Abstract
Introduction:
The increasing availability of robotic devices has led to an increase in their use for procedures such as pyeloplasty, which have been conventionally performed laparoscopically or through open surgery. We perform both laparoscopic and robotic-assisted pyeloplasty routinely and have compared these techniques in a set of concurrent cohorts, operated by the same surgeon.
Materials and Methods:
A chart review was performed of all cases of Robot-assisted laparoscopic pyeloplasty (RALP) and conventional laparoscopic pyeloplasty (CLP) performed by a single surgeon, from September 2006 to July 2010. The choice of procedure depended upon the availability of the robot on the given day. A lateral transperitoneal approach was used in all cases. All anastomoses were stented antegrade. A diuretic renogram was obtained in all patients between six to twelve weeks after stent removal. Success was defined as a resolution of symptoms with non-obstructive outflow on the renogram.
Results:
Thirty patients underwent 31 laparoscopic pyeloplasties (20 RALPs and 11 CLPs), with one patient undergoing bilateral simultaneous robotic procedures. The robotic procedures were superior in terms of shorter operating time by 20 minutes on an average. Furthermore, 35% of the robotic procedures were performed in under 90 minutes, while the minimum time taken for laparoscopy was 110 minutes. All procedures in both cohorts were successful with no complications in either group. The surgeon recorded subjective ergonomic benefits with the use of the robot.
Conclusions:
Robotic assistance helps decrease the operative time for laparoscopic pyeloplasty. It seems ergonomically superior for the surgeon, allowing multiple procedures in the same list. These may be important benefits in busy centers.
Keywords: Laparoscopy, pyeloplasty, robot, Ureteropelvic junction obstruction
INTRODUCTION
Laparoscopic repair of ureteropelvic junction obstruction (UPJO) has become a standard-of-care technique in both children and adults.[1] The increasing availability of surgical robots in large hospitals has resulted in an increase in the number of procedures that are being performed with robotic assistance. Pyeloplasty is one such procedure. However, this widening of indications is often accompanied by doubts about the true benefit of robotic assistance for procedures where laparoscopy potentially provides the same results.[2] Once a robot is available, there is a tendency to use robotic assistance rather than perform conventional laparoscopy, and most data comparing the outcomes of laparoscopy and robotics is non-concurrent or multiple surgeon series. We acquired a four-arm da Vinci S surgical system in August 2006, and have been routinely using it for procedures that we originally performed laparoscopically or through open approaches. However, logistic constraints often result in our resorting to conventional laparoscopy, allowing us the opportunity to compare a concurrent cohort of patients undergoing the same surgery by the same surgeon. Dismembered pyeloplasty for UPJO is the most common surgery where we use conventional laparoscopy (CLP) and robotic assistance (RALP) with almost equal frequency. We report our comparative outcomes with these procedures and also look at certain ‘unmeasured’ parameters, which may help determine the relative indications of the two approaches.
MATERIALS AND METHODS
A chart review was performed of all cases of RALP and CLP performed by a single surgeon from September 2006 to July 2010. All procedures were performed within the same time period and the surgeon had experience of less than 10 CLPs prior to this period. Pyeloplasty was performed for standard indications. The decision to perform RALP or CLP was based on the availability of the robot on the day the patient was scheduled for surgery. A lateral transperitoneal approach was used in all cases. For RALP, three arms of the four-arm da Vinci S surgical system were used with one additional 12 mm port for the assistant. For CLPs, a three port technique was used in all cases. An additional 5mm port was used for liver retraction in right-sided procedures. Our robotic technique of RALP has been previously described.[3,4] All anastomoses in both sets of cases were performed with 5-0 polyglactin sutures. An antegrade ureteric stent was also placed in all patients. A peri-renal drain placed at the end of the procedure was removed when the 24-hour output was less than 50 mL. Urethral catheters were removed the following day. A diuretic renogram was obtained between six and twelve weeks after stent removal. Success was defined as the resolution of symptoms with non-obstructive outflow on the renogram. All patients provided informed consent for the surgeries.
RESULTS
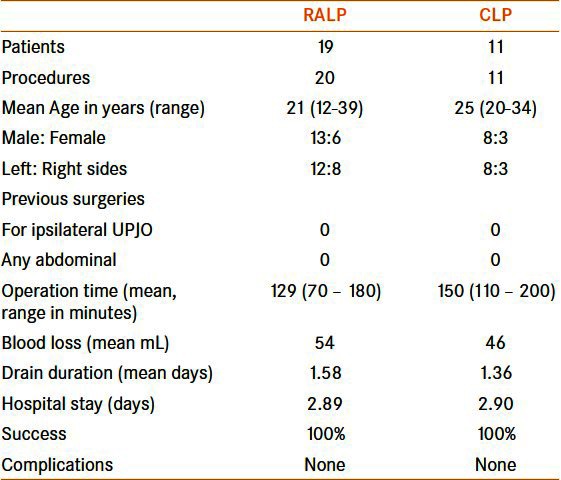
In the period under review, 30 patients underwent 31 laparoscopic pyeloplasties (RALP: 19 patients — 20 sides; CLP: 11). One patient in the robotic group underwent bilateral simultaneous procedures, which has been previously reported.[5] Patient and operative data are given in Table 1. The two groups were comparable in all baseline parameters. The operating time (including docking time) for robotic procedures was shorter by an average of 20 minutes. This was not statistically significant. However, while 35% of the robotic procedures were performed in under 90 minutes, the minimum time taken for laparoscopy was 110 minutes, with most (90%) being over 120 minutes. There were no complications in either group and the procedures were successful in all patients at the first follow-up scan.
Table 1.
Comparative data
On days when the robot was available, often two pyeloplasties were performed in one list. However, on no occasion were two CLPs performed on the same day. Although it was not measured objectively, the principal reason for this was surgeon fatigue after the CLP.
DISCUSSION
Laparoscopy is one of the most significant advances of the twenty-first century surgical armamentarium, allowing significantly better cosmesis, lower pain, blood loss, and convalescence, with no loss of functional or oncological outcomes. One of the major issues with laparoscopy was the steep learning curve, partly due to the two-dimensional vision and limited movement of instruments. This was particularly evident in reconstructive procedures, which, in urology, consisted mainly of vesicourethral anastomosis and pyeloplasty. This led to these procedures being classified as ‘advanced’ and were performed by relatively few very skilled surgeons.[6]
Robotic assistance available to urology from the early 2000s, helped overcome these major limitations. The initial reports of robotic radical prostatectomy clearly stated the benefit laparoscopy naïve surgeons derived from robotic assistance, enabling a wider availability of minimally invasive procedures.[7,8] Once robotic devices became widely available, they began to be used for an increasing number of procedures, which were hitherto routinely performed with conventional laparoscopy, with excellent outcomes. The high costs associated with the robot dampened the enthusiasm for its routine use, particularly when laparoscopy allowed similar outcomes.
The data on RALP versus CLP has generally been conflicting. A recent meta-analysis by Braga et al., found only eight published articles, where RALP and CLP were directly compared.[3] They found the operating time in RALP to be shorter by about 10 minutes and the hospital stay to be shorter by about half-a-day. Compilations and success rates were similar in both groups. Our findings were somewhat similar to this report. Our operating times were 20 minutes shorter on an average, while all other parameters were similar. An interesting finding in our data was that a larger number of robotic procedures tended to be of short duration compared to pure laparoscopic ones. This would suggest a minimum time required in CLP that was difficult to further shorten.
Surgical experience is probably the most important factor in determining the outcomes. Among the eight series reviewed by Braga et al., the maximal operating time advantage for robotic assistance was seen in a series where the surgeons had relatively lower laparoscopy experience.[9] The impact of the learning curve on the outcomes of laparoscopic pyeloplasty has been well-established.[10] It is evident that for surgeons who perform few CLPs or are in the early part of their laparoscopy career, robotic assistance may provide advantages.
The strength of our study lies in the fact that it is a single surgeon evaluation of a concurrent cohort, minimizing the impact of the learning curve. This is different from most other single surgeon series where the comparison is non-concurrent.[11–14] Among these comparative studies, Bernie et al.[12] reported one very similar to ours. They compared the outcomes of the first seven cases, each of laparoscopic and robotic pyeloplasties by the same surgeon and found no difference between the two procedures. However, the series were not concurrent. The CLPs were performed before embarking on robotic procedures and the experience was thus not comparable. Another single surgeon comparative report by Link et al.,[13] however, found results contrary to most other series. They noted significantly longer operating times for RALP in comparison with CLP. Again, this series was not concurrent and the RALPs reported were performed before the CLPs. Their results were particularly surprising, as the authors had significant experience in both procedures and should not have been hampered by any learning curve.
A significant, unmeasured, parameter noted in our series was of surgeon fatigue. Despite only marginally higher operative times, fatigue at the end of a well-performed conventional laparoscopic pyeloplasty discouraged the performance of a second procedure the same day. Increasing fatigue results in increased tremor and placing precise sutures can be difficult when the surgeon is tired.[15] This became evident to us when we realized that we were routinely performing more than one reconstructive procedure, pyeloplasty or radical prostatectomy, when robotic assistance was available, while on no day were two CLPs performed. Surgeon fatigue has been a poorly studied phenomenon. Although it has been previously documented that laparoscopy is associated with increased risk of injuries to the surgeon, a comparison of the ergonomic outcomes between robotics and laparoscopy for the surgeon would be worth performing.[16]
Finally, as with previously published studies, we found no significant difference in the outcomes between RALP and conventional pyeloplasty. We believe that this is only to be expected. Ultimately, robotic assistance simply refines laparoscopy and does not change the basic surgical approach. There is thus unlikely to be any significant improvement in the outcomes, which are already very good. However, potential benefits to surgeons and busy hospitals would accrue from even marginal decrease in operating time and reduction in surgeon fatigue. Both of these have the potential to contribute to a decrease in the overall cost of the procedure and increase its acceptability.
CONCLUSIONS
Robotic assistance helps decrease the operative time for laparoscopic pyeloplasty. It seems ergonomically superior for the surgeon, allowing multiple procedures in the same list. These may be important benefits in busy centers.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Winfield HN. Management of adult ureteropelvic junction obstruction-is it time for a new gold standard? J Urol. 2006;176:866–7. doi: 10.1016/j.juro.2006.06.094. [DOI] [PubMed] [Google Scholar]
- 2.Rassweiler J, Pini G, Gözen AS, Klein J, Teber D. Role of laparoscopy in reconstructive surgery. Curr Opin Urol. 2010;20:471–82. doi: 10.1097/MOU.0b013e32833f21bd. [DOI] [PubMed] [Google Scholar]
- 3.Gupta NP, Mukherjee S, Nayyar R, Hemal AK, Kumar R. Transmesocolic robotic pyeloplasty: Single center experience. J Endourol. 2009;23:945–8. doi: 10.1089/end.2008.0430. [DOI] [PubMed] [Google Scholar]
- 4.Gupta NP, Nayyar R, Hemal AK, Mukherjee S, Kumar R, Dogra PN. Outcome analysis of robotic pyeloplasty: A large single-centre experience. BJU Int. 2010;105:980–3. doi: 10.1111/j.1464-410X.2009.08983.x. [DOI] [PubMed] [Google Scholar]
- 5.Kumar R, Yadav R, Kolla SB. Case report: Simultaneous bilateral robot-assisted dismembered pyeloplasties for bilateral ureteropelvic junction obstruction: Technique and literature review. J Endourol. 2007;21:750–3. doi: 10.1089/end.2006.0386. [DOI] [PubMed] [Google Scholar]
- 6.Wolf JS. Laparoscopic transperitoneal pyeloplasty. J Endourol. 2011;25:173–8. doi: 10.1089/end.2010.0605. [DOI] [PubMed] [Google Scholar]
- 7.Ahlering TE, Skarecky D, Lee D, Clayman RV. Successful transfer of open surgical skills to a laparoscopic environment using a robotic interface: Initial experience with laparoscopic radical prostatectomy. J Urol. 2003;170:1738–41. doi: 10.1097/01.ju.0000092881.24608.5e. [DOI] [PubMed] [Google Scholar]
- 8.Rocco B, Matei DV, Melegari S, Ospina JC, Mazzoleni F, Errico G, et al. Robotic vs open prostatectomy in a laparoscopically naive centre: A matched-pair analysis. BJU Int. 2009;104:991–5. doi: 10.1111/j.1464-410X.2009.08532.x. [DOI] [PubMed] [Google Scholar]
- 9.Braga LH, Pace K, DeMaria J, Lorenzo AJ. Systematic review and meta-analysis of robotic-assisted versus conventional laparoscopic pyeloplasty for patients with ureteropelvic junction obstruction: Effect on operative time, length of hospital stay, postoperative complications, and success rate. Eur Urol. 2009;56:848–57. doi: 10.1016/j.eururo.2009.03.063. [DOI] [PubMed] [Google Scholar]
- 10.Rassweiler JJ, Teber D, Frede T. Complications of laparoscopic pyeloplasty. World J Urol. 2008;26:539–47. doi: 10.1007/s00345-008-0266-z. [DOI] [PubMed] [Google Scholar]
- 11.Gettman MT, Peschel R, Neururer R, Bartsch G. A comparison of laparoscopic pyeloplasty performed with the daVinci robotic system versus standard laparoscopic techniques: Initial clinical results. Eur Urol. 2002;42:453–7. doi: 10.1016/s0302-2838(02)00373-1. [DOI] [PubMed] [Google Scholar]
- 12.Bernie JE, Venkatesh R, Brown J, Gardner TA, Sundaram CP. Comparison of laparoscopic pyeloplasty with and without robotic assistance. JSLS. 2005;9:258–61. [PMC free article] [PubMed] [Google Scholar]
- 13.Link RE, Bhayani SB, Kavoussi LR. A prospective comparison of robotic and laparoscopic pyeloplasty. Ann Surg. 2006;243:486–91. doi: 10.1097/01.sla.0000205626.71982.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hemal AK, Mukherjee S, Singh K. Laparoscopic pyeloplasty versus robotic pyeloplasty for ureteropelvic junction obstruction: A series of 60 cases performed by a single surgeon. Can J Urol. 2010;17:5012–6. [PubMed] [Google Scholar]
- 15.Margossian H, Garcia-Ruiz A, Falcone T, Goldberg JM, Attaran M, Miller JH, et al. Robotically assisted laparoscopic tubal anastomosis in a porcine model: A pilot study. J Laparoendosc Adv Surg Tech A. 1998;8:69–73. doi: 10.1089/lap.1998.8.69. [DOI] [PubMed] [Google Scholar]
- 16.Gofrit ON, Mikahail AA, Zorn KC, Zagaja GP, Steinberg GD, Shalhav AL. Surgeons' perceptions and injuries during and after urologic laparoscopic surgery. Urology. 2008;71:404–7. doi: 10.1016/j.urology.2007.07.077. [DOI] [PubMed] [Google Scholar]


