Abstract
Patients over age 60 comprise the majority of those diagnosed with acute myeloid leukemia (AML), but treatment approaches in this population are variable, with many uncertainties and controversies. Our group conducted a literature review to summarize the latest information and to develop a consensus document with practical treatment recommendations. We addressed five key questions: selection criteria for patients to receive intensive induction chemotherapy; optimal induction and post-remission regimens; allogeneic hematopoietic stem cell transplantation (HSCT); treatment of patients not suitable for induction chemotherapy; and treatment of patients with prior hematological disorders or therapy-related AML. Relevant literature was identified through a PubMed search of publications from 1991 to 2012. Key findings included the recognition that cytogenetics and molecular markers are major biologic determinants of treatment outcomes in the older population, both during induction therapy and following HSCT. Although disease-specific and patient-specific risk factors for poor outcomes are more common in the older population, age is not in itself sufficient grounds for withholding established treatments, including induction and consolidation chemotherapy. The role of HSCT and use of hypomethylating agents are discussed. Finally, suggested treatment algorithms are outlined, based on these recommendations.
Keywords: Acute myeloid leukemia, chemotherapy, cytogenetics, prognosis, hematopoietic stem cell transplantation, hypomethylating agent
Introduction
Treatment of older patients with acute myeloid leukemia (AML) has been hampered by uncertainties. Patients over age 60, who make up more than 50% of the AML population [1], have different biological and clinical features compared to younger patients [2,3]. Older patients are more likely to have cytogenetic abnormalities associated with poorer outcomes [2,4-13], a history of antecedent hematological disorder (AHD) [14] and co-morbidities or poor performance status that can limit treatment options and lead to reduced dose intensity [2]. For these reasons, there is considerable variability in how older patients are treated, specifically with respect to intensive induction chemotherapy, post-remission therapy, and hematopoietic stem cell transplantation (HSCT). The advent of newer therapies, such as hypomethylating agents, has led to further uncertainty about which treatment to offer to different subsets of patients.
In order to clarify some of these issues, a panel of ten Canadian hematologists specializing in AML undertook a review of the literature on AML in older patients. Five key clinical questions were addressed, and recommendations were formulated for each, based on the best available evidence and clinical judgment. Finally, a series of treatment algorithms was created, based on these recommendations.
Methods
A committee of ten leukemia experts from across Canada worked on the guidelines. The committee determined the five relevant questions, and then worked in pairs to review and evaluate the relevant literature relating to each question. Initially, a PubMed search of English-language clinical trials and meta-analyses published from 1991 to 2011 was conducted to ensure that all relevant studies were included. Case reports were excluded, as were pilot studies, studies using < 30 patients, phase I studies, economic analyses and quality-of-life studies. The authors then added supplemental literature as required, and provided further insights based on personal and institutional experience and judgment. No formal evaluation of evidence was conducted. The five groups then developed written working outlines and drafted treatment recommendations for each question. These were subsequently combined into a consensus document, which was modified and approved by the Chair (JMB). Panel members subsequently met as a group and agreed on the treatment recommendations for each of the five clinical questions. Dissenting opinions were to be noted in the final document.
Results
Question # 1: What are the major criteria to determine who is a suitable candidate for intensive induction chemotherapy?
Influence of age
Controversy persists over the upper age appropriate for intensive induction therapy [5]. Many studies have shown increasing age to be associated with a worse prognosis [6-8,14], but the influence of performance status, co-morbidities and disease biology on these outcomes has been unclear, as these factors also worsen with increasing age. Recent evidence suggests that these factors are more important than age per se [5,7,14]. One retrospective study of 291 newly diagnosed AML patients receiving induction therapy compared patients aged 60-69 to those aged 70-82 [5,9]. Patients were selected for intensive treatment on the basis of overall fitness, as determined by the treating physician, and patient preference after discussion with the physician. Patients ≥ age 70 were less likely to receive induction therapy; however, among those who received induction, no significant differences were noted in terms of complete remission (CR) rate, early death (ED) or overall survival (OS) [5,9]. A number of other recent studies support the observation that comorbidities, performance status and disease biology are more important determinants of treatment outcome than age [15-17]. These studies suggest that, if patients are pre-selected based on medical fitness and favorable disease biology, age per se is not a factor in determining suitability for induction chemotherapy. However, few patients over age 80 would meet such criteria, and some studies have indicated that patients in this age group have much higher early mortality and inferior survival with induction therapy [15,18].
Complete remission (CR) achievement and duration predict survival
Achievement of CR has been considered a prerequisite for improving survival using chemotherapy [10] and thus has provided a standard point from which to compare outcomes and determine prognostic factors. Success in achieving CR with induction chemotherapy depends on both the anti-leukemic efficacy of the therapy and the patient’s ability to tolerate it [11]. However, OS also depends on the duration of CR, as a brief CR duration produces only limited survival benefit.
Cytogenetic abnormalities as predictors of CR and survival
A number of studies, including some in the elderly, have clearly identified cytogenetics as the most powerful disease biology-related predictor of response and survival using standard induction chemotherapy. AML patients have been stratified into risk categories based on major cytogenetic scoring systems, particularly the Medical Research Council (MRC) [9,12,19] and Eastern Cooperative Oncology Group (ECOG) [20,21] classifications. Although slight differences exist, both systems have identified three major cytogenetic risk categories: favorable, intermediate and adverse. While the relative incidence of adverse cytogenetic risk profiles increases with age [8,9,12-14], the effect of specific cytogenetic abnormalities on clinical outcomes is independent of age. In addition, an extremely high-risk category has been identified, based on the presence of multiple monosomies [22-24]. Reported CR and survival rates associated with each of these categories are shown in Table 1.
Table 1.
Cytogenetic/molecular risk categories and clinical outcomes
| Cytogenetic risk category | Karyotype | Complete remission | Overall survival | References |
|---|---|---|---|---|
| Favorable | t(15;17), t(8;21), inv(16) | 75-88% | 3-yr 38% | [8,19,32,117,118] |
| -OR- | 5-yr 17-38% | |||
| Normal karyotype with NPM1 mut/FLT3 wt | 68-83% | 3-yr 29-33% | [26,28,32] | |
| 5-yr OS 21% | ||||
| Intermediate | Normal karyotype not associated with favorable molecular markers; cytogenetic abnormalities not included in other groups | 51-63% | 3-yr 18% | [8,19] |
| 5-yr 11-16% | ||||
| Adverse | Complex (3 or more, not including a favorable abnormality), monosomy (especially complete or partial deletion of 5 or 7), inv(3), t(9;22), 11q23 or 17p abnormalities | 26-40% | 3-yr < 5% | [15,18,19,32,117] |
For older patients with adverse-risk cytogenetics, remissions with standard induction chemotherapy are typically brief (3-6 months); median OS is in the range of 6 months [8,9,19], which compares with 3-4 months with supportive care alone [9,25]. Because of this limited efficacy, there is broad consensus in the group that such patients should not be offered induction chemotherapy outside the setting of a clinical trial, unless a stem cell donor is available and there is an intention to proceed rapidly to HSCT.
Older patients with t(8;21), inv(16) and t(15;17) have demonstrated high CR rates and favorable survival and should be offered intensive chemotherapy if their functional status and medical history suggest they will tolerate the procedure [26]. Evidence in younger patients indicates that those with t(8;21) or inv(16) and a corresponding c-kit mutation have a high relapse rate and brief OS [27]. However, the prognostic and practical implications of c-kit mutations are not well studied in older patients.
For patients with intermediate-risk cytogenetics, CR rates are in the 60% range, and median CR duration is around 9 months [8,9]; these patients are also considered suitable for standard induction chemotherapy. However, relapse rates are in excess of 80%, with a correspondingly low 3-5 year OS (see Table 1). These patients should therefore be considered for either HSCT, if they are eligible, or a clinical trial with an intention of prolonging survival.
Some patients present with prominent symptoms and signs due to rapidly progressive, high white cell count (> 100 x 109/L) disease and require immediate induction therapy. In such cases the physician should not wait for cytogenetic results, and induction therapy should be initiated promptly if the patient is otherwise fit for such treatment.
Molecular genetics in patients with intermediate cytogenetic risk
In older patients with AML arising de novo, 45-50% have a normal karyotype, placing the patient in the intermediate cytogenetic risk group [14,15,28]. In this setting, molecular genetic testing can provide useful prognostic information [13,18,19,29]. The presence of a nucleophosmin (NPM1) mutation has been associated with superior outcomes in older patients with normal karyotype. Becker et al [28] found that NPM1 mutation was associated with a higher CR rate (84% vs 48%; P < 0.001), as well as longer disease-free survival (DFS) (P = 0.047; 3-year rates, 23% vs 10%) and OS (P < 0.001; 3-year rates, 35% vs 8%). Another large European study confirmed the favorable impact of NPM1 mutations in older patients [26]. There are conflicting data suggesting that other mutations, such as IDH1/2, may influence prognosis in younger patients with NPM1 mutations [30,31]; corresponding data in older patients are lacking.
In contrast, FLT3-ITD mutations do not seem to affect the CR rate [32], and the influence on OS in older patients has varied among studies [28,32]. The weight of evidence in younger patients clearly indicates that these patients are at high risk for early relapse. However, several studies in older patients undergoing induction therapy have not demonstrated an independent impact of FLT3-ITD mutations on OS [26,33,34]. These patients, as is the case with other intermediate-risk patients, may be offered induction therapy, but with an intention of proceeding to HSCT or as part of a clinical trial. The use of FLT3 inhibitors upfront, either alone or in combination with chemotherapy, is still considered investigational. A CEBPα mutation, particularly when biallelic, has been associated with reduced relapse rates in younger patients [35], but this mutation is less common and has not yet been studied systematically in older patients. Similar to what has recently been observed in younger patients with AML, it is anticipated that in the foreseeable future, refined molecular prognostication will assume a more prominent role in the appropriate management of older patients as well.
Patient-specific co-morbidity factors
Because patients with even moderate degrees of co-morbidity are often excluded from clinical studies, the proportion of older patients who might benefit from intensive induction is unclear. For similar reasons, the prognostic relevance of co-morbidity is difficult to estimate. Nonetheless, physicians must take co-morbidity into account when identifying patients likely to tolerate treatment [6,17].
Prognostic tools developed to predict treatment-related mortality include the Charleston Comorbidity Index (CCI), which has been adapted for use in AML [36], and the Hematopoietic Cell Transplantation Comorbidity Index (HCT-CI). The latter tool, encompassing multiple organ co-morbidities [37], was evaluated retrospectively in 177 elderly patients with AML [38]. An HCT-CI of ≥ 3 was found to correlate with higher induction mortality (29%) and lower median OS [38]. Malfuson et al [39], in a retrospective analysis of 415 patients enrolled in the ALFA-9803 trial, also found that an HCT-CI of ≥ 3 was independently predictive of inferior survival, with a 12-month OS of approximately 11% [39]. A more recent study, using a multicomponent model, found that a number of factors, including performance status, white blood cell count, serum creatinine and albumin, influenced early mortality with induction therapy [17]. Although providing useful guidance in decision making, such indices and models have not yet been validated prospectively in older AML patients.
Relapsed AML
For relapsed patients, the duration of first complete remission (CR-1) is the strongest predictor of the likelihood of responding to re-induction chemotherapy. Patients with CR-1 duration of < 1 year have a low CR-2 rate and inferior survival with re-induction [40,41], and patients with adverse-risk cytogenetics have a CR-2 probability of only 20% [42]. These subgroups derive little benefit with intensive re-induction, particularly in older patients where tolerance of further intensive chemotherapy is poor. Patients ≥ age 60 have lower CR-2 rates compared to younger patients [43]. Older patients with CR-1 duration of ≥ 12 months and an intermediate- or favorable-risk karyotype have a reasonable chance of achieving CR-2 and may be considered for intensive re-induction if they are still medically fit. However, since second remissions are rarely durable, these patients should be considered for HSCT or investigative approaches in CR-2 to try to prevent relapse.
Recommendations
1. Although overall suitability for induction chemotherapy declines with increasing age, age per se should not be the sole determinant of eligibility for induction chemotherapy. Patients > age 70 may be offered induction therapy if they meet the other criteria below.
2. Patients judged to be at high risk of induction mortality, based on the presence of major comorbidities, should be offered non-intensive treatment options. Although co-morbidity indices are helpful in determining suitability for intensive chemotherapy, they have not been validated prospectively in the induction setting and should not replace clinical judgment. Discussion of these risks with the patient and the family are important to guide decision making.
3. For patients deemed medically fit and opting for intensive therapy, cytogenetic results are crucial to assess the potential benefit of such treatment, and should be provided in less than 1 week.
a. Patients with adverse cytogenetic profiles have low CR rates and little OS benefit compared to best supportive care alone. Therefore, in most cases they should not be offered standard induction chemotherapy outside of a clinical trial. An exception would be a potential HSCT candidate, with a suitable donor (see Q3 below), in whom induction therapy may be attempted as a means of subsequently proceeding to transplant.
b. Patients with a favorable cytogenetic profile or a normal karyotype with a favorable molecular profile (e.g., NPM1 mutated/FLT3-ITD negative), should be offered induction chemotherapy with curative intent.
c. Patients with an intermediate cytogenetic profile appear to have an OS benefit with induction therapy, but outcomes are still unsatisfactory because of high relapse rates. These patients may still be offered induction chemotherapy but should also be considered for clinical trials and other post-remission strategies, including HSCT.
d. Patients who are ill due to rapidly progressive, high white cell count disease should have induction therapy initiated immediately, if they are otherwise medically fit, even if cytogenetics results are not yet available, as these patients are at high risk of early death from progressive disease.
4. Molecular data (e.g. NPM1, FLT3, and other mutations) influence relapse rates and survival. However, as CR rates are > 50% in these molecular subgroups, we do not at this time recommend using these data to guide decision-making with respect to which patients to offer induction therapy.
5. For relapsed patients, re-induction therapy may be offered to fit patients with intermediate- or favorable-risk cytogenetics and a CR-1 duration of ≥ 12 months.
6. All older individuals with AML should receive a consultation with a physician with expertise in managing leukemia in older patients. Patients not otherwise suitable for standard therapy, based on the criteria above, should be offered the option of referral to a center that offers clinical trials for such patients.
Question # 2: How should we treat older patients who are considered suitable for induction chemotherapy?
Standard chemotherapy
Standard induction chemotherapy is the so-called 7+3 regimen, consisting of cytarabine (Ara-C) 100-200 mg/m2 by continuous IV infusion for 7 days, plus daunorubicin IV for 3 days. A recent phase III study in older patients demonstrated superiority of 90 mg/m2 over 45 mg/m2, with a higher CR rate, and better OS in subgroups such as patients age 60-65 and those with favorable karyotype [42]. Although there have not been any studies comparing 60 to 90 mg/m2, reported CR rates and OS with 60 mg/m2 in older patients appear comparable to those in the 90 mg/m2 dose in this study [9].
Other anthracyclines and anthracenediones, particularly idarubicin and mitoxantrone, may also be used [21]. Optimal dosing of idarubicin is 12 mg/m2/day x 3 [44] and mitoxantrone 12 mg/m2/day x 3 [21]. In contrast, no benefit was found with higher doses of cytarabine [45], and high-dose cytarabine has been associated with neurologic toxicity in older patients [46].
According to evidence from published clinical trials, the expected CR rate with standard induction chemotherapy is 41-62% in elderly patients, and the risk of early death is 7-16% (Table 2). There is no evidence to show superiority of alternative regimens such as mitoxantrone-etoposide (NOVE) or topotecan-mitoxantrone as first induction [47,48].
Table 2.
Clinical outcomes in five trials comparing induction chemotherapy regimens in older AML patients. Conventional regimens are shown in gray, comparators in white. Note that early death rates are consistently higher than would be expected from data in the literature on younger AML patients

|
ADE = daunorubicin + cytarabine + etoposide; Ara-C = cytarabine; COAP = cylophosphamide, vincristine, cytarabine and prednisolone; d = day; DAT = daunorubicin + cytarabine + thioguanine; DNR = daunorubicin; E = etoposide; IA = idarubicin; hr = hour; MA = mitoxantrone; MAC = mitoxantrone + cytarabine; PSC = P-glycoprotein; q = every; TG = thioguanine.
Although gemtuzumab ozogamicin (GO) as a single agent is not as effective as standard induction therapy [49], it may improve the efficacy of 7+3 induction therapy in some older patients. In a recent phase III clinical trial, older patients up to age 70 received GO in three fractionated doses (3 mg/m2/day on days 1, 4 and 7), in addition to standard 7+3 induction chemotherapy with 60 mg/m2 daunorubicin [50]. GO-treated patients showed improved OS compared to standard induction chemotherapy alone; 2-year event-free survival (EFS) was 15.6% in the standard treatment group, compared to 41.4% in the standard treatment plus GO group (P = 0.0018). The UK NCRI AML16 trial, a similar study using one dose of GO in combination with 7+3 in older patients (aged 51-84) also found an improved relapse-free survival and OS from CR in the GO arm. Patients with secondary AML or adverse-risk cytogenetics did not benefit from the addition of GO [51]. GO is currently not available in North America and some other jurisdictions.
Alternative approaches to first induction
Several alternative agents, including amsacrine, clofarabine and the hypomethylating agents azacitidine and decitabine, may be considered in selected older AML patients with poor performance status or adverse cytogenetics.
Amsacrine is associated with less cardiotoxicity than anthracyclines [52] and has been used in combination with cytarabine as induction therapy for both younger and older patients with AML. Results are comparable to those using daunorubicin [53,54]. Amsacrine represents an alternative to anthracyclines for patients with impaired cardiac function, but it poses a risk of arrhythmia in patients with low serum potassium, low magnesium values and prolonged QTc intervals [52]. Patients’ electrolytes should therefore be corrected prior to treatment.
Clofarabine, a newer-generation nucleoside analog, was administered as a single agent to patients aged ≥ 60 years during induction at 30 mg/m2/day and at 20 mg/m2/day during reinduction/consolidation, to a maximum of six cycles. CR rates in the presence of 1, 2 or 3 poor risk factors at baseline (age, poor performance status, adverse cytogenetics and/or AHD) were 54%, 51% and 48%, respectively. Toxicity was acceptable, and the early death rate was 9.8% [55]. Hence, clofarabine may be a useful alternative for some patients who would not be expected to respond to 7+3 induction and for those in whom anthracycline avoidance is considered desirable because of prior anthracycline use or moderate cardiac impairment [56]. Another study in patients aged ≥ 60 years suggested that the addition of low-dose cytarabine to clofarabine was well tolerated and improved CR rates and EFS compared to a historical group that received clofarabine alone [57]. An ongoing UK trial is comparing clofarabine plus daunorubicin with 7+3 in fit older patients.
Hypomethylating agents
Retrospective data [58] suggest that the use of azacitidine in selected older AML patients may produce OS rates similar to those of patients receiving induction chemotherapy (with median OS 11.2 months with intensive chemotherapy vs. 13.7 months with azacitidine). A similar study from MD Anderson also found similar survival in older AML patients receiving hypomethyating agent therapy, compared to intensive chemotherapy [59]. However, as these analyses were retrospective, the groups may not have been equivalent; in particular, patients with rapidly proliferating disease in practice are more likely to receive intensive chemotherapy rather than hypomethylating agents. There are no prospective phase III data comparing decitabine or azacitidine to standard induction chemotherapy. Thus, there are currently insufficient data to recommend hypomethylating agent therapy over induction chemotherapy in intermediaterisk older AML patients who are otherwise medically fit for intensive therapy.
Primary induction failure
For patients failing 7+3 induction, a second induction using a non-cross-resistant chemotherapy regimen, may be used in intermediateor favorable-risk cytogenetic patients who are still considered candidates for intensive therapy. Re-induction regimens may include mitoxantrone plus etoposide (NOVE) [47]; for more fit patients, adding intermediate-dose cytarabine (MEC or NOVE-HiDAC) may produce higher CR rates [60,61] but with greater toxicity. Clofarabine plus intermediate-dose cytarabine is an alternative re-induction strategy [62]. However, patients with an adverse-risk karyotype have low CR rates with re-induction [62], and these patients should probably be considered for clinical trials or supportive care.
Consolidation after CR
Unless proceeding directly to HSCT, most patients receive consolidation chemotherapy, although the magnitude of its benefit in older patients remains unclear. A variety of post-remission strategies have been employed. There is no evidence from prospective studies that intermediate- or high-dose cytarabine (HiDAC, 0.5-3 g/m2) is superior to conventional dose consolidation chemotherapy in older patients [63,64]. Recently, a retrospective study from Princess Margaret Cancer Centre found a superior DFS in patients over age 60 with intermediate-risk cytogenetics who received 2 consolidation cycles containing HiDAC 1.5 g/m2 over 3 hours x 6 doses plus daunorubicin, compared to 7+3 followed by NOVE [65]. There was no benefit to HiDAC in patients with adverse-risk cytogenetics. However, prospective studies using such a regimen are lacking. The optimal number of post-remission cycles remains unclear, and one cycle may be sufficient [66,67].
Despite this, there is evidence in younger patients, based on retrospective data, that consolidation using repetitive cycles of HiDAC (3 g/m2) is associated with improved DFS [68] and OS [63,69,70] in patients with t(8;21) or inv(16). We therefore believe it is reasonable to utilize this strategy as well in older fit patients with these abnormalities. However, as HiDAC poses a higher risk of cerebellar toxicity in patients over age 60, such patients should receive a reduced HiDAC dosing schedule, e.g. 1-1.5 g/m2 every 12 hours on treatment days 1, 3 and 5 [71].
Data from two French studies suggest that, in older patients, lower-intensity, prolonged consolidation may produce results at least comparable to those of more intensive strategies [72,73]. One study compared conventional consolidation with an outpatient regimen consisting of six less intensive consolidation cycles in 236 patients who achieved CR. Prolonged treatment was preferred to intensive chemotherapy on the basis of significantly greater OS and DFS, as well as lower toxicity [72,73].
For patients judged medically unfit for intensive post-remission therapy following induction, low-dose cytarabine may potentially prolong remission duration, although it probably does not improve long-term survival [74]. Given the high relapse rates associated with older AML patients, novel post-remission strategies are warranted and these patients should be considered for clinical trials, particularly for those who are not candidates for HSCT.
Acute promyelocytic leukemia (APL)
APL is rare in older patients, but has a favorable prognosis if the patient survives the initial treatment period. CR rates are in the 80% to 90% range, and 3 year OS is in the 50% range or higher, even in patients aged 70 and older [75-77]. Consequently, all patients except the very frail should be considered for treatment with curative intent.
The standard induction treatment for APL in patients > age 60 currently consists of all-trans retinoic acid (ATRA) plus an anthracycline, either idarubicin or daunorubicin [75-77]. Fit older patients with high WBC counts should also receive cytarabine [77]. Post-remission therapy usually consists of two cycles of treatment using similar drugs, often followed by maintenance ATRA. However, as older patients are more prone to anthracycline-induced cardiomyopathy, left ventricular function should be closely monitored [76]. Molecular monitoring for PML-RAR transcripts is recommended, as in younger patients. For relapsed patients, arsenic trioxide is the treatment of choice; it is usually well tolerated and may produce long second remissions [78]. Recent studies suggest that arsenic plus ATRA may be as effective as anthracycline-based chemotherapy when given as first-line therapy [79]; it is not yet approved for this indication but may be considered in selected patients in whom anthracyclines or intensive chemotherapy are contraindicated.
Recommendations
1. Older patients who are deemed suitable candidates should receive induction treatment consisting of an anthracycline or anthracenedione for 3 days plus cytarabine at a conventional dose (100-200 mg/m2) for 7 days. Acceptable anthracyclines/anthracenediones include:
a. Daunorubicin 60-90 mg/m2 daily x 3 days.
b. Idarubicin 12 mg/m2 daily x 3.
c. Mitoxantrone 12 mg/m2 daily x 3.
2. For patients with contraindications to anthracyclines (e.g., impaired left ventricular function or extensive prior anthracycline exposure), amsacrine may be substituted. Clofarabine, with or without cytarabine, may also be considered for such patients. Pending new phase III trial data in AML patients, there are insufficient data to recommend hypomethylating agents over standard induction therapy in intermediate-risk AML patients who are medically fit for induction chemotherapy.
3. For patients achieving CR, consolidation chemotherapy is recommended for patients who are still medically fit for such therapy:
a. For patients with t(8;21) or inv(16), modified high-dose cytarabine-based consolidation is recommended, with reduced dosing (e.g., 1-1.5 g/m2 over 2-3 hours x 6 doses), to minimize the risk of central nervous system toxicity.
b. For patients with intermediate-risk cyotgenetics, there are retrospective data supporting the use of modified high-dose cytarabine-based consolidation over conventional-dose therapy. However, in the absence of prospective data, no firm recommendation can be made.
c. In patients with adverse risk cytogenetics, conventional dose consolidation therapy is adequate. There is no evidence that any one consolidation regimen is superior.
d. The optimal number of post-remission cycles in older patients is unclear. There is no evidence that additional cycles beyond the first produce superior outcomes, although this issue has not been adequately evaluated.
e. Alternatives to consolidation include:
i. Proceeding to HSCT without consolidation (see Q3 below).
ii. Low-dose maintenance chemotherapy (e.g., low-dose cytarabine) for patients who are no longer judged medically fit or decline further intensive treatment.
iii. No active treatment or supportive care only for patients who decline or are unfit for any further chemotherapy.
4. For patients aged 60-70, there is recent evidence that adding gemtuzumab in fractionated doses to standard induction therapy results in improved outcomes. It is strongly recommended that this agent be approved for use in induction therapy for these patients.
5. For primary induction failures, a non-cross-resistant regimen (e.g., NOVE +/– modified high-dose cytarabine) is acceptable therapy for patients who are still candidates for intensive therapy.
6. Older patients with APL should receive induction therapy with ATRA, with or without an anthracycline. For relapsed patients, arsenic trioxide therapy is appropriate for re-induction.
7. Given the high relapse rates in most AML subtypes, older patients should be encouraged to enroll in clinical trials using novel induction and post-remission strategies.
Question # 3: Which older patients should be considered for allogeneic stem cell transplantation (HSCT)?
Cytogenetics as an independent prognostic factor
Selecting patients for HSCT depends on weighing the benefits of the procedure relative to the expected outcome with post-remission chemotherapy alone, as well as the relative risks of these options. Given the profoundly invasive nature of HSCT and the poor function of many AML patients, neither the lowest-risk nor the frailest patients should generally be selected for HSCT. The former are excluded because their prognosis with chemotherapy alone is good, the latter because of treatment-related mortality.
Reduced-intensity conditioning in older patients
In younger patients at high risk of relapse, HSCT in CR-1 appears to be superior to other treatments in reducing relapse risk and thus extending survival [80-82]. However, the risk of transplant-related morbidity and mortality increases with age. The introduction of non-myeloablative and reduced-intensity conditioning (RIC)-HSCT has improved the tolerability of transplantation so that it could be applied more broadly in the older AML population. This approach is being evaluated in a prospective, international phase 3 study [83]. Recent retrospective analyses indicate that for medically fit older patients, RIC-HSCT is well tolerated, with acceptable treatment-related mortality [84,85]. Progression free survival (PFS) and OS did not differ significantly between patients in the 60-65 and 65+ age groups, according to one report [84].
Recent evidence indicates that HSCT may improve survival for patients over age 60 when compared to chemotherapy alone [86-88]. Kurosawa et al [87] showed a significantly improved 3-year OS of HSCT vs. no transplant (P = 0.012) in a group of older patients (median age 60). In this study, cytogenetic risk, but not patient age, was significantly associated with RFS and OS in multivariate analysis. Although proper randomized data are lacking in the older population, there is a general consensus in the group that RIC-HSCT may be considered for appropriate candidates up to age 70.
The decision to proceed with HSCT is based on a number of factors: (1) the response to induction chemotherapy, (2) the cytogenetic and molecular genetic risk profile, (3) the patient’s fitness based on co-morbidities and (4) the availability of a suitable human leukocyte antigen (HLA) matched donor.
Response to induction
There is general consensus that the patient must have achieved CR with induction or other therapy. RIC-HSCT for older patients not in remission are associated with prohibitively high failure rates [89] and should not be undertaken outside of a clinical trial. For patients with relapsed disease, HSCT may be considered for those who achieve CR-2 with re-induction therapy. Gyurkocza et al recently documented 5-year OS of 34% in a group of 71 older patients in CR-2. However, these authors noted that the risk of relapse was 2.5 times higher than in patients treated in CR-1 (P < 0.001) [89]. Therefore, for patients considered at high risk of relapse, it is preferable to transplant patients in CR-1.
Risk profile
As discussed in Q1 (above), AML patients can be stratified into favorable and unfavorable categories, based predominantly on cytogenetics [19,90]. Patients judged to be at high risk of relapse should be considered for HSCT in CR-1 [8,86]. These include patients with adverse-risk cytogenetics and those with intermediate-risk cytogenetics, except those with favorable molecular profiles (NPM1 mutated/FLT3-ITD negative or CEBPA double mutants). Although older patients with favorable-risk cytogenetics (or intermediate-risk with favorable molecular profiles) have inferior survival compared to younger patients with the same characteristics, there are insufficient data to support recommending HSCT in older patients with these favorable features.
Cytogenetic risk classification is the most important determinant of outcome in patients receiving RIC-HSCT. HSCT can to some extent overcome the effects of adverse cytogenetic and molecular genetic risk [91,92], and results from non-randomized studies appear to favor HSCT in these patients, even allowing for patient selection. However, it is recognized that most reported series in older patients are highly selected, and prospective comparative studies in older patients are needed, comparing HSCT to conventional treatment approaches.
Comorbidity
The HCT-CI was developed to better define those patients with an unacceptable risk of fatal outcome with HCT [37]. Compared with the CCI, the HCT-CI has refined the definition of several co-morbidities, improving the sensitivity and specificity for predicting non-relapse mortality (NRM) [37]. Recent overall improvements in HSCT and the development of reduced-intensity conditioning has permitted wider use of HSCT in patients with co-morbidities and in patients > 60 years of age, often resulting in durable leukemia-free survival [84,85,93-96].
Donor availability
HSCT is generally performed using hematopoietic stem cells (HSCs) either from an HLA-matched sibling or from a matched unrelated donor (MUD) with at least a 9/10 antigen match. Siblings and 10/10 MUDs are probably equivalent options, based on recent data [89]; 9/10 MUD HSCT is associated with higher toxicity and treatment-related mortality [89], but this option is also considered acceptable in patients at high risk of relapse.
The difficulty of finding an appropriate donor has spurred the search for alternative sources of HSCs, including haploidentical related donors with two or more antigenic mismatches, or cord blood with three or fewer mismatches [87]. Although recent data are promising, it is preferable for alternative-donor HSCT to be done within the context of prospective clinical trials until further results are available [87,97-99].
Recommendations
1. When an HLA-matched related or unrelated donor is available, HSCT is an appropriate treatment option for suitable patients aged > 60 with AML who are in CR-1 and have one of the following:
a. Intermediate-risk karyotype, with the exception of those with favorable molecular profiles.
b. Adverse-risk karyotype.
c. t(8;21) or inv(16) with c-kit mutation.
2. HSCT should also be considered for patients in CR-2, although efficacy data in older patients are limited, and relapse rates are higher than for those transplanted in CR-1.
3. HSCT should employ non-myeloablative or RIC regimens in patients aged > 60.
4. The HCT-CI should be used to help determine eligibility for HSCT.
5. In higher-risk patients with no available 6/6-matched sibling or 9-10/10 MUD, alternative-donor transplants (haploidentical donors and cord blood sources) may be considered but should be done as part of a clinical trial.
6. Otherwise-suitable patients with treatment-induced AML or AML arising from an antecedent disorder (AHD) should be considered eligible for transplantation (see Q5).
Question # 4: How should we treat older patients who are not considered suitable for induction chemotherapy?
Patients who are not being considered for induction chemotherapy or for subsequent HSCT constitute a diverse group including individuals judged too frail for these procedures and those who would not benefit from them. They may also include patients who refuse consent or who, for reasons of personal choice or access, cannot be accommodated or treated. Major treatment options for these patients include best supportive care (BSC) with or without hydroxyurea; low-dose cytarabine; hypomethylating agents; and investigational therapies. For patients receiving BSC, trial data suggest a typical OS of approximately 3.5 months, with a 1-year survival of 10% to 15% [25]. These findings provide a benchmark from which to compare outcomes with active intervention and can be used to guide clinical decision making.
Low-dose cytarabine
The MRC AML 14 trial [10], the only randomized trial comparing BSC with hydroxyurea to low-dose cytarabine, demonstrated a significant advantage for cytarabine treatment, with 18% achieving CR. Cytarabine treatment was associated with increased OS in all age groups. However, only patients with favorable- or intermediate-risk cytogenetics achieved a CR with cytarabine. There were no remissions, and correspondingly no survival advantage, with low-dose cytarabine in the adverse-risk cytogenetics group.
Hypomethylating agents
A phase III study of patients with AML (20-30% blasts) and multilineage dysplasia compared azacitidine to conventional care regimens (most of whom received either either BSC or low-dose cytarabine) [100,101]. CR rates for azacitidine were similar to those observed with low-dose cytarabine. However, the azacitidine arm had a significantly greater 2-year OS (50% vs 16%; P = 0.001) compared to the conventional care arm, most of whom received non-intensive therapy. OS was longer in patients who experienced complete or partial response or hematological improvement with azacitidine, relative to those who had no response [102]. This is in contrast to the expected findings with cytarabine treatment, namely that survival benefits are limited to patients experiencing CR [10,101]. A recent study in older AML patients unfit for, or unresponsive to, induction therapy reached a similar conclusion regarding survival benefit with azacitidine using a 5-day-per-week schedule, even in the absence of CR [103]. An ongoing phase III trial (NCT01074047) is comparing azacitidine with conventional care regimens in older patients with higher-blast-count AML.
Cytogenetic risk group remains an important prognostic factor with azacitidine, with adverse risk groups having inferior OS and 2-year survival. However, even in patients with adverse cytogenetic risk, azacitidine treatment was associated with significantly greater survival, relative to conventional treatment (2-year OS rate 38% vs 0%; P = 0.01) [101].
A multicentre phase III randomized trial was recently reported, comparing decitabine to either BSC alone or low-dose cytarabine in AML patients ≥ age 65 [104]. Most patients in the supportive-care arm (88%) received cytarabine. This study found that the CR rate was higher in the decitabine arm (17.8% vs 7.8%; P = 0.001). There was a non-significant increase in OS in the decitabine arm (P = 0.11) that reached statistical significance (P = 0.037) at a subsequent unplanned survival analysis. Subgroup analysis showed an OS benefit in the decitabine arm for patients ≥ age 75 and in those with > 30% marrow blasts, intermediate-risk karyotype, de novo AML and ECOG performance status (PS) 2; however, a multivariate analysis was not done. Adverse events were similar between the decitabine and cytarabine groups [104].
HDAC inhibitors and other investigational agents
A variety of investigational agents have been used alone or in combination with hypomethylating agents and low-dose cytarabine in older, unfit AML patients. These have included histone deacetylase (HDAC) inhibitors such as valproic acid and vorinostat [105-107], tipifarnib [25], laromustine [108], temozolomide [109] and others. Despite encouraging results in some of these, none have yet been demonstrated to be more effective than either hypomethylating agents or low-dose cytarabine alone [110-112]. The largest phase III trial of such agents found no survival benefit to tipifarnib compared to BSC in previously untreated AML patients over age 70 [25].
Recommendations for patients unsuitable for induction therapy
1. For patients with 20% to 30% bone marrow blasts with multilineage dysplasia, azacitidine should be offered as standard treatment. For patients not able to receive azacitidine, low-dose cytarabine is acceptable for those with intermediate- and favorable-risk cytogenetics.
2. For all other patients, consider cytogenetic risk:
a. Intermediate-risk and favorable-risk cytogenetics: Low-dose cytarabine is reasonable initial treatment based on the MRC AML 14 study. Decitabine is also a reasonable choice, if available, based on recent phase III data, and may be superior to cytarabine in patients with de novo AML and those ≥ age 75. Data from a similar ongoing trial with azacitidine are not yet available.
b. Adverse-risk cytogenetics: No effective treatment is available. Low-dose cytarabine is ineffective in this setting and should not be offered, while decitabine was not shown to be superior. The standard treatment is BSC.
3. All patients who are unfit for intensive induction therapy should be offered participation in a clinical trial using novel therapeutic approaches, given the overall poor outcomes in such patients.
Question # 5: How should we treat older patients with secondary AML?
Patients with AML arising from an AHD or from prior treatment have an inferior prognosis with standard induction chemotherapy, compared to those with de novo AML [113]. Such cases, sometimes described collectively as secondary AML, are also more likely to have adverse-risk cytogenetics [113]. Studies using multivariate analysis, or otherwise correcting for cytogenetic risk group, indicate that karyotype is a more important predictor of prognosis than prior disease history per se [9,26,39,114]. Accordingly, patients with AML arising from an AHD, and with an intermediate-risk karyotype, have CR rates and OS comparable to those of patients with de novo AML [114]. In secondary AML patients > age 60, there is no evidence that the usual molecular risk factors, NPM1 and FLT3 status, are of major prognostic importance [115].
In one study, patients with prior MDS previously treated with lenalidomide or hypomethylating agents appeared to have a poorer response rate to subsequent induction therapy, relative to patients receiving only supportive care or other treatment for their earlier disease [114]. While it was suggested that the prior treatment may have altered the susceptibility of the leukemic cells to subsequent therapy, it is also possible that the prognosis in these cases was intrinsically poor. These retrospective results have not yet been verified in a prospective study.
Secondary AML arising from a prior myeloproliferative disorder (MPD) is associated with a poorer prognosis with induction therapy, compared to AML arising from a prior MDS or other types of AHD [116]. A longer duration of the AHD [6], and a longer time between diagnosis of the AHD and progression to AML [114], have also been associated with shorter survival with induction therapy.
Allo-HSCT is a promising approach for secondary AML patients achieving CR. In a large cohort of de novo or secondary AML patients (median age 60 years) undergoing RIC-HSCT in CR, AHD was not an independent risk factor for relapse or progression [89].
Recommendations
1. Older patients should not be denied induction chemotherapy solely on the basis of having transformed from a prior MDS or having received prior chemotherapy for another malignancy. Secondary AML patients with intermediate- or favorable-risk cytogenetics should be offered induction chemotherapy if they are otherwise medically fit, as per Q2.
2. Secondary AML patients with adverse-risk cytogenetics, or transforming from a prior MPD, should be considered for other treatment options. These may include:
a. Hypomethylating agent therapy, such as azacitidine, if the bone marrow shows 20% to 30% blasts with multilineage dysplasia.
b. Clinical trial, if available.
c. Supportive care alone.
3. Potential HSCT candidates should be offered induction therapy with a view toward proceeding to HSCT if response is achieved, as in de novo AML. Some panel members felt that hypomethylating agent therapy is also an acceptable initial treatment for patients with 20% to 30% blasts and multilineage dysplasia, if a suitable donor has not yet been identified.
Conclusion
Several key recommendations evolved from this consensus. First, for older patients considered medically fit, who opt for intensive induction chemotherapy, cytogenetic information is critical in order to facilitate treatment decisions and should be provided in a timely manner. Older patients with adverse-risk cytogenetics derive little benefit from standard induction therapy, and other approaches should be considered. Conversely, patients should not be denied induction chemotherapy solely on the basis of age, having transformed from a prior MDS, or having leukemia that arose from prior chemotherapy.
For patients not suitable for induction chemotherapy, an assessment of the percentage of bone marrow blasts will guide treatment decisions. For patients with 20% to 30% blasts with dysplasia, azacitidine is the recommended agent. For patients with > 30% bone marrow blasts with intermediate-risk cytogenetics, low-dose cytarabine or decitabine are reasonable as initial treatment, pending further trial data.
The key recommendations stemming from the discussions are summarized in the algorithms shown in Figures 1, 2 and 3.
Figure 1.

Treatment of older AML patients deemed medically fit for induction who are also potential candidates for hematopoietic stem cell transplant (HSCT). BSC = best supportive care; CR = complete response; HiDAC = high-dose cytarabine.
Figure 2.
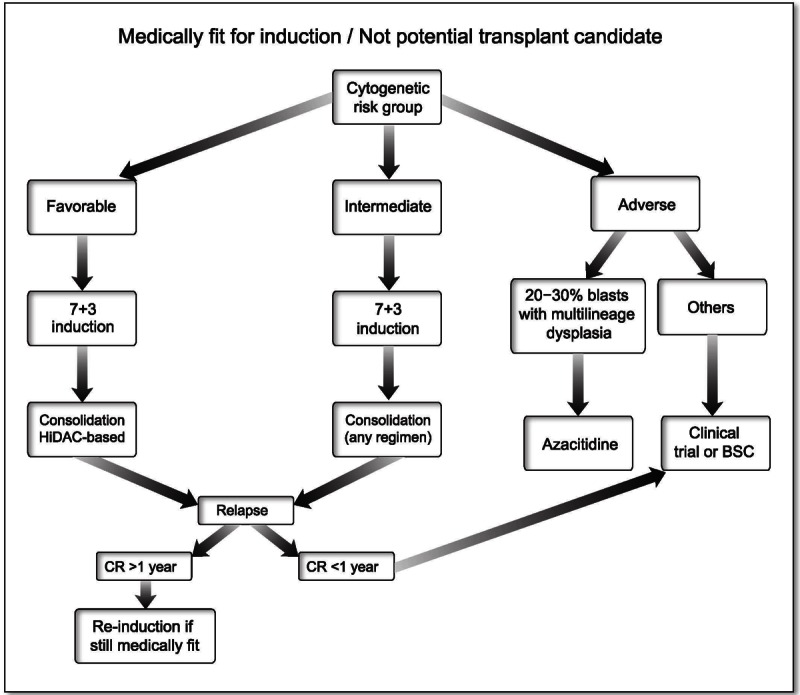
Treatment of older AML patients deemed medically fit for induction who are not candidates for HSCT. BSC = best supportive care; CR = complete remission; HiDAC = high-dose cytarabine.
Figure 3.

Treatment of older AML patients not deemed fit for induction. BSC = best supportive care; LD-AraC = low-dose cytarabine.
Acknowledgements
The authors wish to acknowledge the contribution of a medical communication company (SCRIPT, Toronto, ON, Canada) and Zoe Agnidis, MSc, to the literature review and the development of early drafts of this manuscript. Celgene Canada provided unrestricted support for the work of the panel. The opinions and analyses discussed here are entirely those of the physician-authors.
Conflict of interest
Joseph Brandwein, MD, FCRCP: Advisory board(s): Celgene, Novartis, Merck, Pfizer, Sunesis. Research funding: Novartis, Merck. Michelle Geddes, MD, FRCPC: Advisory board(s): Celgene, Schering Plough, Novartis. Research support: Celgene, Novartis. Jeannine Kassis, MD, No conflicts of interest to declare. Andrea K Kew, MD, FRCPC: No conflicts of interest to declare. Brian Leber, MDCM, FRCPC: Honoraria and Speaker’s Bureau: Celgene. Thomas Nevill, M.D., FRCPC: Advisory boards: Celgene, Novartis. Mitchell Sabloff, MD: Advisory boards: Celgene, Merck, Pfizer, Novartis, Research support: Celgene, Novartis, Roche. Irwindeep Sandhu, MD, FRCPC: Advisory Boards: GlaxoSmithKline, Celgene, Genzyme, Alexion, Speaker: Celgene, Janssen. Andre C Schuh, MD, FRCPC: Grant funding: Celgene, Bayer, Advisory Boards: Celgene, Genzyme, Speaker: Celgene, Novartis. John M Storring, MD, CM, FRCPC: Advisory board(s): Celgene, Novartis, Alexion, Genzyme, Speaker fees: Celgene, Novarits. Research Support: Celgene, Boeringher-Ingelheim. John Ashkenas, PhD: Contribution supported by a grant from Celgene Canada. JA declares no other conflicts.
References
- 1.Dombret H, Raffoux E, Gardin C. New insights in the management of elderly patients with acute myeloid leukemia. Curr Opin Oncol. 2009 Nov;21:589–93. doi: 10.1097/CCO.0b013e3283313e10. [DOI] [PubMed] [Google Scholar]
- 2.Rathnasabapathy R, Lancet JE. Management of Acute Myelogenous Leukemia in the Elderly. Cancer Control. 2003 Nov-Dec;10:469–77. doi: 10.1177/107327480301000605. [DOI] [PubMed] [Google Scholar]
- 3.Stone RM. The difficult problem of acute myeloid leukemia in the older adult. CA Cancer J Clin. 2002 Nov-Dec;52:363–71. doi: 10.3322/canjclin.52.6.363. [DOI] [PubMed] [Google Scholar]
- 4.Juliusson G, Antunovic P, Derolf A, Lehmann S, Mollgard L, Stockelberg D, Tidefelt U, Wahlin A, Hoglund M. Age and acute myeloid leukemia: real world data on decision to treat and outcomes from the Swedish Acute Leukemia Registry. Blood. 2009 Apr 30;113:4179–4187. doi: 10.1182/blood-2008-07-172007. [DOI] [PubMed] [Google Scholar]
- 5.Gupta V, Xu W, Keng C, Alibhai SMH, Brandwein J, Schimmer A, Schuh A, Yee K, Minden MD. The outcome of intensive induction therapy in patients ≥ 70 years with acute myeloid leukemia. Leukemia. 2007;21:1321–1324. doi: 10.1038/sj.leu.2404655. [DOI] [PubMed] [Google Scholar]
- 6.Kantarjian H, O’Brien S, Cortes J, Giles F, Faderl S, Jabbour E, Garcia-Manero G, Wierda W, Pierce S, Shan J, Estey E. Results of intensive chemotherapy in 998 patients age 65 years or older with acute myeloid leukemia or high-risk myelodysplastic syndrome: predictive prognostic models for outcome. Cancer. 2006 Mar 1;106:1090–1098. doi: 10.1002/cncr.21723. [DOI] [PubMed] [Google Scholar]
- 7.Wheatley K, Brookes CL, Howman AJ, Goldstone AH, Milligan DW, Prentice AG, Moorman AV, Burnett AK United Kingdom National Cancer Research Institute Haematological Oncology Clinical Studies Group, Acute Myeloid Leukaemia Subgroup. Prognostic factor analysis of the survival of elderly patients with AML in the MRC AML11 and LRF AML14 trials. Br J Haematol. 2009 Jun;145:598–605. doi: 10.1111/j.1365-2141.2009.07663.x. [DOI] [PubMed] [Google Scholar]
- 8.Fröhling S, Schlenk RF, Kayser S, Morhardt M, Benner A, Döhner K, Döhner H German-Austrian AML Study Group. Cytogenetics and age are major determinants of outcome in intensively treated acute myeloid leukemia patients older than 60 years: results from AMLSG trial AML HD98-B. Blood. 2006 Nov 15;108:3280–3288. doi: 10.1182/blood-2006-04-014324. [DOI] [PubMed] [Google Scholar]
- 9.Gupta V, Chun K, Yi QL, Minden M, Schuh A, Wells R, Brandwein J. Disease biology rather than age is the most important determinant of survival of patients > or = 60 years with acute myeloid leukemia treated with uniform intensive therapy. Cancer. 2005 May 15;103:2082–2090. doi: 10.1002/cncr.21006. [DOI] [PubMed] [Google Scholar]
- 10.Burnett AK, Milligan D, Prentice AG, Goldstone AH, McMullin MF, Hills RK, Wheatley K. A comparison of low-dose cytarabine and hydroxyurea with or without all-trans retinoic acid for acute myeloid leukemia and high-risk myelodysplastic syndrome in patients not considered fit for intensive treatment. Cancer. 2007 Mar 15;109:1114–1124. doi: 10.1002/cncr.22496. [DOI] [PubMed] [Google Scholar]
- 11.Jehn U, Suciu S, Thomas X, Lefrere F, Muus P, Berneman Z, Marie JP, Adamo F, Fillet G, Nobile F, Ricciuti F, Leone G, Rizzoli V, Montanaro M, Beeldens F, Fazi P, Mandelli F, Willemze R, de Witte T, Amadori S. Non-infusional vs intravenous consolidation chemotherapy in elderly patients with acute myeloid leukemia: final results of the EORTC-GIMEMA AML-13 randomized phase III trial. Leukemia. 2006 Oct;20:1723–1730. doi: 10.1038/sj.leu.2404356. [DOI] [PubMed] [Google Scholar]
- 12.Grimwade D, Hills RK, Moorman AV, Walker H, Chatters S, Goldstone AH, Wheatley K, Harrison CJ, Burnett AK National Cancer Research Institute Adult Leukaemia Working Group. Refinement of cytogenetic classification in acute myeloid leukemia: determination of prognostic significance of rare recurring chromosomal abnormalities among 5876 younger adult patients treated in the United Kingdom Medical Research Council trials. Blood. 2010 Jul 22;116:354–365. doi: 10.1182/blood-2009-11-254441. [DOI] [PubMed] [Google Scholar]
- 13.Leith CP, Kopecky KJ, Godwin J, McConnell T, Slovak ML, Chen IM, Head DR, Appelbaum FR, Willman CL. Acute myeloid leukemia in the elderly: assessment of multidrug resistance (MDR1) and cytogenetics distinguishes biologic subgroups with remarkably distinct responses to standard chemotherapy. A Southwest Oncology Group study. Blood. 1997 May 1;89:3323–3329. [PubMed] [Google Scholar]
- 14.Buchner T, Berdel WE, Haferlach C, Haferlach T, Schnittger S, Muller-Tidow C, Braess J, Spiekermann K, Kienast J, Staib P, Gruneisen A, Kern W, Reichle A, Maschmeyer G, Aul C, Lengfelder E, Sauerland MC, Heinecke A, Wormann B, Hiddemann W. Age-related risk profile and chemotherapy dose response in acute myeloid leukemia: a study by the German Acute Myeloid Leukemia Cooperative Group. J. Clin. Oncol. 2009 Jan 1;27:61–9. doi: 10.1200/JCO.2007.15.4245. [DOI] [PubMed] [Google Scholar]
- 15.Farag SS, Archer KJ, Mrozek K, Ruppert AS, Carroll AJ, Vardiman JW, Pettenati MJ, Baer MR, Qumsiyeh MB, Koduru PR, Ning Y, Mayer RJ, Stone RM, Larson RA, Bloomfield CD. Pretreatment cytogenetics add to other prognostic factors predicting complete remission and long-term outcome in patients 60 years of age or older with acute myeloid leukemia: results from Cancer and Leukemia Group B 8461. Blood. 2006 Jul 1;108:63–73. doi: 10.1182/blood-2005-11-4354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vey N, Coso D, Bardou VJ, Stoppa AM, Braud AC, Bouabdallah R, Sainty D, Mozziconacci MJ, Lafage M, Damaj G, Blaise D, Gastaut JA, Maraninchi D. The benefit of induction chemotherapy in patients age > or = 75 years. Cancer. 2004 Jul 15;101:325–331. doi: 10.1002/cncr.20353. [DOI] [PubMed] [Google Scholar]
- 17.Walter RB, Othus M, Borthakur G, Ravandi F, Cortes JE, Pierce SA, Appelbaum FR, Kantarjian HA, Estey EH. Prediction of early death after induction therapy for newly diagnosed acute myeloid leukemia with pretreatment risk scores: a novel paradigm for treatment assignment. J. Clin. Oncol. 2011 Nov 20;29:4417–23. doi: 10.1200/JCO.2011.35.7525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kantarjian H, Ravandi F, O’Brien S, Cortes J, Faderl S, Garcia-Manero G, Jabbour E, Wierda W, Kadia T, Pierce S, Shan J, Keating M, Freireich EJ. Intensive chemotherapy does not benefit most older patients (age 70 years or older) with acute myeloid leukemia. Blood. 2010 Nov 25;116:4422–4429. doi: 10.1182/blood-2010-03-276485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grimwade D, Walker H, Oliver F, Wheatley K, Harrison C, Harrison G, Rees J, Hann I, Stevens R, Burnett A, Goldstone A. The importance of diagnostic cytogenetics on outcome in AML: analysis of 1,612 patients entered into the MRC AML 10 trial. The Medical Research Council Adult and Children’s Leukaemia Working Parties. Blood. 1998 Oct 1;92:2322–2333. [PubMed] [Google Scholar]
- 20.Rowe JM, Kim HT, Cassileth PA, Lazarus HM, Litzow MR, Wiernik PH, Tallman MS. Adult patients with acute myeloid leukemia who achieve complete remission after 1 or 2 cycles of induction have a similar prognosis: a report on 1980 patients registered to 6 studies conducted by the Eastern Cooperative Oncology Group. Cancer. 2010 Nov 1;116:5012–5021. doi: 10.1002/cncr.25263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rowe JM, Neuberg D, Friedenberg W, Bennett JM, Paietta E, Makary AZ, Liesveld JL, Abboud CN, Dewald G, Hayes FA, Tallman MS, Wiernik PH, Eastern Cooperative O. A phase 3 study of three induction regimens and of priming with GM-CSF in older adults with acute myeloid leukemia: a trial by the Eastern Cooperative Oncology Group. Blood. 2004 Jan 15;103:479–485. doi: 10.1182/blood-2003-05-1686. [DOI] [PubMed] [Google Scholar]
- 22.Breems DA, Van Putten WLJ, De Greef GE, Van Zelderen-Bhola SL, Gerssen-Schoorl KBJ, Mellink CHM, Nieuwint A, Jotterand M, Hagemeijer A, Beverloo HB, Lowenberg B. Monosomal karyotype in acute myeloid leukemia: a better indicator of poor prognosis than a complex karyotype. J. Clin. Oncol. 2008 Oct 10;26:4791–7. doi: 10.1200/JCO.2008.16.0259. [DOI] [PubMed] [Google Scholar]
- 23.Medeiros BC, Othus M, Fang M, Roulston D, Appelbaum FR. Prognostic impact of monosomal karyotype in young adult and elderly acute myeloid leukemia: the Southwest Oncology Group (SWOG) experience. Blood. 2010 Sep 30;116:2224–2228. doi: 10.1182/blood-2010-02-270330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Perrot A, Luquet I, Pigneux A, Mugneret F, Delaunay J, Harousseau JL, Barin C, Cahn JY, Guardiola P, Himberlin C, Recher C, Vey N, Lioure B, Ojeda-Uribe M, Fegueux N, Berthou C, Randriamalala E, Béné MC, Ifrah N, Witz F Groupe Ouest-Est des Leucémies Aiguës et Maladies du Sang. Dismal prognostic value of monosomal karyotype in elderly patients with acute myeloid leukemia: a GOELAMS study of 186 patients with unfavorable cytogenetic abnormalities. Blood. 2011 Jul 21;118:679–685. doi: 10.1182/blood-2010-09-307264. [DOI] [PubMed] [Google Scholar]
- 25.Harousseau JL, Martinelli G, Jedrzejczak WW, Brandwein JM, Bordessoule D, Masszi T, Ossenkoppele GJ, Alexeeva JA, Beutel G, Maertens J, Vidriales MB, Dombret H, Thomas X, Burnett AK, Robak T, Khuageva NK, Golenkov AK, Tothova E, Mollgard L, Park YC, Bessems A, De Porre P, Howes AJ. A randomized phase 3 study of tipifarnib compared with best supportive care, including hydroxyurea, in the treatment of newly diagnosed acute myeloid leukemia in patients 70 years or older. Blood. 2009 Aug 6;114:1166–1173. doi: 10.1182/blood-2009-01-198093. [DOI] [PubMed] [Google Scholar]
- 26.Röllig C, Thiede C, Gramatzki M, Aulitzky W, Bodenstein H, Bornhäuser M, Platzbecker U, Stuhlmann R, Schuler U, Soucek S, Kramer M, Mohr B, Oelschlaegel U, Stölzel F, von Bonin M, Wermke M, Wandt H, Ehninger G, Schaich M Study Alliance Leukemia. A novel prognostic model in elderly patients with acute myeloid leukemia: results of 909 patients entered into the prospective AML96 trial. Blood. 2010 Aug 12;116:971–978. doi: 10.1182/blood-2010-01-267302. [DOI] [PubMed] [Google Scholar]
- 27.Paschka P, Marcucci G, Ruppert AS, Mrózek K, Chen H, Kittles RA, Vukosavljevic T, Perrotti D, Vardiman JW, Carroll AJ, Kolitz JE, Larson RA, Bloomfield CD Cancer and Leukemia Group B. Adverse prognostic significance of KIT mutations in adult acute myeloid leukemia with inv(16) and t(8;21): a Cancer and Leukemia Group B Study. J. Clin. Oncol. 2006 Aug 20;24:3904–11. doi: 10.1200/JCO.2006.06.9500. [DOI] [PubMed] [Google Scholar]
- 28.Becker H, Marcucci G, Maharry K, Radmacher MD, Mrozek K, Margeson D, Whitman SP, Wu YZ, Schwind S, Paschka P, Powell BL, Carter TH, Kolitz JE, Wetzler M, Carroll AJ, Baer MR, Caligiuri MA, Larson RA, Bloomfield CD. Favorable prognostic impact of NPM1 mutations in older patients with cytogenetically normal de novo acute myeloid leukemia and associated gene- and microRNA-expression signatures: a Cancer and Leukemia Group B study. J. Clin. Oncol. 2010 Feb 1;28:596–604. doi: 10.1200/JCO.2009.25.1496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Appelbaum FR, Kopecky KJ, Tallman MS, Slovak ML, Gundacker HM, Kim HT, Dewald GW, Kantarjian HM, Pierce SR, Estey EH. The clinical spectrum of adult acute myeloid leukaemia associated with core binding factor translocations. Br J Haematol. 2006 Oct;135:165–73. doi: 10.1111/j.1365-2141.2006.06276.x. [DOI] [PubMed] [Google Scholar]
- 30.Marcucci G, Maharry K, Wu YZ, Radmacher MD, Mrozek K, Margeson D, Holland KB, Whitman SP, Becker H, Schwind S, Metzeler KH, Powell BL, Carter TH, Kolitz JE, Wetzler M, Carroll AJ, Baer MR, Caligiuri MA, Larson RA, Bloomfield CD. IDH1 and IDH2 gene mutations identify novel molecular subsets within de novo cytogenetically normal acute myeloid leukemia: a Cancer and Leukemia Group B study. J. Clin. Oncol. 2010 May 10;28:2348–2355. doi: 10.1200/JCO.2009.27.3730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Patel JP, Gonen M, Figueroa ME, Fernandez H, Sun Z, Racevskis J, Van Vlierberghe P, Dolgalev I, Thomas S, Aminova O, Huberman K, Cheng J, Viale A, Socci ND, Heguy A, Cherry A, Vance G, Higgins RR, Ketterling RP, Gallagher RE, Litzow M, van den Brink MR, Lazarus HM, Rowe JM, Luger S, Ferrando A, Paietta E, Tallman MS, Melnick A, Abdel-Wahab O, Levine RL. Prognostic relevance of integrated genetic profiling in acute myeloid leukemia. N Engl J Med. 2012 Mar 22;366:1079–1089. doi: 10.1056/NEJMoa1112304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rollig C, Bornhauser M, Thiede C, Taube F, Kramer M, Mohr B, Aulitzky W, Bodenstein H, Tischler HJ, Stuhlmann R, Schuler U, Stolzel F, von Bonin M, Wandt H, Schafer-Eckart K, Schaich M, Ehninger G. Long-term prognosis of acute myeloid leukemia according to the new genetic risk classification of the European LeukemiaNet recommendations: evaluation of the proposed reporting system. J. Clin. Oncol. 2011 Jul 10;29:2758–65. doi: 10.1200/JCO.2010.32.8500. [DOI] [PubMed] [Google Scholar]
- 33.Meshinchi S, Stirewalt DL, Alonzo TA, Zhang Q, Sweetser DA, Woods WG, Bernstein ID, Arceci RJ, Radich JP. Activating mutations of RTK/ras signal transduction pathway in pediatric acute myeloid leukemia. Blood. 2003;102:1474–1479. doi: 10.1182/blood-2003-01-0137. [DOI] [PubMed] [Google Scholar]
- 34.Ferrara F, Criscuolo C, Riccardi C, Izzo T, Pedata M, Copia C, Vicari L, Tarsitano M, Palmieri S, Pane F. FLT3 mutations have no prognostic impact in elderly patients with acute myeloid leukemia and normal karyotype. Am J Hematol. 2009;84:532–535. doi: 10.1002/ajh.21458. [DOI] [PubMed] [Google Scholar]
- 35.Taskesen E, Bullinger L, Corbacioglu A, Sanders MA, Erpelinck CA, Wouters BJ, van der Poel-van de Luytgaarde SC, Damm F, Krauter J, Ganser A, Schlenk RF, Löwenberg B, Delwel R, Döhner H, Valk PJ, Döhner K. Prognostic impact, concurrent genetic mutations, and gene expression features of AML with CEBPA mutations in a cohort of 1182 cytogenetically normal AML patients: further evidence for CEBPA double mutant AML as a distinctive disease entity. Blood. 2011;117:2469–2475. doi: 10.1182/blood-2010-09-307280. [DOI] [PubMed] [Google Scholar]
- 36.Etienne A, Esterni B, Charbonnier A, Mozziconacci MJ, Arnoulet C, Coso D, Puig B, Gastaut JA, Maraninchi D, Vey N. Comorbidity is an independent predictor of complete remission in elderly patients receiving induction chemotherapy for acute myeloid leukemia. Cancer. 2007 Apr 1;109:1376–1383. doi: 10.1002/cncr.22537. [DOI] [PubMed] [Google Scholar]
- 37.Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG, Storer B. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood. 2005 Oct 15;106:2912–2919. doi: 10.1182/blood-2005-05-2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Giles FJ, Borthakur G, Ravandi F, Faderl S, Verstovsek S, Thomas D, Wierda W, Ferrajoli A, Kornblau S, Pierce S, Albitar M, Cortes J, Kantarjian H. The haematopoietic cell transplantation comorbidity index score is predictive of early death and survival in patients over 60 years of age receiving induction therapy for acute myeloid leukaemia. Br J Haematol. 2007 Feb;136:624–7. doi: 10.1111/j.1365-2141.2006.06476.x. [DOI] [PubMed] [Google Scholar]
- 39.Malfuson JV, Etienne A, Turlure P, de Revel T, Thomas X, Contentin N, Terré C, Rigaudeau S, Bordessoule D, Vey N, Gardin C, Dombret H Acute Leukemia French Association (ALFA) Risk factors and decision criteria for intensive chemotherapy in older patients with acute myeloid leukemia. Haematologica. 2008 Dec;93:1806–1813. doi: 10.3324/haematol.13309. [DOI] [PubMed] [Google Scholar]
- 40.Chevallier P, Labopin M, Turlure P, Prebet T, Pigneux A, Hunault M, Filanovsky K, Cornillet-Lefebvre P, Luquet I, Lode L, Richebourg S, Blanchet O, Gachard N, Vey N, Ifrah N, Milpied N, Harousseau JL, Bene MC, Mohty M, Delaunay J. A new Leukemia Prognostic Scoring System for refractory/relapsed adult acute myelogeneous leukaemia patients: a GOELAMS study. Leukemia. 2011;25:939–944. doi: 10.1038/leu.2011.25. [DOI] [PubMed] [Google Scholar]
- 41.Kurosawa S, Yamaguchi T, Miyawaki S, Uchida N, Sakura T, Kanamori H, Usuki K, Yamashita T, Okoshi Y, Shibayama H, Nakamae H, Mawatari M, Hatanaka K, Sunami K, Shimoyama M, Fujishima N, Maeda Y, Miura I, Takaue Y, Fukuda T. Prognostic factors and outcomes of adult patients with acute myeloid leukemia after first relapse. Haematologica. 2010;95:1857–1864. doi: 10.3324/haematol.2010.027516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Litzow MR, Othus M, Cripe LD, Gore SD, Lazarus HM, Lee SJ, Bennett JM, Paietta EM, Dewald GW, Rowe JM, Tallman MS. Failure of three novel regimens to improve outcome for patients with relapsed or refractory acute myeloid leukaemia: a report from the Eastern Cooperative Oncology Group. Br J Haematol. 2012 Jan;148:217–225. doi: 10.1111/j.1365-2141.2009.07917.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Leopold LH, Willemse R. The treatment of acute myeloid leukemia in first relapse: A comprehensive review of the literature. Leuk Lymphoma. 2002;43:1715–1727. doi: 10.1080/1042819021000006529. [DOI] [PubMed] [Google Scholar]
- 44.Pautas C, Merabet F, Thomas X, Raffoux E, Gardin C, Corm S, Bourhis JH, Reman O, Turlure P, Contentin N, de Revel T, Rousselot P, Preudhomme C, Bordessoule D, Fenaux P, Terre C, Michallet M, Dombret H, Chevret S, Castaigne S. Randomized study of intensified anthracycline doses for induction and recombinant interleukin-2 for maintenance in patients with acute myeloid leukemia age 50 to 70 years: results of the ALFA-9801 study. J. Clin. Oncol. 2010 Feb 10;28:808–814. doi: 10.1200/JCO.2009.23.2652. [DOI] [PubMed] [Google Scholar]
- 45.Schiller G, Nimer S, Gajewski J, Lee M, Ho W, Territo M, Champlin R. Effect of Induction Cytarabine Dose Intensity on Long-Term Survival in Acute Myelogenous Leukemia: Results of a Randomized, Controlled Study. Leuk Lymphoma. 1993 Sep;11:69–77. doi: 10.3109/10428199309054732. [DOI] [PubMed] [Google Scholar]
- 46.Weick JK, Kopecky KJ, Appelbaum FR, Head DR, Kingsbury LL, Balcerzak SP, Bickers JN, Hynes HE, Welborn JL, Simon SR, Grever M. A randomized investigation of high-dose versus standard-dose cytosine arabinoside with daunorubicin in patients with previously untreated acute myeloid leukemia: a Southwest Oncology Group study. Blood. 1996 Oct 15;88:2841–2851. [PubMed] [Google Scholar]
- 47.Van Der Jagt R, Robinson KS, Belch A, Yetisir E, Wells G, Larratt L, Shustik C, Gluck S, Stewart K, Sheridan D Canadian Leukemia Studies Group. Sequential response-adapted induction and consolidation regimens idarubicin/cytarabine and mitoxantrone/etoposide in adult acute myelogenous leukemia: 10 year follow-up of a study by the Canadian Leukemia Studies Group. Leuk Lymphoma. 2006 Apr;47:697–706. doi: 10.1080/10428190500467917. [DOI] [PubMed] [Google Scholar]
- 48.Ziogas DC, Voulgarelis M, Zintzaras E. A network meta-analysis of randomized controlled trials of induction treatments in acute myeloid leukemia in the elderly. Clin Ther. 2011 Mar;33:254–79. doi: 10.1016/j.clinthera.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 49.Estey EH, Thall PF, Giles FJ, Wang XM, Cortes JE, Beran M, Pierce SA, Thomas DA, Kantarjian HM. Gemtuzumab ozogamicin with or without interleukin 11 in patients 65 years of age or older with untreated acute myeloid leukemia and high-risk myelodysplastic syndrome: comparison with idarubicin plus continuous-infusion, high-dose cytosine arabinoside. Blood. 2002 Jun 15;99:4343–4349. doi: 10.1182/blood.v99.12.4343. [DOI] [PubMed] [Google Scholar]
- 50.Castaigne S, Pautas C, Terre C, Raffoux E, Bordessoule D, Bastie JN, Legrand O, Thomas X, Turlure P, Reman O, De Revel T, Gastaud L, de Gunsberg N, Contentin N, Henry E, Marolleau JP, Aljijakli A, Rousselot P, Fenaux F, Preudhomme C, Chevret S, Dombret H. Effect of gemtuzumab ozogamicin on survival of adult patients with de-novo acute myeloid leukaemia (ALFA-0701): a randomised, open-label, phase 3 study. Lancet. 2012;379:1508–1516. doi: 10.1016/S0140-6736(12)60485-1. [DOI] [PubMed] [Google Scholar]
- 51.Burnett AK, Hills RK, Hunter AE, Milligan D, Kell WJ, Wheatley K, Yin JL, Ali S, Kjeldsen L, Bowen D, Russell NH. The Addition of Gemtuzumab Ozogamicin to Intensive Chemotherapy in Older Patients with AML Produces a Significant Improvement in Overall Survival: Results of the UK NCRI AML16 Randomized Trial. Blood. 2011:118. [Google Scholar]
- 52.Arlin ZA, Feldman EJ, Mittelman A, Ahmed T, Puccio C, Chun HG, Cook P, Baskind P, Marboe C, Mehta R. Amsacrine is safe and effective therapy for patients with myocardial dysfunction and acute leukemia. Cancer. 1991;68:1198–1200. doi: 10.1002/1097-0142(19910915)68:6<1198::aid-cncr2820680603>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 53.Berman E, Arlin ZA, Gaynor J, Miller W, Gee T, Kempin SJ, Mertelsmann R, Andreeff M, Reich L, Nahmias N, et al. Comparative trial of cytarabine and thioguanine in combination with amsacrine or daunorubicin in patients with untreated acute nonlymphocytic leukemia: results of the L-16M protocol. Leukemia. 1989 Feb;3:115–121. [PubMed] [Google Scholar]
- 54.Kessler T, Mohr M, Muller-Tidow C, Krug U, Brunnberg U, Mohr B, Schliemann C, Sauerland C, Serve H, Buchner T, Berdel WE, Mesters RM. Amsacrine containing induction therapy in elderly AML patients: comparison to standard induction regimens in a matchedpair analysis. Leuk Res. 2008 Mar;32:491–494. doi: 10.1016/j.leukres.2007.06.015. [DOI] [PubMed] [Google Scholar]
- 55.Kantarjian HM, Erba HP, Claxton D, Arellano M, Lyons RM, Kovascovics T, Gabrilove J, Craig M, Douer D, Maris M, Petersdorf S, Shami PJ, Yeager AM, Eckert S, Abichandani R, Faderl S. Phase II study of clofarabine monotherapy in previously untreated older adults with acute myeloid leukemia and unfavorable prognostic factors. J. Clin. Oncol. 2010 Feb 1;28:549–55. doi: 10.1200/JCO.2009.23.3130. [DOI] [PubMed] [Google Scholar]
- 56.Agura E, Cooper B, Holmes H, Vance E, Berryman RB, Maisel C, Li S, Saracino G, Tadic-Ovcina M, Fay J. Report of a phase II study of clofarabine and cytarabine in de novo and relapsed and refractory AML patients and in selected elderly patients at high risk for anthracycline toxicity. Oncologist. 2011;16:197–206. doi: 10.1634/theoncologist.2010-0220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Faderl S, Ravandi F, Huang X, Garcia-Manero G, Ferrajoli A, Estrov Z, Borthakur G, Verstovsek S, Thomas DA, Kwari M, Kantarjian HM. A randomized study of clofarabine versus clofarabine plus low-dose cytarabine as front-line therapy for patients aged 60 years and older with acute myeloid leukemia and high-risk myelodysplastic syndrome. Blood. 2008 Sep 1;112:1638–1645. doi: 10.1182/blood-2007-11-124602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Serrano J, de la Fuente A, Bergua J, Falantes J, Eusebio MC, Antionio LJ, Martinez-Losada MC, Casano J, Romero A, Elena P, Mendez G, Tabares S, Thomas JF, Joaquin SJ, Antonio T. 5-Azacytidine Versus Intensive Chemotherapy or BSC in Elderly (>60 years) Acute Myeloid Leukemia Patients. A Retrospective Analysis. 53rd ASH Annual Meeting and Exposition. 2011 San Diego Conference Centre. [Google Scholar]
- 59.Quintas-Cardama A, Ravandi F, Liu-Dumlao T, Brandt M, Faderl S, Pierce S, Borthakur G, Garcia-Manero G, Cortes J, Kantarjian H. Epigenetic therapy is associated with similar survival compared with intensive chemotherapy in older patients with newly diagnosed acute myeloid leukemia. Blood. 2012 Dec 6;120:4840–5. doi: 10.1182/blood-2012-06-436055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Brandwein JM, Gupta V, Schuh AC, Schimmer AD, Yee K, Xu W, Messner HA, Lipton JH, Minden MD. Predictors of response to reinduction chemotherapy for patients with acute myeloid leukemia who do not achieve complete remission with frontline induction chemotherapy. Am J Hematol. 2008;83:54–58. doi: 10.1002/ajh.21034. [DOI] [PubMed] [Google Scholar]
- 61.Trifilio SM, Rademaker AW, Newman D, Coyle K, Carlson-Leuer K, Mehta J, Altman J, Frankfurt O, Tallman MS. Mitoxantrone and etoposide with or without intermediate dose cytarabine for the treatment of primary induction failure or relapsed acute myeloid leukemia. Leuk Res. 2012 Apr;36:394–396. doi: 10.1016/j.leukres.2011.10.027. [DOI] [PubMed] [Google Scholar]
- 62.Faderl S, Gandhi V, O’Brien S, Bonate P, Cortes J, Estey E, Beran M, Wierda W, Garcia-Manero G, Ferrajoli A, Estrov Z, Giles FJ, Du M, Kwari M, Keating M, Plunkett W, Kantarjian H. Results of a phase 1-2 study of clofarabine in combination with cytarabine (ara-C) in relapsed and refractory acute leukemias. Blood. 2005;105:940–947. doi: 10.1182/blood-2004-05-1933. [DOI] [PubMed] [Google Scholar]
- 63.Mayer RJ, Davis RB, Schiffer CA, Berg DT, Powell BL, Schulman P, Omura GA, Moore JO, McIntyre OR, Frei E 3rd. Intensive postremission chemotherapy in adults with acute myeloid leukemia. Cancer and Leukemia Group B. N Engl J Med. 1994 Oct 6;331:896–903. doi: 10.1056/NEJM199410063311402. [DOI] [PubMed] [Google Scholar]
- 64.Stone RM, Berg DT, George SL, Dodge RK, Paciucci PA, Schulman PP, Lee EJ, Moore JO, Powell BL, Baer MR, Bloomfield CD, Schiffer CA. Postremission therapy in older patients with de novo acute myeloid leukemia: a randomized trial comparing mitoxantrone and intermediate-dose cytarabine with standard-dose cytarabine. Blood. 2001 Aug 1;98:548–553. doi: 10.1182/blood.v98.3.548. [DOI] [PubMed] [Google Scholar]
- 65.Hassanein M, Atenafu EG, Schuh AC, Yee KW, Minden MD, Schimmer AD, Gupta V, Brandwein JM. High-dose cytarabine-based consolidation shows superior results for older AML patients with intermediate risk cytogenetics in first complete remission. Leuk Res. 2013 May;37:556–60. doi: 10.1016/j.leukres.2013.01.001. [DOI] [PubMed] [Google Scholar]
- 66.Burnett AK, Milligan D, Goldstone A, Prentice A, McMullin MF, Dennis M, Sellwood E, Pallis M, Russell N, Hills RK, Wheatley K. The impact of dose escalation and resistance modulation in older patients with acute myeloid leukaemia and high risk myelodysplastic syndrome: the results of the LRF AML14 trial. Br J Haematol. 2009 May;145:318–332. doi: 10.1111/j.1365-2141.2009.07604.x. [DOI] [PubMed] [Google Scholar]
- 67.Goldstone AH, Burnett AK, Wheatley K, Smith AG, Hutchinson RM, Clark RE Medical Research Council Adult Leukemia Working Party. Attempts to improve treatment outcomes in acute myeloid leukemia (AML) in older patients: the results of the United Kingdom Medical Research Council AML11 trial. Blood. 2001 Sep 1;98:1302–1311. doi: 10.1182/blood.v98.5.1302. [DOI] [PubMed] [Google Scholar]
- 68.Miyawaki S, Ohtake S, Fujisawa S, Kiyoi H, Shinagawa K, Usui N, Sakura T, Miyamura K, Nakaseko C, Miyazaki Y, Fujieda A, Nagai T, Yamane T, Taniwaki M, Takahashi M, Yagasaki F, Kimura Y, Asou N, Sakamaki H, Handa H, Honda S, Ohnishi K, Naoe T, Ohno R. A randomized comparison of 4 courses of standard-dose multiagent chemotherapy versus 3 courses of high-dose cytarabine alone in postremission therapy for acute myeloid leukemia in adults: the JALSG AML201 Study. Blood. 2011 Feb 24;117:2366–2372. doi: 10.1182/blood-2010-07-295279. [DOI] [PubMed] [Google Scholar]
- 69.Byrd JC, Dodge RK, Carroll A, Baer MR, Edwards C, Stamberg J, Qumsiyeh M, Moore JO, Mayer RJ, Davey F, Schiffer CA, Bloomfield CD. Patients with t(8;21)(q22;q22) and acute myeloid leukemia have superior failure-free and overall survival when repetitive cycles of high-dose cytarabine are administered. J. Clin. Oncol. 1999 Dec;17:3767–3775. doi: 10.1200/JCO.1999.17.12.3767. [DOI] [PubMed] [Google Scholar]
- 70.Byrd JC, Ruppert AS, Mrozek K, Carroll AJ, Edwards CG, Arthur DC, Pettenati MJ, Stamberg J, Koduru PRK, Moore JO, Mayer RJ, Davey FR, Larson RA, Bloomfield CD. Repetitive cycles of high-dose cytarabine benefit patients with acute myeloid leukemia and inv(16)(p13q22) or t(16;16)(p13;q22): results from CALGB 8461. J. Clin. Oncol. 2004 Mar 15;22:1087–94. doi: 10.1200/JCO.2004.07.012. [DOI] [PubMed] [Google Scholar]
- 71.Network NCC. NCCN Clinical Practice Guidelines in Oncology: National Comprehensive Cancer Network. 2012 Oct 21; doi: 10.6004/jnccn.2004.0021. [DOI] [PubMed] [Google Scholar]
- 72.Gardin C, Turlure P, Fagot T, Thomas X, Terre C, Contentin N, Raffoux E, de Botton S, Pautas C, Reman O, Bourhis JH, Fenaux P, Castaigne S, Michallet M, Preudhomme C, de Revel T, Bordessoule D, Dombret H. Postremission treatment of elderly patients with acute myeloid leukemia in first complete remission after intensive induction chemotherapy: results of the multicenter randomized Acute Leukemia French Association (ALFA) 9803 trial. Blood. 2007 Jun 15;109:5129–5135. doi: 10.1182/blood-2007-02-069666. [DOI] [PubMed] [Google Scholar]
- 73.Itzykson R, Gardin C, Pautas C, Thomas X, Turlure P, Raffoux E, Terré C, Fenaux P, Castaigne S, Dombret H, Boissel N Acute Leukemia French Association (ALFA) Impact of post-remission therapy in patients aged 65-70 years with de novo acute myeloid leukemia: a comparison of two concomitant randomized ALFA trials with overlapping age inclusion criteria. Haematologica. 2011 Jun;96:837–844. doi: 10.3324/haematol.2010.036921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lowenberg B, Suciu S, Archimbaud E, Haak H, Stryckmans P, de Cataldo R, Dekker AW, Berneman ZN, Thyss A, van der Lelie J, Sonneveld P, Visani G, Fillet G, Hayat M, Hagemeijer A, Solbu G, Zittoun R. Mitoxantrone versus daunorubicin in induction-consolidation chemotherapy--the value of low-dose cytarabine for maintenance of remission, and an assessment of prognostic factors in acute myeloid leukemia in the elderly: final report. European Organization for the Research and Treatment of Cancer and the Dutch-Belgian Hemato-Oncology Cooperative Hovon Group. J. Clin. Oncol. 1998 Mar;16:872–881. doi: 10.1200/JCO.1998.16.3.872. [DOI] [PubMed] [Google Scholar]
- 75.Sanz MA, Vellenga E, Rayón C, Díaz-Mediavilla J, Rivas C, Amutio E, Arias J, Debén G, Novo A, Bergua J, de la Serna J, Bueno J, Negri S, Beltrán de Heredia JM, Martín G. All-trans retinoic acid and anthracycline monochemotherapy for the treatment of elderly patients with acute promyelocytic leukemia. Blood. 2004;104:3490–3493. doi: 10.1182/blood-2004-04-1642. [DOI] [PubMed] [Google Scholar]
- 76.Disperati P, Minden MD, Gupta V, Schimmer AD, Schuh AC, Yee KW, Kamel-Reid S, Chang H, Xu W, Brandwein JM. Acute promyelocytic leukemia in patients aged 70 years and over -- a single center experience of unselected patients. Leuk Lymphoma. 2007;48:1654–1658. doi: 10.1080/10428190701472005. [DOI] [PubMed] [Google Scholar]
- 77.Adès L, Chevret S, Raffoux E, de Botton S, Guerci A, Pigneux A, Stoppa AM, Lamy T, Rigal-Huguet F, Vekhoff A, Meyer-Monard S, Maloisel F, Deconinck E, Ferrant A, Thomas X, Fegueux N, Chomienne C, Dombret H, Degos L, Fenaux P European Acute Promyelocytic Leukemia Group. Is cytarabine useful in the treatment of acute promyelocytic leukemia? Results of a randomized trial from the European Acute Promyelocytic Leukemia Group. J Clin Oncol. 2006;24:5703–5710. doi: 10.1200/JCO.2006.08.1596. [DOI] [PubMed] [Google Scholar]
- 78.Soignet SL, Frankel SR, Douer D, Tallman MS, Kantarjian H, Calleja E, Stone RM, Kalaycio M, Scheinberg DA, Steinherz P, Sievers EL, Coutré S, Dahlberg S, Ellison R, Warrell RPJ. United States multicenter study of arsenic trioxide in relapsed acute promyelocytic leukemia. J. Clin. Oncol. 2001;19:3852–3860. doi: 10.1200/JCO.2001.19.18.3852. [DOI] [PubMed] [Google Scholar]
- 79.Ghavamzadeh A, Alimoghaddam K, Rostami S, Ghaffari SH, Jahani M, Iravani M, Mousavi SA, Bahar B, Jalili M. Phase II study of single-agent arsenic trioxide for the front-line therapy of acute promyelocytic leukemia. J. Clin. Oncol. 2011;29:2753–2757. doi: 10.1200/JCO.2010.32.2107. [DOI] [PubMed] [Google Scholar]
- 80.Cornelissen JJ, van Putten WLJ, Verdonck LF, Theobald M, Jacky E, Daenen SMG, van Marwijk Kooy M, Wijermans P, Schouten H, Huijgens PC, van der Lelie H, Fey M, Ferrant A, Maertens J, Gratwohl A, Lowenberg B. Results of a HOVON/SAKK donor versus no-donor analysis of myeloablative HLA-identical sibling stem cell transplantation in first remission acute myeloid leukemia in young and middle-aged adults: benefits for whom? Blood. 2007 May 1;109:3658–3666. doi: 10.1182/blood-2006-06-025627. [DOI] [PubMed] [Google Scholar]
- 81.Jourdan E, Boiron JM, Dastugue N, Vey N, Marit G, Rigal-Huguet F, Molina L, Fegueux N, Pigneux A, Recher C, Rossi JF, Attal M, Sotto JJ, Maraninchi D, Reiffers J, Bardou VJ, Esterni B, Blaise D. Early allogeneic stem-cell transplantation for young adults with acute myeloblastic leukemia in first complete remission: an intent-to-treat long-term analysis of the BGMT experience. J. Clin. Oncol. 2005 Oct 20;23:7676–84. doi: 10.1200/JCO.2005.02.5940. [DOI] [PubMed] [Google Scholar]
- 82.Yanada M, Matsuo K, Emi N, Naoe T. Efficacy of allogeneic hematopoietic stem cell transplantation depends on cytogenetic risk for acute myeloid leukemia in first disease remission: a metaanalysis. Cancer. 2005 Apr 15;103:1652–1658. doi: 10.1002/cncr.20945. [DOI] [PubMed] [Google Scholar]
- 83.Kiss TL, Anderson H, Brinch L, Delage R, Finke J, Ljungman P, Remes K, Sabloff M, Spearing R. Allogeneic-related stem cell transplantation with reduced-intensity conditioning versus best standard of care in older patients with acute myeloid leukaemia in first complete remission. Interim analysis of a prospective multi center phase III trial. 36th Annual Meeting of the European Group for Blood and Marrow Transplantation. 2010 Mar 24; Vienna, Austria. [Google Scholar]
- 84.Koreth J, Aldridge J, Kim HT, Alyea EP 3rd, Cutler C, Armand P, Ritz J, Antin JH, Soiffer RJ, Ho VT. Reduced-intensity conditioning hematopoietic stem cell transplantation in patients over 60 years: hematologic malignancy outcomes are not impaired in advanced age. Biol Blood Marrow Transplant. 2010 Jun;16:792–800. doi: 10.1016/j.bbmt.2009.12.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.McClune BL, Weisdorf DJ, Pedersen TL, Tunes da Silva G, Tallman MS, Sierra J, Dipersio J, Keating A, Gale RP, George B, Gupta V, Hahn T, Isola L, Jagasia M, Lazarus H, Marks D, Maziarz R, Waller EK, Bredeson C, Giralt S. Effect of age on outcome of reduced-intensity hematopoietic cell transplantation for older patients with acute myeloid leukemia in first complete remission or with myelodysplastic syndrome. J. Clin. Oncol. 2010 Apr 10;28:1878–87. doi: 10.1200/JCO.2009.25.4821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Estey E, de Lima M, Tibes R, Pierce S, Kantarjian H, Champlin R, Giralt S. Prospective feasibility analysis of reduced-intensity conditioning (RIC) regimens for hematopoietic stem cell transplantation (HSCT) in elderly patients with acute myeloid leukemia (AML) and high-risk myelodysplastic syndrome (MDS) Blood. 2007 Feb 15;109:1395–1400. doi: 10.1182/blood-2006-05-021907. [DOI] [PubMed] [Google Scholar]
- 87.Kurosawa S, Yamaguchi T, Uchida N, Miyawaki S, Usuki K, Watanabe M, Yamashita T, Kanamori H, Tomiyama J, Nawa Y, Yano S, Takeuchi J, Yakushiji K, Sano F, Uoshima N, Yano T, Nannya Y, Moriuchi Y, Miura I, Takaue Y, Fukuda T. Comparison of allogeneic hematopoietic cell transplantation and chemotherapy in elderly patients with non-M3 acute myelogenous leukemia in first complete remission. Biol Blood Marrow Transplant. 2011 Mar;17:401–11. doi: 10.1016/j.bbmt.2010.07.013. [DOI] [PubMed] [Google Scholar]
- 88.Mohty M, de Lavallade H, Ladaique P, Faucher C, Vey N, Coso D, Stoppa AM, Gastaut JA, Blaise D. The role of reduced intensity conditioning allogeneic stem cell transplantation in patients with acute myeloid leukemia: a donor vs no donor comparison. Leukemia. 2005 Jun;19:916–920. doi: 10.1038/sj.leu.2403770. [DOI] [PubMed] [Google Scholar]
- 89.Gyurkocza B, Storb R, Storer BE, Chauncey TR, Lange T, Shizuru JA, Langston AA, Pulsipher MA, Bredeson CN, Maziarz RT, Bruno B, Petersen FB, Maris MB, Agura E, Yeager A, Bethge W, Sahebi F, Appelbaum FR, Maloney DG, Sandmaier BM. Nonmyeloablative allogeneic hematopoietic cell transplantation in patients with acute myeloid leukemia. J. Clin. Oncol. 2010 Jun 10;28:2859–67. doi: 10.1200/JCO.2009.27.1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wheatley K, Burnett AK, Goldstone AH, Gray RG, Hann IM, Harrison CJ, Rees JK, Stevens RF, Walker H. A simple, robust, validated and highly predictive index for the determination of risk-directed therapy in acute myeloid leukaemia derived from the MRC AML 10 trial. United Kingdom Medical Research Council’s Adult and Childhood Leukaemia Working Parties. Br J Haematol. 1999 Oct;107:69–79. doi: 10.1046/j.1365-2141.1999.01684.x. [DOI] [PubMed] [Google Scholar]
- 91.Chalandon Y, Barnett MJ, Horsman DE, Conneally EA, Nantel SH, Nevill TJ, Nitta J, Shepherd JD, Sutherland HJ, Toze CL, Hogge DE. Influence of cytogenetic abnormalities on outcome after allogeneic bone marrow transplantation for acute myeloid leukemia in first complete remission. Biol Blood Marrow Transplant. 2002;8:435–43. doi: 10.1053/bbmt.2002.v8.pm12234169. [DOI] [PubMed] [Google Scholar]
- 92.Schlenk RF, Döhner K, Krauter J, Fröhling S, Corbacioglu A, Bullinger L, Habdank M, Späth D, Morgan M, Benner A, Schlegelberger B, Heil G, Ganser A, Döhner H German-Austrian Acute Myeloid Leukemia Study Group. Mutations and treatment outcome in cytogenetically normal acute myeloid leukemia. N Engl J Med. 2008 May 1;358:1909–18. doi: 10.1056/NEJMoa074306. [DOI] [PubMed] [Google Scholar]
- 93.Bertz H, Potthoff K, Finke J. Allogeneic stem-cell transplantation from related and unrelated donors in older patients with myeloid leukemia. J. Clin. Oncol. 2003 Apr 15;21:1480–4. doi: 10.1200/JCO.2003.09.110. [DOI] [PubMed] [Google Scholar]
- 94.Gooley TA, Chien JW, Pergam SA, Hingorani S, Sorror ML, Boeckh M, Martin PJ, Sandmaier BM, Marr KA, Appelbaum FR, Storb R, McDonald GB. Reduced mortality after allogeneic hematopoietic-cell transplantation. N Engl J Med. 2010 Nov 25;363:2091–101. doi: 10.1056/NEJMoa1004383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Hegenbart U, Niederwieser D, Sandmaier BM, Maris MB, Shizuru JA, Greinix H, Cordonnier C, Rio B, Gratwohl A, Lange T, Al-Ali H, Storer B, Maloney D, McSweeney P, Chauncey T, Agura E, Bruno B, Maziarz RT, Petersen F, Storb R. Treatment for acute myelogenous leukemia by low-dose, total-body, irradiation-based conditioning and hematopoietic cell transplantation from related and unrelated donors. J. Clin. Oncol. 2006 Jan 20;24:444–53. doi: 10.1200/JCO.2005.03.1765. [DOI] [PubMed] [Google Scholar]
- 96.Shapira MY, Resnick IB, Bitan M, Ackerstein A, Samuel S, Elad S, Miron S, Zilberman I, Slavin S, Or R. Low transplant-related mortality with allogeneic stem cell transplantation in elderly patients. Bone Marrow Transplant. 2004 Jul;34:155–9. doi: 10.1038/sj.bmt.1704540. [DOI] [PubMed] [Google Scholar]
- 97.Wong R, Giralt SA, Martin T, Couriel DR, Anagnostopoulos A, Hosing C, Andersson BS, Cano P, Shahjahan M, Ippoliti C, Estey EH, McMannis J, Gajewski JL, Champlin RE, de Lima M. Reduced-intensity conditioning for unrelated donor hematopoietic stem cell transplantation as treatment for myeloid malignancies in patients older than 55 years. Blood. 2003 Oct 15;102:3052–3059. doi: 10.1182/blood-2003-03-0855. [DOI] [PubMed] [Google Scholar]
- 98.Schetelig J, Bornhauser M, Schmid C, Hertenstein B, Schwerdtfeger R, Martin H, Stelljes M, Hegenbart U, Schafer-Eckart K, Fussel M, Wiedemann B, Thiede C, Kienast J, Baurmann H, Ganser A, Kolb HJ, Ehninger G. Matched unrelated or matched sibling donors result in comparable survival after allogeneic stem-cell transplantation in elderly patients with acute myeloid leukemia: a report from the cooperative German Transplant Study Group. J. Clin. Oncol. 2008 Nov 10;26:5183–91. doi: 10.1200/JCO.2007.15.5184. [DOI] [PubMed] [Google Scholar]
- 99.Shimoni A, Kroger N, Zabelina T, Ayuk F, Hardan I, Yeshurun M, Shem-Tov N, Avigdor A, Ben-Bassat I, Zander AR, Nagler A. Hematopoietic stem-cell transplantation from unrelated donors in elderly patients (age >55 years) with hematologic malignancies: older age is no longer a contraindication when using reduced intensity conditioning. Leukemia. 2005 Jan;19:7–12. doi: 10.1038/sj.leu.2403591. [DOI] [PubMed] [Google Scholar]
- 100.Fenaux P, Mufti GJ, Hellstrom-Lindberg E, Santini V, Finelli C, Giagounidis A, Schoch R, Gattermann N, Sanz G, List A, Gore SD, Seymour JF, Bennett JM, Byrd J, Backstrom J, Zimmerman L, McKenzie D, Beach C, Silverman LR International Vidaza High-Risk MDS Survival Study Group. Efficacy of azacitidine compared with that of conventional care regimens in the treatment of higher-risk myelodysplastic syndromes: a randomised, open-label, phase III study. Lancet Oncol. 2009 Mar;10:223–232. doi: 10.1016/S1470-2045(09)70003-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Fenaux P, Mufti GJ, Hellstrom-Lindberg E, Santini V, Gattermann N, Germing U, Sanz G, List AF, Gore S, Seymour JF, Dombret H, Backstrom J, Zimmerman L, McKenzie D, Beach CL, Silverman LR. Azacitidine prolongs overall survival compared with conventional care regimens in elderly patients with low bone marrow blast count acute myeloid leukemia. J. Clin. Oncol. 2010 Feb 1;28:562–9. doi: 10.1200/JCO.2009.23.8329. [DOI] [PubMed] [Google Scholar]
- 102.Itzykson R, Thepot S, Quesnel B, Dreyfus F, Beyne-Rauzy O, Turlure P, Vey N, Recher C, Dartigeas C, Legros L, Delaunay J, Salanoubat C, Visanica S, Stamatoullas A, Isnard F, Marfaing-Koka A, de Botton S, Chelghoum Y, Taksin AL, Plantier I, Ame S, Boehrer S, Gardin C, Beach CL, Ades L, Fenaux P Groupe Francophone des Myelodysplasies(GFM) Prognostic factors for response and overall survival in 282 patients with higher-risk myelodysplastic syndromes treated with azacitidine. Blood. 2011 Jan 13;117:403–411. doi: 10.1182/blood-2010-06-289280. [DOI] [PubMed] [Google Scholar]
- 103.Al-Ali HK, Jaekel N, Junghanss C, Maschmeyer G, Krahl R, Cross M, Hoppe G, Niederwieser D. Azacitidine in patients with acute myeloid leukemia medically unfit for or resistant to chemotherapy: a multicenter phase I/II study. Leuk Lymphoma. 2012 Jan;53:110–117. doi: 10.3109/10428194.2011.606382. [DOI] [PubMed] [Google Scholar]
- 104.Kantarjian HM, Thomas XG, Dmoszynska A, Wierzbowska A, Mazur G, Mayer J, Gau JP, Chou WC, Buckstein R, Cermak J, Kuo CY, Oriol A, Ravandi F, Faderl S, Delaunay J, Lysak D, Minden M, Arthur C. Multicenter, Randomized, Open-Label, Phase III Trial of Decitabine Versus Patient Choice, With Physician Advice, of Either Supportive Care or Low-Dose Cytarabine for the Treatment of Older Patients With Newly Diagnosed Acute Myeloid Leukemia. J. Clin. Oncol. 2012 Jun 11;30:2670–2677. doi: 10.1200/JCO.2011.38.9429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Kuendgen A, Schmid M, Schlenk R, Knipp S, Hildebrandt B, Steidl C, Germing U, Haas R, Dohner H, Gattermann N. The histone deacetylase (HDAC) inhibitor valproic acid as monotherapy or in combination with all-trans retinoic acid in patients with acute myeloid leukemia. Cancer. 2006 Jan 1;106:112–119. doi: 10.1002/cncr.21552. [DOI] [PubMed] [Google Scholar]
- 106.Raffoux E, Cras A, Recher C, Boelle PY, de Labarthe A, Turlure P, Marolleau JP, Reman O, Gardin C, Victor M, Maury S, Rousselot P, Malfuson JV, Maarek O, Daniel MT, Fenaux P, Degos L, Chomienne C, Chevret S, Dombret H. Phase 2 clinical trial of 5-azacitidine, valproic acid, and all-trans retinoic acid in patients with high-risk acute myeloid leukemia or myelodysplastic syndrome. Oncotarget. 2010 May;1:34–42. doi: 10.18632/oncotarget.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Corsetti MT, Salvi F, Perticone S, Baraldi A, De Paoli L, Gatto S, Pietrasanta D, Pini M, Primon V, Zallio F, Tonso A, Alvaro MG, Ciravegna G, Levis A. Hematologic improvement and response in elderly AML/RAEB patients treated with valproic acid and low-dose Ara-C. Leukemia Research. 2011 Aug;35:991–997. doi: 10.1016/j.leukres.2011.02.021. [DOI] [PubMed] [Google Scholar]
- 108.Giles F, Rizzieri D, Karp J, Vey N, Ravandi F, Faderl S, Khan KD, Verhoef G, Wijermans P, Advani A, Roboz G, Kantarjian H, Bilgrami SF, Ferrant A, Daenen SM, Karsten V, Cahill A, Albitar M, Mufti G, O’Brien S. Cloretazine (VNP40101M), a novel sulfonylhydrazine alkylating agent, in patients age 60 years or older with previously untreated acute myeloid leukemia. J. Clin. Oncol. 2007 Jan 1;25:25–31. doi: 10.1200/JCO.2006.07.0961. [DOI] [PubMed] [Google Scholar]
- 109.Brandwein JM, Yang L, Schimmer AD, Schuh AC, Gupta V, Wells RA, Alibhai SM, Xu W, Minden MD. A phase II study of temozolomide therapy for poor-risk patients aged >or=60 years with acute myeloid leukemia: low levels of MGMT predict for response. Leukemia. 2007;21:821–824. doi: 10.1038/sj.leu.2404545. [DOI] [PubMed] [Google Scholar]
- 110.Amadori S, Suciu S, Selleslag D, Stasi R, Alimena G, Baila L, Rizzoli V, Borlenghi E, Gaidano G, Magro D, Torelli G, Muus P, Venditti A, Cacciola E, Lauria F, Vignetti M, de Witte T. Randomized trial of two schedules of low-dose gemtuzumab ozogamicin as induction monotherapy for newly diagnosed acute myeloid leukaemia in older patients not considered candidates for intensive chemotherapy. A phase II study of the EORTC and GIMEMA leukaemia groups (AML-19) Br J Haematol. 2010 May;149:376–82. doi: 10.1111/j.1365-2141.2010.08095.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Lancet JE, Gojo I, Gotlib J, Feldman EJ, Greer J, Liesveld JL, Bruzek LM, Morris L, Park Y, Adjei AA, Kaufmann SH, Garrett-Mayer E, Greenberg PL, Wright JJ, Karp JE. A phase 2 study of the farnesyltransferase inhibitor tipifarnib in poor-risk and elderly patients with previously untreated acute myelogenous leukemia. Blood. 2007 Feb 15;109:1387–1394. doi: 10.1182/blood-2006-04-014357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Schiller GJ, O’Brien SM, Pigneux A, Deangelo DJ, Vey N, Kell J, Solomon S, Stuart RK, Karsten V, Cahill AL, Albitar MX, Giles FJ. Single-agent laromustine, a novel alkylating agent, has significant activity in older patients with previously untreated poor-risk acute myeloid leukemia. J. Clin. Oncol. 2010 Feb 10;28:815–21. doi: 10.1200/JCO.2009.24.2008. [DOI] [PubMed] [Google Scholar]
- 113.Godwin JE, Kopecky KJ, Head DR, Willman CL, Leith CP, Hynes HE, Balcerzak SP, Appelbaum FR. A double-blind placebo-controlled trial of granulocyte colony-stimulating factor in elderly patients with previously untreated acute myeloid leukemia: a Southwest oncology group study (9031) Blood. 1998 May 15;91:3607–3615. [PubMed] [Google Scholar]
- 114.Bello C, Yu D, Komrokji RS, Zhu W, Wetzstein GA, List AF, Lancet JE. Outcomes after induction chemotherapy in patients with acute myeloid leukemia arising from myelodysplastic syndrome. Cancer. 2011 Apr 1;117:1463–1469. doi: 10.1002/cncr.25598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Stolzel F, Pfirrmann M, Aulitzky WE, Kaufmann M, Bodenstein H, Bornhauser M, Rollig C, Kramer M, Mohr B, Oelschlagel U, Schmitz N, Soucek S, Thiede C, Ehninger G, Schaich M Study Alliance Leukemia. Risk stratification using a new prognostic score for patients with secondary acute myeloid leukemia: results of the prospective AML96 trial. Leukemia. 2011 Mar;25:420–428. doi: 10.1038/leu.2010.279. [DOI] [PubMed] [Google Scholar]
- 116.Koh Y, Kim I, Bae JY, Song EY, Kim HK, Yoon SS, Lee DS, Park SS, Park MH, Park S, Kim BK. Prognosis of secondary acute myeloid leukemia is affected by the type of the preceding hematologic disorders and the presence of trisomy 8. Jpn J Clin Oncol. 2010 Nov;40:1037–45. doi: 10.1093/jjco/hyq097. [DOI] [PubMed] [Google Scholar]
- 117.van der Holt B, Breems DA, Berna Beverloo H, van den Berg E, Burnett AK, Sonneveld P, Lowenberg B. Various distinctive cytogenetic abnormalities in patients with acute myeloid leukaemia aged 60 years and older express adverse prognostic value: results from a prospective clinical trial. Br J Haematol. 2007 Jan;136:96–105. doi: 10.1111/j.1365-2141.2006.06403.x. [DOI] [PubMed] [Google Scholar]
- 118.Appelbaum FR, Gundacker H, Head DR, Slovak ML, Willman CL, Godwin JE, Anderson JE, Petersdorf SH. Age and acute myeloid leukemia. Blood. 2006 May 1;107:3481–3485. doi: 10.1182/blood-2005-09-3724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Anderson JE, Kopecky KJ, Willman CL, Head D, O’Donnell MR, Luthardt FW, Norwood TH, Chen IM, Balcerzak SP, Johnson DB, Appelbaum FR. Outcome after induction chemotherapy for older patients with acute myeloid leukemia is not improved with mitoxantrone and etoposide compared to cytarabine and daunorubicin: a Southwest Oncology Group study. Blood. 2002 Dec 1;100:3869–3876. doi: 10.1182/blood-2001-12-0354. [DOI] [PubMed] [Google Scholar]
- 120.van der Holt B, Lowenberg B, Burnett AK, Knauf WU, Shepherd J, Piccaluga PP, Ossenkoppele GJ, Verhoef GE, Ferrant A, Crump M, Selleslag D, Theobald M, Fey MF, Vellenga E, Dugan M, Sonneveld P. The value of the MDR1 reversal agent PSC-833 in addition to daunorubicin and cytarabine in the treatment of elderly patients with previously untreated acute myeloid leukemia (AML), in relation to MDR1 status at diagnosis. Blood. 2005 Oct 15;106:2646–2654. doi: 10.1182/blood-2005-04-1395. [DOI] [PubMed] [Google Scholar]
- 121.Löwenberg B, Ossenkoppele GJ, van Putten W, Schouten HC, Graux C, Ferrant A, Sonneveld P, Maertens J, Jongen-Lavrencic M, von Lilienfeld-Toal M, Biemond BJ, Vellenga E, van Marwijk Kooy M, Verdonck LF, Beck J, Döhner H, Gratwohl A, Pabst T, Verhoef G Dutch-Belgian Cooperative Trial Group for Hemato-Oncology (HOVON); German AML Study Group (AMLSG); Swiss Group for Clinical Cancer Research (SAKK) Collaborative Group. High-dose daunorubicin in older patients with acute myeloid leukemia. N Engl J Med. 2009 Sep 24;361:1235–48. doi: 10.1056/NEJMoa0901409. [DOI] [PubMed] [Google Scholar]


