Abstract
Purpose:
There are many techniques of harvesting vascularized skin flaps from penile skin for hypospadias repairs. Here, we review our experience with the use of longitudinal dorsal island flap (LDIF) for mid- and proximal hypospadias repairs and to assess the results and complications of onlay and tubularized repairs.
Materials and Methods:
We retrospectively reviewed the data of all children with hypospadias operated by a single surgeon using the LDIF technique. The severity of hypospadias, technique, complications, and follow-up were assessed.
Results:
Over a 9.4-year period, 102 children (mean age 4.2 years, range 6 months to 11 years) were operated for primary hypospadias using the LDIF technique. All children had poorly formed urethral plates and hence were considered unsuitable for tubularized incised plate repair. The hypospadias was classified as midpenile, proximal penile/penoscrotal or perineal in 29, 64, and 9 children respectively. Onlay LDIF repair was done in 85 children, while in 17 children, tubularized LDIF repair was performed. At a mean follow-up of 1.8 years, complications occurred in 12 (12%) children. Complications were more common after tubularized repairs than onlay repairs (24% vs. 9.5%). All glans dehiscences occurred after onlay repairs, while meatal stenosis and diverticulum occurred after tubularized repairs. No child had urethral stenosis after onlay repair, and uroflow studies in 16 children demonstrated normal curves and flow rates.
Conclusions:
We report the use of LDIF for single-stage mid and proximal hypospadias repair with good success and an acceptable complication rate. Onlay repairs had fewer complications than tubularized repairs. Our results indicate that the specific advantages and versatility of LDIF make it a good option to consider in cases of hypospadias with poorly developed urethral plates where onlay or substitution urethroplasty is indicated.
Keywords: Chordee, dorsal, hypospadias, onlay, urethroplasty
INTRODUCTION
Hypospadias is a common congenital defect, and whenever possible, a single-stage repair is desirable. The Snodgrass (TIP) repair is widely used for distal hypospadias, but for more proximal hypospadias or hypospadias with poorly formed urethral plate, vascularized skin flaps are employed for substitution urethroplasty. A number of techniques for using vascularized prepucial and penile skin flaps are available. Transversely oriented island flaps from the inner prepuce have certain disadvantages like penile torsion/rotation. Outer skin necrosis is a problem when the two prepucial layers are separated, while poor cosmetic appearance on the ventrum results when both inner and outer prepuce are transferred ventrally as one unit. To overcome these drawbacks, we have been employing the Longitudinal Dorsal Island Flap (LDIF), both as onlay and tubularized urethroplasty. This technique was previously described by Scuderi and popularized by others, with some modifications.[1–5] We present our experience with the use of LDIF for single-stage hypospadias repair in 102 patients, and compare onlay versus tubularized repairs.
MATERIALS AND METHODS
From April 2002 to August 2011, 102 patients with primary hypospadias underwent single-stage repair using LDIF. All children had poorly formed urethral plates and hence were considered unsuitable for tubularized incised plate repair. The hypospadias was classified as midpenile, proximal penile/ penoscrotal or perineal, based on the level of division of corpus spongiosum. In cases with severe chordee requiring division of urethral plate, the metal position was judged after the chordee correction. For some proximal hypospadias cases beyond the penoscrotal junction (scrotal or perineal), the length of island flap may be a limitation. In such cases, our policy is to consider other repairs, including a 2-staged repair; such cases are not included in the present report. The surgical steps of LDIF have already been well described in the literature.[4] Briefly, the penis is degloved completely preserving the urethral plate. The thin distal urethra, when present, is cut back till the level of normal, spongiosum-covered urethra. Chordee correction is assessed by visual assessment in children with mild chordee; in children with severe curvature, chordee correction is assessed by the artificial erection test. In children with residual chordee after complete penile degloving, the urethral plate is divided at the point of maximum curvature. The fibrotic urethral plate and the dysplastic corpus spongiosum are excised to straighten the penis. Once chordee is corrected, glans wings are raised and the length of LDIF required is measured and outlined on the dorsal skin in the midline, extending proximally from the cut edge of the prepuce. Most of the flap is obtained from the outer prepuce, and the distal half of the dorsal penile skin is utilized when necessary; care is taken not to extend the proximal extent of the flap onto the proximal half of dorsal skin. The width of the flap is chosen in such a way that it gives a neourethral caliber of at least 8--10 F in infants and 10--12 F in older children. In cases requiring urethral plate transaction for chordee correction, a wider LDIF is taken for tubularization. The LDIF is carefully and meticulously isolated on its vascular pedicle, separating it from the two lateral skin flaps. Care is however taken not to devascularize these lateral flaps, as they would be used for providing ventral skin cover. Here lies the main advantage of LDIF; due to the axial blood supply to the flaps, all the three flaps can be dissected without compromising the vascularity. Once dissected free, the LDIF is transposed ventrally by buttonholing the center of its mesentery at its base. Thus transposed, the LDIF lies in perfect apposition to the urethral plate without any penile rotation. Onlay urethroplasty is done with a single running stitch of 6/0 vicryl (on double needle) on both sides, starting at the base and continuing distally. The distal part of the flap is sutured to the distal half of the glans after wide glans wings mobilization. For tubularized repairs, a wide proximal anastomosis is fashioned by spatulating the original meatus. A 7 or 8 F feeding tube is kept as a stent and fixed to the glans with a stitch. The suture lines are covered by the mesentery of the LDIF on all sides with interrupted stitches. Glansplasty is completed with 1 or 2 5/0 vicryl stitches. The distal edge of the LDIF is sutured to the glans to provide a wide neomeatus. It is very important to avoid a tight glansplasty. A good prepucial collar is then fashioned. A ventral skin cover is provided by rotating the two lateral dorsal flaps; the more robust and better vascularized flap is used for providing the ventral skin cover [Figure 1]. The feeding tube is left into the diaper as a drip stent for 7--14 days. The children were discharged from the hospital after 1--2 days, and dressing and catheter management was done on outpatient basis. During follow-up, children were examined at 1 month and 3 months, after which yearly follow-up examination was advised. For the past 3 years, we have been performing uroflow studies in all toilet-trained children at follow-up at least 3 months after a successful operation.
Fig 1.
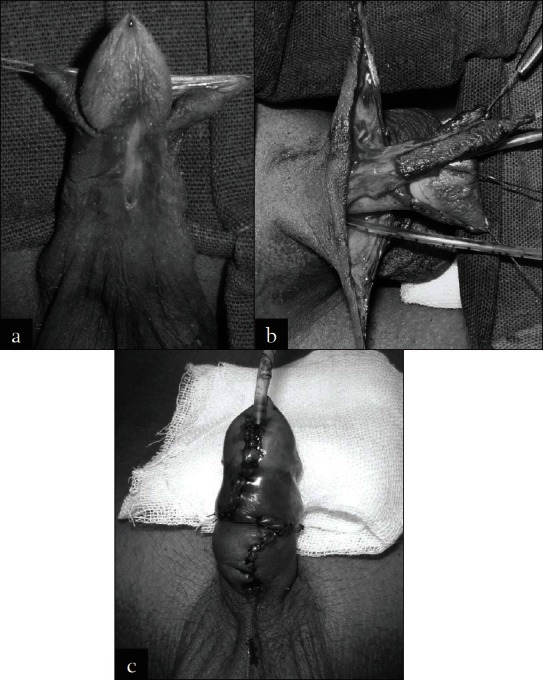
(a) Midpenile hypospadias with poorly formed urethral plate. (b) LDIF (view from dorsum) isolated on vascular pedicle. Note the preserved vasculature to both lateral flaps. (c) Completed repair
RESULTS
From April 2002 to August 2011, 102 children (age 6 months to 11 years, mean 4.2 years) underwent single-stage repair of primary hypospadias using the LDIF technique by a single surgeon. The hypospadias was classified as midpenile, proximal penile/penoscrotal or perineal in 29, 64, and 9 children respectively. Eighty-five children had mild to moderate chordee that was corrected by complete penile degloving and these underwent onlay LDIF repair. In 17 children with residual chordee, urethral plate division and excision along with excision of dysplastic corpus spongiosum was required for chordee correction; tubularized LDIF repair was done in these cases. The length of neourethra created was 14--45 mm (mean 23mm). The average length of neourethra in tubularized repairs was 30 mm. The follow-up ranged from 1 month to 5.2 years (mean 1.8 years). The oldest child is 16 years at follow-up. The shape of the meatus was transverse in children with a shallow glans and vertical in children with a deep glans groove. Complications developed in 8 of 85 children (9.4%) undergoing onlay repair (4 glans dehiscence and 5 fistulae), while 4 of 17 children (24%) undergoing tubularized repair developed complications (3 fistulae and 1 neourethral diverticulum, all 4 had meatal stenosis). Thus, the overall complication rate was 12% (12 of 102 children). In six children, fistula repair was successfully completed at a second operation. Two children are awaiting fistula repair. Of the three children with glans dehiscence, one child underwent reoperation with satisfactory result, while the parents refused further surgery in two children. The child with neourethral diverticulum was lost to follow-up after 6 months when he was advised reoperation. Although no formal scoring was done for the results, in 96 of 102 children (96%), the parents were satisfied with the cosmetic result. Uroflow studies done in 16 children revealed normal (bell shaped) curves with normal flow rates in all of them [Figure 2].
Fig 2.
Uroflow study in a 9-year-old boy 3 months after an LDIF repair demonstrates a normal Bell-shaped curve
DISCUSSION
We review our single-surgeon experience with LDIF for repair of moderate and severe hypospadias in over 100 children. Our results show that single-stage hypospadias repair with LDIF has good success with acceptable complication rates. Our overall complication rate of 12 % favorably compares with other series of mid or proximal hypospadias repairs using the TIP or onlay urethroplasty techniques.[6–10] The most significant finding was the absence of penile torsion or skin necrosis in our series. Our complications with tubularized repairs were significantly more than with onlay LDIF repairs (24% vs. 9.5%). This finding of increased complications with tubularized island flap repairs has been reported previously by others. Due to the better understanding of chordee and its correction with urethral plate preservation, more onlay repairs are being performed, with better results and less complications.[11] However, in children with severe chordee requiring division of urethral plate, considering that most of them would have required a 2-stage repair, a 75% success with single stage tubularized LDIF repair my be still acceptable. Our complication rate of 24% for tubularized repairs favorably compares with other series of tubularized island flap repairs.[7,8,12,13]
In our experience, LDIF has certain advantages over the transverse prepucial flaps. Due to the axial blood supply to the LDIF, it is possible to preserve the blood supply to both the lateral flaps also, which provide ventral skin cover.[4,14] Moreover, according to plastic surgical principles, an axial flap has better blood supply than a random flap.[15] The transverse prepucial island flap has a good axial blood supply; however, necrosis of outer skin and sometimes, the neourethra itself, is a possibility. Necrosis and sloughing of the neourethra has been reported after transverse prepucial island flap repair in 7% of cases.[16] On the other hand, we have not had a single case of flap ischaemia or necrosis with LDIF. A transverse prepucial flap, if dissected up to the base, can be transposed ventrally without penile torsion in most cases; however, penile torsion is a significant risk when a transverse prepucial flap is transposed ventrally and is then oriented in a vertical fashion for urethroplasty.[7,10] In contrast, due to the natural longitudinal orientation of the LDIF, there is no risk of penile rotation or torsion when the flap is transposed ventrally.[4] Thus, no child in our series had penile torsion. Another advantage of the LDIF is that the mesentery of the flap naturally falls in place to cover the neourethral suture lines.[4,14]
The goal of hypospadias surgery is to provide a satisfactory functional and cosmetic result. Functional result means a good caliber neourethra that transmits urine without excess resistance. In children with distal and midpenile hypospadias with a good urethral plate, the TIP repair gives excellent cosmetic and functional results and is our first choice of repair in such cases. However, hypospadias with poorly formed urethral plate and more proximal hypospadias may not be suitable for TIP repair. Holland and Smith studied the impact of urethral plate width and depth on the results following TIP repair for distal hypospadias.[17] They noted that fistulae occurred more commonly in children with narrow (<8mm width) urethral plates while shallow or flat urethral plates resulted in neourethral stenosis after TIP repairs. In their series of 48 boys with distal hypospadias undergoing TIP repair, the overall incidence of neourethral stenosis was 19%, while 40% of boys with a shallow urethral plate developed neourethral stenosis. Of all the complications of hypospadias repair, urethral stricture is the most complex and difficult to repair. Several reports have documented abnormal flow curves with obstructive pattern after TIP repair even in the absence of an actual stricture.[18–20] Braga et al.[21] reported a very high incidence (66.7%) of plateau uroflow curve in boys with penoscrotal hypospadias repaired using the TIP technique. They proposed that the obstructed flow pattern may be secondary to a stiff urethra with low compliance. The long-term effects of these findings on lower urinary tract function are presently unknown. In contrast, the incidence of neourethral strictures reported after onlay island flap urethroplasty has been very low, ranging from 0% to 2.83%.[9,13] We have had no case of neourethral stenosis after onlay LDIF repair in our series. The small number of children in this study subjected to uroflow studies demonstrated satisfactory curves and flow rates. This is because of the ability with onlay repairs to consistently create a good caliber neourethra irrespective of the width or depth of the urethral plate.
There are many techniques to create vascularized island flaps from prepucial and penile skin. Most of these use the inner prepucial skin. In a recent review of the Asopa procedure in 48 patients, Singh et al.[7] reported a complication rate of 22%, mostly fistulas (8 of 11 complications). They observed that tubularized repairs had more complications than onlay repairs. Four of their patients (8%) had some degree of penile torsion. Patel et al.[8] reported good long-term results with a minimum of 10-year follow-up after island tube and island onlay hypospadias repair. They observed that vascularized flaps based on genital skin did not have the long-term stricture rate seen with the use of nongenital skin for substitution urethroplasty. They also observed that tubularized repairs had more complications. To overcome the problem of penile torsion associated with the original Duckett's technique, these authors recently modified the technique by buttonholing the base of the mesentery for ventral transposition of the flap.[22] In a series of 421 hypospadias repairs using the SIS onlay flap, Sedberry-Ross et al.[9] reported good functional and cosmetic result with 0% incidence of neourethral stricture, which they considered the most appealing aspect of their technique. They reported a reoperation rate of 7% for distal and 38% for proximal hypospadias, compared with our results of 9.5% and 28% complications for onlay and tubularized LDIF. Barroso et al.[10] reported the use of a double onlay prepucial flap for single-stage urethroplasty, a technique they developed to overcome the problems with regular onlay island flap repairs, namely penile torsion and necrosis of outer prepucial skin. They reported 75% success with mid- and proximal hypospadias repair using this technique. The present technique of harvesting a longitudinal flap from the dorsal midline skin and prepuce has previously been reported with good success. Perovic and Vukadinovic[4] reported on the use of LDIF in 92 patients with few (5%) complications. They used LDIF as onlay, and recently combined LDIF with buccal mucosal graft for single-stage repair of severe hypospadias.[5] Scuderi et al.[3] recently reviewed their 23-year experience with vertical prepucial flap. About two-thirds of their patients had distal hypospadias, and they reported a 98% overall success with one operation. In contrast, we manage most of our distal hypospadias using the TIP technique, and reserve the LDIF for more proximal hypospadias. In our view, there are some unique advantages of the LDIF. The main limitation of LDIF, as with other island flaps, is the limitation of the length of urethra that can be bridged. It is important that while harvesting long flaps, one must take care not to include hair-bearing skin. Most of our LDIF is harvested from the outer prepuce, which can provide 2--2.5 cm length (the mean length of LDIF in our series is 23 mm). When longer flaps are required, the flap is extended on to the distal penile skin, which is hairless.[4,5] Care must be taken not to raise the flap from the proximal half of penile skin. Because the LDIF is raised from nonhair bearing skin, it has been employed successfully in adolescents and adults also.[4]
Interestingly, we noted that the types of complications arising after onlay and tubularized repairs were different. Glans dehiscence was more common after onlay repair, presumably because the bulk of tissue over which the glans needs to be sutured. All the glans dehiscences occurred early in our experience. A more extensive glans wings mobilization has virtually eliminated this problem in the later cases. Snodgrass et al. reported a 5% glans dehiscence after TIP repair, especially in proximal hypospadias.[23] In our series, meatal stenosis did not occur after onlay repairs, but was common after tubularized island flap repairs, where the most distal part of the neourethral tube may have developed compromised vascularity, especially after glansplasty was completed. Once meatal stenosis is developed, it leads to other complications like fistula and urethral diverticulum. In our series, meatal stenosis was the common feature in all four cases that developed complications following tubularized LDIF repair. Weiner et al. also noted that the type and severity of complications were different between onlay and tubularized island flap repairs, although the overall rate of complications was similar in both groups.[12] They also noted, like us, that diverticulae of the neourethra occurred after tubularized repairs and not with onlay repairs.
In conclusion, we report the use of LDIF for single-stage mid and proximal hypospadias repair in 102 children with good success and a relatively low complication rate. Onlay repairs had fewer complications than tubularized repairs. Our results indicate that the specific advantages and versatility of LDIF make it a good option to consider in cases of hypospadias with poorly developed urethral plates where single-stage onlay or substitution urethroplasty is indicated.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Scuderi N, Campus GV. A new technique for hypospadias one-stage repair. Chir Palst. 1983;7:103–6. [Google Scholar]
- 2.Santanelli F, Blomqvist G, Paolini G, Frati R. correction of hypospadias with a vertical prepucial island flap: The Gotebor g experience of 47 patients. Scand J Plast Reconstr Hand Surg. 2001;35:301–4. doi: 10.1080/028443101750523221. [DOI] [PubMed] [Google Scholar]
- 3.Scuderi N, Chiummariello S, De Gado F. Correction of hypospadias with a vertical prepucial island flap: A 23 years experience. J Urol. 2005;175:1083–7. doi: 10.1016/S0022-5347(05)00407-6. [DOI] [PubMed] [Google Scholar]
- 4.Perovic SV, Vukadinovic V. Onlay island flap urethroplasty for severe hypospadias: A variant of the technique. J Urol. 1994;151:711–4. doi: 10.1016/s0022-5347(17)35067-x. [DOI] [PubMed] [Google Scholar]
- 5.Djordjevic ML, Majstorovic M, Stanojevic D, Bijic M, Kojovic V, Vukadinovic V, et al. Combined buccal mucosa graft and dorsal skin flap for repair of severe hypospadias. Urology. 2008;71:821–5. doi: 10.1016/j.urology.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 6.Snodgrass WT, Yucel S. Tubularized incised plate for midshaft and proximal hypospadias repair. J Urol. 2007;177:698–702. doi: 10.1016/j.juro.2006.09.104. [DOI] [PubMed] [Google Scholar]
- 7.Singh BP, Solanki FS, Kapoor R, Dassi V, Kaswan HK, Agarwal V, et al. Factors predicting success in hypospadias repair using prepucial flap with limited pedicle mobilization (Asopa procedure) Urology. 2010;76:92–6. doi: 10.1016/j.urology.2010.01.020. [DOI] [PubMed] [Google Scholar]
- 8.Patel RP, Shukla AR, Snyder HM., 3rd The island tube and island onlay hypospadias repairs offer excellent long-term outcomes: A 14-year follow-up. J Urol. 2004;172:1717–9. doi: 10.1097/01.ju.0000138903.20136.22. [DOI] [PubMed] [Google Scholar]
- 9.Sedberry-Ross S, Stisser BC, Henderson CG, Rushton HG, Belman AB. Split prepuce in situ onlay hypospadias repair: 17 years experience. J Urol. 2007;178:1663–7. doi: 10.1016/j.juro.2007.03.198. [DOI] [PubMed] [Google Scholar]
- 10.Barroso U, Jr, Jednak R, Barthold JS, Gonzalez R. Further experience with the double onlay prepucial flap for hypospadias repair. J Urol. 2000;164:998–1001. doi: 10.1097/00005392-200009020-00020. [DOI] [PubMed] [Google Scholar]
- 11.Baskin LS, Duckett JW, Ueoka K, Seibold J, Snyder HM. Changing concepts of hypospadias curvature lead to more onlay island flap procedures. J Urol. 1994;151:191–6. doi: 10.1016/s0022-5347(17)34915-7. [DOI] [PubMed] [Google Scholar]
- 12.Weiner JS, Sutherland RW, Roth DR, Gonzales ET., Jr Comparison of onlay and tubularized island flaps of inner prepucial skin for the repair of proximal hypospadias. J Urol. 1997;158:1172–4. doi: 10.1097/00005392-199709000-00123. [DOI] [PubMed] [Google Scholar]
- 13.Castanon M, Munoz E, Carrasco R. treatment of proximal hypospadias with a tubularized island flap urethroplasty and the onlay technique: A comparative study. J Pediatr Surg. 2000;35:1453–5. doi: 10.1053/jpsu.2000.16412. [DOI] [PubMed] [Google Scholar]
- 14.Radojicic ZI, Perovic SV. Classification of prepuce in hypospadias according to morphological abnormalities and their impact on hypospadias repair. J Urol. 2004;172:301–4. doi: 10.1097/01.ju.0000129008.31212.3d. [DOI] [PubMed] [Google Scholar]
- 15.Jordan GH. Principles of tissue handling and transfer. J Urol. 1999;162:1213–7. doi: 10.1016/S0022-5347(01)68137-0. [DOI] [PubMed] [Google Scholar]
- 16.Elbakry A. Complications of the prepucial island flap-tube urethroplasty. BJU Int. 1999;84:89–94. doi: 10.1046/j.1464-410x.1999.00097.x. [DOI] [PubMed] [Google Scholar]
- 17.Holland AJ, Smith GH. Effect of the depth and width of the urethral plate on tubularized incised plate urethroplasty. J Urol. 2000;164:489–91. [PubMed] [Google Scholar]
- 18.Scarpa MG, Castagnetti M, Berrettini A, Rigamonti W, Musi L. Urinary function after Snodgrass repair of distal hypospadias repair: Comparison with Mathieu repair. Pediatr Surg Int. 2010;26:519–22. doi: 10.1007/s00383-010-2569-6. [DOI] [PubMed] [Google Scholar]
- 19.Holmdahl G, Karstrom L, Abrahamsson K. Hypospadias repair with tubularized incised plate: Is uroflowmetry necessary postoperatively? J Pediatr Urol. 2006;2:304–7. doi: 10.1016/j.jpurol.2005.11.018. [DOI] [PubMed] [Google Scholar]
- 20.Wolffenbuttel KP, Wondergem N, Hoefnagels JJ. Abnormal urine flow in boys with distal hypospadias before and after correction. J Urol. 2006;176:1733–6. doi: 10.1016/S0022-5347(06)00614-8. [DOI] [PubMed] [Google Scholar]
- 21.Braga LH, Pippe Salle JL, Lorenzo AJ, Skeldon S, Dave S, Farhat WA, et al. Comparative analysis of Tubularized incised plate versus Onlay island flap urethroplasty for penoscrotal hypospadias. J Urol. 2007;178:1451–6. doi: 10.1016/j.juro.2007.05.170. [DOI] [PubMed] [Google Scholar]
- 22.Patel RP, Shukla AR, Austin C, Canning DA. Modified tubularized transverse prepucial island flap repair for severe proximal hypospadias. BJU Int. 2005;95:901–4. doi: 10.1111/j.1464-410X.2005.05425.x. [DOI] [PubMed] [Google Scholar]
- 23.Snodgrass W, Cost N, Nakonezny PA, Bush N. Analysis of risk factors for glans dehiscence after tubularized incised plate hypospadias repair. J Urol. 2011;185:1845–9. doi: 10.1016/j.juro.2010.12.070. [DOI] [PubMed] [Google Scholar]


