Abstract
Objective
To assess recent trends in nonalcoholic fatty liver disease (NAFLD) prevalence among US adolescents.
Study design
Cross-sectional data from 12 714 12–19 year olds (exclusions: chronic hepatitis, hepatotoxic medications) in the National Health and Examination Survey between 1988–1994 and 2007–2010 were used to estimate trends in suspected NAFLD, defined as overweight (body mass index ≥85th percentile) plus elevated alanine aminotransferase levels (boys >25.8 U/L; girls >22.1 U/L). Linear trends in prevalence and the independent effect of demographic indicators and adiposity on NAFLD risk were tested using regression models. Complex sampling methods and P values of <.05 were used to assess statistical significance.
Results
Suspected NAFLD prevalence (SE) rose from 3.9% (0.5) in 1988–1994 to 10.7% (0.9) in 2007–2010 (P < .0001), with increases among all race/ethnic subgroups, males and females, and those obese (P trend ≤.0006 for all). Among those obese, the multivariate adjusted odds of suspected NAFLD were higher with increased age, body mass index, Mexican American race, and male sex; the adjusted odds in 2007–2010 were 2.0 times those in 1988–1994. In 2007–2010, 48.1% (3.7) of all obese males and 56.0% (3.5) of obese Mexican American males had suspected NAFLD.
Conclusion
Prevalence of suspected NAFLD has more than doubled over the past 20 years and currently affects nearly 11% of adolescents and one-half of obese males. The rapid increase among those obese, independent of body mass index, suggests that other modifiable risk factors have influenced this trend.
Nonalcoholic fatty liver disease (NAFLD), is the most common form of liver disease in children.1 A chronic, obesity associated condition, NAFLD can lead to cirrhosis and liver failure over time.2 It is also an independent risk factor for cardiovascular disease and liver cancer.3 Although previous studies have demonstrated differences in NAFLD prevalence rates across race/ethnicity,4,5 sex,6 age,7 and weight status8 subgroups, recent trends among adolescents and adolescent subgroups are not currently available. It is suspected that pediatric NAFLD prevalence has increased in parallel to the increasing trends in overweight and obesity over the past 3 decades9 because of its association with obesity.
Previous reports have used varying approaches to estimate the prevalence of NAFLD.10 Expert Committee guidelines recommend the use of serum transaminase levels11 to screen for NAFLD though the specific cutpoints for defining elevation have not been specified. Alanine aminotransferase (ALT) levels at cutpoints of 30 U/L7 and 40 U/L6 have been commonly used but recent data suggests that such upper limits, which were defined using populations that included persons with subclinical liver disease, are too high.12 Schwimmer et al recently evaluated the normal distribution of ALT levels in US adolescents and proposed a new set of cutpoints for screening for NAFLD based on the 95th percentile of this distribution, 25.8 U/L for boys and 22.1 U/L for girls.6 A comparison of the results using these cutpoints to those obtained using liver ultrasound demonstrated that these sex-specific cutpoints were much more sensitive than the cutpoint of >30 (sensitivity 80% vs 36% for girls and 92% vs 32% for boys) and still highly specific (79% vs 92% for girls and 85% vs 96% for boys).6
The purpose of this study was to use national data, collected using the same or similar methods over the past 3 decades, to estimate current NAFLD prevalence rates among US adolescents and to determine if these rates have risen in line with the increase in obesity prevalence over this period.
Methods
We used national data from 12–19 year olds enrolled in the National Health and Nutrition Examination Survey 1988–1994 (NHANES III) or the continuous National Health and Nutrition Examination Survey (NHANES) between 1999 and 2010 (n = 14 918). NHANES is a cross-sectional survey of the US civilian, noninstitutionalized population designed to obtain nationally representative estimates on diet and health indicators. The sampling methodology is described elsewhere.13 Subjects in the continuous NHANES were grouped into three 4-year periods, 1999–2002, 2003–2006, and 2007–2010 to provide sample sizes large enough to allow for subgroup analyses. Study subjects were excluded for known chronic liver disease (hepatitis B or C; n = 146), missing ALT data (n = 1476), missing data on covariates (n = 294), and treatment with hepatotoxic medications (n = 288; NHANES 1999–2010 only) for a final sample of 12 714. Institutional review board approval from the National Center for Health Statistics was obtained for this study. Signed, informed consent was obtained by National Center for Health Statistics from the parents/guardians of all participants and assent was obtained from all participants.14
Suspected NAFLD was defined as elevated ALT in an overweight or obese child (body mass index [BMI] for age and sex (BMI >85th percentile). Although NAFLD can occur in healthy weight children (particularly those approaching the 85th percentile BMI percentile), it is much more likely to occur in those overweight or obese.7 Elevated ALT was defined using the sex-specific cutpoints recently proposed by Schwimmer et al1 (>25.8 U/L for boys and >22.1 U/L for girls). For comparison purposes, national estimates were also obtained using ALT cutpoints of >30 U/L and >40 U/ L. Serum ALT levels were determined using the enzymatic rate method.15 We examined trends in suspected NAFLD by: weight category, including overweight (BMI 85th –<95th percentile), obese (BMI ≥95th percentile), and severely obese (BMI ≥99th percentile)16; sex; and race/ethnicity (non-Hispanic white, and non-Hispanic black, Mexican American, and other). High waist circumference, a measure of central adiposity, was defined as exceeding the 90th percentile for age, race, and sex as determined by Fernandez et al using data from adolescents participating in NHANES III.17
Statistical Analyses
Complex survey procedures in SAS 9.2 (SAS Institute, Cary, North Carolina) were used for all analyses. Variances were adjusted to account for the sampling methods used and weight factors were applied to estimates to make them representative of the US population. Frequency procedures were used to obtain unadjusted estimates of NAFLD prevalence at each time point studied and to assess trends nationally and by demographic and weight status subgroups. Linear trend testing was done using χ2 tests for trend. Multivariate regression models controlling for age, sex, and race/ethnicity were used to examine the trends in NAFLD prevalence, elevated waist circumference, and BMI z-score among obese males and females. Finally, logistic regression models were used to assess the independent effects of known risk factors (age, sex, race/ethnicity, BMI, and waist circumference) on the odds of suspected NAFLD prevalence among a subsample including only obese adolescents and to compare this risk over time.
Results
A description of the weighted sample for each of the 4 study cycles is provided in Table I. There were no significant differences in age, sex, and percent overweight between NHANES III and the most recently released data cycles (2007–2010), but the proportion of adolescents who were Mexican American, obese, or severely obese did increase over the study period (P for trend <.0001 for all).
Table I.
| 1988–1994 N = 2748 | 1999–2002 N = 4004 | 2003–2006 N = 3824 | 2007–2010 N = 2138 | P trend | |
|---|---|---|---|---|---|
| Age, y | 15.4 (0.1) | 15.5 (0.1) | 15.5 (0.1) | 15.5 (0.1) | .43 |
| Sex, % male | 51.0 (1.8) | 51.4 (1.0) | 51.8 (1.1) | 52.1 (1.2) | .61 |
| Race/ethnicity | |||||
| White (non-Hispanic), % | 67.1 (2.4) | 58.9 (2.0) | 63.0 (2.8) | 58.9 (2.8) | .13 |
| Black (non-Hispanic), % | 14.7 (1.3) | 14.2 (1.7) | 15.2 (1.8) | 14.2 (1.2) | .99 |
| Mexican-American, % | 8.6 (1.0) | 10.9 (1.4) | 11.6 (1.5) | 13.6 (1.9) | .02 |
| Other, % | 9.5 (1.6) | 16.1 (2.1) | 10.2 (1.1) | 13.3 (1.7) | .77 |
| Overweight (BMI 85th – <95th percentile), % | 15.9 (1.0) | 15.8 (0.8) | 17.6 (0.9) | 17.7 (1.0) | .09 |
| Obese (BMI ≥95th percentile), % | 11.2 (1.0) | 18.1 (0.8) | 19.2 (1.3) | 20.0 (1.1) | <.0001 |
| Severe obesity (BMI ≥99th percentile), % | 1.5 (0.4) | 3.6 (0.5) | 4.6 (0.6) | 5.5 (0.9) | <.0001 |
| BMI, z-score | 0.38 (0.03) | 0.54 (0.03) | 0.60 (0.04) | 0.64 (0.03) | <.0001 |
| Waist circumference, cm | 77.0 (0.5) | 80.5 (0.4) | 81.8 (0.5) | 81.7 (0.4) | <.0001 |
Weighted estimates.
Figures presented are means (SE) unless indicated as %.
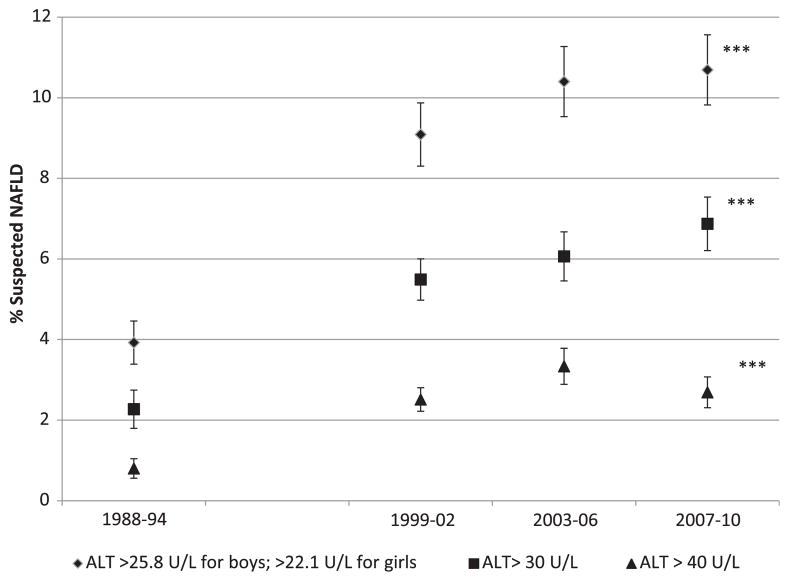
Trends in the unadjusted prevalence of suspected NAFLD, using each of the 3 cutpoints for elevated ALT, doubled among US adolescents between 1988–1994 and 2007–2010, rising from 0.8%–2.7% (P < .0001) using the most specific cutpoint of >40 U/L; from 2.3%–6.9% (P < .0001) using the more sensitive cutpoint of >30 U/L, and from 3.9%–10.7% using the recently defined sex-specific cutpoints of >25.8 U/L for boys and >22.1 U/L for girls (P < .0001) (Figure 1).
Figure 1.
Trends in the unadjusted prevalence of suspected NAFLD among US adolescents 12–19 years old (N = 12 714) defined using overweight plus various cutpoints for elevated ALT, including sex-specific (>25.8 U/L for boys and >22.1 U/L for girls) as well as alternative cutpoints of >40 U/L and >30 U/ L. P for linear trend <.0001 for all.
In stratified analyses, increasing trends in suspected NAFLD prevalence (defined using the sex-specific cutpoints) were observed among all race/ethnic subgroups, among both males and females, and among those obese (Table II). The observed increase in the prevalence among those overweight was not significant. Prevalence was highest among Mexican Americans and lowest among non-Hispanic blacks. Suspected NAFLD prevalence among males was 2 to 3 times that of females.
Table II.
Trends in mean ALT and in the prevalence of suspected NAFLD among US adolescents (12–19 y) by race/ethnicity, sex, and weight status, NHANES 1988–1994 to 2009–2010
| 1988–1994 | 1999–2002 | 2003–2006 | 2007–2010 | P = trend | |
|---|---|---|---|---|---|
| All adolescents | N = 2739 | N = 4004 | N = 3824 | N = 2138 | |
| ALT, mean, U/L | 13.3 (0.3) | 19.1 (0.4) | 19.7 (0.2) | 19.8 (0.3) | <.0001 |
| Suspected NAFLD,* % | 3.9 (0.5) | 9.1 (0.8) | 10.4 (0.9) | 10.7 (0.9) | <.0001 |
| Prevalence of suspected NAFLD* by adolescent subgroup | |||||
| N = 708 | N = 962 | N = 989 | N = 673 | ||
| Non-Hispanic white, % | 4.5 (0.8) | 7.4 (1.1) | 9.7 (1.1) | 10.1 (1.4) | .0006 |
| N = 946 | N = 1167 | N = 1342 | N = 494 | ||
| Non-Hispanic black, % | 1.9 (0.6) | 7.6 (0.9) | 7.8 (0.8) | 9.7 (1.4) | <.0001 |
| N = 953 | N = 1536 | N = 1218 | N = 577 | ||
| Mexican American, % | 5.4 (0.8) | 15.4 (1.1) | 14.9 (0.9) | 15.2 (1.5) | <.0001 |
| N = 1280 | N = 2011 | N = 1956 | N = 1159 | ||
| Males, % | 5.6 (1.1) | 12.1 (1.2) | 14.6 (1.3) | 14.7 (1.3) | <.0001 |
| N = 1459 | N = 1993 | N = 1868 | N = 979 | ||
| Females, % | 2.1 (0.6) | 5.9 (0.8) | 5.8 (0.7) | 6.3 (0.9) | .002 |
| N = 458 | N = 689 | N = 672 | N = 392 | ||
| Overweight (BMI 85th – <95th percentile), % | 10.1 (2.3) | 20.5 (2.5) | 17.8 (1.8) | 17.2 (2.6) | .14 |
| N = 393 | N = 843 | N = 43 | N = 482 | ||
| Obese (BMI ≥95th percentile), % | 20.7 (3.6) | 32.4 (2.4) | 37.9 (2.6) | 38.2 (2.9) | <.0001 |
| N = 67 | N = 184 | N = 214 | N = 133 | ||
| Severely obese (BMI ≥99th percentile), % | 27.2 (10.0) | 52.1 (5.2) | 58.8 (4.1) | 51.6 (7.2) | .03 |
All results are proportions with SE unless indicated as a mean.
Suspected NAFLD = overweight or obesity + ALT >25.8 boys or >22.1 for girls.
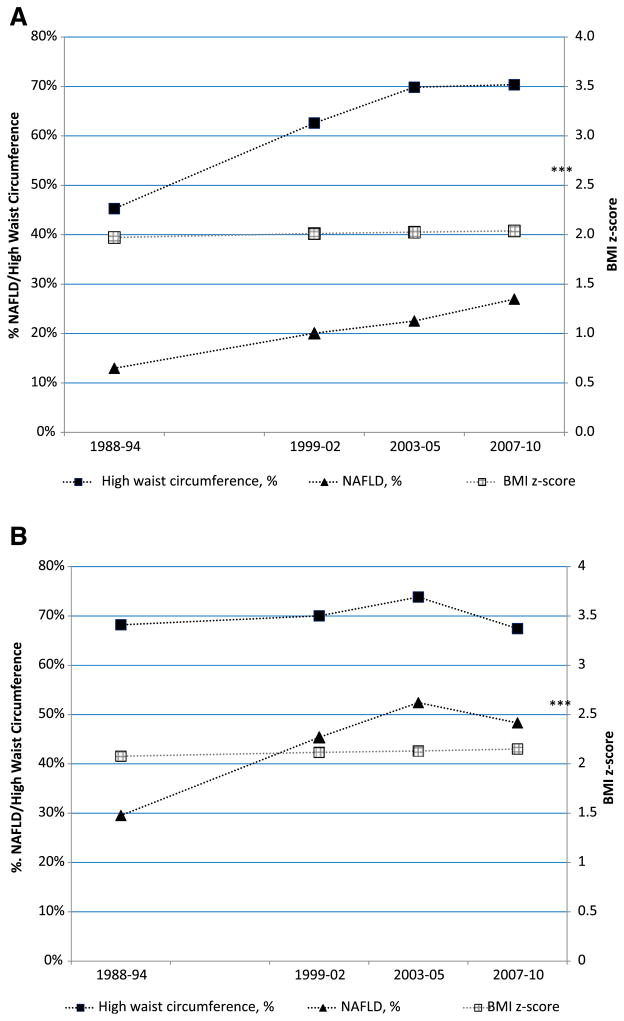
Among obese females, the prevalence of suspected NAFLD, adjusted for age, race/ethnicity and waist circumference, rose from 13.0% (0.03)–27.0% (0.04) (P for trend = .01) (Figure 2; available at www.jpeds.com). Among obese males, prevalence rose from 29.5% (0.06)–48.3% (0.03) (P for trend = .005) (Figure 2). The prevalence of high waist circumference increased among obese females but not obese males. BMI z-score did not increase significantly in either group. Obese males with a high waist circumference were more likely than obese females to have suspected NAFLD, 45.7% vs 18.4%, respectively (not shown).
Figure 2.
Trends in the adjusted prevalence of suspected NAFLD (overweight plus ALT >25.8 U/L for boys and >22.1 U/ L for girls), the prevalence of high waist circumference (>90th sex and age percentile), and mean BMI z-score among A, obese female and B, obese male adolescents in the NHANES III through NHANES 2007–2010. Estimates were adjusted for age and race/ethnicity. P for linear trend was <.0001 for the prevalence of NAFLD in both males and female and for the prevalence of high waist circumference among females. Trends in BMI z-score were not significant for either males or females.
The results of multivariate logistic regression models (Table III) among all adolescents demonstrated that increased age (years), increased BMI (z-score), Mexican American ethnicity (compared with non-Hispanic whites), and being male were all associated with significantly increased risk of NAFLD. Being non-Hispanic black was associated with lower risk compared with non-Hispanic whites. A high waist circumference, when controlling for all covariates, was not associated with increased NAFLD risk. The multivariate adjusted odds of NAFLD in 2007–2010 were 2.0 times those in 1988–1994.
Table III.
Factors associated with increased odds of suspected NAFLD among obese adolescents in the US (N = 2535)
| Effect | N (%) | OR | 95% CI | |
|---|---|---|---|---|
| Age, year | - | 1.2 | 1.2 | 1.3 |
| BMI, z-score | - | 6.5 | 3.6 | 11.6 |
| Race | ||||
| White | 843 (55.0) | reference | ||
| Mexican American | 393 (14.9) | 1.6 | 1.2 | 2.0 |
| Black | 482 (18.4) | 0.4 | 0.3 | 0.6 |
| Other | 817 (11.8) | 1.2 | 0.9 | 1.8 |
| Waist circumference | ||||
| Low (≤90th percentile) | 878 (29.3) | reference | ||
| High (>90th percentile) | 1657 (70.7) | 0.8 | 0.6 | 1.2 |
| Study Year | ||||
| 1988–1994 | 393 (14.9) | reference | ||
| 1999–2002 | 817 (25.2) | 1.8 | 1.1 | 2.9 |
| 2003–2005 | 843 (29.5) | 2.4 | 1.5 | 4.0 |
| 2007–2010 | 482 (30.4) | 2.3 | 1.4 | 3.9 |
Discussion
The findings of this study demonstrate that the prevalence of suspected NAFLD has risen substantially, doubling among US adolescents over the previous 3 decades. Increases in prevalence were observed among both males and females and among all race/ethnic subgroups. Applying the NAFLD prevalence rate of 3.9% observed in 1998–1994 and that of 10.7% observed in 2007–2008 to the estimated total population of adolescents during these time periods (determined using the sampling weights provided by NHANES), this increase represents approximately 2 million additional adolescents with chronic liver disease who are at increased risk of liver failure, cardiovascular disease, and liver cancer in adulthood.
Although the increasing prevalence of obesity and severe obesity over the study period is a likely explanation for some of the observed increase in suspected NAFLD, the findings of this study highlight the importance of other factors. Among those obese, the only weight subgroup to demonstrate a significant increase in suspected NAFLD, the prevalence of severe obesity increased from only 3% in 1988–1994 to 11% in 2007–2010, and the prevalence of suspected NAFLD over the same time period increased from 20% to nearly 40%. Despite the observed increase in severe obesity, the mean BMI z-score did not increase significantly among either obese males or obese females.
As has been demonstrated previously among other populations, NAFLD risk among US adolescents was shown here to be higher with increased age and BMI z-score, male sex, and Mexican American race.1 In 2007–2010, 48% of obese males and 56% of obese Mexican American males had suspected NAFLD. Although the increase in the proportion of Mexican American adolescents over the study period may have contributed to the rise in the NAFLD prevalence rates, the increase in the odds of suspected NAFLD among obese adolescents since 1988–1994 when controlling for race/ethnicity as well as age, sex, BMI, and waist circumference suggests that lifestyle changes have also played a role. Previous research suggests an association between diet, specifically increased consumption of sugar sweetened beverages,10,18,19 and NAFLD risk.
ALT elevation, as applied in this study, is useful as a screening tool and previous studies have supported its utility in both clinical use and population studies. Cutpoints of 30 U/L7 and 40 U/L20,21 have been used in both research studies and clinical practice. Tazawa et al evaluated obese children in Japan in the mid-1990s and found that of those with an ALT >30 IU/L, 83% had an ultrasound consistent with NAFLD (fatty changes).22 The more recent study by Schwimmer et al compared sex-specific cutpoints of 26 U/L for boys and 22 U/L for girls to the results using a cutpoint of >30 U/L and demonstrated substantially improved sensitivity with good specificity for NAFLD.6 In this study, we chose to use these sex-specific cutpoints and added the additional requirement of being overweight or obese to improve the specificity of our analysis and avoid overestimating prevalence.
This study has several strengths, including the availability of multiple, national-level samples collected over a 30-year time period. Data from these samples provided a means for making estimates, representative of the US adolescent population, over a period of substantial change in obesity prevalence. The use of the same or similar data collection methods at each time point and the availability of a sensitive and specific, sex-based measure of suspected NAFLD increases the validity of the results obtained. The use of biologic measures to assess suspected NAFLD, collected using trained personnel and standardized methods, decreases the risk of systematic bias and random error. The availability of anthropometric and demographic data made it possible to assess trends in key subgroups and to assess the independent effect of known or suspected risk factors.
This study was also subject to some limitations. Data on specific medications used was not available for participants in NHANES III, which prohibited us from excluding subjects in 1988–1994 based on their use of hepatotoxic medications as we were able to do for all later time points. This limitation may have resulted in an overestimation of the true prevalence of NAFLD in 1988–1994, but any effect is expected to be minimal as less than 0.03% of the sample in NHANES 1999–2010 reported taking medications known to be hepatotoxic. Also, as the blood samples used to test ALT levels in NHANES III were frozen before they were thawed and analyzed,23 this could have resulted in an attenuation in ALT levels. Although a single freeze-thaw cycle has been shown to decrease ALT levels by as much 8%,24 such a decrease would have had little impact on suspected NAFLD trends in this study as the difference in ALT levels between 1988–1994 and 1999–2002 was 43.6%. Finally, data on alcohol consumption was not collected in subjects <20 years old in NHANES 1999–2010, therefore, we could not assess or control for possible alcohol-induced ALT elevation among the adolescents in this study.
Acknowledgments
Supported by the National Institutes of Health/National Institute of Diabetes and Digestive and Kidney Diseases (K23DK080953 to M.V.)
Glossary
- ALT
Alanine aminotransferase
- BMI
Body mass index
- NAFLD
Nonalcoholic fatty liver disease
- NHANES
National Health and Nutrition Examination Survey
- NHANES III
National Health and Nutrition Examination Survey 1988–1994
Footnotes
The authors declare no conflicts of interest.
References
- 1.Schwimmer JB, Deutsch R, Kahen T, Lavine JE, Stanley C, Behling C. Prevalence of fatty liver in children and adolescents. Pediatrics. 2006;118:1388–93. doi: 10.1542/peds.2006-1212. [DOI] [PubMed] [Google Scholar]
- 2.Kopec KL, Burns D. Nonalcoholic fatty liver disease: a review of the spectrum of disease, diagnosis, and therapy. Nutr Clin Pract. 2011;26:565–76. doi: 10.1177/0884533611419668. [DOI] [PubMed] [Google Scholar]
- 3.Dunn W, Xu R, Wingard DL, Rogers C, Angulo P, Younossi ZM, et al. Suspected nonalcoholic fatty liver disease and mortality risk in a population-based cohort study. Am J Gastroenterol. 2008;103:2263–71. doi: 10.1111/j.1572-0241.2008.02034.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Graham RC, Burke A, Stettler N. Ethnic and sex differences in the association between metabolic syndrome and suspected nonalcoholic fatty liver disease in a nationally representative sample of US adolescents. J Pediatr Gastroenterol Nutr. 2009;49:442–9. doi: 10.1097/MPG.0b013e31819f73b4. [DOI] [PubMed] [Google Scholar]
- 5.Quiros-Tejeira RE, Rivera CA, Ziba TT, Mehta N, Smith CW, Butte NF. Risk for nonalcoholic fatty liver disease in Hispanic youth with BMI ≥95th percentile. J Pediatr Gastroenterol Nutr. 2007;44:228–36. doi: 10.1097/MPG.0b013e31802d4acc. [DOI] [PubMed] [Google Scholar]
- 6.Schwimmer JB, Dunn W, Norman GJ, Pardee PE, Middleton MS, Kerkar N, et al. SAFETY study: alanine aminotransferase cutoff values are set too high for reliable detection of pediatric chronic liver disease. Gastroenterology. 2010;138:1357–64. doi: 10.1053/j.gastro.2009.12.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Strauss R, Barlow S, Dietz W. Prevalence of abnormal serum amino-transferase values in overweight and obese adolescents. J Pediatr. 2000;136:727–33. [PubMed] [Google Scholar]
- 8.Arsenault BJ, Beaumont EP, Despres JP, Larose E. Mapping body fat distribution: a key step towards the identification of the vulnerable patient? Ann Med. 2011 doi: 10.3109/07853890.2011.605387. http://dx.doi.org/10.3109/07853890.2011.605387. [DOI] [PubMed]
- 9.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA. 2012;307:483–90. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vos MB, McClain CJ. Nutrition and nonalcoholic fatty liver disease in children. Curr Diab Rep. 2008;8:399–406. doi: 10.1007/s11892-008-0069-z. [DOI] [PubMed] [Google Scholar]
- 11.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl 4):S164–92. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 12.Prati D, Taioli E, Zanella A, Della Torre E, Butelli S, Del Vecchio E, et al. Updated definitions of healthy ranges for serum alanine aminotransferase levels. Ann Intern Med. 2002;137:1–10. doi: 10.7326/0003-4819-137-1-200207020-00006. [DOI] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention (CDC). National Center for Health Statistics (NCHS) [Accessed September 14, 2011];Key Concepts About NHANES Survey Design. Available at: http://www.cdc.gov/nchs/tutorials/Nhanes/SurveyDesign/SampleDesign/Info1.htm.
- 14.Grundy SM, Bilheimer D, Blackburn H. Rationale of the diet-heart statement of the American Heart Association. Report of Nutrition Committee Circulation. 1982;65:839A–54A. [PubMed] [Google Scholar]
- 15.National Center for Health Statistics, Centers for Disease Control and Prevention. [Accessed May 26, 2012];Laboratory Procedures Used for the Third National Health and Nutrition Examination Survey (NHANES III), 1988–1994. Available at: http://www.cdc.gov/nchs/data/nhanes/nhanes3/cdrom/nchs/manuals/labman.pdf.
- 16.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, et al. CDC growth charts: United States. Advance data. 2000;8:1–27. [PubMed] [Google Scholar]
- 17.Fernandez JR, Redden DT, Pietrobelli A, Allison DB. Waist circumference percentiles in nationally representative samples of African-American, European-American, and Mexican-American children and adolescents. J Pediatr. 2004;145:439–44. doi: 10.1016/j.jpeds.2004.06.044. [DOI] [PubMed] [Google Scholar]
- 18.Vos MB, Colvin R, Belt P, Molleston JP, Murray KF, Rosenthal P, et al. Correlation of vitamin E, uric acid, and diet composition with histologic features of pediatric NAFLD. J Pediatr Gastroenterol Nutr. 2012;54:90–6. doi: 10.1097/MPG.0b013e318229da1a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vos MB, Kimmons JE, Gillespie C, Welsh J, Blanck HM. Dietary Fructose Consumption Among US Children and Adults: the Third National Health and Nutrition Examination Survey. Medscape J Med. 2008;10:160. [PMC free article] [PubMed] [Google Scholar]
- 20.Schwimmer JB, McGreal N, Deutsch R, Finegold MJ, Lavine JE. Influence of gender, race, and ethnicity on suspected fatty liver in obese adolescents. Pediatrics. 2005;115:e561–5. doi: 10.1542/peds.2004-1832. [DOI] [PubMed] [Google Scholar]
- 21.Siest G, Schiele F, Galteau MM, Panek E, Steinmetz J, Fagnani F, et al. Aspartate aminotransferase and alanine aminotransferase activities in plasma: statistical distributions, individual variations, and reference values. Clin Chem. 1975;21:1077–87. [PubMed] [Google Scholar]
- 22.Tazawa Y, Noguchi H, Nishinomiya F, Takada G. Serum alanine amino-transferase activity in obese children. Acta Paediatrica (Oslo, Norway:1992) 1997;86:238–41. doi: 10.1111/j.1651-2227.1997.tb08881.x. [DOI] [PubMed] [Google Scholar]
- 23.National Center for Health Statistics, Centers for Disease Control and Prevention. [Accessed May 26, 2012];NHANES III Lab Public-Use Data Files Usage Notes. Available at: http://www.cdc.gov/nchs/nhanes/nhanes3/lab_usagenotes.htm.
- 24.Prasad R, Welch C. Effect of pyrldoxal 5-phosphate on the stability of alanlne aminotransferase. Clin Chem. 1992;38:2340–1. [PubMed] [Google Scholar]