Abstract
We examined the relationship between parent-perceived neighborhood safety and children's physical activity, sedentary behavior, body mass, and obesity status using 9 years of longitudinal data (1999–2007) on a cohort of approximately 19,000 US kindergartners from the Early Childhood Longitudinal Study. Children's height and weight measurements and parent perceptions of neighborhood safety were available in kindergarten and in the first, third, fifth, and eighth grades. Dependent variables included age- and gender-specific body mass index percentile, obesity status, and parent- or child-reported weekly physical activity and television-watching. Pooled cross-sectional and within-child longitudinal regression models that controlled for child, family, and school characteristics were fitted. Both cross-sectional and longitudinal models indicated that children whose parents perceived their neighborhoods as unsafe watched more television and participated in less physical activity, although the magnitude of this association was much weaker in longitudinal models. However, there was no significant association between parent-perceived neighborhood safety and children's body mass index.
Keywords: body mass index, motor activity, obesity, residence characteristics
Despite evidence that the prevalence of obesity among children and adolescents has plateaued in recent years, it remains a significant public health concern. Approximately 19% of 6- to 19-year-olds are now considered obese (1). The potential for social and physical environments to affect energy balance and obesity among children and adolescents is well recognized (2). Consequently, there has been an increased focus on understanding the influence of environmental factors such as food environment (3–5); access to parks, playgrounds, and recreational facilities (6–8); walkability (9, 10); safety and physical disorder (11–14); neighborhood socioeconomic disadvantage; and collective efficacy (12, 15–17).
Neighborhood safety represents one potentially important, yet less researched, environmental influence on young children's activity behaviors and obesity. Understanding this link is particularly important in the current economic climate as the labor and housing market crises promote concerns about crime and deterioration of neighborhoods. Conceptually, neighborhood safety is likely to influence overall physical activity primarily through outdoor physical activity (see conceptual model in Lake et al. (18)). Time spent outdoors is one of the strongest correlates of physical activity among young children (19–21), and the safety of play spaces is one of the primary factors parents consider in selecting locations for young children's physical activity (22). Because young children's outdoor time is largely regulated by parents, parent perceptions of neighborhood safety are likely to have the most direct influence on the nature and extent of children's outdoor play (23). Parent perceptions are influenced by myriad factors, including actual crime levels in the neighborhood, neighborhood disadvantage (e.g., socioeconomic conditions, social incivilities, physical disorder), individual characteristics (e.g., gender, age, socioeconomic status, victimization experience), and media coverage (24–26). While the link between neighborhood safety and children's obesity is primarily mediated by overall physical activity, another potential channel is dietary changes associated with increased sedentary behavior. For example, outdoor play may be replaced by television-watching, which is associated with increased snack and beverage consumption (27–30).
The limited empirical evidence examining the relationship between neighborhood safety (perceived or objective) and children's energy expenditure and body mass provides mixed results (2, 31, 32). While some studies find that perceptions of safety are correlated with children's physical activity (11, 33–36), a recent literature review concluded that most studies reported null effects (37). Evidence examining the link between neighborhood safety and body weight is even sparser and provides similarly mixed results (12, 13, 38, 39). An important methodological concern for both literatures is that the evidence is based primarily on cross-sectional studies, which may suffer from bias if unmeasured individual or neighborhood characteristics influence perceptions of safety as well as activity behaviors and obesity. In addition, most studies are based on small or localized samples that may have limited generalizability.
To address these concerns, we examined whether changes in parent perceptions of neighborhood safety are associated with changes in children's physical activity, television-watching, body mass index (BMI), and obesity using longitudinal data on a large national sample of children from kindergarten through eighth grade. We hypothesize that a deterioration in parent-perceived neighborhood safety would reduce children's overall physical activity and increase television-watching, BMI, and obesity. We also considered differences by gender, since evidence from smaller studies suggests that girls' activity behaviors may be more responsive to safety concerns (40).
MATERIALS AND METHODS
Data
We analyzed data from the Early Childhood Longitudinal Study—Kindergarten Class (ECLS-K), a longitudinal survey of a nationally representative cohort of US kindergarteners starting in the fall of 1998. The ECLS-K used a multistage probability sample design where the primary sampling units were counties or groups of counties. Schools were sampled within primary sampling units and children within schools (41). Students were followed from kindergarten through eighth grade (1999–2007). Sponsored by the National Center for Education Statistics, the study collected information on children's cognitive, health, and developmental outcomes and contextual data on their families, teachers, and schools. Approximately 18,900 children had complete data for the primary explanatory variable of interest (neighborhood safety) and at least 1 nonmissing dependent variable in kindergarten. Attrition decreased this number in subsequent waves: 15,350 (first grade), 13,330 (third grade), 10,950 (fifth grade), and 8,300 (eighth grade). Attrition was largely due to children who changed schools between waves and were not selected for follow-up. Attrition bias is minimized because the ECLS-K followed a random subsample of half the movers in each wave until fifth grade and all the movers between grades 5 and 8. Children with incomplete BMI data in kindergarten through eighth grade were more likely to be black, Hispanic, and of lower socioeconomic status, but there were no statistically significant differences in mean BMI, obesity, gender, and age at kindergarten. Reported sample sizes have been rounded to the nearest 10 as required by the ECLS-K restricted-use data agreement. Sociodemographic characteristics at baseline are reported in Web Table 1, available at http://aje.oxfordjournals.org/.
Dependent variables
BMI percentile and obesity status
Trained ECLS-K staff measured children's height and weight at each wave using a Shorr Board (Shorr Productions LLC, Olney, Maryland) with an accuracy of 0.01 cm and a Seca digital bathroom scale (model 840; Seca North America West, Chino, California) with an accuracy of 0.1 kg, respectively. Children were asked to remove shoes and other heavy clothing before the measurements. Height and weight were each measured twice to minimize error. Composite height and weight were computed by ECLS-K staff from the 2 readings, which were then used to compute a composite BMI (details in Web Appendix). We calculated age- and gender-specific BMI percentiles based on the 2000 BMI-for-age growth charts issued by the Centers for Disease Control and Prevention (42) to account for differential trends in body growth and fat change across age and gender. A child was classified as obese if BMI percentile was greater than or equal to 95.
Physical activity
The number of days per week on which the child engaged in at least 20 minutes of vigorous exercise was reported by the parent in kindergarten, third, and fifth grades and by the child in eighth grade.
Sedentary behavior
The child's usual number of hours of television-viewing per week was reported by the parent in kindergarten, first, third, and fifth grades and by the child in eighth grade.
Measures of neighborhood safety
Parent perception of neighborhood safety was derived from the survey question “How safe is it for children to play outside during the day in your neighborhood?” Parents indicated whether it was “very safe,” “somewhat safe,” or “not at all safe” in each wave. Because a small proportion responded “not at all safe” (less than 3%), we constructed a dichotomous measure equal to 1 if the parent reported the neighborhood “somewhat safe” or “not at all safe.” Based on this dichotomy, we also constructed a cumulative measure of exposure that captures the number of waves the parent reported the neighborhood unsafe.
Other covariates
Individual-level covariates included age in months, gender, race/ethnicity (non-Hispanic white, non-Hispanic black, Asian, Hispanic, and other race or multirace), mother's education (less than high school, high school graduate or equivalent, some college, and college graduate or higher), annual household income (in categories), urbanicity (urban area, city, town), single-parent household, and number of siblings in the household. Our models also controlled for school-level proxies for socioeconomic conditions, including an indicator for private school, share of minority children in the school, and school size, although we also tested the sensitivity of our results to their exclusion. For children with missing data on covariates (approximately 3%), we replaced missing values with their mean and added binary variables for each covariate indicating which observations were mean-replaced; in sensitivity analyses, we tested the robustness of our findings to casewise deletion of observations with missing data.
Statistical analyses
We first fitted ordinary least-squares regression models by pooling kindergarten through eighth grade data for comparison to previous cross-sectional studies. Both unadjusted and adjusted cross-sectional models were estimated. In addition to the covariates described above, the adjusted models included time (grade)-fixed effects to address differences in parental perceptions of neighborhood safety as children age. However, as discussed previously, even adjusted cross-sectional models are vulnerable to bias from potential endogeneity if unobserved individual and neighborhood characteristics are correlated with perceived neighborhood safety and obesity-related outcomes. For example, parents with a greater preference for healthy living may be more likely to reside in safer neighborhoods and engage in preventive health behaviors that lower BMI. To address such time-invariant unobservables, we leveraged the longitudinal aspect of our data to estimate child fixed-effects models. These within-child linear regressions examined how changes in perceptions of neighborhood safety over time are associated with changes in activity behaviors and BMI for the same child.
We examined the sensitivity of our results in several ways. First, we fitted the longitudinal models separately for movers (i.e., children who changed residence between kindergarten and eighth grade) and nonmovers because changes in their perceived safety over time may come from different sources. For nonmovers, changes in perceived safety would reflect changes in how parents perceive the same neighborhood. However, for those who moved, changes also reflect changes in the neighborhood itself, which may be endogenous to children's health-related outcomes and could introduce bias. To ensure that we accurately measured mover and nonmover status, only children who participated in all waves were included in this analysis. Next, we fitted the longitudinal models by gender to examine whether girls' outcomes respond more strongly to parental perceptions of neighborhood safety as documented in prior cross-sectional studies. Third, we tested the sensitivity of our results to restricting the sample to kindergarten through fifth grade to address concerns that activity behaviors were reported by the child in the eighth grade instead of the parent. Also, by eighth grade, children make more of their own decisions, and parental perceptions may have less influence on the nature and extent of outdoor play. Thus, we conducted weighted longitudinal regression analyses, though we caution that the sample was reduced substantially because longitudinal weights were only available for children who participated in each survey wave. And finally, we examined whether cumulative exposure to an unsafe neighborhood was associated with children's activity and BMI. Our main models linked current perceptions to contemporaneous behavior and outcomes. However, if the effects of neighborhood safety translate into BMI and behavior changes only over a longer period, then these contemporaneous models may be inappropriate. Cumulative models were estimated only for the fifth and eighth grades because we needed sufficient prior waves to construct the cumulative exposure measures. Only children participating in all prior waves were included in order to construct an accurate measure of prior exposure. Fifth (and eighth)-grade BMI was regressed on the number of waves (up to and including the current wave) in which the parent perceived the neighborhood as unsafe. While this model is not purely longitudinal, we controlled for children's kindergarten BMI so that we were essentially comparing the change in BMI among children who had more cumulative exposure to unsafe neighborhoods versus less. In other words, these regressions controlled for selection into neighborhoods based on BMI at school entry.
Statistical analyses were conducted using Stata 10.1 (StataCorp LP, College Station, Texas). Our main estimates were unweighted because ECLS-K's longitudinal weights were not always ideal for all our outcomes and were only available for children who were measured in all included waves (41). Moreover, weighting was not appropriate for the pooled cross-sectional analyses. Therefore, weighted longitudinal estimates are shown only in a sensitivity analysis.
The unit of analysis was a child-wave observation. Standard errors were clustered at the child level to account for multiple observations per child, but further adjustments for the complex survey design were not feasible in Stata for fixed-effects models.
RESULTS
Descriptive results
Table 1 shows the means and proportions for the neighborhood safety and dependent variables by wave. In kindergarten, 30.2% of parents reported living in a neighborhood that was somewhat or not at all safe for children to play outside. By the end of eighth grade, this proportion had declined significantly to 20.0% (P < 0.001). As the cohort aged, the amount of physical activity and television-watching increased, as did the mean BMI percentile and the proportion obese.
Table 1.
Children's Neighborhood Safety, BMI, Physical Activity, and Television-Viewing Characteristics, by Grade, United States, 1999–2007
| Kindergarten (n = 18,900) |
First Grade (n = 15,350) |
Third Grade (n = 13,330) |
Fifth Grade (n = 10,950) |
Eighth Grade (n = 8,300) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | % | Mean (SD) | % | Mean (SD) | % | Mean (SD) | % | Mean (SD) | % | |
| Neighborhood safety | ||||||||||
| Parents report neighborhood as somewhat or not at all safe for children to play outside in | 30.2 | 26.9 | 23.4 | 23.6 | 20.0 | |||||
| Physical activity and sedentary behavior | ||||||||||
| Reported days of vigorous physical activity per week | 3.9 (2.3) | NA | 3.9 (2.0) | 3.7 (1.9) | 4.6 (2.0) | |||||
| Reported hours of television- watching per week | 14.1 (8.3) | 13.4 (9.1) | 13.5 (8.9) | 14.4 (8.7) | 23.2 (19.2) | |||||
| Children's body mass | ||||||||||
| Obesity | 11.6 | 13.1 | 18.6 | 20.3 | 17.6 | |||||
| BMI percentile | 61.0 (28.6) | 61.3 (28.9) | 64.6 (29.1) | 65.4 (29.9) | 64.4 (28.7) | |||||
Abbreviations: BMI, body mass index; NA, not available; SD, standard deviation.
There was considerable within-child variation in parent-perceived safety over time, which is important for estimating the longitudinal models. Between kindergarten and eighth grade, approximately 13% of parents developed more positive perceptions, 8% developed more negative perceptions, and 16% were mixed. The remaining parents consistently responded “somewhat or not at all safe” (9%) or “very safe” (53%) in all waves.
Regression results
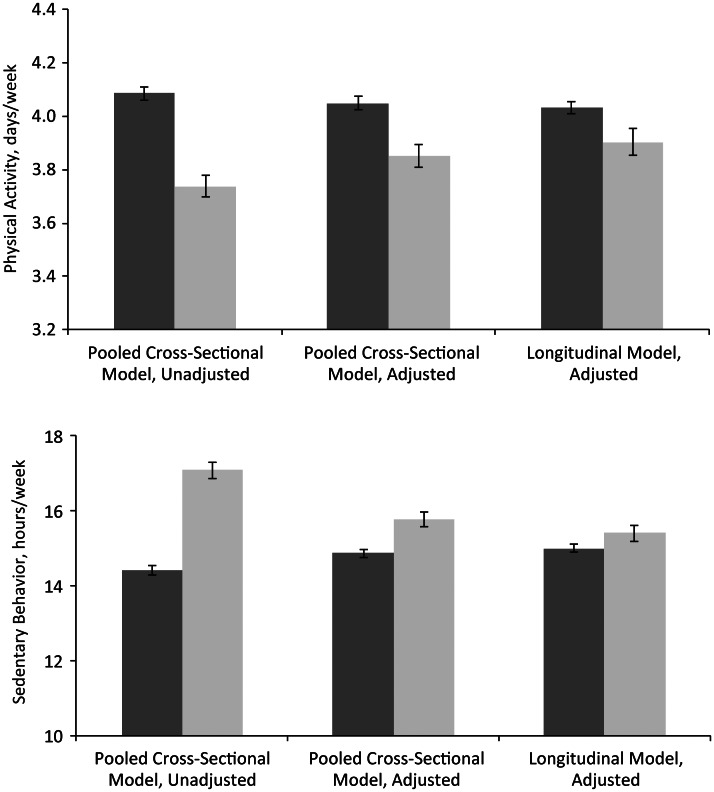
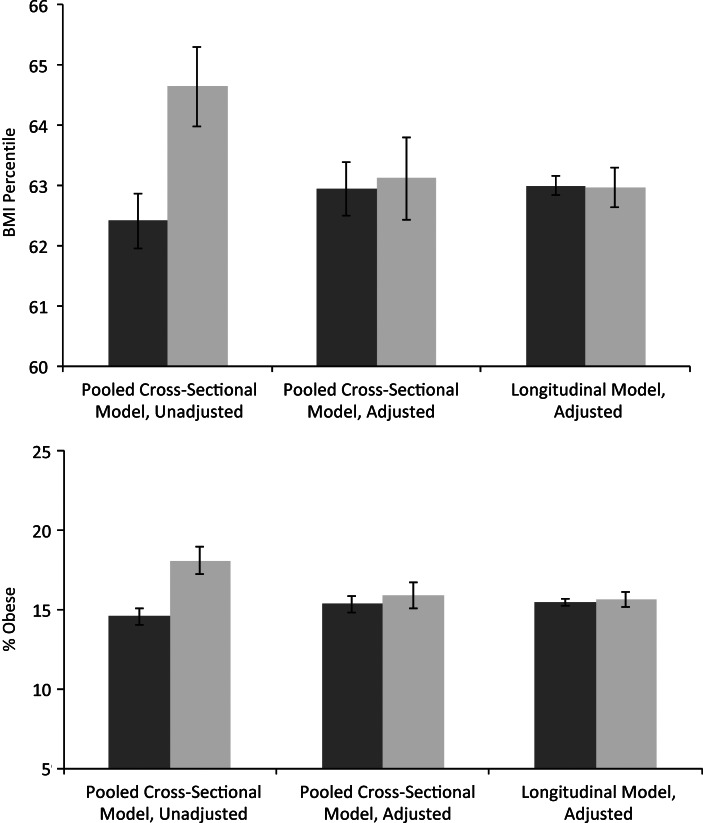
Figures 1 and 2 show predicted values for activity behaviors and BMI-related outcomes, respectively, by perceived neighborhood safety from unadjusted cross-sectional, adjusted cross-sectional, and adjusted longitudinal regression models. Pooled cross-sectional models without other covariates showed that children living in neighborhoods perceived as unsafe by their parents had significantly lower physical activity and significantly higher television-watching, BMI percentile, and obesity relative to those in neighborhoods perceived to be safe. However, these differences became much smaller as observed and unobserved factors were controlled for and remained statistically significant only for the activity behaviors (see detailed estimates in Table 2; full regression results are reported in Web Tables 2 and 3). In particular, the longitudinal models showed that changes in parents' perception of neighborhood safety from “very safe” to “somewhat or not at all safe” were associated with 0.13 fewer days per week of vigorous physical activity (β = −0.127; 95% confidence interval (CI): −0.192, −0.063) and 0.40 additional hours per week of television-watching (β = 0.404; 95% CI: 0.115, 0.694), but were not associated with significant changes in BMI percentile or obesity. These findings were robust to the exclusion of school-level covariates and casewise deletion in lieu of mean imputation for missing data.
Figure 1.
Estimated relationship between parent-perceived neighborhood safety and children's physical activity (top) and sedentary behavior (bottom) in pooled cross-sectional and longitudinal models, United States, 1999–2007. Dark gray columns indicate a neighborhood perceived as safe; light gray columns indicate a neighborhood perceived as not safe. Bars, 95% confidence interval.
Figure 2.
Estimated relationship between parent-perceived neighborhood safety and children's body mass index (BMI; weight (kg)/height (m)2) percentile (top) and obesity (bottom) in pooled cross-sectional and longitudinal models, United States, 1999–2007. Dark gray columns indicate a neighborhood perceived as safe; light gray columns indicate a neighborhood perceived as not safe. Bars, 95% confidence interval.
Table 2.
Regression Estimates (β and Standard Error) for the Relationship Between Parent-Perceived Neighborhood Safety and Children's Physical Activity, Television-Watching, BMI, and Obesity From Full-Sample and Sensitivity Analyses, United States, 1999–2007
| Model Descriptiona | Physical Activity, hours/week | Television-Watching, hours/week | BMIb Percentilec | Obesityd | |
|---|---|---|---|---|---|
| Full samplee | |||||
| Cross-sectional (unadjusted) | −0.349 (0.024)f** | 2.667 (0.123)** | 2.226 (0.368)** | 0.035 (0.005)** | |
| Cross-sectional (adjusted) | −0.200 (0.025)** | 0.910 (0.122)** | 0.175 (0.377) | 0.005 (0.005) | |
| Longitudinal | −0.127 (0.033)** | 0.404 (0.148)** | −0.030 (0.213) | 0.002 (0.003) | |
| Moving statusg | |||||
| Movers | Longitudinal | −0.198 (0.062)** | 0.598 (0.279)* | 0.550 (0.418) | −0.001 (0.006) |
| Nonmovers | Longitudinal | −0.053 (0.058) | 0.482 (0.277) | −0.247 (0.396) | −0.007 (0.006) |
| Genderg | |||||
| Boys | Longitudinal | −0.142 (0.047)** | 0.419 (0.221) | −0.175 (0.311) | 0.003 (0.005) |
| Girls | Longitudinal | −0.118 (0.046)* | 0.387 (0.196)* | 0.136 (0.293) | 0.001 (0.004) |
| Dropping eighth-grade waveg | Longitudinal | −0.184 (0.037)** | 0.269 (0.114)* | −0.121 (0.231) | 0.001 (0.003) |
| With longitudinal weights (children with data in all waves)g | Longitudinal | −0.046 (0.086) | 1.323 (0.630)* | −0.195 (0.675) | −0.009 (0.009) |
| Cumulative neighborhood safetyg | |||||
| Fifth grade | Fifth-grade cross-sectional regression with controls for kindergarten BMI | −0.128 (0.017)** | 0.171 (0.085)* | 0.168 (0.213) | 0.005 (0.003) |
| Eighth grade | Eighth-grade cross-sectional regression with controls for kindergarten BMI | −0.052 (0.018)** | 0.801 (0.168)** | 0.208 (0.214) | 0.001 (0.003) |
Abbreviation: BMI, body mass index.
* P < 0.05; **P < 0.01.
a All models controlled for child's age, mother's education, household income, urbanicity, number of siblings, single-parent household, private school indicator, percentage of minority children in school, and total school enrollment. The cross-sectional models additionally controlled for child's gender and race. The cumulative exposure model also controlled for BMI percentile in kindergarten.
b Weight (kg)/height (m)2.
c Age- and gender-specific BMI percentiles were calculated on the basis of the 2000 BMI-for-age growth charts issued by the Centers for Disease Control and Prevention (42) to account for differential trends in body growth and fat change across age and gender. A child was classified as obese if his or her BMI percentile was greater than or equal to 95.
d The β coefficients capture the change in the probability of being obese (see footnote c). For example, a β of 0.035 means that there is a 3.5-percentage-point increase in the likelihood of being obese.
e Unweighted sample sizes for the full sample regressions (first section of table) ranged from 49,980 to 62,090 for the pooled cross-sectional models and from 44,250 to 58,280 for the longitudinal models.
f Numbers in parentheses, standard error.
g The sample sizes in the fourth-to-sixth sections of the table (as a proportion of the corresponding longitudinal sample) were: movers—25%, nonmovers—30%; boys—50%, girls—50%; dropping eighth-grade wave—86%; with longitudinal weights—50%; and cumulative neighborhood safety—80% of fifth- and eighth-grade samples.
Sensitivity analyses
First, we estimated the longitudinal regressions separately for the mover and nonmover samples (Table 2). Estimates from the mover sample were similar to our main results. However, in the nonmover sample, we found no significant associations with physical activity, television-watching, BMI, or obesity. With respect to gender, we found similar associations between neighborhood safety and children's activity behaviors, BMI, and obesity between boys and girls (Table 2, third section). Likewise, excluding the eighth-grade wave yielded similar results as the full sample (Table 2, fourth section). Next, we used the longitudinal weights, which reduced our sample by more than 50% (Table 2, fifth section). Unsafe neighborhoods were associated with significantly higher television-watching (P < 0.05) but not physical activity, BMI, or obesity. Finally, cross-sectional models with the cumulative measure of neighborhood safety yielded similar results (Table 2, fifth section); conditional on baseline BMI, the number of waves of exposure to unsafe neighborhoods was associated with significantly less physical activity in fifth and eighth grades and more television-watching in eighth grade, but was not associated with BMI or obesity in either grade.
DISCUSSION
This study provides new evidence on the relationships between parent-perceived neighborhood safety and children's activity behaviors and obesity using longitudinal data on a national sample of children. Only a few existing studies have used longitudinal data on large national samples to examine the relationship between perceived neighborhood safety and children's adiposity (14, 38, 43). However, even these studies do not address potential bias due to unobserved confounders because their estimates are derived from random-effects models. Using longitudinal data on both safety and children's outcomes in a fixed-effects approach allowed us to control for selection as well as time-invariant unobservables (such as preferences) that may have confounded previous studies. Indeed, results from Hausman tests for the BMI model do not support the use of random effects in our case. The considerable variation during the 9-year period in parental perceptions of neighborhood safety as well as children's activity behaviors and BMI allowed us to fit the fixed-effects models effectively.
The child fixed-effect models also provided insight into whether unobservables, such as preferences or genetics, bias the results from cross-sectional studies common in this literature. While parent-perceived neighborhood safety was significantly associated with physical activity and television-watching, even in fixed-effect models, these associations were weaker than those estimated from cross-sectional models. This suggests that cross-sectional models overestimate the relationship between perceived neighborhood safety and children's activity behaviors due to unobserved differences between children living in safe versus unsafe neighborhoods that independently influence activity behaviors. Despite a significant relationship in the unadjusted cross-sectional models, no significant relationships were documented for BMI or obesity in the adjusted cross-sectional and longitudinal models.
Our findings were robust to several sensitivity tests and sample restrictions. The lone exception was the lack of any association between neighborhood safety and physical activity in the nonmover sample despite a significant relationship in the mover sample. While the smaller sample size may contribute, the null finding is also consistent with some upward bias in our main estimates and provides further support that perceived neighborhood safety is not a significant risk factor for obesity in young children. While some cross-sectional studies have found that unsafe neighborhoods translate into less physical activity and higher BMI among girls (13, 40), our gender-specific longitudinal models identified similar effects for boys and girls. Finally, we also fitted “dose-response” models that examined whether cumulative exposure to unsafe neighborhoods mattered, and found no evidence supporting a relationship for BMI despite evidence of a relationship with activity behaviors. To our knowledge, prior studies have not examined the role of cumulative exposure to unsafe neighborhoods among children.
We considered potential explanations for the null findings for children's BMI and obesity. Insufficient statistical power seems unlikely given that BMI was systematically measured and so less vulnerable to nonrandom measurement error than our parent- and child-reported activity measures. However, we had sufficient power to detect significant differences in these reported measures. Moreover, the coefficients in our BMI and obesity models were very small and precisely estimated. A more plausible explanation is that the relationship with activity behaviors, while statistically significant, may not be large enough to significantly impact energy balance. Indeed, the coefficients suggest only a 3% difference over respective means at baseline for physical activity and television-watching. This finding also suggests that there may be some substitution across types of activity (e.g., outdoors vs. indoors) or that other factors may play a larger role in activity decisions.
Our study focused on parent perceptions of neighborhood safety and did not examine “objective” measures, such as crime rates and physical disorder, mainly because these were not available at a sufficiently fine geography for our data. There are several advantages to using parental perceptions in our context. First, unlike older children and adults, young children's outdoor time is largely regulated by parents and, therefore, parent perceptions are likely to have the most direct influence on children's outdoor play. Second, perceptions of safety are arguably the more relevant construct for examining changes in behavior vis-à-vis objective measures—that is, parents must first perceive that there is a problem in their neighborhood before they modify their children's activity behaviors (18, 44). As discussed above, objective measures are correlated with perceptions of safety; however, the estimated correlation varies considerably across studies, suggesting the importance of other factors (44, 45). Third, unlike geography-based objective measures, perceptions allow each parent to determine the relevant neighborhood definition for the purposes of his or her own child's outdoor play. Finally, perceived measures have the advantage that, unlike objective measures, they allow parents to differentially weight various aspects of the physical and social environment to arrive at an overall measure. Differences in weights parents assign to the various safety aspects might dilute the associations with objective measures of safety.
Despite its strengths, our study had some limitations. First, measures of physical activity and television-watching are reported by parents and children and may therefore suffer from measurement error. Prior review studies (46, 47) found the validity and reliability coefficients of parent reports (for children) and self-reports (for adolescents) acceptable, though lower than those for objective measures. Moreover, given that our purpose was not to accurately estimate the prevalence of these behaviors in the population but to consider changes in these behaviors within groups, these measures are acceptable. Second, our measure of physical activity only captured vigorous activity; therefore, we were unable to examine how changes in neighborhood safety may influence moderate- or low-intensity activities (e.g., walking). However, our null findings for BMI and obesity suggest that any potential effects on these activities are likely to be small as well. We also lacked insight into other mechanisms such as changes in diet because overall diet quality and caloric intake were not collected. The ECLS-K collected frequency of intake of a limited set of food items, but only in 2 waves. Third, while the child fixed-effect models controlled for time-invariant unobserved differences across children living in neighborhoods perceived as safe versus unsafe, there may still have been time-varying unobserved confounders that may have introduced bias. Fourth, while our results suggest no association between perceived neighborhood safety and children's BMI in the short run, there is evidence that obesogenic behaviors can persist into adulthood (48). That is, watching more television or exercising less during childhood may be habit-forming and their consequences may only emerge over a longer time period than was used in this study. Finally, as discussed above, our analyses were largely unweighted and did not adjust for the complex survey design; therefore, readers should be cautious about inferring representativeness.
In summary, our findings suggest that parent perceptions of neighborhood safety do not represent a significant risk factor for obesity among school-aged children during the time frame analyzed. Future research should examine the replicability of these findings and their underlying mechanisms.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: RAND Corporation, Santa Monica, California (Ashlesha Datar); RAND Corporation, Boston, Massachusetts (Nancy Nicosia); and Pardee RAND Graduate School, RAND Corporation, Santa Monica, California (Victoria Shier).
This work was supported by grant 1R03HD061688-01A1 from the National Institute of Child Health and Human Development.
All opinions are those of the authors and do not represent the opinions of the funding agency.
Conflict of interest: none declared.
REFERENCES
- 1.Ogden CL, Carroll MD, Curtin LR, et al. Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA. 2010;303(3):242–249. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 2.Spruijt-Metz D. Etiology, treatment, and prevention of obesity in childhood and adolescence: a decade in review. J Res Adolesc. 2011;21(1):129–152. doi: 10.1111/j.1532-7795.2010.00719.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Powell LM, Auld MC, Chaloupka FJ, et al. Associations between access to food stores and adolescent body mass index. Am J Prev Med. 2007;33(4):S301–S307. doi: 10.1016/j.amepre.2007.07.007. [DOI] [PubMed] [Google Scholar]
- 4.Auld MC, Powell LM. Economics of food energy density and adolescent body weight. Economica. 2009;76(304):719–740. [Google Scholar]
- 5.Sturm R. Disparities in the food environment surrounding US middle and high schools. Public Health. 2008;122(7):681–690. doi: 10.1016/j.puhe.2007.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Babey SH, Hastert TA, Huang W, et al. Sociodemographic, family, and environmental factors associated with active commuting to school among US adolescents. J Public Health Policy. 2009;30(1):S203–S220. doi: 10.1057/jphp.2008.61. [DOI] [PubMed] [Google Scholar]
- 7.Colabianchi N, Kinsella AE, Coulton CJ, et al. Utilization and physical activity levels at renovated and unrenovated school playgrounds. Prev Med. 2009;48(2):140–143. doi: 10.1016/j.ypmed.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 8.Pate RR, Colabianchi N, Porter D, et al. Physical activity and neighborhood resources in high school girls. Am J Prev Med. 2008;34(5):413–419. doi: 10.1016/j.amepre.2007.12.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spence JC, Cutumisu N, Edwards J, et al. Influence of neighbourhood design and access to facilities on overweight among preschool children. Int J Pediatr Obes. 2008;3(2):109–116. doi: 10.1080/17477160701875007. [DOI] [PubMed] [Google Scholar]
- 10.Nelson N, Woods C. Obesogenic environments: are neighbourhood environments that limit physical activity obesogenic? Health Place. 2009;15(4):917–924. doi: 10.1016/j.healthplace.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 11.Molnar BE, Gortmaker SL, Bull FC, et al. Unsafe to play? Neighborhood disorder and lack of safety predict reduced physical activity among urban children and adolescents. Am J Health Promot. 2004;18(5):378–386. doi: 10.4278/0890-1171-18.5.378. [DOI] [PubMed] [Google Scholar]
- 12.Franzini L, Elliott MN, Cuccaro P, et al. Influences of physical and social neighborhood environments on children's physical activity and obesity. Am J Public Health. 2009;99(2):271. doi: 10.2105/AJPH.2007.128702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bacha JM, Appugliese D, Coleman S, et al. Maternal perception of neighborhood safety as a predictor of child weight status: the moderating effect of gender and assessment of potential mediators. Int J Pediatr Obes. 2010;5(1):72–79. doi: 10.3109/17477160903055911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cecil-Karb R, Grogan-Kaylor A. Childhood body mass index in community context: neighborhood safety, television viewing, and growth trajectories of BMI. Health Soc Work. 2009;34(3):169–177. doi: 10.1093/hsw/34.3.169. [DOI] [PubMed] [Google Scholar]
- 15.Cradock AL, Kawachi I, Colditz GA, et al. Neighborhood social cohesion and youth participation in physical activity in Chicago. Soc Sci Med. 2009;68(3):427–435. doi: 10.1016/j.socscimed.2008.10.028. [DOI] [PubMed] [Google Scholar]
- 16.Greves Grow HM, Cook AJ, Arterburn DE, et al. Child obesity associated with social disadvantage of children's neighborhoods. Soc Sci Med. 2010;71(3):584–591. doi: 10.1016/j.socscimed.2010.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kimbro RT, Brooks-Gunn J, McLanahan S. Young children in urban areas: links among neighborhood characteristics, weight status, outdoor play, and television watching. Soc Sci Med. 2011;72(5):668–676. doi: 10.1016/j.socscimed.2010.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lake AA, Townshend TG, Alvanides S. Obesogenic Environments: Complexities, Perceptions, and Objective Measures. Chichester, United Kingdom: Wiley-Blackwell; 2010. [Google Scholar]
- 19.Klesges RC, Eck LH, Hanson CL, et al. Effects of obesity, social interactions, and physical environment on physical activity in preschoolers. Health Psychol. 1990;9(4):435–449. doi: 10.1037//0278-6133.9.4.435. [DOI] [PubMed] [Google Scholar]
- 20.Sallis JF, Nader PR, Broyles SL, et al. Correlates of physical activity at home in Mexican-American and Anglo-American preschool children. Health Psychol. 1993;12(5):390–398. doi: 10.1037//0278-6133.12.5.390. [DOI] [PubMed] [Google Scholar]
- 21.Baranowski T, Thompson WO, DuRant RH, et al. Observations on physical activity in physical locations: age, gender, ethnicity, and month effects. Res Q Exerc Sport. 1993;64(2):127–133. doi: 10.1080/02701367.1993.10608789. [DOI] [PubMed] [Google Scholar]
- 22.Sallis JF, McKenzie TL, Elder JP, et al. Factors parents use in selecting play spaces for young children. Arch Pediatr Adolesc Med. 1997;151(4):414–417. doi: 10.1001/archpedi.1997.02170410088012. [DOI] [PubMed] [Google Scholar]
- 23.Kalish M, Banco L, Burke G, et al. Outdoor play: a survey of parent's perceptions of their child's safety. J Trauma. 2010;69(4):S218–S222. doi: 10.1097/TA.0b013e3181f1eaf0. [DOI] [PubMed] [Google Scholar]
- 24.Taylor RB, Harrell AV. Physical Environment and Crime. Washington, DC: National Institute of Justice; 1996. [Google Scholar]
- 25.Austin DM, Furr LA, Spine M. The effects of neighborhood conditions on perceptions of safety. J Crim Justice. 2002;30(5):417–427. [Google Scholar]
- 26.Callanan VJ. Media consumption, perceptions of crime risk and fear of crime: examining race/ethnic differences. Sociol Perspect. 55(1):93–115. [Google Scholar]
- 27.Francis LA, Lee Y, Birch LL. Parental weight status and girls’ television viewing, snacking, and body mass indexes. Obes Res. 2003;11(1):143–151. doi: 10.1038/oby.2003.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Phillips SM, Bandini LG, Naumova EN, et al. Energy-dense snack food intake in adolescence: longitudinal relationship to weight and fatness. Obes Res. 2004;12(3):461–472. doi: 10.1038/oby.2004.52. [DOI] [PubMed] [Google Scholar]
- 29.Campbell KJ, Crawford DA, Ball K. Family food environment and dietary behaviors likely to promote fatness in 5–6 year-old children. Int J Obes (Lond) 2006;30(8):1272–1280. doi: 10.1038/sj.ijo.0803266. [DOI] [PubMed] [Google Scholar]
- 30.Wiecha JL, Peterson KE, Ludwig DS, et al. When children eat what they watch: impact of television viewing on dietary intake in youth. Arch Pediatr Adolesc Med. 2006;160(4):436–442. doi: 10.1001/archpedi.160.4.436. [DOI] [PubMed] [Google Scholar]
- 31.Galvez MP, Pearl M, Yen IH. Childhood obesity and the built environment: a review of the literature from 2008–2009. Curr Opin Pediatr. 2010;22(2):202. doi: 10.1097/MOP.0b013e328336eb6f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dunton G, Kaplan J, Wolch J, et al. Physical environmental correlates of childhood obesity: a systematic review. Obes Rev. 2009;10(4):393–402. doi: 10.1111/j.1467-789X.2009.00572.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pham KL, Harrison GG, Kagawa-Singer M. Perceptions of diet and physical activity among California Hmong adults and youths. Prev Chronic Dis. 2007;4(4):A93. [PMC free article] [PubMed] [Google Scholar]
- 34.Romero AJ. Low-income neighborhood barriers and resources for adolescents’ physical activity. J Adolesc Health. 2005;36(3):253–259. doi: 10.1016/j.jadohealth.2004.02.027. [DOI] [PubMed] [Google Scholar]
- 35.Wen LM, Kite J, Merom D, et al. Time spent playing outdoors after school and its relationship with independent mobility: a cross-sectional survey of children aged 10–12 years in Sydney, Australia. Int J Behav Nutr Phys Act. 2009;6:15. doi: 10.1186/1479-5868-6-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Weir LA, Etelson D, Brand DA. Parents’ perceptions of neighborhood safety and children's physical activity. Prev Med. 2006;43(3):212–217. doi: 10.1016/j.ypmed.2006.03.024. [DOI] [PubMed] [Google Scholar]
- 37.Carver A, Timperio A, Crawford D. Playing it safe: the influence of neighbourhood safety on children's physical activity—a review. Health Place. 2008;14(2):217–227. doi: 10.1016/j.healthplace.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 38.Burdette AM, Needham BL. Neighborhood environment and body mass index trajectories from adolescence to adulthood. J Adolesc Health. 2012;50(1):30–37. doi: 10.1016/j.jadohealth.2011.03.009. [DOI] [PubMed] [Google Scholar]
- 39.Burdette HL, Whitaker RC. A national study of neighborhood safety, outdoor play, television viewing, and obesity in preschool children. Pediatrics. 2005;116(3):657. doi: 10.1542/peds.2004-2443. [DOI] [PubMed] [Google Scholar]
- 40.Gomez JE, Johnson BA, Selva M, et al. Violent crime and outdoor physical activity among inner-city youth. Prev Med. 2004;39(5):876–881. doi: 10.1016/j.ypmed.2004.03.019. [DOI] [PubMed] [Google Scholar]
- 41.Tourangeau K, Nord C, Lê T, et al. Early Childhood Longitudinal Study, Kindergarten Class of 1998–99 (ECLS-K), Combined User's Manual for the ECLS-K Eighth-Grade and K-8 Full Sample Data Files and Electronic Codebooks. Washington, DC: National Center for Education Statistics, US Department of Education; 2009. pp. 1–61. :4-1–4-61. [Google Scholar]
- 42.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC growth charts for the United States: methods and development. Vital Health Stat 11. 2002;(246):1–190. [PubMed] [Google Scholar]
- 43.Crawford D, Cleland V, Timperio A, et al. The longitudinal influence of home and neighbourhood environments on children's body mass index and physical activity over 5 years: the CLAN study. Int J Obes. 2010;34(7):1177–1187. doi: 10.1038/ijo.2010.57. [DOI] [PubMed] [Google Scholar]
- 44.Hipp JR. Assessing crime as a problem: the relationship between residents’ perception of crime and official crime rates over 25 years. Crime Delinq. 2010 [published onle ahead of print October 18, 2010]. ( doi:10.1177/0011128710382264). [Google Scholar]
- 45.Elo IT, Mykyta L, Margolis R, et al. Perceptions of neighborhood disorder: the role of individual and neighborhood characteristics. Soc Sci Q. 2009;90(5):1298–1320. doi: 10.1111/j.1540-6237.2009.00657.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Trost SG. State of the art reviews: measurement of physical activity in children and adolescents. Am J Lifestyle Med. 2007;1(4):299–314. [Google Scholar]
- 47.Loprinzi PD, Cardinal BJ. Measuring children's physical activity and sedentary behaviors. J Exerc Sci Fit. 2011;9(1):15–23. [Google Scholar]
- 48.Dietz WH, Gortmaker SL. Preventing obesity in children and adolescents 1. Annu Rev Public Health. 2001;22(1):337–353. doi: 10.1146/annurev.publhealth.22.1.337. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.