EXECUTIVE SUMMARY
As a field that has emerged in recent years, from multidisciplinary roots within long-standing, traditional academic infrastructures, sleep medicine has assumed highly disparate organizational structures at each institution. Access to the creativity, talent, trainees, administration, and financial investment of one or more departments at each medical center has contributed substantially to advances in sleep and biological rhythms. At the same time, however, the variability of the support structure across institutions and the ability of specific departments to develop only the most relevant aspects of a highly multidisciplinary field has substantially limited the growth of sleep medicine. Surveys in 2009 and 2012 by a Presidential Task Force of the Sleep Research Society suggested that strong, independent, self-sufficient, and cohesive administrative structures for sleep medicine were rare, if not absent. Little progress had been made toward organizational structures envisioned in the 2006 Institute of Medicine report, Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem.
This white paper, written by members of the Academic Affairs Committee and then endorsed by the Boards of Directors of both the American Academy of Sleep Medicine and the Sleep Research Society, summarizes challenges to sleep medicine that arise at academic institutions. Examples of specific challenges discussed include the absence or rarity of: sleep center responsibility for sleep faculty recruitment; recruitment packages targeted for sleep; salary equity for identical work within the same sleep center by members of different departments; better equity between academic and nonacademic salaries; reinvestment of clinical or other margins back into sleep; access by qualified individuals to academic positions regardless of original specialty training before sleep; oversight of research space and resources by sleep centers; department-blind access to trainees who stand to gain most from training in sleep medicine; coordinated training in sleep and biological rhythms during preclinical medical school curricula; and sleep graduate training programs and opportunities to attract next-generation researchers into sleep and biological rhythms. Solutions to such challenges are complex and likely to differ between medical centers that themselves often have highly disparate organizational structures. However, a white paper subsequent to this one describes key goals that could be targeted, along with potential mechanisms to help ensure financial and administrative feasibility. The outline of current challenges in this paper, and a future vision and potential solutions in the next, are designed to maximize the potential that academic sleep medicine could have during coming years to improve human health in a most fundamental manner.
1. INTRODUCTION: NEED AND GOALS FOR WHITE PAPERS
Sleep medicine and the science that underlies it represent a relatively new medical discipline that has emerged in part based on combined contributions made by a wide variety of traditional fields. These fields have enjoyed long-established financial, administrative, institutional, and federal support that has fueled much of the growth and early success in sleep and biological rhythms. However, at the institutional level, traditional academic departments maintain most of their focus outside sleep. No traditional department or medical discipline covers the entire breadth of sleep medicine. No departments of sleep medicine exist at academic institutions, and sleep disorders centers rarely have significant oversight of budgets, faculty appointments, and space. This has limited development, visibility, coherent centralized planning, investment, and reinvestment in sleep medicine. In some circumstances current organizational structures do not facilitate optimal care for patients with sleep problems. They can constrain clinical training despite the high public health burden of sleep disorders, and hamper research training despite recognition of fundamental unanswered questions in this field.1 Current administrative structures often divert positive margin generated by sleep medicine away from academic development of sleep programs. Institutional investment in sleep typically remains minimal, and indirect funds from sleep grants rarely are committed to future research of this field. Collaboration between like-minded sleep investigators is diffi-cult because of physical distances and unrelated administrative structures within systems that provide little incentive to cross existing department silos.
This white paper, the first in a series of two, reflects the consensus of the American Academy of Sleep Medicine Academic Affairs Committee, with select external expertise, and is endorsed by both the American Academy of Sleep Medicine and the Sleep Research Society Boards of Directors. This first report examines existing organizational and structural features for academic sleep medicine in the United States, and identifies challenges that emerge from these realities. The second report defines targets and some pathways or structures that could create important progress. The overall goal is not to recommend restriction of sleep medicine from the myriad benefits it continues to receive from close affiliations with traditional specialties that form the roots of this new field. Rather, the aim is to preserve and enhance these collaborative relationships, but at the same time—and critically—encourage new institutional expectations for structural integrity that this field needs to fulfill its promise as a medical and scientific specialty able to deliver the most effective clinical care, train a capable and sufficient workforce, and contribute to fundamental advances in understanding of human health.
2. BACKGROUND
In 2008-9, the Sleep Research Society (SRS) appointed a task force to assess the status of research-oriented academic sleep centers. The SRS Board had identified institutional structures for academic sleep medicine and sleep science as a focus area of high priority, and the task force was asked to conduct a survey of existing structures so that results might inform plans for future recommendations. These efforts also arose in part as follow-up to the 2006 Institute of Medicine report on academic sleep research and sleep medicine in the United States.2
2.1. SRS Presidential Task Force Survey
The task force sent detailed questionnaires on administrative structure as well as clinical, teaching, research, and outreach activities to directors of identified sleep centers. The selected sleep centers were at academic medical centers that participated in a consortium of institutions with NIH-funded Clinical and Translational Science Awards (CTSAs). These institutions were targeted because their sleep disorders centers were considered likely to include many with well-developed academic programs. Completed questionnaires were received from 35 of 38 targeted centers. In May 2012, a few key questions were re-distributed to update the 2009 survey. These key questions focused on administrative and fiscal structures, faculty recruitment processes, training opportunities, research opportunities, and research funding. Updated information was received from 29 respondents.
2.1.1. Existing Structures
Variation in leadership structures between centers was considerable (Figure 1). In 2009 and 2012, about 11% to 12% of responding centers had a director who reported to a dean of a medical school. In 2009, about 18% of surveyed programs were headed by a division director who reported to a department chair, whereas by 2012 this number had increased to 30%. In 2009, 50% of respondents reported that their leadership structure fell into an “other” category. For example, several respondents described council-like structures with a multidisciplinary composition. Although this pattern was a little less prevalent in 2012, “other” remained the largest category choice.
Figure 1.
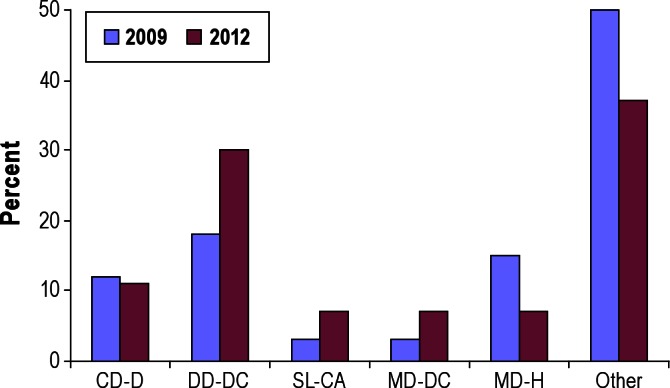
Sleep center leadership and reporting structures. From left to right, sleep center director reports directly to the dean (CD-D), the division director reports directly to the department chair (DD-DC), separate leadership of clinical and academic programs (SL-CA), medical director reports to departmental chair (MD-DC), medical director reports to hospital leadership (MD-H), or another reporting structure (Other).
In 2009, about half of the centers reported a medical school or university-based administrative structure responsible for the clinical, academic, and teaching missions. More than one clinical sleep program existed in 14 of 35 institutions, with 11 of these 14 representing separate pediatric sleep medicine programs. Five programs consisted of a clinical sleep center run by a hospital, with no specific or integrated oversight of institutional sleep research and education.
In 2009, 50% of surveyed centers described themselves as medical school or university-based comprehensive centers responsible for clinical, educational, and research missions; 26% of surveyed centers were divisions or sections within departments, usually within medicine or a section within pulmonary medicine, with slightly under half of these centers in departments of neurology. About 9% described hybrid, or combined model structures. In 2012, 29% of centers were described as comprehensive centers existing within a medical school or university, whereas 54% were described as divisions or sections within departments. Again, hybrid structures were reported by about 14% of respondents. The updated survey results found that just over two-thirds of programs in departments were in divisions of pulmonary and critical care within departments of medicine.
In 2009, 10 programs had one director that reported to a chair or dean. Other programs had multiple directors for various components of the program or multiple reporting lines, creating apparent potential for administrative and programmatic fragmentation. A hospital or private contractor was responsible for managing the sleep laboratory for 19 of the 35 responding programs. Technical revenues did not flow through the sleep programs in about half the programs. In 2009, only 5 among 35, or about 14% of programs reported an ability to recruit and appoint faculty. By 2012, the percentage of programs who reported ability to recruit and appoint faculty climbed slightly, to 25%. However, at all other sleep centers, department chairs were responsible for recruiting faculty, suggesting that many sleep center directors have little or no direct oversight of program development.
Administrative responsibility for research grants was reported by only 12 (34%) of 35 institutions in 2009. Only 20% of these programs, all at CTSA-supported institutions, received any indirect costs from grants. In 2012, 37% reported receiving some indirect costs from grants. Figure 2 shows the percentage of programs that received revenues directly from the following sources in 2009 (lilac) and 2012 (fuchsia): professional revenues (prof), technical revenues (tech), indirect costs associated with grant funds (IDC), graduate medical education income (GME), training grants, revenue sharing mechanism with a private management contractor, other institutional funds to support the academic mission, and operational funds from the department or from the hospital. Results suggest highly disparate levels of access to revenue generated though sleep center activity. Access to professional fees was the most frequently reported, but approximately 25% of centers reported that they lacked even this benefit from their own activity.
Figure 2.
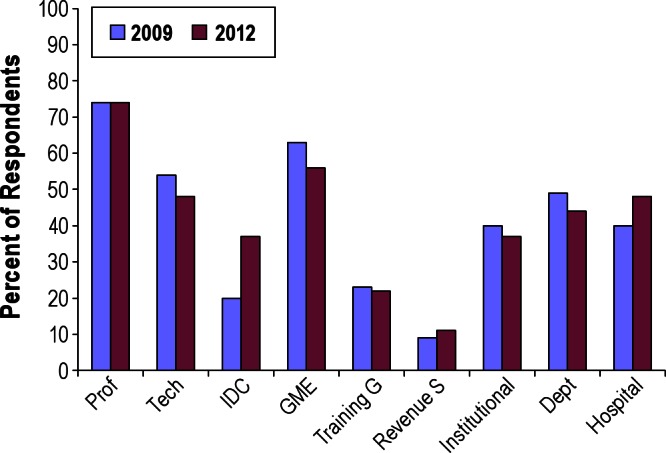
Revenue sources flowing directly through sleep programs. From left to right are shown the percent of respondents in 2009 and then 2012 that indicated professional fees (Prof), technical fees (Tech), indirect grant dollars (IDC), graduate medical education (GME), training grant income (Training G), revenue sharing (Revenue S), institutional revenue (Institutional), departmental revenue (Dept), and hospital revenue (Hospital).
2.1.2. Patient Care
In the more extensive survey completed in 2009, centers reported an average of 6 clinical faculty boarded in sleep medicine and one behavioral sleep medicine specialist. All of the centers had participation of pulmonary sleep faculty, 94% had participation of neurology sleep faculty, and 71% had psychology/behavioral sleep medicine faculty. Other disciplines that were represented in at least half of the centers included internal medicine, pediatrics, psychiatry, surgery, and dentistry. Surprisingly, only 31% of centers reported participation of nursing.
2.1.3. Education
In 2009, most centers reported major educational activities. However, less than half reported running undergraduate or graduate courses in basic sleep science, despite the fact that about half of the centers had graduate students and postdoctoral (PhD) fellows. About three-fourths of the programs reported complete responsibility for clinical sleep education at their institutions, and the remaining programs reported partial responsibility. All programs were highly involved in medical school and clinical postgraduate education. More than three-fourths reported having clinical fellows, and just over a third reported teaching clinical graduate school courses. For research education, half of the programs reported graduate student trainees and PhD postdoctoral trainees. In 2009, about 20% of programs reported having sleep-specific training grants, and this number remained the same in 2012. In 2009, two programs provided about 75% of the 50 total available training slots in sleep research at all the sites.
2.1.4. Research Activity
Most but not all centers had active sleep research programs (Figure 3). Less than one-fourth of programs reported having a current NIH center or program project grant (PPG), but over two-thirds of sites had at least one active R01 award for sleep research. Between 2009 and 2012, K-series grants and industry-supported grants appear to have diminished, whereas awards from the American Academy of Sleep Medicine or Sleep Research Society increased. For clinical research, more than half of programs surveyed reported participation in federally funded multi-site research studies. Surveyed programs on average each had slightly less than 3 basic researchers. In comparison to clinical research, basic research was less consistently represented across centers.
Figure 3.
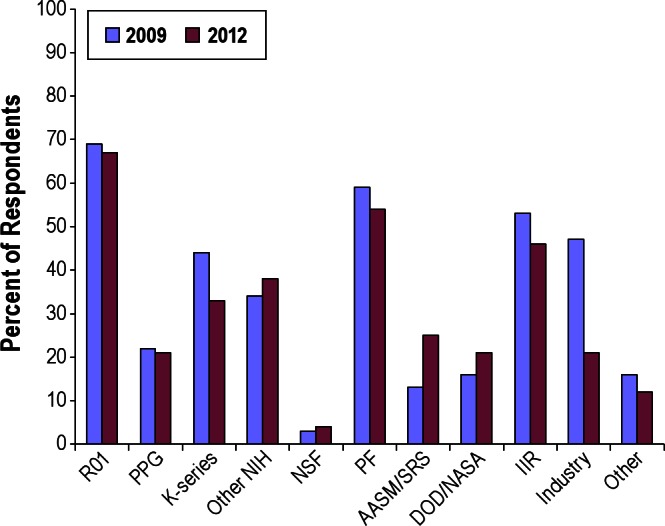
Research funding sources that centers reported, starting from the left with National Institutes of Health (research project support [R01]), program project grant (PPG), mentored research grants (K-series), other NIH grant mechanisms (Other NIH), National Science Foundation (NSF), private foundations (PF), American Academy of Sleep Medicine or Sleep Research Society (AASM/SRS), National Defense and NASA funds (DOD/NASA), industry-sponsored investigator-initiated research (IIR), industry-initiated research such as clinical trials (Industry), and other sources including donations and other forms of institutional grants (Other).
2.1.5. Implications of Survey Results
One striking observation from this group of 35 sleep centers sampled from institutions with CTSAs, located at many of the nation's top-ranked academic medical centers, is that their administrative infrastructures were highly disparate. Strong, independent, self-sufficient, and cohesive administrative structures were rare, if not absent. These sleep centers generally did not have oversight over revenue derived from clinical activities, technical laboratory fees, or grants, nor did they typically receive guaranteed support for academic activities from the medical school, hospital, or physician practice groups. This situation is despite the fact that these centers were at institutions with CTSAs, half of which had sleep research cores supported by their CTSAs. Moreover, survey results revealed a distinct absence of a mechanism by which the multidisciplinary sleep field could develop independently of the department or departments that gave rise to the center at each institution. The result is that faculty cannot be recruited and promoted within the sleep center, but only in accordance with perceived needs and priorities of various parent departments and the traditional disciplines of origin that each does (or does not) represent.
2.2. Institute of Medicine Report and Aftermath
In 2006, the landmark Institute of Medicine report, Sleep Disorders and Sleep Deprivation: an Unmet Public Health Need,2 highlighted some strategies proposed to advance sleep medicine and research, and called for specific commitments to the following:
Increase awareness of the burden of sleep loss and sleep disorders among the general public by developing a multimedia, comprehensive education campaign on the health and economic impact of sleep loss and sleep disorders.
Expand awareness among health care professionals through education and training.
Establish the workforce required to meet the clinical and scientific demands of the field.
Develop and validate existing diagnostic and therapeutic technologies.
Expand accreditation criteria to emphasize treatment, long-term patient care, and chronic disease management strategies.
Increase investment in interdisciplinary sleep programs at academic health centers that emphasize long-term clinical care, training, and research.
Create a national research network that connects individual investigators, research programs, and research centers.
The report also envisioned attributes of 3 types of interdisciplinary academic sleep programs, designed to provide clinical care (Type I); care, training, and research (Type II); and additional capacity for regional coordination of multicenter research trials (Type III). In the years since this report however, no organized national effort has emerged to foster, recognize, or accredit structures that would follow these models. Moreover, the Institute of Medicine report was generally not specific or proscriptive with regard to intra-institutional administrative structures for sleep medicine.
In 2006 and 2007, published opinion pieces by Drs. Michael Silber and Allan Pack highlighted potential advantages of departmental or center-based models for sleep medicine.3,4 Through its Academic Affairs Committee, the AASM created a program to recognize Comprehensive Academic Sleep Programs of Distinction that met pre-specified criteria for strong and exemplary clinical, educational, and research achievements. Emerging visions that were discussed for future academic sleep programs pointed toward interdisciplinary academic units, established as independent entities outside traditional divisions and departments. These units would encompass patient care, research, and educational missions; report directly to institutional leadership; plan sleep faculty recruitment; and oversee budgets related to each of these activities. As few sleep programs were likely to have evolved sufficiently to meet these criteria, requirements for recognition as a Program of Distinction initially emphasized comprehensiveness and integration rather than administrative independence. Plans were envisioned to expand requirements gradually and thereby foster administrative independence in the future. However, after several years, only six sleep programs nationally—at the University of Louisville, Brigham and Women's Hospital, University of Michigan, Wayne State University, Boston Children's Hospital, and University of Washington— had submitted an application and qualified for recognition as a Program of Distinction. In 2012, the AASM Board voted to sunset recognition of Programs of Distinction in favor of other efforts, such as this set of white papers, to move the structural evolution of this academic field forward.
3. CHALLENGES INHERENT TO EXISTING INFRASTRUCTURE
3.1. An Over-Arching Challenge
Sleep centers have often evolved at academic medical systems in a manner that has seemed more opportunistic and haphazard than thoughtfully planned and based on a vision for an ideal structure. Sleep centers are generally based at academic hospitals, often with no parallel inroads or structure at affiliated medical schools. Sleep centers generally accommodate a sleep center faculty only through the traditional department of his or her primary training, rather than a distinct academic sleep unit. As a result of this inherently disjointed basis for academic appointments and activities, several critical, practical challenges have arisen.
First, sleep programs are most often housed within large traditional departments, to which all revenue from clinical, research, and teaching activities flows. Whether and how revenues generated by the sleep program lead to reinvestment into the sleep program is rarely clear. Almost always, decisions about how to direct discretionary resources are not made by sleep specialists. Choices usually are made by senior physician leaders with unquestionably good intent, but limited training in, or exposure to, sleep medicine.5–8 Other choices are made by administrators who are often unaware that sleep medicine and sleep science could offer profound return on investment for human health and overall cost-effectiveness of medical care. As a practical result, sleep scientists and researchers often lack access to institutional allocations for programmatic development, funds from indirect costs of federal grants, chair packages, tuition dollars, and clinical margin. Access to these resources is more often reserved for traditional departments.
The need to break down traditional departmental silos, foster multidisciplinary research, and optimize interdisciplinary patient care has been broadly endorsed, in principle. Existing administrative “center” structures that aim to accomplish this, however, have often been more “virtual” than actual, lacking responsibility for anything beyond enhanced communication between faculty members. For example, sleep centers have not often: (1) served as cost and revenue centers, (2) exercised oversight over academic space assignments, aside from the sleep laboratory or clinic, or (3) taken primary responsibility for sleep faculty recruitment, appointments, and promotions. The cancer center model with assistance from the NIH has been a successful paradigm, based on a “four walls” approach to budgets in which funds enter and leave the centers directly, rather than through traditional component departments of medical schools or health systems. Unfortunately, the cancer center model has seldom been available to sleep centers.
The academic evolutionary process, instead of actively producing similar structures and “homes” across many institutions, has sometimes impeded collaboration and communication among sleep centers that do not share basic features. The disparity of infrastructure and organization has limited development of a unified field. Whereas chairs of neurology departments from around the country can meet annually to discuss challenges, advances, or collaborations with reasonable commonality of duties and responsibilities, directors of academic sleep programs typically find this more difficult. Each leader of a sleep program would find himself or herself in a nearly unique position, dependent on local historical vagaries. Collaboration between sleep program leaders is encumbered by their different background disciplines and departmental affiliations, highly variable responsibility for research, and frequently minimal levels of responsibility for budgets, science, and education. Whereas at a few institutions, directors of sleep disorders centers are highly involved with research in preclinical through translational and clinical areas, most directors have involvement only with clinical research efforts, if any. Preclinical sleep and rhythms science may have no administrative or structural ties whatsoever to the sleep disorders center or to the department that houses the sleep center.
The department or division that houses a sleep center all too often complicates the appointment of multidisciplinary sleep specialists. Pressure can arise on sleep disorders centers to hire faculty whose backgrounds match those of the parent department, even though the best interest of a sleep disorders center is often to hire sleep faculty from a wide range of backgrounds. The home department of the sleep program may not recognize the value in hiring outside their own discipline. Some departments are not permitted to hire outside their primary fields, even if prospective sleep faculty focus entirely on sleep medicine or sleep science that is practiced or researched without difference between those trained in one “primary” field or another. A sleep program that aims to recruit a sleep physician trained in family practice, for example, may find difficulty in obtaining this appointment through the department of family practice, which generally does not hire highly specialized physicians; through pulmonary medicine, which hires only pulmonologists; or through any other traditional department. All sleep medicine fellows are trained to see both adults and children with sleep problems, yet credentialing processes upon subsequent hiring may constrain faculty to see only one age group or the other.
Finally, whereas crosstalk between preclinical, human, translational, and clinical sleep researchers can provide a most stimulating and productive collaborative environment for innovative advances, these types of researchers cannot often be accommodated within the same traditional department at medical schools and medical centers. This situation stands in contrast to arrangements for many other traditional fields, where the necessity for shoulder-to-shoulder interaction between researchers at all segments of the preclinical-to-clinical spectrum has long been recognized. Although “Grand Rounds” often brings opportunities for preclinical scientists to speak to clinical colleagues with related interests, or vice versa, most existing Grand Rounds are supported by traditional departments. Sleep topics in the series are often few and far between, and each sleep specialist—preclinical, translational, or clinical—ends up having more interaction with members of his or her parent department than with many other sleep-interested faculty.
3.2. Challenges to Clinical Care
Existing administrative structures at academic institutions often do not promote optimal patient care for patients with sleep disorders. Patients who have serious sleep problems often remain unreferred, undiagnosed, and untreated.9,10 In part, this reflects the dearth of sleep medicine in medical school curricula and textbooks,6–8 but in addition, non-sleep specialist physicians and patients who seek sleep medicine services sometimes face a complicated series of options among sleep services offered by different departments. Where a patient is ultimately referred can be based on random historical factors, departmental affiliations, or haphazard personal acquaintances. Referrals may be made based on erroneous assumptions, for example, that a board-certified sleep physician with pulmonary background is better trained than others to treat obstructive sleep apnea; that a board-certified sleep physician with neurology background is better prepared to address restless legs syndrome; or that a board-certified sleep physician with psychiatric background is better prepared to address insomnia. Whereas a large, academic, multidisciplinary sleep center may indeed capitalize on diverse sleep specialists' “primary” training for particularly challenging, relatively rare cases, the large majority of patients referred to a sleep disorders center benefit from the clinician's broad expertise in sleep medicine, not another traditional field. All ACGME-approved sleep training, board certification, and accreditation procedures are now designed to ensure that every physician sleep specialist, regardless of background training, can see and treat patients with the full range of conditions that affect sleep and alertness.
When sleep services are offered through multiple separate departments, support staff have less concentrated opportunity to develop sleep-focused expertise and to optimize their skills. For example, frequent staff interaction with providers of durable medical equipment improves familiarity with required processes, and augments staff abilities to educate, anticipate questions, and problem solve difficulties. If this interaction is spread into smaller portions among staff at multiple clinics, the opportunity to streamline an effective system can remain elusive.
The provision of sleep services through different settings and departments at the same academic medical institution can lead to disparate reimbursement for identical services. Physician salaries are often based on background training or department affiliation, rather than specific work performed or expertise required in sleep medicine. For example, for an interpretation of a given sleep study in a given sleep laboratory, an otolaryngology sleep specialist may be reimbursed more than a psychiatry sleep specialist with equivalent seniority. Furthermore, many academic sleep specialists are reimbursed considerably less than those in private practice. Although this discrepancy is common to many areas of medicine, the difference can be exacerbated in sleep medicine when this somewhat procedure-based field is not recognized as distinct from the field of the parent department. For example, a neurology sleep specialist may be compensated equitably in comparison to other neurology department members, based on published neurology salaries, but inequitably in comparison to published sleep specialist salaries.
Finally, academic job opportunities for sleep specialists are often limited, not by their clinical or research interests, but by their original area of “primary” specialization. A psychiatrist may not be a candidate for a position in a pulmonary-based sleep center, whether or not his or her expertise is otherwise optimal for the work involved. This constraint greatly limits the ability of academic sleep centers to ensure a diversified, most effective faculty distribution that can maximize research opportunities, add educational value for trainees, and assure specialized expertise for complicated tertiary care referrals.
3.3. Challenges to Education
Challenges to education in sleep medicine begin in medical school, largely as a consequence of inadequate recognition of sleep and biological rhythms as a distinct field. Didactic sleep training is typically fragmented during the first two years of medical school. Obstructive sleep apnea, for example, may be covered during a course on pulmonary physiology, insomnia presented in a psychiatry sequence, and parasomnias taught in a neurosciences unit. A student could complete the first two years of training without being introduced to the concept that a medical sleep specialist can and does diagnose and treat the entire range of conditions that affect sleep and alertness. In the last two years of medical school, the absence of rotations through an integrated sleep medicine experience does not allow students to rectify their initial impression, or obtain a glimpse of what specialization in sleep medicine might be like. At the residency level, few programs spend dedicated time focused on sleep medicine. Few if any anesthesiology, family practice, internal medicine, neurology, otolaryngology, pediatrics, or psychiatry residencies—one of which is a prerequisite prior to a sleep fellowship—require or recommend a rotation through sleep medicine. Neurology residents are required to rotate through EEG laboratories but not sleep laboratories, even though sleep apnea alone is several times more prevalent than epilepsy.
The existing structure for sleep medicine fellowships is often less than ideal. In contrast to most other fellowship training programs, sleep medicine training lasts only one year. A one-year clinical fellowship rarely allows time to pursue research opportunities. Sleep fellow backgrounds can vary widely, from anesthesiology to family medicine or otolaryngology, as noted above. The one year of sleep medicine clinical training cannot provide all the relevant missing background to any individual trainee. The often-stated goal of training a sleep physician to diagnose and treat any disorder affecting sleep and alertness is challenging to achieve given the highly varied backgrounds and differing educational needs of the individuals entering the program. To some extent, the opportunities and experiences offered to fellows may be circumscribed by the walls of a “home department” that houses the sleep fellowship. This circumstance arises especially when fellows are supported by a department that must collect revenue from the trainees' clinical activity to justify their salary support. In many institutions, sleep fellows are not funded through institutional ACGME funds, and parent departments must often support the costs, sometimes with “strings attached.” Unfortunately, after the ACGME approved a one-year sleep medicine fellowship, medical institutions rarely reallocated GME-funded training slots accordingly; many sleep fellowships still rely on less traditional sources of funding that do not give the training program director complete discretion to apportion learning experiences according to optimal sleep educational priorities.
At present, this Committee is unaware of any graduate training programs specifically focused on sleep research. Although critical masses of faculty who identify themselves primarily as sleep researchers exist at growing numbers of institutions, none has organized a graduate training program focused on sleep and rhythms. Furthermore, few established multidisciplinary graduate training programs, such as neuroscience, genetics, or physiology, have incorporated requirements for courses in sleep science. As a result, future sleep investigators must be recruited from among the ranks of individuals who initially identify their interest in some other discipline. These individuals are attracted into sleep only during their graduate studies, often as a result of the imagination or magnetism of specific faculty whom they happened to encounter. In short, existing funding and organizational structures do not have effective mechanisms beyond chance to ensure the necessary pipeline of sleep-trained scientists who can address major public health issues in sleep medicine.
3.4. Challenges to Research
Challenges to research under current academic institutional administrative structures resemble those described above for clinical and educational aims. Few institutions have sleep medicine or sleep science administrative structures that can create an overall, visionary, bird's-eye-view plan for future research in this field. Sleep research is performed in different departments, and sometimes even different schools and hospitals within the same university system. Research priorities, particularly in relation to opportunities for recruitment or resources, are usually determined by non-sleep specialists. Few opportunities exist for coordinated “city planning” when it comes to sleep and biological rhythms. Moreover, on the financial side, indirect costs from sleep research grants typically flow to the institution and parent departments and in many cases are not available to support specific sleep research, relevant infrastructure, or coordinated planning.
4.0. ADVERSE CONSEQUENCES AND FUTURE DIRECTIONS
These many challenges to academic sleep medicine combine to impede advances in patient care, research, and education that could bring fundamental benefit to human health and well-being. Sleep medicine enjoys little distinct visibility or infrastructure support, even at many large and otherwise successful medical systems. These challenges have slowed the maturation of the field even during years when its urgent pertinence and potential benefit to large numbers of patients have been increasingly recognized, and its services have been well reimbursed. Infrastructure limitations have served to dissuade potential trainees from entering the field as clinicians, researchers, or educators. These limitations have preserved the notion that this field is a secondary rather than primary specialty, despite the fact that many of its practitioners consider sleep medicine to be their primary or only active specialty. In short, these barriers have prevented the natural, coordinated, and timely evolution of the field of sleep medicine at academic centers. The influence however extends well beyond academia, as structural models in the community often follow those established at university-based health systems.
Solutions to the challenges outlined in this white paper will not be easy to conceive or simple to implement. Changes cannot be mandated by this Committee, the American Academy of Sleep Medicine, or the Sleep Research Society. Optimal strategies are likely to differ considerably between institutions because no two academic medical centers have identical structures, funding flow models, established interests, and stake holders, not to mention expertise, services, and capability in sleep and biological rhythms. However, the white paper that follows this one attempts to present, possibly for the first time in a comprehensive overview, several desirable structural goals and general strategies, if not specific structural mandates. The Committee identified these goals, among many potential targets, to be paramount in any organized effort to surmount existing barriers for a new field with enormous untapped potential.
CITATION
Chervin RD; Chesson Jr AL; Benca RM; Greenough GP; O'Hearn DJ; Auckley DH; Littner M; Mullington JM; Malhotra A; Berry RB; Malhotra RK; Schulman DA. Organization and structure for sleep medicine programs at academic institutions: part 1—current challenges. SLEEP 2013;36(6):795-801.
DISCLOSURE STATEMENT
Dr. Chervin receives educational grants from Philips Respironics Inc., Fisher Paykel Inc.; receives honoraria as section editor for UpToDate; receives fees for technology licensed by the University of Michigan to Zansors Inc.; is an advisory board member for the non-profit Sweet Dreamzzz Inc.; is named in patents owned by the University of Michigan for signal analysis diagnostic algorithms and hardware relevant to the assessment and treatment of sleep disorders; and serves on the Boards of Directors of the American Academy of Sleep Medicine, American Board of Sleep Medicine, American Sleep Medicine Foundation, and the International Pediatric Sleep Association. Dr. Benca has consulted for Sanofi-Aventis and Merck. Dr. Auckley has received research support from Teva and equipment for research from ResMed. Dr. Littner has participated in speaking engagements and consulted for Forest Pharmaceuticals. Dr. Atul Malhotra is a consultant for Philips Respironics, SHC, SGS, Apnicure, Apnex, and Pfizer. Dr. Berry has received research support from Dymedix, Inc. The other authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The AASM Board of Directors approved the project, funded and staffed meetings of the Academic Affairs Committee, and provided thoughtful review. The SRS Presidential Task Force on Academic Sleep Centers, chaired by Dr. Ruth Benca, developed the questionnaire used to survey academic sleep centers. Members of that Task Force included Drs. Greg Belenky, Daniel Buysse, Ronald Chervin, Carole Marcus, Emmanuel Mignot, Allan Pack, Kathy Parker, Susan Redline, Timothy Roehrs, Clifford Saper, James Walsh, and Phyllis Zee. The survey was administered and data collected by Andrea Roth and Dr. Ruth Benca at the University of Wisconsin. Dr. Allan Pack generously shared his time to explain successes and challenges encountered at the University of Pennsylvania sleep program.
REFERENCES
- 1.Luyster FS, Strollo PJ, Jr, Zee PC, Walsh JK Boards of Directors of the American Academy of Sleep Medicine and the Sleep Research Society Sleep. A health imperative. Sleep. 2012;35:727–34. doi: 10.5665/sleep.1846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Colten HR, Altevogt BM, editors. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. Washington, DC: The National Academies Press; 2006. [PubMed] [Google Scholar]
- 3.Pack AI. Toward comprehensive interdisciplinary academic sleep centers. Sleep. 2007;30:383–4. doi: 10.1093/sleep/30.4.383. [DOI] [PubMed] [Google Scholar]
- 4.Silber MH. Academic sleep centers of the future: An achievable vision. Sleep. 2007;30:244–5. [PubMed] [Google Scholar]
- 5.Mindell JA, Moline ML, Zendell SM, Brown LW, Fry JM. Pediatricians and sleep disorders: training and practice. Pediatrics. 1994;94:194–200. [PubMed] [Google Scholar]
- 6.Teodorescu MC, Avidan AY, Teodorescu M, et al. Sleep medicine content of major medical textbooks continues to be underrepresented. Sleep Med. 2007;8:271–6. doi: 10.1016/j.sleep.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 7.Rosen RC, Rosekind M, Rosevear C, Cole WE, Dement WC. Physician education in sleep and sleep disorders: a national survey of U.S. medical schools. Sleep. 1993;16:249–54. doi: 10.1093/sleep/16.3.249. [DOI] [PubMed] [Google Scholar]
- 8.Strohl KP, Haponik EE, Sateia MJ, et al. The need for a knowledge system in sleep and chronobiology. Acad Med. 2000;75:819–21. doi: 10.1097/00001888-200008000-00013. [DOI] [PubMed] [Google Scholar]
- 9.Young T, Evans L, Finn L, Palta M. Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle-aged men and women. Sleep. 1997;20:705–6. doi: 10.1093/sleep/20.9.705. [DOI] [PubMed] [Google Scholar]
- 10.Chervin RD, Archbold KH, Panahi P, Pituch KJ. Sleep problems seldom addressed at two general pediatric clinics. Pediatrics. 2001;107:1375–80. doi: 10.1542/peds.107.6.1375. [DOI] [PubMed] [Google Scholar]


