffee-ground vomiting when her warfarin was stopped and a surgical opinion was sought. Plain x-ray abdomen showed huge gas shadow consistent with gastric outlet obstruction.
Fig. 1.
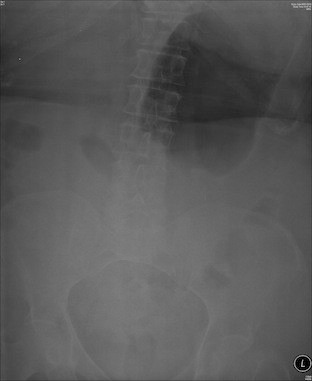
Abdominal x-ray showing huge gas shadow consistent with gastric outlet obstruction
A repeat blood test on day 2 of admission revealed low haemoglobin of 7.0 compared to 11.0 gm on admission and she received two units of blood. She had persistently low potassium for which reason she was transferred to HDU where she received K replacement. She was started on IV digoxin and naso-gastric tube was already inserted due to persistent bilious vomiting.
Despite no obvious cause of blood loss her haemoglobin was discovered to be low again at 8.5 gm on day 6 of admission. At this time, she received two more units of blood. An upper G I endoscopy (OGD) was arranged which revealed extensive mucosal oedema, bruising and narrowing of the first and second parts of the duodenum. CT scan of the abdomen was performed, which revealed a 10cm RUQ mass, compressing on and contiguous with 2nd part of duodenum, presumed to be a sizeable haematoma. A small amount of free blood in the peritoneal cavity and pelvis was also noted.
Fig. 2.
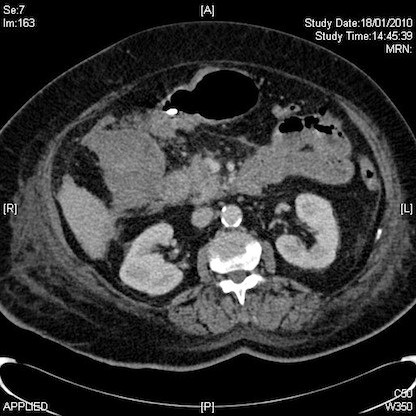
Abdominal CT Scan revealed a 10cm right upper quadrant mass
Once the diagnosis of gastric outlet obstruction due to compressing haematoma was established on CT, she received vitamin K and subsequently was managed conservatively under the combined care of the surgeons, haematologist, cardiologist and nutritionists. Her nasogastric tube remained in situ and it kept draining loads of biliary aspirate since her admission.
Within a few days she started improving, the aspirate decreased in amount gradually and her laboratory parameters returned slowly to normal. AF was being managed using digoxin and aspirin, warfarin having been permanently discontinued. She was discharged home in a stable condition on day 20 of her admission, when she had completely recovered from gastric outlet obstruction.
Two months following the initial episode, a follow-up OGD and abdominal CT scan were arranged. OGD showed absolutely normal stomach and duodenum. CT scan showed resolving periduodenal haematoma and resolved pelvic haemoperitoneum. She was subsequently seen as an outpatient and discharged from surgical care, with the advice to permanently stop warfarin.
DISCUSSION
MacLauchlan described the first report of intramural intestinal haematoma in an article published in Lancet in 1838 (1) and the first radiological description was made by Liverud (1). In 1904, Sutherland reported a case of traumatic haematoma causing intussusception in a child suffering from Henoch-Schonlein purpura. Four years later, Von-Khautz diagnosed this condition in a patient with haemophilia (2). Following these initial reports, there has been increase in incidence and publications, through the use of warfarin, which is the main risk factor.
Haemorrhage following prolonged anticoagulant administration is a well recognised risk but intramural haematoma of intestine is a rare complication of this therapy (3). The usual presentation of such patients is with abdominal pain and vomiting. Most of patients are likely to have abnormal coagulation profile on admission although this was not the case in our patient. The combination of warfarin induced anticoagulation, bowel wall thickening due to haemorrhage and intestinal obstruction are characteristic of intramural haematoma of small intestine (4).
Plain abdominal X-Ray can be informative, but contrast enhanced abdominal CT is the key to final diagnosis. Gastroscopy may be helpful in few patients, especially those having associated overt gastrointestinal bleeding. Most patients have single haematomas but there had been few cases of multiple hematomas as reported in literature (5). The differential diagnosis of mucosal thickening should include inflammatory diseases, infections, neoplastic conditions and ischemic aetiology (6). Intramural haematoma most commonly involves the jejunum, followed by ileum and the duodenum (7). The intramural bleeding is most commonly located in the submucosa, followed by retroperitoneal, intramesenteric and intraluminal locations (8,9,10).
Most, but not all patients with intramural haematoma are managed conservatively. Aspiration of gastrointestinal contents, bowel rest and reversal of anticoagulant effects, vitamin K and repeated blood transfusions are key to success. Only few patients would require operative intervention.
Non-traumatic duodenal intramural haematoma is extremely rare presentation of anticoagulation therapy and our patient is probably the first in reported literature that presented as a case of gastric outlet obstruction. Clinical suspicion necessitates early imaging and abdominal CT is mandatory to establish a diagnosis. After review of literature reported over more than last fifty years, we recommend that most patients can be managed conservatively, although the duration of treatment may vary between 1-3 weeks. Very close monitoring of anticoagulant treatment in these patients should be followed.
REFERENCES
- 1.McLauchlan J. False aneurysmal tumour occupying nearly the whole of the duodenum. Lancet. 1838;2:203–205 [Google Scholar]
- 2.Von Khautz A. Darmstenose durch submuköse Hämatome bei Hämophilie. Arch Klin Chir. 1908;87:542–551 [Google Scholar]
- 3.Polat C, Dervisoglu A, Guven H, Kaya E, Malazgirt Z, Danaci M, Ozkan K. Anticoagulant-induced intramural intestinal hematoma. American Journal of Emergency Medicine. 2003;21(3):208–211 [DOI] [PubMed] [Google Scholar]
- 4.Cadavid AM, Uribe JD, Mesa M, Escobar S, Sanchez LF. Spontaneous small-bowel hematoma: Report of two cases and literature review. Revista Colombiana de Cardiologia. 2009;16(6):261–265 [Google Scholar]
- 5.Abbas MA, Collins JM, Olden KW, Kelly KA. Spontaneous intramural small-bowel hematoma: clinical presentation and long-term outcome. Archives of Surgery. 2002;137(3)306–10 [DOI] [PubMed] [Google Scholar]
- 6.Lane MJ, Katz DS, Mindelzun RE, Jeffrey RB., Jr Spontaneous intramural small bowel haemorrhage: Importance of non-contrast CT. Clin Radiol. 1997;52:378–380 [DOI] [PubMed] [Google Scholar]
- 7.Cheng J, Vemula N, Gendler S. Small bowel obstruction caused by intramural haemorrhage secondary to anti-coagulant therapy. Acta Gastro-Enterologica Belgica, July 2008;71(3):342–344 [PubMed] [Google Scholar]
- 8.Herbert DC. Anticoagulant therapy and the acute abdomen. Br J Surg. 1968;55: 353–357 [DOI] [PubMed] [Google Scholar]
- 9.Wiot JF, Weinstein AS, Felson B. Duodenal hematoma induced by coumarin. AJR. 1961;86:70–75 [PubMed] [Google Scholar]
- 10.Segaul AI, Mills M, Wertheimer HM. Intramural hematoma of the small intestine as a complication of anticoagulant therapy. Am J Surg. 1964;107:891–894 [DOI] [PubMed] [Google Scholar]


