Abstract
Anastomotic leak after low anterior resection (LAR) in patients with rectal cancer who have received neoadjuvant chemoradiation can be challenging to treat and can lead to the creation of a permanent stoma. We report the case of a post-operative anastomotic leak after a Baker-type anastomosis during a low anterior resection was successfully managed with transanal endoscopic microsurgical (TEM) debridement and repair. TEM can be a successful endoluminal alternative treatment in the management of anastomotic leak after LAR and can prevent the morbidity associated with re-exploration and colostomy.
INTRODUCTION
Anastomotic leak after low anterior resection (LAR) in patients with rectal cancer can be challenging to treat. Incidence of anastomotic leak is 3-21% with mortality rates as high as 22% (1,2). Traditionally, treatment of anastomotic leak after LAR involved resection of the anastomosis with end colostomy or suturing of the anastomosis with proximal diversion. Twenty to 60% of patients with colostomy after repair of anastomotic leak are unable to have colostomy reversal (3). We present a case of anastomotic leak following LAR managed via transanal endoscopic microsurgery (TEM).
CASE REPORT
A 47 year-old woman presented with rectal bleeding. Exam revealed a rectal mass 7 cm from the anal verge. Colonoscopy and biopsy confirmed a 4 cm moderately differentiated adenocarcinoma. CT chest/abd/pelvis showed no metastatic disease. Endorectal ultrasound staged the lesion uT2N1; American Joint Committee on Cancer staging was IIIA (T2 N1 M0).
Seven weeks after neoadjuvant chemoradiotherapy, the patient underwent LAR with diverting loop ileostomy. A Baker-type side-to-end anastomosis was created using a 33-EEA stapler (Covidien/JJ) 5 cm from the perianal skin (Figure 1). Both donuts were circumferential and intact. Leak test of the anastomosis with air insufflation was negative. Final pathology demonstrated no residual tumor. Nineteen lymph nodes were negative. After 6 weeks recovery, she underwent postoperative chemotherapy with modified FOLFOX-6.
Fig. 1.
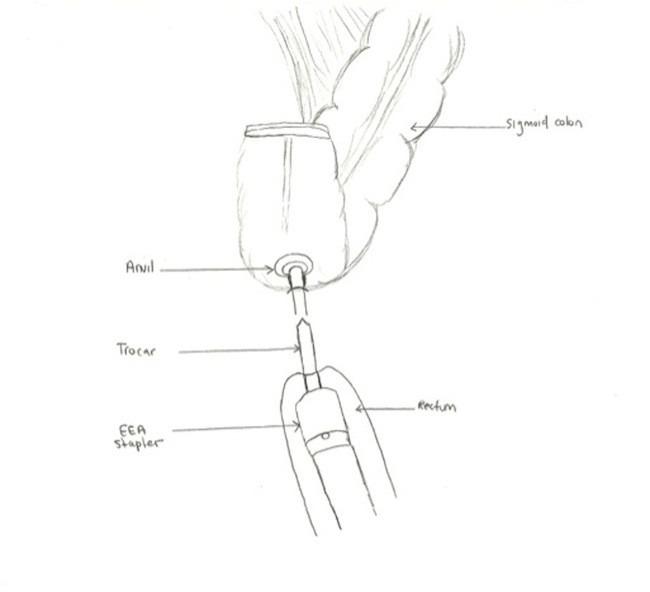
Baker-type side-to-end anastomosis
After completing chemotherapy, the anastomosis was evaluated with gastrograffin enema, which showed a normal anastomosis and no leak (Figure 2). After the enema, the patient experienced rectal pain and fever. Rectal exam revealed a patent anastomosis with mild right-sided tenderness. Flexible sigmoidoscopy revealed a well-healed circular EEA anastomosis. The linear staple line revealed a 3 mm defect (Figure 3). Contrast CT scan of the abdomen and pelvis demonstrated a 2 cm fluid collection along the linear staple line with small amount of free air in adjacent mesenteric fat (Figure 4). Two-week of antibiotics facilitated symptom resolution. Follow-up CT scan documented resolution of the abscess and air.
Fig. 2.
Gastrograffin enema demonstrating normal anastomosis with no leak
Fig. 3.
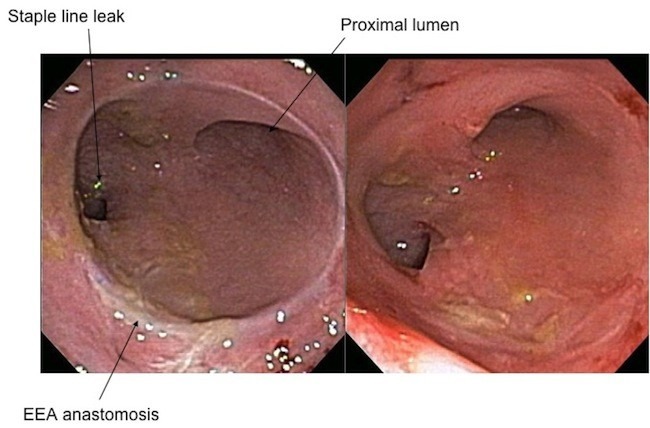
Flexible sigmoidoscopy shows healed EEA anastomosis
Fig. 4.
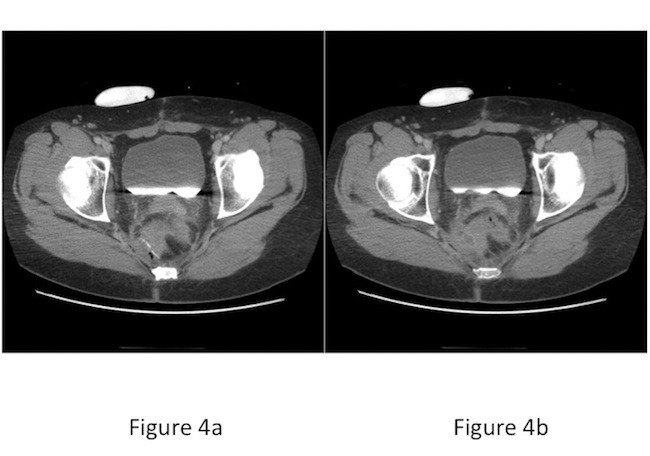
CT scan of abdomen/pelvis a) Small amount of free air adjacent to linear staple line, b) Abscess adjacent to linear staple line
Flexible sigmoidoscopy performed 5 months later was unchanged without evidence of inflammation. After endoscopic exam, she developed recurrent pain and fever. Repeat CT with rectal contrast demonstrated a recurrent 18 x 11 mm pre-sacral abscess but no leakage of rectal contrast from the staple line. Symptoms resolved with intravenous antibiotics. Follow-up CT documented resolution of the abscess.
With persistent anastomotic leak despite multiple courses of antibiotics and fecal diversion, options considered for definitive repair included resection of anastomosis and recreation of the colon-anal anastomosis via hand-sewn approach; resection of anastomosis with end colostomy; attempt at repair/resection of colon distal to EEA staple line; or a novel endoscopic approach. After extensive discussion, we proceeded with transanal endoscopic repair 8 months after diagnosis of anastomotic leak and 15 months after LAR.
Under general anesthesia the sphincter was dilated with the Pratt anoscope. The 40 mm Wolf proctoscope could not be advanced beyond the circular EEA anastomosis. A pliable single incision laparoscopic surgery (SILS) device was inserted across the EEA staple line without difficulty. Through this device, two 5-mm and one 10-mm trocar were used. Insufflation was achieved (7 mmHg). The leak site was identified (Figure 5). Attempts to suture the area closed with 3-0 PDS were unsuccessful due to the small confines of the colon distal to the EEA anastomosis. An Endostitch was used to place a figure-of-eight suture at the leak site. Friable, chronically inflammed tissue tore when the knot was secured. With manipulation, a small amount of pus drained from the chronic abscess cavity. Hook electrocautery opened the linear staple line; inflammatory tissue debrided and wound edges cauterized. She recovered from the procedure uneventfully and discharged on postoperative day one. Eight weeks later, flexible endoscopy confirmed healing of the cavity. CT scan showed no recurrent abscess or leak. She returned for closure of the loop ileostomy. At 3-months follow-up, there is no evidence of recurrent infection and no symptoms of fecal incontinence.
Fig. 5.

Leak site from linear staple line
DISCUSSION
Surgery is evolving from open to more minimally invasive techniques. Studies have shown laparoscopic surgery is associated with decreased postoperative pain, shorter length of stay, improved cosmesis and earlier return to normal daily activities (4,5). TEM is a minimally invasive technique being used more frequently for treatment of rectal diseases.
Khoury et al. examined effects of reoperation after colorectal resection (6). Eighty-nine patients with colorectal cancer were studied; 40 (45%) required reoperation for anastomotic leak and/or intra-abdominal abscess. The group of patients requiring reoperation had significantly higher morbidity, including infections and number of readmissions when compared to the group that didn't require reoperation.
TEM can be used as a minimally invasive approach to anastomotic leak in select patients after LAR for rectal cancer. TEM provides an alternative to major redo pelvic surgery, which carries the risk of intra-operative and postoperative complications resulting in permanent stoma creation, and prevents the morbidity associated with re-exploration and colostomy.
REFERENCES
- 1.Harris LJ, Phillips BR, Maxwell PJ, Isenberg GA, et al. Outcomes of Low Anterior Resection Anastomotic Leak after Preoperative Chemoradiation Therapy for Rectal Cancer. The American Surgeon. 2010; 76:747–751 [PubMed] [Google Scholar]
- 2.Phillips BR, Harris LJ, Maxwell PJ, et al. Anastomotic Leak Rate after Low Anterior Resection for Rectal Cancer after Chemoradiation Therapy. The American Surgeon. 2010; 76:869–871 [PubMed] [Google Scholar]
- 3.Makela JT, Kiviniemi H, Laitinen S. Risk Factors for Anastomotic Leakage after Left-Sided Colorectal Resection with Rectal Anastomosis. Dis Colon Rectum. 2003; 46(5):653–660 [DOI] [PubMed] [Google Scholar]
- 4.Cuschieri A. Laparoscopic surgery: Current status, issues and future developments. Surgeon. 2005; 3(3):125–138 [DOI] [PubMed] [Google Scholar]
- 5.Brody F M., Holzman M., Tarnoff, et al. Summaries of the SAGES 2007 reoperative minimally invasive surgery symposium. Surg Endosc. 2008; 22: 232–244 [DOI] [PubMed] [Google Scholar]
- 6.Khoury W, Lavery IC, Kiran RP. Impact of early reoperation after resection for colorectal cancer on long-term oncologic outcomes. Colorectal Disease. 2011; e-published [DOI] [PubMed] [Google Scholar]


