Abstract
Acute appendicitis is a frequent pathology encountered by general surgeons. On the differential of aetiologies that can lead to this diagnosis lies the spectrum of infectious disease. We present a case report of a patient who presented to our institution as a classic acute appendicitis. Upon histological analysis it became evident that he had spirochetosis of the cecum and appendix. This paper reviews the literature on this rare infectious aetiology. A synopsis of the microbiology, epidemiology, clinical manifestations and treatments for intestinal spirochetosis is described. At large, the aim of this paper is to heighten awareness of this disease amongst clinicians and specifically surgeons.
INTRODUCTION
A man presented with clinical and radiographic evidence consistent with an acute appendicitis. After an ileocolic resection he was found to have intestinal spirochetosis of the caecum. We describe his case and review the literature on this rare pathogen.
CASE REPORT
A 50-year–old- male presented to our institution in November with a three-day history of right lower quadrant abdominal pain associated with nausea. He denied any other symptoms. His past medical history was significant for gastroesophageal reflux disease and migraine headaches. His only medication was a daily Esomeprazole.
Upon assessment in the emergency department, he did not appear ill and was afebrile. Abdominal examination revealed localized guarding at McBurney's point. His white blood cell count was 12.0 x 109 cells/L. Computed tomography abdomen and pelvis revealed a markedly dilated appendix measuring 1.3 cm with fat stranding and enlarged lymph nodes. The caecal wall appeared irregular and thickened (Figure 1). The clinical impression at the time was consistent with an acute appendicitis with a potential caecal neoplasm.
Fig. 1.
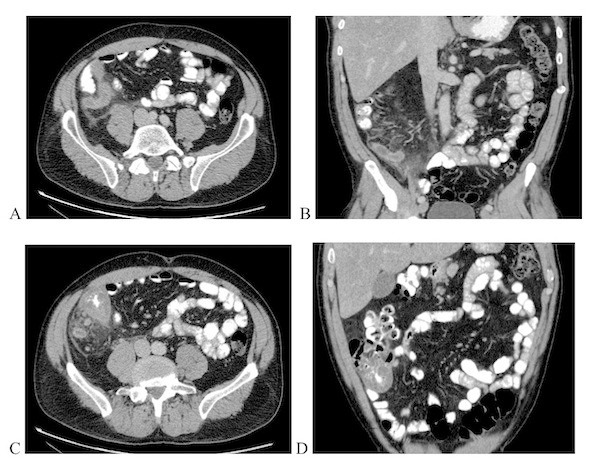
Computed tomography images obtained preoperatively. Axial (a) and coronal (b) views of inflamed appendix. Axial (c) and coronal (d) views of thickened caecal wall and adenopathy.
The patient was given intravenous antibiotics and taken to the operating room within 5 hours of his initial presentation. A transverse right lower quadrant incision of the abdomen revealed an enlarged, firm appendix adherent to the lateral peritoneum was identified. The area of caecum surrounding the appendiceal base was firm and adjacent mesentery was oedematous. A neoplasm could not be adequately ruled out in the setting of an emergency operation with difficult anatomical visualization. An ileocolic resection was therefore performed with creation of a standard functional end-to-end ileocolic anastomosis using gastrointestinal staplers.
The patient tolerated the procedure well and was discharged home on postoperative day 7. The patient was also placed on a 10-day course of antibiotics (Ciprofloxacin and Metronidazole) postoperatively as the intra-operative impression was highly suspicious for a contained perforated viscus.
At follow-up 10 days post-discharge the patient complained of occasional loose bowel movements but was otherwise feeling well. His pathology was consistent with an acute appendicitis. Twelve reactive lymph nodes were noted, all negative for malignancy. An unexpected finding of substantial eosinophilic infiltration of the appendix was identified. Further examination showed intestinal spirochetosis along the caecal border (Figure 2).
Fig 2.
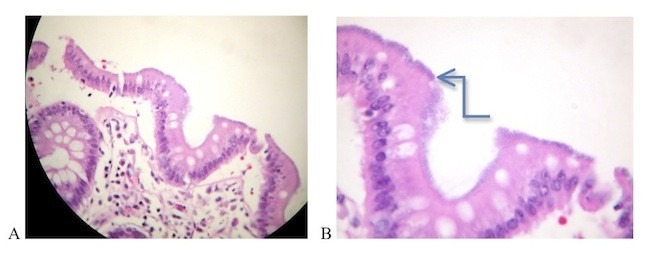
Histopathology of appendix and cecum (a): Appendix. Eosinophils and neutrophils predominantly visualized in appendix mucosa. (H&E staining, light microscopy, magnification x 200) (b): Caecum. Note false brush border (arrow) composed of intestinal spirochetosis adhering to caecal mucosal epithelium. (H&E staining, light microscopy, magnification x 400)
The patient returned for follow up one month after surgery and was clinically well. At a subsequent visit 3 months later, he had a colonoscopy showing few diveritcula and a significant spasm. To our knowledge, he continues to remain asymptomatic.
DISCUSSION
Intestinal Spirochetosis (IS) was first discovered in 1719 by van Leeuwenhoek who analyzed his own stool and identified small mobile spiral organisms.(1) IS is a rare disease wherein gram negative bacteria belonging to the Spirochetes species infect the gastrointestinal tract. Spirochete organisms are classified into 3 groups: Spirochaetaceae, Leptospiraceae and Brachyspiraceae (2). Two distinct groups have been identified to predominantly colonize human colorectum: Brachyspira Aalborgi and Brachyspira Pilosicoli.
Morphologically, IS is characterized by the presence of microorganisms attached to colorectal epithelial cells in a perpendicular fashion. Histologically they form a diffuse blue fringe along the border of the epithelial layer (with hematoxylin-eosin staining). This finding has been named the “false brush border”. Although invasion beyond the mucosal border is rare, mast cell and IgE plasma cell reactions have been reported. It is suspected that loss of integrity of the mucosal surface may play a role in the mechanism of invasion.(1)
The epidemiology of IS was first described in the 20th century. A report published in 1923 in Chicago revealed a 28% prevalence in stools of healthy individuals (3). Since then, other reports have demonstrated a direct relationship between the incidence of spirochetosis and rapidly growing industrial towns, homosexual men and patients infected with the human immunodeficiency virus (HIV) (2). Prevalence ranges from 1-5% in healthy individuals and within developed countries (4) to 64.3% in healthy individuals in a village in India (5). Difficulty with measuring prevalence resides in the sensitivities of methods of detection, which over the years has encompassed histology, microscopy, PCR, and in-situ-hybridization from fecal and/or tissue specimens.
The endoscopic appearance of IS unfortunately does not aid in its diagnosis. A retrospective study examined the colonoscopic descriptions of 15 patients with biopsies consistent with IS. Seven patients were noted to have a “polypoid” appearance, an “erythematous mucosa” was noted in one patient, a “lesion” was noted in one patient and the remaining 6 patients had normal mucosa (6). IS has been described to involve the mucosa of the colon, rectum and appendix.
The severity of clinical manifestation has been correlated with the degree of histological invasion as evidenced by intestinal epithelial injury. However, it must be noted that presence of fecal spirochetes does not coincide with symptomatology. Many individuals found to harbour spirochetes have been asymptomatic. Associated symptoms described include blood tinged feces, abdominal pain, constipation and most commonly diarrhea (1). A little over ten cases of systemic spirochetemia (mainly secondary to B. Pilosicoli) have been described in critically ill patients (7).
Few reports in the literature (amounting to less than 30 patients) have described patients with intestinal spirochetosis who presented with a clinical and histological picture of acute appendicitis (8,9). In 1984, Henrik-Nielson and colleagues studied 681 appendiceal specimens and found IS to be associated with 12.3% of clinically suspicious appendicitis that proved to be histologically normal whereas only 0.7% of IS cases had a co-existing confirmed appendicitis on histology (8). Intestinal spirochetosis in the appendix, therefore, has a spectrum of presentation ranging from asymptomatic to fulminant histologically proven appendicitis.
No consensus guidelines for the treatment of intestinal spirochetosis exists as only successful case reports of trial antibiotic regimens have been described. Generally, a trial of antibiotic therapy is warranted, especially when the patient is symptomatic and/or histology shows signs of invasion. Treatment with metronidazole administered at 500 mg q.i.d. for 10 days has been reported to eradicate symptoms and may lead to negative fecal cultures and improvement in histological features (4).
At our institution, we treat many patients with HIV. It is estimated that the prevalence of IS in the HIV and in the homosexual population is as high as 54% (1). Most of these patients present with a chronic diarrhea and have a delayed diagnosis secondary to prolonged culture growth and low suspicion of this aetiology. In about two thirds of cases, patients with HIV diagnosed with IS suffer from severe underlying disease and/or immunosuppression leading to death (10). Awareness of this disease entity should be heightened among surgeons especially those who treat patients with HIV.
References
- 1.Korner M, Gebbers J.-O. Clinical Significance of Human Intestinal Spirochetosis- A Morphologic Approach. Infection 2003;5:341–349 [DOI] [PubMed] [Google Scholar]
- 2.Eriandson KM, Klingler ET. Intestinal spirochetosis: epidemiology, microbiology and clinical significance. Clin Microb Newsletter. 2005;12(5):91–96 [Google Scholar]
- 3.Parr LE. Intestinal Spirochetosis. J Infect Dis. 1923;33:369–83 [Google Scholar]
- 4.Peghini PL, Guccion JG, Sharma A. Improvement of chronic diarrhea after treatment for intestinal spirochetosis. Dig Dis Sci. 2000;45(5):1006–10 [DOI] [PubMed] [Google Scholar]
- 5.Teglbajaerg PS. Intestinal Spirochaetosis. Curr Top Pathol. 1990;81:247–56 [PubMed] [Google Scholar]
- 6.Alsaigh N, Fogt F. Intestinal spirochetosis: clinicopathological features with review of the literature. Colorectal Dis 2002;4(2):97–100 [DOI] [PubMed] [Google Scholar]
- 7.Bait-Merabet L, Thille A, Legrand P, Brun-Buisson C, Cattoir V. Brachyspira Piloscoli bloodstreem infections: a case report and review of the literature. Ann Clin Microbiol Antimicrob. 2008;7:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Henrik-Nielsen R, Lundbeck FA, Teglbjaerg PS, Ginnerup P, Hovind-Hougen K. Intestinal spirochetosis of the vermiform appendix. Gastroenterology 1985;88: 971–977 [DOI] [PubMed] [Google Scholar]
- 9.Yang M., Lapham R. Appendiceal Spirochetosis. South Med J. 1997;90(1):30–2 [DOI] [PubMed] [Google Scholar]
- 10.Ena J, Simón-Aylón A, Pasquau F. Intestinal spirochetosis as a cause of chronic diarrhea in patients with HIV infection: case report and review of literature. Int J STD AIDS 2009;20:803–805 [DOI] [PubMed] [Google Scholar]


