Abstract
Sudden cardiac death in athletes is a recurrent phenomenon at sporting events and during training. Recent studies have associated sudden cardiac death with such cardiovascular conditions as coronary artery anomalies, cardiomyopathies, and electrocardiographic abnormalities, most of which are screenable with modern imaging techniques. We recently inaugurated the Center for Coronary Artery Anomalies at the Texas Heart Institute, which is dedicated to preventing sudden cardiac death in the young and investigating coronary artery anomalies. There, we are conducting 2 cross-sectional studies intended to firmly establish and quantify, in a large group of individuals from a general population, risk factors for sudden cardiac death that arise from specific cardiovascular conditions.
In a pilot screening study, we are using a brief, focused clinical questionnaire, electrocardiography, and a simplified novel cardiovascular magnetic resonance screening protocol in approximately 10,000 unselected 11- to 15-year-old children. Concurrently, we are prospectively studying the prevalence of these same conditions, their severity, and their relation to exercise and mode of death in approximately 6,500 consecutive necropsy cases referred to a large forensic center. Eventually, we hope to use our findings to develop a more efficient method of preventing sudden cardiac death in athletes. We believe that these studies will help quantify sudden cardiac death risk factors and the relevance of associated physical activities—crucial information in evaluating the feasibility and affordability of cardiovascular magnetic resonance-based screening. We discuss the rationale for and methods of this long-term endeavor, in advance of reporting the results.
Key words: Adolescent; adult; arrhythmias, cardiac/complications; coronary vessel anomalies/complications; death, sudden, cardiac/etiology/prevention & control; guidelines as topic; heart defects, congenital/diagnosis; magnetic resonance angiography; mass screening/standards; practice guidelines as topic; preventive medicine; sports medicine
In general, the sudden death of a young athlete is not easily explained by medical experts.1–3 Although exercise is beneficial to most people as a way to augment and maintain health, physical capacity, and longevity, it can increase the risk of sudden cardiac death (SCD) in individuals who carry silent cardiac defects.1 In addition, the well-documented occurrence of SCD during the training of military recruits poses urgent questions.4
The recurrent reports of SCD in sporting arenas emphasize the need not only for a better understanding of the pathophysiologic mechanisms involved, but for more effective policies designed to prevent SCD.2,5–7 This is especially true because the mortality rate remains frustratingly high (70%–95%) for both athletes and nonathletes who have a sudden cardiac arrest outside the hospital.2,8–11 Currently, the recommended preparticipation process for schoolchildren in the United States who want to participate in sports is facultative and involves an outpatient visit with a non-specialist physician or nurse.6,7
We describe the rationale for, and the methods of, our new efforts in this field at the Texas Heart Institute. Because these investigations are ongoing, no results are available for reporting at this time.
Background
The prevailing opinion about SCD prevention is summarized in the following statements from the literature:
In 1992, the American Armed Forces Institute of Pathology published a review of its institutional forensic experience12 in which appeared the clinical history and the pathologic necropsy findings of 242 patients found to have isolated coronary anomalies. The authors concluded that the cause of death was cardiac in 59% of these cases and was exercise-related in 44%.
Eckart and colleagues4 reported their 25-year examination of the causes of SCD in 64 of 6,300,000 recruits (mean age, 18 yr) during 2-month boot-camp training periods. Of the 64 SCDs, 36% were associated with cardiomyopathies and 33% with coronary anomalies. Incidentally, for the first time in the literature, the authors implied (and later confirmed: R.E. Eckart, MD, personal communication, 2009) that anomalous origin of the left coronary artery from the right sinus of Valsalva with an ante-aortic and intramural course was the only lethal coronary artery anomaly (CAA) represented in this population. Of note, Eckart and colleagues13 later reported a lower relative incidence of CAA-related death (8.5% vs 33%) in a series of military personnel aged 35 years or younger, compared with 0.3% in personnel who were older than 35 years.
The American College of Cardiology and the American Heart Association's guidelines for the precertification of athletes state that most SCDs in young athletes are associated with structural heart disease,7 which implies that most causes of SCD can be recognized by screening via cardiovascular magnetic resonance (CMR) or other accurate methods. Only about 3% of the victims of SCD were believed to have structurally normal hearts.7
A report from the Minneapolis Heart Institute14 on its extensive and systematic electronic search—conducted mainly in local newspapers during a period of about 27 years—concluded that “out of all of the U.S. athletes” 12 to 39 years of age, 690 had SCD. Of these, 36% of cases were due to hypertrophic cardiomyopathy (HCM) and 17% to CAAs. Of the culprit CAAs, 19% were reported to be myocardial bridges (although the mechanism by which bridges caused SCD was not described), whereas 54% were instances of anomalous left main coronary artery arising from the right sinus (with an intramural ante-aortic course, presumably), and 13% were instances in which the right coronary artery had its origin at the left sinus. In 30% of the SCD victims who underwent autopsy in this series, no anatomic cause of death could be identified. In addition, SCD occurred before the age of 17 years in 65% of the group and was exercise-related in 82% of the reviewed cases.
Recent reviews of studies regarding the accuracy of methods for imaging CAA concluded that multislice computed tomographic angiography and magnetic resonance angiography of the coronary arteries can accurately identify almost all CAAs that have an ectopic origin and follow an intramural course (that is, the ante-aortic, potentially lethal category).15–18 In contrast, echocardiography was substantially less precise, especially for detecting anomalous right coronary artery from the opposite sinus (R-ACAOS) in adults, among whom the anomaly was found only in about 10% of the expected (general) population,18–21 as established by prevalence data from continuous series of patients who had undergone coronary angiography.22
The popularization of coronary angiography during the last few decades has inspired several retrospective studies of the prevalence of CAAs.22–24 These studies showed that coronary angiography is an accurate method of diagnosing CAAs (for which coronary angiography has received its “gold standard” status). Prospective, dedicated studies have shown that the total prevalence of CAAs identified in the catheterization laboratory is 6%,22 but only 1% of patients with CAA were found to have potentially lethal ectopic coronary arteries, which typically feature an intramural, ante-aortic course.25 We should acknowledge that persons with these catheterization findings tend to be patients in whom significant coronary disease is suspected, and not a random sample of the general population; this introduces a potentially significant bias regarding the applicability of such prevalence data to a general population.
-
Hypertrophic cardiomyopathies, whose traditional definition in adults includes a left ventricular (LV) wall (either free wall or ventricular septum) thickness greater than 1.5 cm,18,26–28 are considered to be present in 0.2% of the general population.26,27 If we were to include in this category HCM associated with a wall thickness of 1.2 through 1.5 cm (a condition called borderline cardiomyopathy, because the upper limit of the normal range of ventricular thickness is considered to be 1.1 cm),26 the prevalence of HCM would be approximately 0.5% of the general population. In 2003 and 2006, important pediatric age data were published regarding the assumed prevalence of dilative cardiomyopathy; these data had been drawn from patients referred to local pediatric cardiology centers for symptoms of heart failure.29,30 The reported incidence of “new cases” of dilative cardiomyopathy in persons 0 to 18 years of age was reported in terms of number per year in an assumed population of 100,000.
The generic definition of HCM in pediatric populations used to be expressed in terms of a wall thickness “2 standard deviations above the normal mean for age, or body mass area.”29,30 In our own CMR study of children 11 to 15 years of age, the specific ranges of normal wall thickness or mass have not yet been established—this is a fundamental aim of our endeavor. One of our objectives is to report the prevalence of anatomically defined cardiomyopathies in a general population (starting with the assumption that the guideline of 2 standard deviations above the mean applies also to our clinical study of the risk of SCD in HCM). We also want to compare the SCD rate in young athletes with that in sedentary young individuals (that is, persons aged 12–35 yr, a commonly used age grouping1,6). For dilative cardiomyopathies, as for HCM, the prevalence is probably also about 0.5%, if myocarditis-related cases are included.3,4,13,14 We expect to be able to validate also the cardiac magnetic resonance data by comparing them with normal ranges of LV anatomy derived from autopsy data (from people who died of noncardiac causes at the same age).
Pre-excitation syndromes, channelopathies, and right ventricular dysplasia—potentially recognizable at routine electrocardiographic (ECG) screening—are probably present in about 0.3% of the general population.31–33
Therefore, at present, it is probably reasonable to assume that 2% to 3% of the general population has cardiovascular conditions (mainly CAA, cardiomyopathies, and channelopathies) that seem to pose a high risk to competitive sportspersons. Considering that the young population constitutes approximately 28% of the total United States population, or about 90 million, the 2% to 3% would correspond to about 2 million people. If we consider only the estimated 1.5 to 10 million “young athletes” in the U.S. (usually defined as “regular runners”) in any given year, 30,000 to 300,000 of them would be expected to carry high-risk cardiovascular conditions (hr-CVCs). Preliminary estimates suggest that 0.1 to 0.6 per 100,000 young people die suddenly of cardiac causes each year, whereas 2 to 7 per 100,000 U.S. athletes die in that manner.1,3,7,10,34
All such estimates are preliminary, mainly because of the methodological limitations of the currently available studies. All of the studies that label CAAs as hr-CVCs lack a clear, specific definition that explains which individual coronary anomalies are capable of causing SCD.35–37 In 2007, we proposed that the acronym ACAOS (anomalous coronary artery origin from the opposite sinus, with an intramural course) be used to refer to types of CAA that have a clear mechanism of ostial obstruction and, hence, a potential to cause myocardial ischemia and possibly SCD.25 Extremely rare conditions capable of causing SCD, such as ostial coronary congenital stenosis or atresia and clotting or rupture of a coronary fistula (but not all cases of coronary fistula), would also be considered potential causes of SCD. These disorders can be excluded from analysis in our current population-based studies, because they are too rare: they occur in less than 1 in 100,000 persons in the general population.37 In contrast, tunneled coronary arteries or myocardial bridges are a typical confounding entity that established guidelines frequently include in the list of causes of SCD in athletes.7,31 Although myocardial bridges are known to alter the coronary blood flow pattern, only exceptional myocardial bridges—probably those accompanied by severe spasticity or clot-complicated occlusions—have recently come to be considered as possible causes of severe ischemia, infarction, and SCD.38
Using autopsy results to study the incidence of SCD due to CAA can also be problematic. A typical question in such a scenario is this: Does the mere presence of a CAA in a patient who dies suddenly constitute sufficient evidence for one to conclude that the SCD was due to the CAA? For example, approximately 1% of the general worldwide population seems to be born with ACAOS. In the autopsy of carriers of ACAOS, if all deaths without another plausible cause were attributed to ACAOS, the mortality rate for this condition would be overestimated. “Premature” CAA-related death remains a poorly supported notion that the relationship between SCD and exercise explains only in part.38,39
Investigators have long struggled with the issue of subclassifying individual cases of ACAOS by their severity, but no widely accepted consensus is available.24 To date, neither anatomic description of severity nor the finding of myocardial scarring in the dependent territory has resulted in meaningful markers of clinical severity (or likely causes of SCD).38,39 The fundamental issues of “numerator” (the prevalence of SCD in young carriers of high-risk conditions) and “denominator” (the prevalence of hr-CVC in a general population that either survives to age 35 or dies of noncardiac causes) have come to be viewed as the critical points (Fig. 1) in the debate about what constitutes “high risk” and about the need for and value of screening (cost-efficiency and affordability).
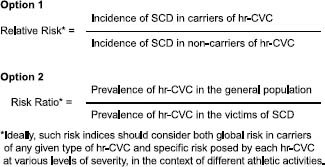
Fig. 1 Possible approaches to quantifying the risk, in the young, of sudden cardiac death (SCD) in association with a given existing high-risk cardiovascular condition (hr-CVC).
In order to properly evaluate the risk associated with pre-existing conditions in a young population, it seems appropriate to first describe several factors in an unselected sample from the general population (Table I). The following values should be among those collected:
TABLE I. Staged Model of Sudden Cardiac Death in the Young
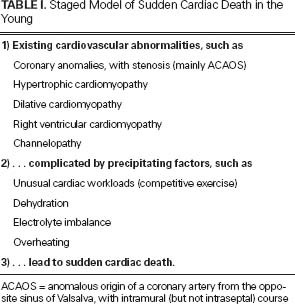
The general prevalence (number of carriers) of each type of hr-CVC;
The severity of each condition, in individual cases. For example, adult cases of HCM can be classified as those with a wall thickness of 1.2 to 1.5 (borderline HCM) versus more than 1.5 cm (HCM). In our population, we will adopt the newly discovered normal range (mean plus double the SD) among children 11 to 15 years of age;
The nature and intensity of the precipitating factors (for example, exercise load, competitive setting, dehydration, or evidence of heat stroke); and
The incidence of SCD in the presence and absence of hr-CVC, as determined by a general-population necropsy survey (Table I and Fig. 1).
Problems with the Status Quo
In a 2007 review,6 Glover and colleagues reiterated their conclusion that SCD “in young trained athletes is a tragic but ultimately low event-rate phenomenon, unlikely to be extinguished by preparticipation screening regardless of the particular strategy used.”
Similar statements have been recurrent in the medical and nonmedical literature,2,40 even though many young athletes die suddenly, on and off the sporting fields, of potentially preventable causes. Is it really impossible or prohibitively expensive to develop a more effective policy and a safer environment for a population that is encouraged to exercise and is applauded for excelling in sports? Today, routine ECG screening is neither the only nor the most accurate option.
Subjects and Methods of 2 Novel Ongoing Studies
We have recently created the Center for Coronary Artery Anomalies, a section of the Texas Heart Institute, with the intention of promoting life-saving research and, eventually, preventive services in the field of sports medicine. We are currently carrying out 2 initial cross-sectional studies that we believe could critically improve our ability to screen young people and more effectively prevent SCD in the young, especially in athletes. We hope that such studies will help medical organizations and society as a whole to recognize that the time is ripe for adopting novel, effective, and affordable preventive medicine in the sports field.
These two studies have been designed—and are concurrently being carried out—in order to fully ascertain the prevalence of hr-CVCs and their mortality implications: the Cardiac Screening MRI (S-MRI) Study, which involves the screening of an unselected cohort of approximately 10,000 middle-school students (ages, 11–15 yr); and the Necropsy Study, which involves a prospective series of approximately 6,500 consecutive necropsies performed at the Harris County Institute of Forensic Sciences (Houston).
Cardiac Screening MRI Study
The purpose of the S-MRI study is to perform, in a general population, an accurate survey of the prevalence of anatomo-functional conditions that have been considered to confer a high risk of cardiovascular death in the young, especially in athletes. The study also includes a brief, focused medical questionnaire and an ECG. The use of the S-MRI protocol, the study design, and the sample size are intended to give our screening study the following features:
Approximately 10,000 schoolchildren will be screened, primarily to enable us to establish definitive prevalence data in multiple subgroups, broken down by body weight/height, ethnicity, race, and sex. We expect the study cohort to be large enough to yield accurate prevalence data regarding at least the most common hr-CVCs, but we recognize that other, less common hr-CVCs might not be adequately represented in our population sample. In addition, in order to optimally avoid pretest bias, screening will be carried out in any assenting children (with consenting parents) 11 to 15 years of age. A recognized drawback of screening children in this age range is that cardiomyopathies tend, phenotypically, to express themselves more fully at later ages.26,27 Therefore, we must acknowledge the possibility that our study will require a second stage in which participants are screened again at an older age. Although this would be an even greater undertaking, it is worth considering, because it would provide an opportunity to refine diagnostic criteria at an early age, potentially enabling us to predict the further evolution of ACAOS, HCM, and dilative cardiomyopathy.
The subjects will be boys and girls of different ethnic and racial backgrounds. Because there is no cost to the candidates or their schools, participation will not be tied to the candidates' socioeconomic status.
Our novel CMR cardiac-screening protocol is currently being performed on an outpatient basis in mobile CMR units without the need for sedation, intravenous access, or contrast administration. We have chosen a protocol for S-MRI screening that involves about 15 minutes of limited, mostly free-breathing, focused data acquisition; the screening is specifically designed to rule out the presence of ACAOS and cardiomyopathies. Specific images include an ECG-gated 3-dimensional gradient echo magnetic resonance angiogram covering the entire aortic root, which is obtained to visualize the origins of the coronary arteries and the locations of the proximal trunks; and the sections of the ventricles (4-chamber, LV outflow tract, and 2-chamber) by which fundamental measurements can be made, such as atrial and ventricular chamber size, segmental wall thickness, LV mass, stroke volume, and cardiac output (Figs. 2 and 3).41,42
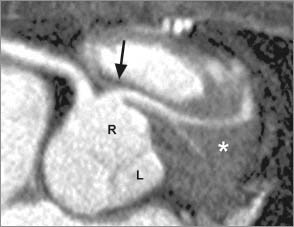
Fig. 2 Cardiovascular magnetic resonance at screening shows a typical coronary artery image in a case of anomalous origin of the left coronary artery from the right sinus of Valsalva, with an intraseptal course (asterisk). Note that the origin of the coronary artery is quite visible, in proximal 2.5- to 3.5-cm segments, including topographic context. The arrow indicates the left main trunk.
L = left sinus of Valsalva; R = right sinus of Valsalva
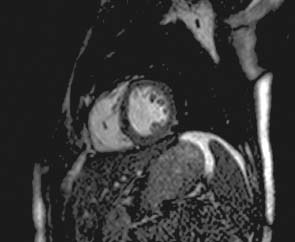
Fig. 3 Typical cross-sectional cardiovascular magnetic resonance image, at the level of the mid-left ventricle in a normal heart, shows clear imaging of the ventricular wall thickness, the papillary muscles, and trabeculations at end-diastole.
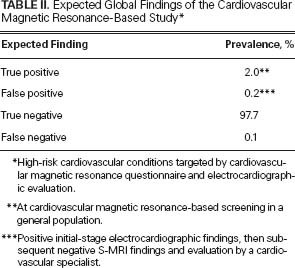
Coronary magnetic resonance angiography is highly reliable for the diagnosis of ACAOS (its ectopic origin and its tangential proximal course30 are suggested in Fig. 2), and it is also quite precise in determining left and right ventricular dimensions and wall thicknesses (see the expected results in Table II).31 When it has an ante-aortic course, ACAOS is always accompanied by an intramural aortic course, as shown in our ongoing extensive study of ACAOS by intravascular coronary ultrasonography.25 The S-MRI protocol41,43 also enables the accurate evaluation of dilative and hypertrophic cardiomyopathies, although it is unlikely that this abbreviated CMR protocol will be able to identify most cases of arrhythmogenic right ventricular dysplasia; in the initial stage of screening, we will rely on ECG and a clinical questionnaire to detect most cases of this rare disorder.32–34 For accuracy in describing coronary anatomy, our protocol seems to be limited only by arrhythmias and patient motion, factors that do not seem to interfere significantly with data acquisition in our targeted age bracket.41,42
TABLE II. Expected Global Findings of the Cardiovascular Magnetic Resonance-Based Study*
Cardiac S-MRI avoids the use of ionizing radiation, unlike multislice computed tomography. Even when used clinically, routine cardiac MR (which involves a much more extensive and time-consuming protocol than does S-MRI) has not caused significant long-term ill effects, despite the millions of scans performed to date.42
Under ideal conditions (under which we use low-overhead, dedicated providers), the cost of performing such a CMR study is calculated to be in the range of U.S. $100 to $500 per case, depending on different overhead and operating policies (data on file, Center for Coronary Artery Anomalies, Houston). These figures include only the direct costs to the provider (lease of new equipment, personnel in the field, non-reusable materials); at this time (when our operation is exclusively dedicated to conducting a preliminary free screening study in a school district), costs cannot include institutional overhead. The cost-effectiveness and, ultimately, the affordability of using a similar screening protocol for preparticipation in specific populations will have to be determined from the prevalence of carriers and the prevalence of SCD in athlete and nonathlete populations, as well as from long-term follow-up data collected after the protocol has been instituted.
In a second-stage, 5-year follow-up study, our CMR screening protocol will be compared with existing preparticipation protocols in terms of cost-effectiveness in preventing SCD. It is expected that the planned CMR-based screening will prove so effective in ruling out hr-CVCs for SCD in young athletes that the currently indicated medical visit to rule out cardiovascular conditions (with follow-up testing for unclear or abnormal initial findings, by use of improvised protocols) could be withheld, resulting in substantial economic savings at this stage of testing (probably comparable to the cost of a routine S-MRI). In our protocol, evaluation by a subspecialty cardiologist will be required only for candidates found to have a definite hr-CVC at the first stage of screening.
Echocardiography is a fair alternative for similar enhanced screening: we decided to try CMR specifically because of its superior precision in diagnosing CAAs of origin and noncompaction cardiomyopathy (an entity that is persistently unclear at its asymptomatic stage, if systolic LV function is preserved). In particular, the confusing nature of ECG findings in many young people (especially findings related to ventricular hypertrophy) has been a fundamental argument in the U.S. for not using ECG for screening purposes.5,32–34 The availability of the concurrent S-MRI data will immediately exclude most false-positive ECG results (which we expect to find in 10%–30% of the screened individuals) and, therefore, eliminate many needless referrals to specialists.
Necropsy Study
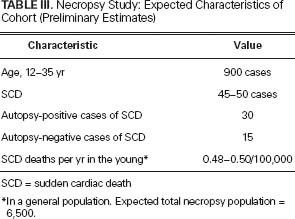
Simultaneous with the CMR-based study, the Necropsy Study aims to re-evaluate the prevalence of the same (CMR-identifiable) hr-CVCs in a consecutive series of cadavers (enabling substudies in cases of SCD vs non-sudden deaths, in younger vs older patients, and in other subgroups of patients) that occur in a large urban area and are studied by autopsy at the Harris County Institute of Forensic Sciences. We estimate that 90% of SCDs that occur in young people in our area will be evaluated by the local forensic center, because SCD usually occurs outside the hospital environment and in persons not previously diagnosed with cardiovascular conditions (see the expected size of the target study cohort in Table III).
TABLE III. Necropsy Study: Expected Characteristics of Cohort (Preliminary Estimates)
This study involves a prospective analysis of data (clinical and necropsy) and is intended to establish differential prevalence data regarding both CAAs and cardiomyopathies in cardiac versus non-cardiac deaths. This study will also test for correlations between the occurrence of SCD in the young and their relevant risk factors, such as sex, age, ethnic background, physical activity at the time of onset of the final event, and athletic versus sedentary habits (Table I).
On the basis of previous necropsy records from the Houston-area population of 4.1 million, we estimate that 6,500 such studies will be performed during the 2-year study period. Of these studies, approximately 900 are expected to be performed on persons who died between the ages of 12 and 35 years. Specific efforts will be made to establish the likely causes and mechanisms of death.9,10,44,45 In addition, histologic evidence of myocardial disarray, scarring, or acute myocardial infarction will be investigated, to evaluate the possibility of scarring in the dependent myocardium, in cases of ACAOS and of HCM.38,39 The severity of both ACAOS and cardiomyopathy will be evaluated by the use of established quantitative macroscopic and microscopic values, which will be measured with novel approaches not used in similar, previous population studies of SCD. Prior necropsy studies regarding the incidence of hr-CVC are few and are generally limited by their retrospective nature and the absence of clear, commonly accepted diagnostic criteria for causes of death.4,15,38,39
Correlation of the Data Obtained from the Two Studies
The final reconciliation of data obtained from CMR-based and necropsy-based studies will introduce specific statistical multifactorial analyses that are crucially important for quantifying the risk of SCD in a general population and in defined subgroups. It is obvious that this is only the start of a long-term commitment to the subject matter. The age data from the CMR study will define the “denominator” (that is, the prevalence of mainly congenital conditions considered to significantly increase the risk of SCD), whereas the autopsy study will provide a substantial population-based estimate of the prevalence of the same conditions at the time of SCD in a similar general population. Eventually, we hope to make possible the formulation of new schemes for mandatory preparticipation screening. The cost-effectiveness of CMR-based screening will to some extent be shaped not only by the accuracy of the screening methods (Fig. 4) but also by the risk of SCD in subgroups with hr-CVC.
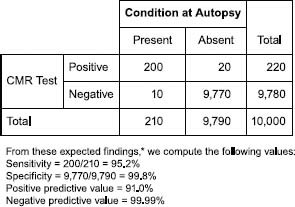
Fig. 4 Calculation of expected sensitivity and specificity in the detection of high-risk cardiovascular conditions (hr-CVCs)* by cardiovascular magnetic resonance (CMR) screening protocol. Correlation of “expected” number of positive CMR findings (abscissa) and “real” positive findings (ordinate) at a theoretical autopsy.
*The hr-CVCs to be screened for are hypertrophic cardiomyopathies, dilative cardiomyopathies, and anomalous coronary artery origin from the opposite sinus (with an intramural course). See text.
Acknowledgment
The authors thank Stephen N. Palmer, PhD, ELS, of the Section of Scientific Publications at the Texas Heart Institute, for expert editing of the manuscript.
Footnotes
Address for reprints: Paolo Angelini, MD, 6624 Fannin St., Suite 2780, Houston, TX 77030
E-mail: PAngelini@leachmancardiology.com
References
- 1.Corrado D, Basso C, Rizzoli G, Schiavon M, Thiene G. Does sports activity enhance the risk of sudden death in adolescents and young adults? J Am Coll Cardiol 2003;42(11):1959–63. [DOI] [PubMed]
- 2.Harrell E. Sudden cardiac death: should young athletes be screened? Time magazine [Internet].
- 3.Maron BJ. Sudden death in young athletes. N Engl J Med 2003;349(11):1064–75. [DOI] [PubMed]
- 4.Eckart RE, Scoville SL, Campbell CL, Shry EA, Stajduhar KC, Potter RN, et al. Sudden death in young adults: a 25-year review of autopsies in military recruits. Ann Intern Med 2004;141(11):829–34. [DOI] [PubMed]
- 5.Chaitman BR. An electrocardiogram should not be included in routine preparticipation screening of young athletes. Circulation 2007;116(22):2610–5. [DOI] [PubMed]
- 6.Glover DW, Glover DW, Maron BJ. Evolution in the process of screening United States high school student-athletes for cardiovascular disease. Am J Cardiol 2007;100(11):1709–12. [DOI] [PubMed]
- 7.Maron BJ, Thompson PD, Ackerman MJ, Balady G, Berger S, Cohen D, et al. Recommendations and considerations related to preparticipation screening for cardiovascular abnormalities in competitive athletes: 2007 update: a scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism: endorsed by the American College of Cardiology Foundation. Circulation 2007;115(12):1643–55. [DOI] [PubMed]
- 8.Atkins DL, Everson-Stewart S, Sears GK, Daya M, Osmond MH, Warden CR, et al. Epidemiology and outcomes from out-of-hospital cardiac arrest in children: the Resuscitation Outcomes Consortium Epistry-Cardiac Arrest. Circulation 2009;119(11):1484–91. [DOI] [PMC free article] [PubMed]
- 9.Donoghue AJ, Nadkarni V, Berg RA, Osmond MH, Wells G, Nesbitt L, et al. Out-of-hospital pediatric cardiac arrest: an epidemiologic review and assessment of current knowledge. Ann Emerg Med 2005;46(6):512–22. [DOI] [PubMed]
- 10.Lotfi K, White L, Rea T, Cobb L, Copass M, Yin L, et al. Cardiac arrest in schools. Circulation 2007;116(12):1374–9. [DOI] [PubMed]
- 11.SOS-KANTO study group. Cardiopulmonary resuscitation by bystanders with chest compression only (SOS-KANTO): an observational study. Lancet 2007;369(9565):920–6. [DOI] [PubMed]
- 12.Taylor AJ, Rogan KM, Virmani R. Sudden cardiac death associated with isolated congenital coronary artery anomalies. J Am Coll Cardiol 1992;20(3):640–7. [DOI] [PubMed]
- 13.Eckart RE, Shry EA, Burke AP, McNear JA, Appel DA, Castillo-Rojas LM, et al. Sudden death in young adults: an autopsy-based series of a population undergoing active surveillance. J Am Coll Cardiol 2011;58(12):1254–61. [DOI] [PubMed]
- 14.Maron BJ, Doerer JJ, Haas TS, Tierney DM, Mueller FO. Sudden deaths in young competitive athletes: analysis of 1866 deaths in the United States, 1980–2006. Circulation 2009;119 (8):1085–92. [DOI] [PubMed]
- 15.Budoff MJ, Ahmed V, Gul KM, Mao SS, Gopal A. Coronary anomalies by cardiac computed tomographic angiography. Clin Cardiol 2006;29(11):489–93. [DOI] [PMC free article] [PubMed]
- 16.Kim WY, Danias PG, Stuber M, Flamm SD, Plein S, Nagel E, et al. Coronary magnetic resonance angiography for the detection of coronary stenoses. N Engl J Med 2001;345(26):1863–9. [DOI] [PubMed]
- 17.Prakken NH, Cramer MJ, Olimulder MA, Agostoni P, Mali WP, Velthuis BK. Screening for proximal coronary artery anomalies with 3-dimensional MR coronary angiography. Int J Cardiovasc Imaging 2010;26(6):701–10. [DOI] [PMC free article] [PubMed]
- 18.American College of Cardiology Foundation Task Force on Expert Consensus Documents, Hundley WG, Bluemke DA, Finn JP, Flamm SD, Fogel MA, et al. ACCF/ACR/AHA/NASCI/SCMR 2010 expert consensus document on cardiovascular magnetic resonance: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents. J Am Coll Cardiol 2010;55(23):2614–62. [DOI] [PMC free article] [PubMed]
- 19.Davis JA, Cecchin F, Jones TK, Portman MA. Major coronary artery anomalies in a pediatric population: incidence and clinical importance. J Am Coll Cardiol 2001;37(2):593–7. [DOI] [PubMed]
- 20.Frommelt PC, Frommelt MA, Tweddell JS, Jaquiss RD. Prospective echocardiographic diagnosis and surgical repair of anomalous origin of a coronary artery from the opposite sinus with an interarterial course. J Am Coll Cardiol 2003;42(1): 148–54. [DOI] [PubMed]
- 21.Pelliccia A, Spataro A, Maron BJ. Prospective echocardiographic screening for coronary artery anomalies in 1,360 elite competitive athletes. Am J Cardiol 1993;72(12):978–9. [DOI] [PubMed]
- 22.Angelini P, Villason S, Chan AV Jr, Diez JG. Normal and anomalous coronary arteries in humans. In: Angelini P, editor. Coronary artery anomalies: a comprehensive approach. Baltimore: Lippincott Williams & Wilkins; 1999. p. 27–150.
- 23.Yamanaka O, Hobbs RE. Coronary artery anomalies in 126,595 patients undergoing coronary arteriography. Cathet Cardiovasc Diagn 1990;21(1):28–40. [DOI] [PubMed]
- 24.Click RL, Holmes DR Jr, Vlietstra RE, Kosinski AS, Kronmal RA. Anomalous coronary arteries: location, degree of atherosclerosis and effect on survival–a report from the Coronary Artery Surgery Study. J Am Coll Cardiol 1989;13(3):531–7. [DOI] [PubMed]
- 25.Angelini P, Flamm SD. Newer concepts for imaging anomalous aortic origin of the coronary arteries in adults. Catheter Cardiovasc Interv 2007;69(7):942–54. [DOI] [PubMed]
- 26.Klues HG, Schiffers A, Maron BJ. Phenotypic spectrum and patterns of left ventricular hypertrophy in hypertrophic cardiomyopathy: morphologic observations and significance as assessed by two-dimensional echocardiography in 600 patients. J Am Coll Cardiol 1995;26(7):1699–708. [DOI] [PubMed]
- 27.Maron BJ, Maron MS, Wigle ED, Braunwald E. The 50-year history, controversy, and clinical implications of left ventricular outflow tract obstruction in hypertrophic cardiomyopathy from idiopathic hypertrophic subaortic stenosis to hypertrophic cardiomyopathy: from idiopathic hypertrophic subaortic stenosis to hypertrophic cardiomyopathy. J Am Coll Cardiol 2009;54(3):191–200. [DOI] [PubMed]
- 28.Rickers C, Wilke NM, Jerosch-Herold M, Casey SA, Panse P, Panse N, et al. Utility of cardiac magnetic resonance imaging in the diagnosis of hypertrophic cardiomyopathy. Circulation 2005;112(6):855–61. [DOI] [PubMed]
- 29.Towbin JA, Lowe AM, Colan SD, Sleeper LA, Orav EJ, Clunie S, et al. Incidence, causes, and outcomes of dilated cardiomyopathy in children. JAMA 2006;296(15):1867–76. [DOI] [PubMed]
- 30.Nugent AW, Daubeney PE, Chondros P, Carlin JB, Cheung M, Wilkinson LC, et al. The epidemiology of childhood cardiomyopathy in Australia. N Engl J Med 2003;348(17):1639–46. [DOI] [PubMed]
- 31.Corrado D, Basso C, Pavei A, Michieli P, Schiavon M, Thiene G. Trends in sudden cardiovascular death in young competitive athletes after implementation of a preparticipation screening program. JAMA 2006;296(13):1593–601. [DOI] [PubMed]
- 32.Corrado D, Pelliccia A, Heidbuchel H, Sharma S, Link M, Basso C, et al. Recommendations for interpretation of 12-lead electrocardiogram in the athlete. Eur Heart J 2010;31(2):243–59. [DOI] [PubMed]
- 33.Steinvil A, Chundadze T, Zeltser D, Rogowski O, Halkin A, Galily Y, et al. Mandatory electrocardiographic screening of athletes to reduce their risk for sudden death: proven fact or wishful thinking? J Am Coll Cardiol 2011;57(11):1291–6. [DOI] [PubMed]
- 34.Maron BJ, Thompson PD, Puffer JC, McGrew CA, Strong WB, Douglas PS, et al. Cardiovascular preparticipation screening of competitive athletes. A statement for health professionals from the Sudden Death Committee (clinical cardiology) and Congenital Cardiac Defects Committee (cardiovascular disease in the young), American Heart Association. Circulation 1996;94(4):850–6. [DOI] [PubMed]
- 35.Angelini P. Coronary artery anomalies: an entity in search of an identity. Circulation 2007;115(10):1296–305. [DOI] [PubMed]
- 36.Angelini P. Coronary artery anomalies and sports activities. In: Lawless CE, editor. Sports cardiology essentials: evaluation, management and case studies. New York: Springer; 2011. p. 277–98.
- 37.Angelini P, Velasco JA, Flamm S. Coronary anomalies: incidence, pathophysiology, and clinical relevance. Circulation 2002;105(20):2449–54. [DOI] [PubMed]
- 38.Basso C, Maron BJ, Corrado D, Thiene G. Clinical profile of congenital coronary artery anomalies with origin from the wrong aortic sinus leading to sudden death in young competitive athletes. J Am Coll Cardiol 2000;35(6):1493–501. [DOI] [PubMed]
- 39.Frescura C, Basso C, Thiene G, Corrado D, Pennelli T, Angelini A, Daliento L. Anomalous origin of coronary arteries and risk of sudden death: a study based on an autopsy population of congenital heart disease. Hum Pathol 1998;29(7):689–95. [DOI] [PubMed]
- 40.Thompson PD, Levine BD. Protecting athletes from sudden cardiac death. JAMA 2006;296(13):1648–50. [DOI] [PubMed]
- 41.Pednekar AS, Muthupillai R, Cheong B, Flamm SD. Automatic computation of left ventricular ejection fraction from spatiotemporal information in cine-SSFP cardiac MR images. J Magn Reson Imaging 2008;28(1):39–50. [DOI] [PubMed]
- 42.Pennell DJ. Cardiovascular magnetic resonance. Circulation 2010;121(5):692–705. [DOI] [PubMed]
- 43.Su JT, Chung T, Muthupillai R, Pignatelli RH, Kung GC, Diaz LK, et al. Usefulness of real-time navigator magnetic resonance imaging for evaluating coronary artery origins in pediatric patients. Am J Cardiol 2005;95(5):679–82. [DOI] [PubMed]
- 44.Bardai A, Berdowski J, van der Werf C, Blom MT, Ceelen M, van Langen IM, et al. Incidence, causes, and outcomes of out-of-hospital cardiac arrest in children. A comprehensive, prospective, population-based study in the Netherlands. J Am Coll Cardiol 2011;57(18):1822–8. [DOI] [PubMed]
- 45.Winkel BG, Holst AG, Theilade J, Kristensen IB, Thomsen JL, Ottesen GL, et al. Nationwide study of sudden cardiac death in persons aged 1–35 years. Eur Heart J 2011;32(8):983–90. [DOI] [PubMed]


