Abstract
Central Giant Cell Granulomas (CGCG) of the jaw are uncommon benign lesions which usually occur in the mandible in young adults. Here we present a case report of a 45-year-old woman who presented with a 5-month history of right nasal obstruction secondary to a large maxillary CGCG. The age, symptoms at presentation, location and radiographic features were not pathognomonic for this lesion. This case helps to demonstrate the wide variation in the clinical, radiological and histopathological features of CGCC and provides an update in current treatment concepts.
INTRODUCTION
The World Health Organisation (2005) define a central giant cell granuloma as a benign intraosseous lesion consisting of fibrous tissue containing foci of haemorrhage and haemosiderin deposits, aggregations of giant cells and reactive bone formation. (1) Although they represent benign pathology they can be subdivided into locally aggressive and non-aggressive types based on clinical, radiological and histopathological features (2,3). They are uncommon lesion with a published incidence of 1.1 per 106 and they usually occur in older children and young adults. (4) Their aetiology remains unclear but they appear to have a slight predilection for females (3,5)
Radiographically, CGCG may appear as a unilocular or multilocular radiolucency, the latter exhibiting internal bony septa (4,5,6). A positive correlation between the size of the lesion and multilocularity has been found (5). The degree of cortication of the margins dictate the definition of its borders radiographically and tooth displacement and root resorption are features of aggressive lesions. (3,6) CT imaging aids surgical treatment planning by demonstrating the extent of the lesion, cortical expansion and bony destruction (7).
CASE REPORT
A 45-year-old woman presented with five months history of nasal obstruction. She was a vegetarian with limited sunshine exposure.
On clinical examination she was found to have complete nasal obstruction on the right side and bulging of the lateral nasal wall was noted. Intra-oral examination revealed buccal expansion of the upper right alveolar bone. A CT scan revealed a large right maxillary antral mass, with areas of radiolucency and radiopacity, extending into the right nasal cavity and ethmoidal air cells (Fig. 1). It appeared to contain flecks of calcification and was closely related to the maxillary molar teeth, however, root resorption and displacement of teeth were not features. A benign odontogenic tumour of the jaw was suspected.
Fig. 1.
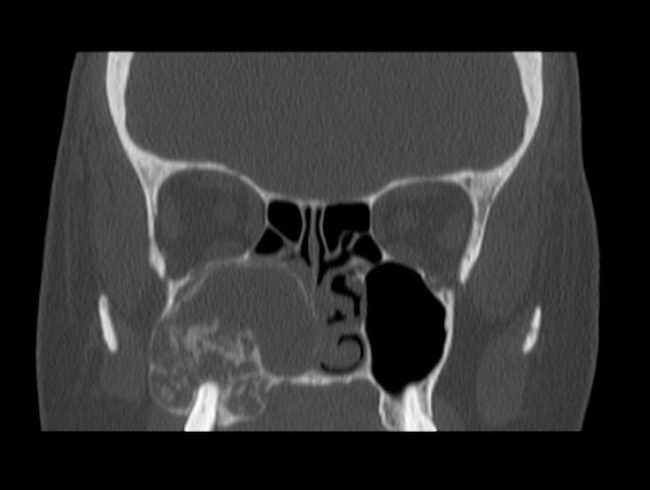
CT Scan revealing a large right maxillary antral mass
An incisional biopsy revealed trabeculae of lamellar and woven bone within a cellular, but cytologically bland fibrous stroma histologically. The bone trabeculae were lined for the most part by a rim of osteoblasts with a zone of osteoid production noted. The stroma contained osteoclast like giant cells, which showed a limited tendency to aggregate around foci of haemorrhage. These features are those of a fibro-osseous lesion with giant cells and were thought to be most in keeping with a central giant cell lesion, either a granuloma or a Brown tumour of hyperparathyroidism.
This led to investigations of hyperparathyroidism with blood tests, including, vitamin D, Calcium, parathyroid hormone level (PTH) and an assessment of renal function. These suggested a picture of vitamin D deficiency (10 nmol/L reference range 75-200 nmol/L) with parathyroid hormone levels, which were only mildly raised (9.5pmol/L reference range of 1.1-6.9 pmol/L). A specialist endocrinology opinion was that this was a picture of simple vitamin D deficiency, unrelated to the lesion in the maxilla, as the results of the parathyroid immunoassay were not considered deranged enough to be consistent with a Brown tumour. Colecalciferol 20,000 IU weekly for 3-6 months was advised followed by further monitoring of blood tests in 3 months to ensure a response.
A decision was made to resect the lesion by surgical curettage. This was carried out via an intra-oral approach under general anaesthetic. A large window of buccal bone was removed with a burr and the tumour was exposed in part. It was noted to vary in consistency from bony hard areas to soft tissue components. Resection was carried out in a piecemeal fashion, with osteotomes and curettage. The tumour filled the antrum and breached the nasal mucosa medially, however the orbital floor was intact. Primary closure was achieved. Post-operative histopathological diagnosis confirmed a lesion composed of numerous anastomosing bony trabeculae between which were islands of fibrous tissue with giant cells and osteoid formation. The appearance was that of a giant cell lesion.
The patient recovered well post operatively and was discharged the following day. She remains under close observation and is well 12 months following the procedure.
DISCUSSION
According to the literature, CGCG is most commonly seen in the first three decades of life, and occurs at least twice as often in the mandible as in the maxilla (4,7). CGCG in the maxilla is likely to present with asymptomatic facial swelling as the cortical bone here is thin and provides little resistance to growth (7). This case did not fit with the characteristic presentation of CGCG. It occurred in the maxilla of a 45-year-old woman; radiological features were not characteristic and there was no evidence of extra-oral facial asymmetry although the lesion was large at presentation.
Surgical curettage remains the most common treatment modality in CGCG. However, recurrence rates of up to 24% have been reported for non-aggressive lesions (3). This has lead to trial of other treatment modalities such as the use of corticosteroids or calcitonin with variable results. This variability may be due to differences in glucocorticoid and calcitonin receptor expression between lesions and this is an area of current research (8). Agents such as interferon and imatinib have also been used in the treatment of aggressive lesions in combination with surgical curettage (9). If recurrence is a problem in this case, treatment with these agents could be considered, however there is little evidence available as yet to support their use (3). A more aggressive surgical resection was not chosen in this case as the current evidence suggests that recurrence is not associated with serious consequences and so the potential loss of form and function associated with en bloc resection is not justified (7).
REFERENCES
- 1.Barnes L, Eveson JW, Reichart P, Sidransky D. World Health Organisation Classification of Tumours. Pathology and Genetics of Head and Neck Tumours. IARC Press; Lyon, France: 2005, Chapter 6, p. 324 [Google Scholar]
- 2.Chuong Kaban, et al. Central giant cell lesions of the jaws: a clinicopathologic study. J Oral Maxillofacial Surg 1986; 44:708–713 [DOI] [PubMed] [Google Scholar]
- 3.De Lange J, Van den Akker HP, Van den Berg H. Central giant cell granuloma of the jaw: a review of the literature with emphasis on therapy options. Oral Surg Oral Med Oral Radiol & Endo 2007; 104:603–615 [DOI] [PubMed] [Google Scholar]
- 4.De Lange J, Van den Akker HP. Clinical and radiological features of central giant-cell lesions of the jaw. Oral surg Oral med Oral path Oral rad Endod 2005; 99:464–470 [DOI] [PubMed] [Google Scholar]
- 5.Kaffe I, Ardekian L, Taicher S, Littner MM, Buchner A. Radiologic features of central giant cell granuloma of the jaws. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1996; 81:720–726 [DOI] [PubMed] [Google Scholar]
- 6.Kruse-Losler B, Diallo R, Gaertner C, Mischke KL, Joos U, Kleinheinz J. Central giant cell granuloma of the jaws: a clinical radiologic and histopathologic study of 26 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006; 101:346–354 [DOI] [PubMed] [Google Scholar]
- 7.Rawashdeh MA, Bataineh AB, Al-Khateeb T. Long-term clinical and radiological outcomes of surgical management of central giant cell granuloma of the maxilla. Int J Oral Maxillofac Surg. 2006; 35:60–66 [DOI] [PubMed] [Google Scholar]
- 8.Nogueira RLM, Faria MHG, Osterne RLV, Cavalcante RB, Ribeiro RA, Rabenhorst SHB. Glucocorticoid and calcitonin receptor expression in central giant cell lesions: implications for therapy. Int. J. Oral Maxillofac Surg. 2012. Available online (doi: 10.1016/j.ijom.2012.01.017) [DOI] [PubMed] [Google Scholar]
- 9.De Lange J, Van Rijn RR, Van den Berg H, Van den Akker HP. Regression of central giant cell granuloma by a combination of imatinib and interferon: a case report. BJOMS. 2009; 47:59–61 [DOI] [PubMed] [Google Scholar]


