Abstract
Sphingosine 1-phosphate (S1P) is a potent sphingolipid mediator that acts through five cognate G protein-coupled receptors (S1P1–S1P5) and regulates many critical biological processes. Recent studies indicated that S1P at nanomolar concentrations significantly reduces cytokine-induced apoptosis of pancreatic β-cells in which genes for S1P1–S1P4 are co-expressed. However, the S1P receptor subtype(s) involved in this effect remains to be clarified. In this study, we investigated the potential role of S1P2 in streptozotocin (STZ)-induced apoptosis of pancreatic β-cells and progression of diabetes. S1P2-deficient (S1P2−/−) mice displayed a greater survive ability, lower blood glucose levels, and smaller numbers of TUNEL-positive apoptotic β-cells to administration of a high dose of STZ than wild-type (WT) mice. S1P2−/− mice showed higher insulin/glucose ratios (an index of relative insulin deficiency) and larger insulin-positive islet areas to administration of a low dose of STZ than WT mice. Moreover, administration of JTE-013, a S1P2-specific antagonist, to WT mice ameliorated STZ-induced blood glucose elevation and reduced the incidence of diabetes. Our findings indicate that blockade of S1P2 signaling attenuates STZ-induced apoptosis of pancreatic β-cells and decreases the incidence of diabetes.
Keywords: Blood glucose, Diabetes, Insulin, S1P2-deficient mice, S1P2-specific antagonist
Introduction
Type 1 diabetes is an autoimmune disease that results in the destruction of pancreatic β-cells, whereas type 2 diabetes is a much more common disorder caused by insulin resistance and relative insulin deficiency. Insulin resistance in type 2 diabetes is initially managed by enhanced secretion of insulin from β-cells; however, this may gradually lead to a decrease in β-cell mass and deterioration of key β-cell functions such as glucose-stimulated insulin secretion. Therefore, β-cell failure is a key pathogenic process in both type 1 and 2 diabetes [1,2].
Sphingosine 1-phosphate (S1P) is a bioactive lipid mediator that exhibits diverse biological functions in most cell types and regulates many pathological processes, acting through five cognate high-affinity receptors (S1P1–S1P5) [3,4]. S1P was found to ameliorate cytokine-induced apoptosis of β-cells [5,6] in which genes for S1P1–S1P4 are co-expressed [7]. Previous studies demonstrated that S1P2 signaling induces intracellular calcium mobilization leading to increased glucose uptake in myoblasts [8], and RNA-based screening for genes that confer insulin resistance to 3T3-L1 adipocytes identified S1pr2 as a candidate [9], suggesting that S1P2 plays an important role in the pathogenesis of diabetes. In the present study, we examined the role of S1P2 in streptozotocin (STZ)-induced apoptosis of β-cells and progression of diabetes using S1P2-deficient (S1P2−/−) mice as well as the S1P2-specific antagonist JTE-013.
Materials and methods
Animals
S1P2−/− mice were generated and genotyped as described previously [10]. S1P2−/− mice were backcrossed with C57BL/6N (Clea Japan, Tokyo, Japan) for seven generations, and thus, littermate wild-type (WT) mice or age-matched (8-week-old) C57BL/6N were used as controls. All mice were fed ad libitum with standard chow/water and kept under a 12-hour light-dark cycle in an air-conditioned room. All animal protocols were approved by the animal care and use committee of Chiba-East National Hospital.
Induction of diabetes by STZ injection
Streptozotocin (STZ, Sigma) was freshly dissolved in 20 mM citrate buffer (pH4.5) and intraperitoneally administered under various conditions in each experiment: 50 mg/kg body weight for 5 consecutive days (50 mg/kg for 5 days), 100 mg/kg for 1 day, or 100 mg/kg for 2 days. Control mice received injections of the citrate buffer. JTE-013 (Calbiochem), a specific S1P2 antagonist [11], was freshly dissolved in saline and intraperitoneally administered at 4 mg/kg for 6 days (one shot prior to STZ and five shots with STZ). Control mice received injections of saline. Blood was collected from the retro-orbital sinus of anesthetized mice and blood glucose levels were measured using the Accu-Chek Aviva system (Roche). Mice were diagnosed with diabetes mellitus (DM) when their blood glucose levels were ≥ 300 mg/dl on two consecutive days [12]. Serum insulin levels were measured using an insulin RIA kit (Millipore) in accordance with the manufacturer’s instructions.
Immunohistochemistry
Pancreata were quickly removed from anesthetized mice, fixed with 3% formalin in phosphate-buffered saline, and embedded in paraffin. To count islet cells, deparaffinized pancreatic sections were immunostained with guinea pig polyclonal anti-insulin antibody (Cell Marque, Rocklin, CA) using a NexES IHC system (Ventana Medical Systems, Tucson, AZ). Full area sizes (mm2) of pancreatic sections (single section per mouse) were measured and the numbers of insulin-positive islets in each section were counted. Apoptotic cells were detected using a terminal deoxynucleotidyl transferase-mediated dUTP nick-end labeling (TUNEL) assay (Apotag Kit; Chemicon) in accordance with the manufacturer’s recommendations. Apoptotic cells per nm2 of islet area were counted in ≥ 10 islets per section.
Statistical analysis
Results are expressed as mean ± SD. All statistical analyses were performed using Dr. SPSS II for Windows (SPSS Inc., Chicago, IL). The existence of significant differences between two groups (with an accuracy of at least 95%) was analyzed using a two-tailed unpaired t-test. Kaplan-Meier analysis was used to examine diabetes-free rates and survival rates, and the differences were determined by log-rank tests. A value of P < 0.05 was considered significant.
Results
S1P2−/− mice were more resistant to administration of a high dose of STZ
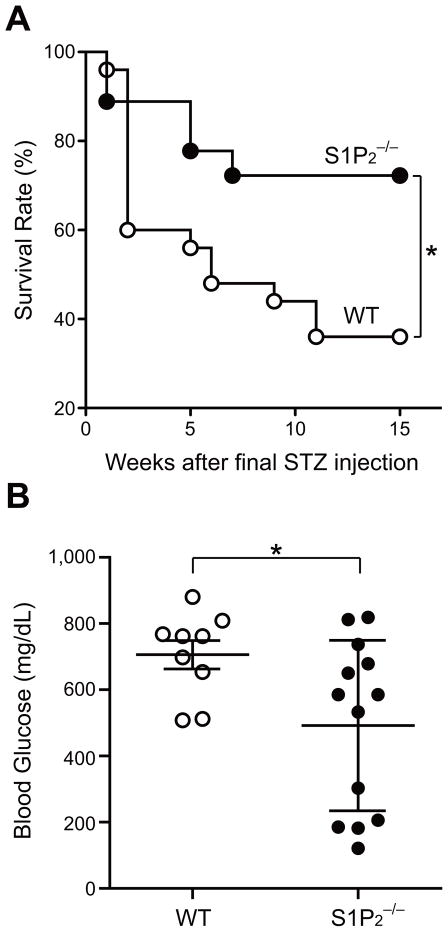
WT and S1P2−/− males were intraperitoneally injected with a high dose of STZ (100 mg/kg for 2 days), and their health status was monitored every week until the 15th week after the final injection. Forty percent (10/25) of WT mice died at the 2nd week, increasing to 64.0% (16/25) by the 11th week. In contrast, S1P2−/− mice show lower death rates of 11.1% (2/18) and 27.7% (5/18), respectively. Kaplan–Meier analysis indicates that S1P2−/− mice were significantly (P = 0.0334) more resistant to STZ toxicity than WT mice (Fig. 1A). At the 15th week after the final injection, serum glucose levels in surviving S1P2−/− mice were significantly lower than those in surviving WT mice (Fig. 1B).
Fig. 1.
S1P2−/− mice were more resistant to administration of a high dose of STZ. (A) Kaplan-Meier survival analysis of WT and S1P2−/− mice (n = 25 and 18, respectively) after the final injection of a high dose of STZ (100 mg/kg for 2 days). (B) Blood glucose levels of randomly fed, surviving WT and S1P2−/− mice at the 15th week after the final STZ injection (n = 9 and 13, respectively). The differences were significant (*P < 0.05).
More β-cells were preserved after STZ injection in S1P2−/− mice
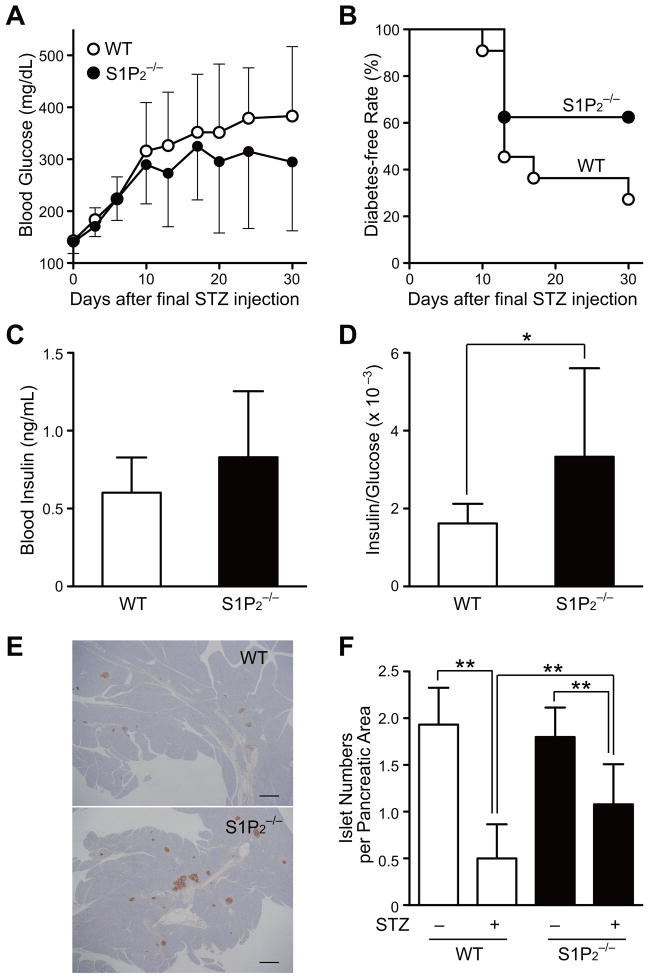
WT and S1P2−/− males were injected with a low dose of STZ (50 mg/kg for 5 days) so that all mice survived until at least the 30th day after the final injection, and blood glucose levels were measured twice a week. There was no significant difference in glucose levels between WT and S1P2−/− mice (Fig. 2A). Eight of eleven (72.7%) WT mice were diagnosed with diabetes compared with only three of eight (37.5%) S1P2−/− mice; however, Kaplan-Meier analysis revealed no significant difference in diabetes-free rates between the two groups (Fig. 2B). Although blood insulin levels in S1P2−/− mice were comparable to those in WT mice at the 30th day after the final STZ injection (Fig. 2C), the insulin/glucose ratios (an index of relative insulin deficiency [13]) were significantly higher in S1P2−/− mice than in WT mice (Fig. 2D). This indicates that insulin was more efficiently secreted in response to blood glucose elevation in S1P2−/− mice than in WT mice. We counted the numbers of insulin-positive islets per pancreatic area at the 30th day after STZ injection. Insulin-positive islets were much more abundant in pancreatic sections from S1P2−/− mice (Fig. 2E). The numbers of insulin-positive islets per pancreatic area in S1P2−/− mice were comparable to those in WT mice without STZ, because more islet cells (per pancreatic area) withstood STZ-induced cytotoxicity in S1P2−/− mice (Fig. 2F). Taken together, these findings indicate that more islet β-cells were preserved after STZ injection in S1P2−/− mice than in WT mice.
Fig. 2.
More β-cells were preserved after STZ injection in S1P2−/− mice. WT and S1P2−/− mice (n = 11 and 8, respectively) were administered a low dose of STZ (50 mg/kg for 5 consecutive days intraperitoneally). (A) Blood glucose levels in randomly fed WT and S1P2−/− mice after STZ injection. (B) Kaplan-Meier analysis of diabetes-free rates after STZ injection. (C) Serum insulin levels (ng/ml) at the 30th day after the final STZ injection. (D) Blood insulin/glucose ratios (× 10−3) as an index of relative insulin deficiency at the 30th day after the last STZ injection. (E) Representative images of insulin-positive islets in pancreas at the 30th day after the final STZ injection. Bars: 200 μm. (F) Numbers of insulin-positive islets per pancreatic area (mm2) without (n = 5 each for WT and S1P2−/− mice) or with STZ injection (at the 30th day after the final STZ injection). *P < 0.05 and **P < 0.01.
More islet cells were protected against STZ-induced apoptosis in S1P2−/− mice
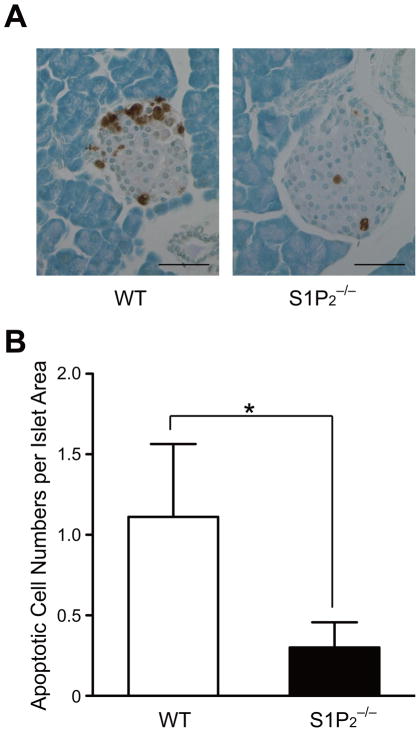
The administration of STZ is known to induce apoptosis of islet β-cells [13,14]. WT and S1P2−/− males were intraperitoneally injected with a high dose of STZ (100 mg/kg for 1 day), and apoptosis of islet cells was evaluated the following day. Histological analysis revealed that TUNEL-positive apoptotic islet cells were less abundant in S1P2−/− mice than in WT mice (Fig. 3A). The number of apoptotic cells per nm2 of islet area in S1P2−/− mice was 27% of that in WT mice (Fig. 3B), indicating that the lack of S1P2 protects islet cells from STZ-induced apoptosis.
Fig. 3.
More islet cells were protected against STZ-induced apoptosis in S1P2−/− mice. Mice were injected with a high dose of STZ (100 mg/kg for 1 day) and apoptotic β-cells were identified by immunostaining (A) TUNEL-positive apoptotic β-cells in pancreatic sections obtained from WT and S1P2−/− mice. Bars: 50 μm. (B) Numbers of apoptotic cells per islet area (nm2) of WT and S1P2−/− mice (n = 10 each). The difference is significant (*P < 0.0001).
JTE-013 decreased the incidence of diabetes
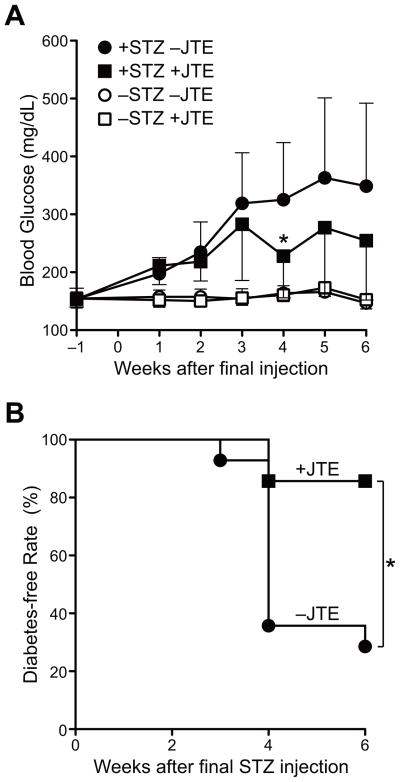
We examined the effect of JTE-013, a specific S1P2 antagonist, on the incidence of STZ-induced diabetes. JTE-013 (4 mg/kg) was intraperitoneally injected for 6 days (one shot prior to STZ and five shots with STZ (50 mg/kg)), and blood glucose elevation after the final STZ injection was examined every week. Glucose levels at the 4th week after the final STZ injection were significantly lower in JTE-013-treated mice than JTE-013-untreated mice (Fig. 4A). Glucose levels were not indistinguishable between JTE-013-treated and JTE-013-untreated mice in the absence of STZ. Among STZ-injected mice, 71.4% (10/14) of JTE-013-untreated mice were found to be diabetic compared with only 14.3% (2/14) of JTE-013-treated mice by the 6th week after the final STZ injection. Kaplan-Meier analysis indicates that JTE-013 treatment significantly (P = 0.0024) decreased the incidence of diabetes (Fig. 4B).
Fig. 4.
JTE-013 decreased the incidence of diabetes. JTE-013 (4 mg/kg) or saline was intraperitoneally injected for 6 days (one shot prior to STZ and five shots with a high dose of STZ (50 mg/kg)). (A) Changes in blood glucose levels of randomly fed mice with/without STZ or JTE-013 injection. Sample numbers are 14 for +STZ/−JTE-013 (closed circles), +STZ/+JTE-013 (closed squares), −STZ/−JTE-013 (open circles), and −STZ/+JTE-013 (open squares). The effects of JTE-013 were significant at the 4th weeks after the final STZ injection (*P < 0.01). (B) Kaplan-Meier analysis of diabetes-free rates after STZ injection. Co-injection with JTE-013 significantly reduced the diabetes-free rates (*P < 0.01).
Discussion
We found that the blockade of S1P2 signaling prevents the onset of diabetes by protecting islet β-cells from STZ-induced injury (Fig. 2 and 3). S1P2 is known to couple with Gq, activate phospholipase C that leads to Ca2+ mobilization, and induce the activation of extracellular-regulated kinase, stress-activated protein kinase/c-jun N-terminal kinase, and mitogen-activated protein kinase (MAPK) p38 [15,16]. The activation of MAPK p38 is a critical event leading to β-cell apoptosis and promoting peripheral insulin resistance [17,18,19], and thus mice lacking MAPK p38 were found to be protected against pancreatic β-cell failure and insulin resistance [14]. Therefore, blockade of S1P2 signaling may lead to deactivation of MAPK p38 and attenuation of STZ-induced β-cell failure/progression of diabetes. The present study bears analogy to our previous one, in which accelerated regeneration of hepatocytes was observed after liver injury in S1P2−/− mice [20], and may suggest generalization of cell protective effect by S1P2 inactivation. Recently, it has been suggested that S1P2 may protect against diabetes by preventing insulin resistance; S1P2−/− mice showed insulin resistance [9] and S1P2 signaling increased glucose uptake in myoblasts [8]. Although further studies are necessary to solve this inconsistency with our findings, the protective effect on pancreatic β-cells resulting from S1P2 inactivation may have surpassed the undesired insulin resistance in our system.
We further explored the possibility that the S1P2-specific antagonists have potential for use in the treatment of diabetes. JTE-013 decreased blood glucose levels (Fig. 4A) and reduced the incidence of diabetes in STZ-injected mice (Fig. 4B). It has been shown that FTY720, a pro-drug against all the S1P receptors except S1P2 (i.e., S1P1 and S1P3–5), reduces the incidence of diabetes in mice [21]. These results suggest that the protective effects of S1P against diabetes (including blockade of immune cell migration) may be mediated by non-S1P2-type S1P receptors. In this context, selective inactivation of pro-diabetic S1P2 and preservation of anti-diabetic non-S1P2-type S1P receptors by S1P2-specific antagonists may have strong potential as a future anti-diabetic strategy; the ligand S1P is abundant in the blood stream [22].
Conclusion
We report here that selective blockade of S1P2 signaling attenuates STZ-induced apoptosis of pancreatic β-cells and decreases the incidence of diabetes in mice. Modulation of S1P signaling may provide a new avenue for the treatment of diabetes.
Acknowledgments
We thank Ms. Mori Tachibana and Ms. Akiko Miyashita for technical support. This work was supported by research grants from the Policy-based Medical Service Network for the National Hospitals of Japan (to T.I.), the Takeda Science Foundation (to I.I.), and the National Institutes of Health (DA019674 and NS048478 to J.C.).
Abbreviations
- MAPK
mitogen-activated protein kinase
- S1P
sphingosine 1-phosphate
- S1P2
sphingosine 1-phosphate receptor 2
- STZ
Streptozotocin
- TUNEL
terminal deoxynucleotidyl transferase-mediated dUTP nick-end labeling
- WT
wild-type
References
- 1.Muoio DM, Newgard CB. Mechanisms of disease: molecular and metabolic mechanisms of insulin resistance and beta-cell failure in type 2 diabetes. Nat Rev Mol Cell Biol. 2008;9:193–205. doi: 10.1038/nrm2327. [DOI] [PubMed] [Google Scholar]
- 2.Zhang B, Lu Y, Campbell-Thompson M, Spencer T, Wasserfall C, Atkinson M, Song S. Alpha1-antitrypsin protects beta-cells from apoptosis. Diabetes. 2007;56:1316–1323. doi: 10.2337/db06-1273. [DOI] [PubMed] [Google Scholar]
- 3.Ishii I, Fukushima N, Ye X, Chun J. Lysophospholipid receptors: signaling and biology. Annu Rev Biochem. 2004;73:321–354. doi: 10.1146/annurev.biochem.73.011303.073731. [DOI] [PubMed] [Google Scholar]
- 4.Takabe K, Paugh SW, Milstien S, Spiegel S. “Inside-out” signaling of sphingosine-1-phosphate: therapeutic targets. Pharmacol Rev. 2008;60:181–195. doi: 10.1124/pr.107.07113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Laychock SG, Sessanna SM, Lin MH, Mastrandrea LD. Sphingosine 1-phosphate affects cytokine-induced apoptosis in rat pancreatic islet beta-cells. Endocrinology. 2006;147:4705–4712. doi: 10.1210/en.2006-0456. [DOI] [PubMed] [Google Scholar]
- 6.Rutti S, Ehses JA, Sibler RA, Prazak R, Rohrer L, Georgopoulos S, Meier DT, Niclauss N, Berney T, Donath MY, von Eckardstein A. Low- and high-density lipoproteins modulate function, apoptosis, and proliferation of primary human and murine pancreatic beta-cells. Endocrinology. 2009;150:4521–4530. doi: 10.1210/en.2009-0252. [DOI] [PubMed] [Google Scholar]
- 7.Laychock SG, Tian Y, Sessanna SM. Endothelial differentiation gene receptors in pancreatic islets and INS-1 cells. Diabetes. 2003;52:1986–1993. doi: 10.2337/diabetes.52.8.1986. [DOI] [PubMed] [Google Scholar]
- 8.Rapizzi E, Taddei ML, Fiaschi T, Donati C, Bruni P, Chiarugi P. Sphingosine 1-phosphate increases glucose uptake through trans-activation of insulin receptor. Cell Mol Life Sci. 2009;66:3207–3218. doi: 10.1007/s00018-009-0106-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tu Z, Argmann C, Wong KK, Mitnaul LJ, Edwards S, Sach IC, Zhu J, Schadt EE. Integrating siRNA and protein-protein interaction data to identify an expanded insulin signaling network. Genome Res. 2009;19:1057–1067. doi: 10.1101/gr.087890.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ishii I, Ye X, Friedman B, Kawamura S, Contos JJ, Kingsbury MA, Yang AH, Zhang G, Brown JH, Chun J. Marked perinatal lethality and cellular signaling deficits in mice null for the two sphingosine 1-phosphate (S1P) receptors, S1P(2)/LP(B2)/EDG-5 and S1P(3)/LP(B3)/EDG-3. J Biol Chem. 2002;277:25152–25159. doi: 10.1074/jbc.M200137200. [DOI] [PubMed] [Google Scholar]
- 11.Ohmori T, Yatomi Y, Osada M, Kazama F, Takafuta T, Ikeda H, Ozaki Y. Sphingosine 1-phosphate induces contraction of coronary artery smooth muscle cells via S1P2. Cardiovasc Res. 2003;58:170–177. doi: 10.1016/s0008-6363(03)00260-8. [DOI] [PubMed] [Google Scholar]
- 12.Matarese G, Sanna V, Lechler RI, Sarvetnick N, Fontana S, Zappacosta S, La Cava A. Leptin accelerates autoimmune diabetes in female NOD mice. Diabetes. 2002;51:1356–1361. doi: 10.2337/diabetes.51.5.1356. [DOI] [PubMed] [Google Scholar]
- 13.Le May C, Chu K, Hu M, Ortega CS, Simpson ER, Korach KS, Tsai MJ, Mauvais-Jarvis F. Estrogens protect pancreatic beta-cells from apoptosis and prevent insulin-deficient diabetes mellitus in mice. Proc Natl Acad Sci USA. 2006;103:9232–9237. doi: 10.1073/pnas.0602956103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sumara G, Formentini I, Collins S, Sumara I, Windak R, Bodenmiller B, Ramracheya R, Caille D, Jiang H, Platt KA, Meda P, Aebersold R, Rorsman P, Ricci R. Regulation of PKD by the MAPK p38delta in insulin secretion and glucose homeostasis. Cell. 2009;136:235–248. doi: 10.1016/j.cell.2008.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ancellin N, Hla T. Differential pharmacological properties and signal transduction of the sphingosine 1-phosphate receptors EDG-1, EDG-3, and EDG-5. J Biol Chem. 1999;274:18997–19002. doi: 10.1074/jbc.274.27.18997. [DOI] [PubMed] [Google Scholar]
- 16.Gonda K, Okamoto H, Takuwa N, Yatomi Y, Okazaki H, Sakurai T, Kimura S, Sillard R, Harii K, Takuwa Y. The novel sphingosine 1-phosphate receptor AGR16 is coupled via pertussis toxin-sensitive and -insensitive G-proteins to multiple signalling pathways. Biochem J. 1999;337:67–75. [PMC free article] [PubMed] [Google Scholar]
- 17.Hirosumi J, Tuncman G, Chang L, Gorgun CZ, Uysal KT, Maeda K, Karin M, Hotamisligil GS. A central role for JNK in obesity and insulin resistance. Nature. 2002;420:333–336. doi: 10.1038/nature01137. [DOI] [PubMed] [Google Scholar]
- 18.Kaneto H, Nakatani Y, Miyatsuka T, Kawamori D, Matsuoka TA, Matsuhisa M, Kajimoto Y, Ichijo H, Yamasaki Y, Hori M. Possible novel therapy for diabetes with cell-permeable JNK-inhibitory peptide. Nat Med. 2004;10:1128–1132. doi: 10.1038/nm1111. [DOI] [PubMed] [Google Scholar]
- 19.Makeeva N, Myers JW, Welsh N. Role of MKK3 and p38 MAPK in cytokine-induced death of insulin-producing cells. Biochem J. 2006;393:129–139. doi: 10.1042/BJ20050814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ikeda H, Watanabe N, Ishii I, Shimosawa T, Kume Y, Tomiya T, Inoue Y, Nishikawa T, Ohtomo N, Tanoue Y, Iitsuka S, Fujita R, Omata M, Chun J, Yatomi Y. Sphingosine 1-phosphate regulates regeneration and fibrosis after liver injury via sphingosine 1-phosphate receptor 2. J Lipid Res. 2009;50:556–564. doi: 10.1194/jlr.M800496-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maki T, Gottschalk R, Ogawa N, Monaco AP. Prevention and cure of autoimmune diabetes in nonobese diabetic mice by continuous administration of FTY720. Transplantation. 2005;79:1051–1055. doi: 10.1097/01.tp.0000161220.87548.ee. [DOI] [PubMed] [Google Scholar]
- 22.Yatomi Y, Igarashi Y, Yang L, Hisano N, Qi R, Asazuma N, Satoh K, Ozaki Y, Kume S. Sphingosine 1-phosphate, a bioactive sphingolipid abundantly stored in platelets, is a normal constituent of human plasma and serum. J Biochem. 1997;121:969–973. doi: 10.1093/oxfordjournals.jbchem.a021681. [DOI] [PubMed] [Google Scholar]