Abstract
Primary cardiac tumors do not occur frequently, and only one quarter of them, chiefly sarcomas, are malignant. Patients with angiosarcoma typically have a shorter survival time than do patients with other sarcomas, and the prognosis for survival depends strictly on the stage of the disease at the time of diagnosis and the possibility of complete surgical excision. Chemotherapy and radiotherapy have well-established postoperative roles because of the high probability of metastasis.
We report the case of a 25-year-old man who presented with pericardial effusion and echocardiographic evidence of an intracavitary right atrial mass but without the bulky, infiltrative growth typical of this location of the disease. Malignancy was suggested by the clinical presentation, the location of the mass in the right side of the heart, and the absence of conditions favoring thrombus formation. After complete surgical excision, the mass was confirmed to be an angiosarcoma. Conventional adjuvant chemotherapy and maintenance therapy with inhibitors of CD117 (c-kit) and vascular endothelial growth factor relieved the patient's clinical symptoms and enabled his long-term, disease-free survival. In addition to reporting this case, we discuss aspects of the diagnosis and treatment of angiosarcoma.
Key words: Antineoplastic combined chemotherapy protocols/therapeutic use; chemotherapy, adjuvant; disease-free survival; heart neoplasms/drug therapy/epidemiology/surgery; prognosis; sarcoma/surgery/therapy; treatment outcome
Cardiac angiosarcoma, the most common malignant tumor of the heart, originates from mesenchymal tissue and endothelial subepicardium. Although angiosarcoma constitutes approximately 31% of all malignant tumors, it is a rare cardiac disease. Immediate treatment is crucial. The diagnosis of angiosarcoma is often delayed, because early signs can be absent or generic. Indicative symptoms of potential cardiac disease—exertional dyspnea, chest pain, cough, syncope, arrhythmias, clinical and instrumental evidence of pericardial effusion leading to cardiac tamponade, and pleural effusion—occur late in the progression of angiosarcoma. Right atrial presentation is the most common and often the most difficult to diagnose, because the mass tends to extend exteriorly into the adjacent pericardium and develop in the right side of the heart through the great veins and tricuspid valve at a later stage of the disease.
We report the case of a patient who presented with pericardial effusion and evidence of a right atrial mass that was suspected to be malignant, and we discuss aspects of the diagnosis and treatment of angiosarcoma.
Case Report
In December 2010, a 25-year-old man presented at our institution with pericardial effusion and a right atrial mass. His symptoms of sudden severe chest pain and moderate dyspnea had begun 2 months before the current presentation. He had initially been admitted to a primary care center, where the pericardial effusion was diagnosed and treated with indomethacin. Because of persistent dyspnea, he was referred to another hospital, where an echocardiogram showed a right atrial mass, and cardiac magnetic resonance revealed characteristics of angiosarcoma. A fine-needle aspiration biopsy of the mass yielded only inflammatory cells. Results of a total-body computed tomographic (CT) scan confirmed the presence of a right atrial mass without apparent metastasis (Fig. 1).

Fig. 1 Computed tomogram of the chest shows right atrial enlargement (arrow).
At the presentation in late 2010, the patient was asymptomatic and reported no personal or family history of tumors. However, he was affected by familial dyslipidemia and asthma. Results of a cardiac clinical examination and chest radiography were not unusual. An electrocardiogram showed sinus tachycardia at 105 beats/min with high P waves. Transthoracic and transesophageal echocardiograms showed pericardial effusion in the presence of a 4.8 × 3.9-cm intracavitary mass that adhered to the upper lateral wall of the right atrium. The mass involved the right atrial appendage but not the venae cavae or tricuspid valve (Fig. 2). The patient's right ventricular dimensions were at the upper limits of normal, and contractility was preserved.
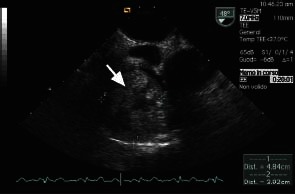
Fig. 2 Transesophageal echocardiogram shows the mass (arrow) inside the right atrium.
The patient was taken for surgical removal of the mass. After pericardiotomy, the right atrium appeared to adhere to the adjacent pericardium. Normothermic cardiopulmonary bypass was started after we dissected the right atrial wall from the pericardium. On the beating heart and with use of total extracorporeal circulation, we approached the right atrium through a longitudinal incision 0.5 cm from the right atrioventricular groove. We excised an ovoid mass together with the atrial wall around the junction with the venae cavae, achieving a complete macroscopic resection (Fig. 3). We then reconstructed the right atrium, using a large patch of autologous pericardium. The total time of cardiopulmonary bypass was 70 minutes.
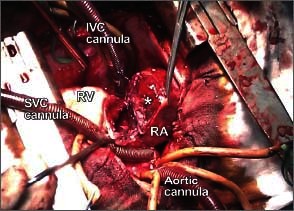
Fig. 3 Intraoperative photograph shows the mass (asterisk) adhering to the right atrial wall
IVC = inferior vena cava; RA = right atrium; RV = right ventricle; SVC = superior vena cava
The histologic characteristics of the mass suggested myocardial angiosarcoma: sinusoidal vascular channels full of red blood cells and lined with atypical endothelial cells, and areas of round, spindle, and polyhedral cells with frequent mitotic figures interspersed (Fig. 4). Immunohistochemical analysis was positive for vimentin, CD31, CD34, actin, and focal factor VIII. The margins of the excised mass were free of infiltrative disease. The pericardial samples consisted of fibrinous deposits with lymphocytes and reactive mesothelial cells and were negative for malignant cells. In anticipation of the patient's need for therapy with multikinase inhibitors, we performed an immunohistochemical evaluation for CD117 (c-kit) and epidermal growth factor receptor (EGFR). There was mild plurifocal positivity for c-kit; however, the results for EGFR were negative.
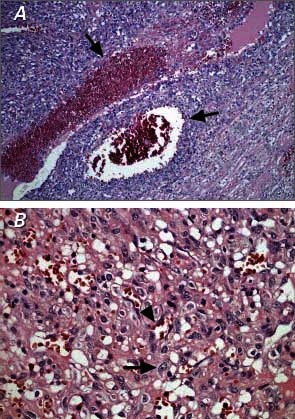
Fig. 4 Photomicrographs of the lesion show A) sinusoidal vascular channels (arrows) (H & E, orig. ×100), and B) atypical endothelial cells with granular or glassy cytoplasm (arrow) and intraluminal red blood cells (arrowhead) (H & E, orig. ×400).
The patient was discharged from the hospital 6 days postoperatively after normal echocardiographic results. An early postoperative total-body CT scan and bone scintigraphy showed no residual or metastatic disease. The patient was referred to oncologists and underwent 4 cycles of chemotherapy with gemcitabine and docetaxel, followed by 30 fractions of external radiotherapy. Because of a suspected lesion in the inferior right pulmonary lobe that appeared on CT in the 9th postoperative month, we introduced oral maintenance therapy with a c-kit inhibitor (imatinib) for 3 months. This therapy was discontinued when the lesion was found to be resolved at the next follow-up examination. Eighteen months postoperatively, the patient had a local recurrence of disease that was treated with weekly paclitaxel for 6 cycles. As of March 2013, the patient was in good general condition after chemotherapy stabilized the disease, and he was to begin radiation therapy.
Discussion
Primary cardiac tumors have had a prevalence of only 0.02% in a review of autopsy series.1 Metastatic tumors are 20 to 40 times more frequent: the primary neoplasms are lymphoma, leukemia, malignant melanoma, lung cancer, and breast cancer. Moreover, only one quarter of the primary cardiac tumors in the adult population are malignant; of these, most are sarcomas. Without surgical resection, patients with angiosarcoma typically live for 9 to 12 months.2 This survival time is short compared with that of other cardiac sarcomas,3,4 and a patient's longevity strictly depends on the stage of the disease and the possibility of complete surgical excision.3 Early diagnosis is crucial for rapid, complete removal of the tumor. However, diagnosis can be a challenge, because cardiac angiosarcomas often remain clinically silent until the disease is advanced. Most cases are diagnosed incidentally or during screening examinations after pericardial effusion. Angiosarcoma usually appears as a bulky, infiltrative growth with early metastasis in the right side of the heart; however, it sometimes exhibits slow intracavitary development that mimics a myxoma or thrombotic mass. The location of the tumor and the absence of conditions leading to thrombus formation play an important role in suggesting possible malignancy, because cardiac malignancies have a tendency to occur in the right side of the heart.5
There is little agreement on the choice of chemotherapeutic agents for angiosarcoma after resection. Chemotherapy and radiotherapy have a well-established place in the therapeutic algorithm, because angiosarcomas have a high probability of metastatic diffusion.6 The most common chemotherapeutic drugs are adriamycin, ifosfamide, cyclophosphamide, vincristine, and dacarbazine, and paclitaxel is also typically administered weekly. Tailored chemotherapy might overcome resistance to the principal drugs that are used to treat certain malignancies. The most important targets in this therapeutic approach are cytokines and their receptors, which are involved in cell growth, survival, and differentiation through kinase signaling pathways. Multikinase inhibitors are not conventional drugs in angiosarcoma therapy; they are typically reserved for stromal tumors (for example, gastrointestinal) in which there is a high expression of CD117 and vascular endothelial growth factor. Two recent phase II trials of sorafenib, bevacizumab, and imatinib in the treatment of advanced or metastatic angiosarcoma have yielded objective data on the efficacy of these anti-angiogenetic drugs.7 In our patient, the specific findings of the CD117 receptor enabled us to use this family of drugs as maintenance therapy after satisfactory results were attained through the combination of surgery and conventional chemotherapy.
Footnotes
Address for reprints: Marianna Buonocore, MD, Via Torretta di Siena 66, Torre Annunziata 80058, Naples, Italy
E-mail: mariannabuonocore@rocketmail.com
References
- 1.Reynen K. Frequency of primary tumors of the heart. Am J Cardiol 1996;77(1):107. [DOI] [PubMed]
- 2.Pigott C, Welker M, Khosla P, Higgins RS. Improved outcome with multimodality therapy in primary cardiac angiosarcoma. Nat Clin Pract Oncol 2008;5(2):112–5. [DOI] [PubMed]
- 3.Simpson L, Kumar SK, Okuno SH, Schaff HV, Porrata LF, Buckner JC, Moynihan TJ. Malignant primary cardiac tumors: review of a single institution experience. Cancer 2008; 112(11):2440–6. [DOI] [PubMed]
- 4.Llombart-Cussac A, Pivot X, Contesso G, Rhor-Alvarado A, Delord JP, Spielmann M, et al. Adjuvant chemotherapy for primary cardiac sarcomas: the IGR experience. Br J Cancer 1998;78(12):1624–8. [DOI] [PMC free article] [PubMed]
- 5.Patel J, Sheppard MN. Pathological study of primary cardiac and pericardial tumours in a specialist UK centre: surgical and autopsy series. Cardiovasc Pathol 2010;19(6):343–52. [DOI] [PubMed]
- 6.Blackmon SH, Reardon MJ. Surgical treatment of primary cardiac sarcomas. Tex Heart Inst J 2009;36(5):451–2. [PMC free article] [PubMed]
- 7.Penel N, Marreaud S, Robin YM, Hohenberger P. Angiosarcoma: state of the art and perspectives. Crit Rev Oncol Hematol 2011;80(2):257–63. [DOI] [PubMed]


